Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 13
Effect of Ageing Process and Brushing on Color Stability and Surface Roughness of Treated White Spot Lesions: An in vitro Analysis
Authors Almulhim K , Khan AS , Alabdulghani H , Albasarah S , Al-Dulaijan Y , al-Qarni FD
Received 17 August 2021
Accepted for publication 15 September 2021
Published 1 October 2021 Volume 2021:13 Pages 413—419
DOI https://doi.org/10.2147/CCIDE.S334633
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Christopher E. Okunseri
Khalid Almulhim,1 Abdul Samad Khan,1 Hanan Alabdulghani,2 Sara Albasarah,2 Yousif Al-Dulaijan,3 Faisal D al-Qarni3
1Department of Restorative Dental Sciences, College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 2College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia; 3Department of Substitutive Dental Sciences, College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
Correspondence: Faisal D al-Qarni
Department of Substitutive Dental Sciences, College of Dentistry, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
Tel +966 13 333 1404
Email [email protected]
Purpose: To evaluate the effect of ageing process and brushing on the color stability and surface roughness of white spot lesions treated with resin infiltration or remineralization.
Patients and Methods: Artificial white spot lesions were created on the facial surface of extracted bovine teeth. Specimens were divided into three main groups based on treatment received: resin infiltration (Icon), MI Paste Plus (MI) or no treatment (control). Specimens underwent pH cycling for 7 days, followed by brushing with toothbrush simulator. Specimens were then immersed in three different solutions (water, cranberry juice, or coffee) for 7 days. Surface roughness (SR) and color stability (CS) assessments were performed at baseline and after each test. One-way and two-way ANOVA were used to calculate the statistical comparisons between the groups and significance considered at P < 0.05.
Results: Icon group had the least color change after pH cycling, while MI showed the least color change after brushing test. Immersion in coffee produced the highest color change in all groups, followed by cranberry juice. Icon group had the best color stability when immersed in cranberry juice or coffee. Control and the MI treated specimens showed gradual increase of SR after pH cycling and brushing test, while Icon group had improved surface properties. Brushing test alone produced less color change in comparison with immersion in cranberry juice and coffee; however, brushing increased SR.
Conclusion: Icon treatment showed superior color stability and surface roughness, compared to the control and the MI treated teeth. Brushing had less influence on color change compared to the immersion in cranberry juice or coffee.
Keywords: white spot lesion, surface roughness, color stability, resin infiltration
Introduction
White spot lesion (WSL) is a localized area of demineralization which is observed as a white opaque spot and considered as the first sign of dental caries.1,2 WSL is commonly associated with orthodontic treatment, poor oral hygiene, and some are related to enamel developmental defects such as hypoplasia and hypocalcification.2,3 The prevalence of WSL among orthodontic patients ranges from 2–96% and is mostly on the labial surface of the lateral incisors.3,4 These lesions should be detected early to prevent further demineralization and cavitation.5 WLS can be treated with multiple treatment options starting from traditional restorations, veneers, and crowns which need removal of enamel beyond the demineralized area and may also reach dentin layer.2 Topical remineralization of these lesions can also be done either with casein phosphopeptide amorphous calcium phosphate (CPP-ACP) such as MI Paste, and MI Paste plus, or with fluoride toothpaste, varnish, mouthwash, and gels.1,2,4,6 Another treatment option of WSL is micro-abrasion and bleaching which can be done when remineralization is insufficient.2 Moreover, a non-invasive approach using resin infiltration material (Icon) has also been found to be effective in treating WSL.1,4–6
Resin infiltration is a non-invasive restorative treatment option for initial caries lesion. It has the ability to penetrate and fill the porous widened inter-crystalline spaces of demineralized enamel, thereby blocking the microporosities mechanically, preventing the entry of acids, and arresting the lesion. This was discussed as early as 1970s;7,8 in vitro studies found that resin infiltration significantly enhances the surface hardness of WSL when compared with other surface treatments.6 In vivo studies have also proven the effectiveness of resin infiltration in treating WSL, and showed significantly improved clinical appearance.2,9 However, surface properties of resin-infiltrated WSLs, when compared to sound enamel, are still unknown.6
Longevity of resin restorative materials is still a major concern due to the challenges of the oral environment. They undergo color changes when exposed to chromogenic foods, which in turn lead to compromised esthetics and patient dissatisfaction.2,5,10 Another factor that may affect color stability is the surface roughness of the restoration, which can be increased due to mechanical effect of toothbrushing. Moreover, the oral cavity constantly goes through chemical and physical changes that have been reported to influence surface properties of resin restorative materials as well as their longevity and durability.5
This study aimed to evaluate the effect of ageing process and brushing on the color stability (CS) and surface roughness (SR) of treated WSL with non-invasive restorative treatments. The null hypothesis of this study was that the ageing process, brushing and beverages’ consumption do not affect the color stability and surface roughness of treated WSL with non-invasive restorative treatments.
