Back to Journals » Patient Preference and Adherence » Volume 15
Effect of a Template Case Report Based on Cognitive Task Analysis on Emergency Thinking Ability of Resident Doctors in Standardized Training
Authors Guo H, Qi HJ, Li XR, Xu N, Zhao Q, Shen ZS, Jia YJ, Li JG
Received 14 January 2021
Accepted for publication 15 June 2021
Published 15 July 2021 Volume 2021:15 Pages 1585—1591
DOI https://doi.org/10.2147/PPA.S302025
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Naifeng Liu
Hui Guo,1,* Hui-Jun Qi,1,* Xu-Rui Li,2 Ning Xu,1 Qian Zhao,1 Zhang-Shun Shen,1 Yang-Juan Jia,1 Jian-Guo Li1
1Department of Emergency, Hebei General Hospital, Shijiazhuang, 050051, People’s Republic of China; 2Department of General Practice, Hebei General Hospital, Shijiazhuang, 050051, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jian-Guo Li
Department of Emergency, Hebei General Hospital, No. 348 West HePing Boulevard, Shijiazhuang, 050051, People’s Republic of China
Tel +86 18633012328
Email [email protected]
Objective: To explore the effect of a template case report based on cognitive task analysis on the emergency thinking ability of resident doctors in standardized training.
Methods: The doctors were split into two groups, according to the date they joined the emergency department (n = 40, each group): the observation and control groups. In the observation group, the resident doctors’ teachers in standardized training adopted the cognitive task analysis method to determine the primary links of emergency thinking, made case templates, and carried out training based on the case template report. In the control group, traditional teaching methods were used by the teachers.
Results: In the observation and control groups, the scores at departure were 88.10 ± 3.88 and 75.23 ± 7.19, respectively (P < 0.05), and the student’s ability improvement rates were 92.5% and 75.0% (P < 0.01). In addition, the awareness rate of “know how to study” and “know how to work in emergency” in the observation group was 90% and 90%, respectively. The rate of doctors that considered “missed diagnosis and misdiagnosis can be reduced” was 85%, and the rate of doctors that considered “help to learn in other departments in the future” was 80%.
Conclusion: Template case reports based on the cognitive task analysis for emergency thinking training can help resident doctors in standardized training improve their emergency thinking ability.
Keywords: emergency thinking, case report, process thinking, semeiology, rules from the physician
Introduction
Emergency medicine covers a wide range of diseases, which can lead to uncertainty and unpredictability. It remains a significant challenge for clinical teaching to let resident doctors in standardized training (ST doctors) master the diagnosis and treatment of many kinds of diseases in a short period.1 Therefore, it is more important to train ST doctors for emergency clinical thinking, which is more feasible and effective, and requires less effort, than to master specific diseases.2,3 However, the traditional clinical teaching model was less focused on the training of emergency thinking, and the teaching methods of hospitals in different regions and levels are quite diverse. Hence, there is an urgent need to establish a clinical teaching model suitable for emergency medicine development.4,5 Since the 1980s, the “cognitive revolution” based on psychology and pedagogy has accelerated the development of cognitive task analysis (CTA), which gradually replaced traditional task analysis, and achieved remarkable results.4 The high risk of emergency needs the experience accumulation and process optimization skills of emergency physicians to ensure the safety of patients. In addition, as mentioned before, the complexity of emergency patients makes it difficult to construct an emergency teaching system. To overcome these difficulties, through the cognitive task analysis method,5,6 combined with the clinical characteristics of emergency, the emergency process was summed up, and a case template developed, thereby helping ST doctors to be able to establish the clinical thinking mode quickly. Emergency medicine has a wide range, with a high degree of randomness and unpredictability. Professional emergency doctors still feel that they are walking on thin ice, and it is even more difficult for the regularized doctors who are new to the emergency department to adapt. According to the survey. Teaching methods such as leading teachers, daily ward rounds, standard diagnosis and treatment videos, clinical skill training, writing of medical documents, and analysis of typical medical records still have some deficiencies in the training of clinical thinking ability.9 How to make the students adapt to the study of emergency department in a short time is worth discussing.
Traditional training is mainly dependent on experience, so it is a decision in an emergency. It is also based on experience.2,3 Thus, it is different among individuals, and teachers have varied thinking in prioritizing. Therefore, the present study aims to investigate the effect of a template case report based on CTA on the emergency thinking ability of ST doctors, and explore its clinical effect, to identify the homogenous training model for emergency thinking, and help ST doctors quickly understand the characteristics of de-escalation thinking in an emergency, and master the emergency workflow.
Materials and Methods
Subjects
The ST doctors who joined the Emergency Department of our hospital from October 2018 to March 2019 were included in the present study. According to the date they joined the Emergency Department (n = 40, each group), these doctors were assigned into two groups: the observation group and the control group. October 2018–December 2018: control group; January 2019–March 2019: observation group. Forty people were in each group. In this study, there were two months for training, examination, and evaluation cycle into the emergency rotation with more than two months for the doctor as the research object. The ST doctors in the observation group accepted the report template case teaching methods. It should be noted that the doctors are all graduate students. There were 24 doctors (60%) with no working experience from our college and 13 doctors (32.5%) with 3-5 years of working experience from other colleges. And there were three doctors (7.5%) who were graduate students. The traditional teaching method was adopted in the control group. A total of 40 subjects were included, including 11 males (27.5%) and 29 females (72.5%). There were 23 doctors (57.5%) with no working experience from our college, all of whom have graduate degrees; 13 doctors (32.5%) with 3-5 years of working experience from other colleges, all of whom have bachelor degrees; and 4 doctors (10%) who were graduate students. Although people with work experience may be different, there is no statistical difference between entrance examination and age. After careful evaluation, we believe that the two groups are comparable. This study was exempted by the Ethics Committee of Hebei General Hospital because it involved only information recorded by investigators in a manner that did not allow identification of subjects either directly or through identifiers associated with the subjects. All ST doctors provided signed informed consent. The ST doctors’ backgrounds were relatively clear (Supplemental Table), and the cognitive background differences between the two groups were re-evaluated through the entrance examination.