Materials and Methods
Specimen Size and Preparation
Ninety sound extracted bovine teeth were collected and carefully cleaned and disinfected. Teeth were then stored in distilled water until use in order to prevent micro-organism accumulation and growth. Artificial WSL was created on the facial flat surface of each tooth by placing 6 mm diameter circular sticker in the selected site of the WSL, while the remaining exposed surface was covered with acid resistant nail polish.11 The sticker was removed after the nail polish dried, leaving the 6 mm circle of enamel exposed to create the WSL on it. Demineralization solution was prepared as described in Table 1, with pH = 4.4, that was refreshed every 3 days. Each specimen was immersed in 15 mL of demineralization solution in a sealed glass container for 96 hours to create WSL. Then specimens were thoroughly washed under running distilled water for 5 minutes.12 WSL was then inspected using an optical microscope (Olympus BX51, Olympus, Miami, FL, USA).
 |
Table 1 Demineralization/Remineralization Solutions13 |
Treatment of WSL
Specimens were divided into three main groups based on the treatment to be received.
- Control group (no treatment): 30 specimens were stored in distilled water.
- Icon (resin infiltration): 30 specimens were treated with resin material for infiltration (Icon, DMG, Hamburg, Germany). The infiltration treatment was performed following the manufacturer’s instructions:
- Icon-Etching for 2 min.
- Water rinse and air dry for 30 s.
- Icon-Dry for 30 s.
- Previous steps repeated 2 more times.
- Icon-Infiltrant for 3 min then light cure 40 s.
- Icon-Infiltrant for 1 min then light cure 40 s.
- Finishing and polishing with Sof–Lex XT discs (3M ESPE, St Paul, Minnesota) gradually from the mid-coarse to the extra-fine disc. A slow-speed handpiece was used with water spray (15,000 rpm, 15 seconds/disc) using intermittent brushing movement and gentle pressure.
- 3. MI Paste Plus: 30 specimens were treated with MI Paste Plus (MI Paste Plus, GC America Inc, Alsip, IL, USA) application to the site by a cotton swab then washed with normal saline after 5 min.
After treatment, all specimens were evaluated for surface roughness and color stability as baseline records.
pH Cycling
All specimens were exposed to pH cycling using demineralization/remineralization solutions to evaluate the acid resistance of the treated surfaces. Each specimen was placed in the 15 mL of demineralization solution in a sealed glass container for 8 h and then washed thoroughly under running distilled water for 5 min. Then every specimen was immersed in 15 mL of remineralization solution for 16 h in sealed glass containers and then washed thoroughly under running distilled water for 5 min, which completed one cycle. Solutions were refreshed every 3 days and pH was maintained at 4.4 for demineralization solution and 7 for remineralization solution. A total of seven cycles (7 days) were conducted for each specimen. The components of the demineralization and remineralization solutions are listed in Table 1.
Brushing Test
Ten specimens from each group were subjected to brushing test. Toothbrushing simulator machine (Toothbrush simulator ZM-3.8. SD Mechatronik gmbh, Feldkirchen-Westerham. Germany) was used containing soft toothbrushes with nylon bristles. Total of 224,000 cycles were used to simulate 0.7 years of brushing by applying a brushing movement with a load of 2 N on the specimen surfaces, an amplitude of excursion of 20 mm, and a speed of 4.5 movements per second.
Immersion in Solutions
From each group, 6 specimens were immersed in distilled water as a control solution, while 6 specimens were immersed in cranberry juice (Ocean Spray, Lakeville-Middleboro, Mass, USA), and the other 6 specimens were immersed in coffee (Nescafe Gold, Nestle, Frankfurt, Germany). To prepare the coffee solution, 10 g of coffee was poured in 500 mL of boiling distilled water then cooled in room temperature. The specimens were immersed in their designated solution for 7 days, solutions were changed every day, to simulate extrinsic dietary staining. The specimens of all groups were then re-evaluated for surface roughness and color stability after the immersion.
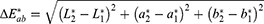
Color Stability Assessment
The color of the specimens was measured with a spectrophotometer (X-Rite, Grand Rapids, MI, USA) for digital color measurements. The color measurements were recorded by means of the CIELAB (Commission International de L’Eclairage L*a*b) color notation system. The baseline measurements of all specimens were made (immediately after the treatment), after pH cycling, after brushing test, and after immersing in different staining solutions. ΔE was calculated using the following formula:
Surface Roughness Assessment
Surface roughness of all specimens was measured using Contour GT Surface Roughness Tester (3D profilometer. Bruker, AZ, USA). Three measurements were recorded for each specimen and the average was calculated. Measurements were taken at different time intervals for all the specimens; at baseline (immediately after the treatment), after pH cycling, after brushing, and after immersing in different staining solutions.
Statistical Analysis
Results were presented as mean and standard deviations. One-way analysis of variance (ANOVA) was used to calculate the statistical comparisons between the groups.
Two-way ANOVA was employed to study combined comparison between the treatment types and the subject test. Significance was considered at p < 0.05.
Results
Color Stability
Means and standard deviations (SD) of ΔE values are presented in Table 2. Icon group was found to have the least color change after pH cycling. However, MI Paste Plus showed the least color change after brushing test. Immersion in coffee was found to show the highest change in color among all groups, followed by juice, then water. The highest ΔE was found in MI Paste Plus group that was immersed in coffee. The least ΔE was found in MI Paste Plus group that was immersed in water.
 |
Table 2 One-Way ANOVA Analysis of the Subject Tests for ΔE |
One-way ANOVA analysis (Table 2) showed a statistically significant difference in ΔE between the subject tests in the control and MI Paste Plus treatment types (p<0.05), which was only observed after immersion in cranberry juice and coffee (p<0.05).
Two-way ANOVA analysis showed statistically significant difference in ΔE between the treatment type and between the subject test (p<0.05) as shown in Table 3. Moreover, a statistically significant difference was found in the interaction between the treatment type and the subject test (p<0.05).
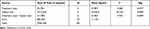 |
Table 3 Two-Way ANOVA Analysis of ΔE Between the Treatment Types and Between the Subject Tests |
Surface Roughness
With regards to surface roughness (SR) of treated teeth, both control and MI treated groups showed gradual increase of SR after pH cycling and brushing test. On the other hand, Icon group showed improvement in its surface properties. Table 4 shows the mean SR (μm) of all groups. The highest mean SR was in the MI treatment type after brushing. The least SR was in control group after being immersed in coffee.
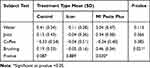 |
Table 4 One-Way ANOVA Analysis of the Subject Tests for SR (μm) |
One-way ANOVA showed the significance in SR between different treatment types with the different subject tests (Table 4). A statistically significant difference in SR was found between the subject tests in MI treatment type only (p<0.05).
One-way ANOVA analysis (Table 4) between the different subject tests showed a statistically significant difference in SR between the treatment types in brushing only (p<0.05).
Two-way ANOVA showed a statistically significant difference in SR (mean difference between baseline and brushing/immersion) between the solution only (p<0.05). As shown in Table 5, the interaction between the treatment type and the solution was statistically significant (p<0.05).
 |
Table 5 Two-Way ANOVA Analysis of SR (μm) Between the Treatment Types and Between the Subject Tests |
Discussion
As white spot lesions are commonly seen in dental practice and its treatment is recommended as early as possible to prevent further progression, multiple treatment options have been introduced including non-invasive restorative treatments.1,2,5 Resin infiltration (Icon) is one of the recent and promising non-invasive restorative treatment options.6–8 However, behavior under simulated oral conditions remains uncertain.2,5,6,10 This study aimed to evaluate the effect of ageing process and brushing on the color stability and surface roughness of WSL treated with non-invasive restorative treatments. The null hypothesis of this study was rejected as the ageing process, brushing, and beverages’ consumption did not affect the color stability and surface roughness of WSL treated with resin infiltration.
Patients are mostly concerned with esthetics and masking the white appearance of the WSL. Therefore, color stability assessment was done in this study considering the influence of common chromogenic liquids such as coffee and cranberry juice. Brushing WSL is another factor that affects the color stability mechanically by affecting the surface roughness of the restoration.
The change in color was highest in the untreated WSL, while the WSL treated with Icon had superior color stability after pH cycling. This is in agreement with a previous study, where resin infiltration with Icon was capable of masking the initial caries lesion after treatment as well as after subsequent pH cycling.14 Another in vitro study also showed that resin infiltration reliably masks artificial caries lesions and proved to be resistant to staining.15 However, WSL treated with Icon had the highest color change, while a previous study reported conflicting results, as infiltrated white lesions resisted mechanical abrasion that was done by brushing simulator.5 The different results may be due to the different number of cycles, as the previous study performed 10,000 strokes of tooth brushing, while in this study specimens were subjected to 224,000 cycles.
Upon immersion in commonly consumed beverages, coffee was found to have the most intense and dark stains in all groups, followed by cranberry juice. That is in agreement with many previous studies.17–19 This staining effect could be due to the presence of tannic acid and pigments in coffee with low polarity that cause staining due to their affinity to the polymer network, and the presence of anthocyanin pigment in cranberry juice.20
A previous study reported that highly concentrated fluoride treatments inhibit further progression of WSL, however, the unfavorable appearance of the lesions was not considerably masked.14 Similarly, this study showed that WSLs treated with MI had the most color change after immersion in coffee and juice.
In the present study, Icon infiltration improved the surface roughness of WSL compared to untreated lesions. This is in agreement with a previous study which reported that Icon reduced roughness, although not equal to sound enamel.16 After pH cycling, WSLs treated with Icon showed improved surface roughness compared to MI treated, and untreated WSL, while in a previous study, it has been reported that the resin infiltrant was unable to protect enamel from pH cycling in terms of surface roughness. This could be due to differences in pH cycling methods.5
After brushing, WSL treated with Icon showed improved surface roughness compared to MI treated, and untreated WSL. This is in agreement with a previous study where brushing stimulation was unable to remove resin infiltrant.5 This mechanical load resistance could be due to the thick layer of material, since two layers of resin infiltrant are recommended by the manufacturer. In addition, cranberry juice was found to have the worst effect on surface roughness among all groups, followed by coffee. This could be attributed to the acidic pH of cranberry juice, and the fact that it contains anthocyanin; a food pigment that is present in grapes, blueberries, and cranberries, which has also been reported to cause discoloration in red wines.20
Resin infiltration (Icon) can be used as non-invasive restorative treatment for treating white spot lesions, which could effectively mask the white appearance and have acceptable color stability, and improved surface roughness.6–8
Further studies testing the effect of thermal changes to better simulate oral conditions are needed. Additionally, pH cycling could be extended for more than 7 cycles to simulate longer period of ageing. Extracted human teeth may be used for future studies to better simulate clinical conditions.
Conclusion
WSL treated with Icon resin infiltration had better outcomes in terms of color stability and surface roughness, compared to the MI treated teeth and untreated WSL. Moreover, brushing the treated WSL showed less effect on color change compared to the effect after immersion in juice and coffee. Also, immersion in coffee showed the highest staining effect on treated and untreated WSL.
Acknowledgments
The authors would like to thank Mr. Robert Caravana for his assistance in conducting the tests, and Dr. Ashwin Shetty for statistical consultation and analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Heymann GC, Grauer D. A contemporary review of white spot lesions in orthodontics. J Esthet Restor Dent. 2013;25:85–95. doi:10.1111/jerd.12013
2. Senestraro SV, Crowe JJ, Wang M, et al. Minimally invasive resin infiltration of arrested white-spot lesions: a randomized clinical trial. J Am Dent Assoc. 2013;144(9):997–1005. doi:10.14219/jada.archive.2013.0225
3. Srivastava K, Tikku T, Khanna R, Sachan K. Risk factors and management of white spot lesions in orthodontics. J Orthod Sci. 2013;2:43–49. doi:10.4103/2278-0203.115081
4. Sangamesh B, Kallury A. Iatrogenic effects of orthodontic treatment–review on white spot lesions. Int J Sci Eng Res. 2011;2:2–16.
5. Neres ÉY, Moda MD, Chiba EK, Briso A, Pessan JP, Fagundes TC. Microhardness and roughness of infiltrated white spot lesions submitted to different challenges. Oper Dent. 2017;42(4):428–435. doi:10.2341/16-144-L
6. Zakizade M, Davoudi A, Akhavan A, Shirban F. Effect of resin infiltration technique on improving surface hardness of enamel lesions: a systematic review and meta-analysis. J Evid Based Dent Pract. 2020;20:101405. doi:10.1016/j.jebdp.2020.101405
7. Davila JM, Buonocore MG, Greeley CB, Provenza DV. Adhesive penetration in human artificial and natural white spots. J Dent Res. 1975;54:999–1008. doi:10.1177/00220345750540054201
8. Kielbassa AM, Muller J, Gernhardt CR. Closing the gap between oral hygiene and minimally invasive dentistry: a review on the resin infiltration technique of incipient (proximal) enamel lesions. Quintessence Int. 2009;40:663–681.
9. Borges AB, Caneppele TM, Masterson D, Maia LC. Is resin infiltration an effective esthetic treatment for enamel development defects and white spot lesions? A systematic review. J Dent. 2017;56:11–18. doi:10.1016/j.jdent.2016.10.010
10. Cohen-Carneiro F, Pascareli AM, Christino MR, Vale HF, Pontes DG. Color stability of carious incipient lesions located in enamel and treated with resin infiltration or remineralization. Int J Paediatr Dent. 2014;24:277–285. doi:10.1111/ipd.12071
11. Gurdogan EB, Ozdemir-Ozenen D, Sandalli N. Evaluation of surface roughness characteristics using atomic force microscopy and inspection of microhardness following resin infiltration with icon®. J Esthet Restor Dent. 2017;29:201–208. doi:10.1111/jerd.12279
12. Mandava J, Reddy YS, Kantheti S, et al. Microhardness and penetration of artificial white spot lesions treated with resin or colloidal silica infiltration. J Clin Diagn Res. 2017;11:ZC142–ZC146.
13. Firzok H, Zahid S, Asad S, Manzoor F, Khan AS, Shah AT. Sol-gel derived fluoridated and non-fluoridated bioactive glass ceramics-based dental adhesives: compositional effect on re-mineralization around orthodontic brackets. J Non Cryst Solids. 2019;521:119469. doi:10.1016/j.jnoncrysol.2019.119469
14. Wierichs RJ, Kogel J, Lausch J, Esteves-Oliveira M, Meyer-Lueckel H. Effects of self-assembling peptide P11-4, fluorides, and caries infiltration on artificial enamel caries lesions in vitro. Caries Res. 2017;51:451–459. doi:10.1159/000477215
15. Paris S, Schwendicke F, Keltsch J, Dörfer C, Meyer-Lueckel H. Masking of white spot lesions by resin infiltration in vitro. J Dent. 2013;41:e28–e34. doi:10.1016/j.jdent.2013.04.003
16. Yazkan B, Ermis RB. Effect of resin infiltration and microabrasion on the microhardness, surface roughness and morphology of incipient carious lesions. Acta Odontol Scand. 2018;76:473–481. doi:10.1080/00016357.2018.1437217
17. Bagheri R, Burrow MF, Tyas M. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J Dent. 2005;33(5):389–398. doi:10.1016/j.jdent.2004.10.018
18. Fay RM, Walker CS, Powers JM. Discoloration of a compomer by stains. J Gt Houst Dent Soc. 1998;69:12–13.
19. Chan KC, Fuller JL, Hormati AA. The ability of foods to stain two composite resins. J Prosthet Dent. 1980;43(5):542–545. doi:10.1016/0022-3913(80)90328-5
20. Oliveros Soles J. In-vitro Beverage Discoloration, Stain Removal and Tooth-Brushing Abrasion of Crown and Bridge Provisional Materials [Doctoral dissertation, Boston Univeristy]. 2017. Available from: https://open.bu.edu/handle/2144/26379.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.