Inclusion and Exclusion Criteria
Inclusion criteria: (1) ST doctors who joined the Emergency Department of our hospital from October 2018 to March 2019, and (2) who provided signed informed consent. Exclusion criteria: (1) ST doctors who participated in other teaching and training activities, (2) ST doctors who asked for leave or withdrew during the training, and (3) ST doctors who were unable to participate in the graduation examination due to personal reasons.
Teaching Methods
Teaching
All the teachers we selected are experienced emergency department physicians who have obtained the qualification of attending physician in the emergency department for more than five years and obtained the qualification of teaching physician in regular training through professional teacher training. The template was developed through discussion by emergency experts.
With over five years of work experience, they can conduct symptom-oriented clinical practice research and are skilled in diagnosing and differential diagnosis of common, frequently-occurring, and acute diseases in the emergency department. The “three basics” (basic theory, basic skills, basic operation) assessment performance is good, and the level is equivalent.
In the first week of admission, all ST doctors in the Emergency Department were intensively taught by the teaching secretary. The introduction to symptomatology with emergency thinking was taught. The contents mainly included three aspects: the process of differential diagnosis of symptomatology, the manner of de-escalation thinking—which means that the patients’ diseases are excluded according to particular methods, from life-threatening conditions to general diseases, from rapidly progressing to slowly progressing diseases, from organic diseases to functional disorders—and first aid treatment. The presenter made the courseware. The observation group adopted the template case report method, while the control group adopted the traditional case report method.
In the traditional group, the patient’s general condition, chief complaint, history of present illness, physical examination, laboratory examination, diagnosis, and discussion were recorded. The process is thinking what the disease could be, and then verify what it is not the disease. Our approach was to record cases entirely in the actual treatment process template, similar to “tabletop deduction.” The order is chief complaint, general condition (condition rating), and the severity of the patient’s condition. If the patient is seriously ill, ask only about the history of the present illness, perform the necessary physical examination and rapid laboratory tests, obtain the laboratory results report, then carry out a second assessment to determine the diagnosis. If the patient is mildly ill, a detailed history of the present illness and a thorough physical examination will be conducted, along with specific laboratory tests. The results will be reported, and then the diagnosis will be re-assessed.
Establishment of the Case Template
The present study adopted the case teaching method.6–8 The teacher formulated the case template in accordance with the de-escalation principle of emergency, which was guided by the symptoms of emergency patients, and ordered with the time sequence of a patient’s diagnosis and treatment. This fully simulated the actual situation of an emergency doctor’s reception. Using chest pain as an example, if the patient with chest pains visits a doctor, the vital signs (temperature, pulse, respiration, blood pressure, SpO2, and consciousness) are assessed, and the ABCs (A = airway; B = breathing; C = circulation) are evaluated to identify abnormalities. If the ABCs are abnormal, they enter the rescue process. If there is no abnormality, they will enter the hierarchical diagnosis process: confirm the authenticity of the chest pain, distinguish if the “chest pain” is high-risk or low-risk according to the symptoms, and screen according to the processes for high-risk and low-risk “chest pain.” According to the procedure stipulated in the case template and the principle of “de-escalation thinking,” the ST doctors would check the causes individually.
Case Report and Expert Comments
ST doctors performed a case report and raised one or two questions for interaction. The expert commented on the early assessment, symptomatic identification, diagnostic procedures, rescue measures, and communication with patients and summarized the thinking defects of any mistakes and the lessons in diagnosis and treatment.
Efficacy Evaluation Method
In the present study, case analysis tests were performed uniformly at the ST doctors’ admission and leaving dates. The types and difficulty of questions were similar between the two groups. In each test, the ST doctors did not write the name and source of the training but only wrote a number managed by the teaching director. At the time of departure, the teaching secretary distributed a self-designed and anonymous questionnaire to ST doctors, which covered “teaching satisfaction, evaluation of self-competence and evaluation of teaching methods”. Upon leaving the department, the secretarial questionnaire was issued by the teaching secretary to the ST doctors, which covered the “teaching satisfaction, self-assessment evaluation, and evaluation of teaching methods.” The case analysis test results at admission and departure, teaching satisfaction evaluation, self-evaluation, and teaching method evaluation results were compared between the two groups.
Statistical Analysis
Data were analyzed using statistical software SPSS 17.0. Measurement data were expressed as mean ± standard deviation, and count data were expressed in percentage (%). The normality of variables was tested using a W-test. The homogeneity of variance was tested using an F-test. The data were compared between the two groups using a t-test. Non-normally distributed means or normally distributed means with the heterogeneity of multiple samples were evaluated using a non-parametric test. Count data were evaluated using a chi-square test. P < 0.05 was considered statistically significant.
Results
Comparison of Teaching results Between the Two Groups
No one was excluded as per the exclusion criteria. There were forty in the observation group and forty in the control group. There was no difference in basic knowledge and cognitive ability between the two groups. The scores of case analysis and examinations in the observation group and control group at admission were 65.50 ± 7.19 and 66.80 ± 9.10, respectively, but the difference was not statistically significant (P > 0.05). The scores at departure were 88.10 ± 3.88 and 75.23 ± 7.19, respectively, and the difference was statistically significant (P < 0.05) (Table 1). The observation and control groups questionnaire results were as follows: in the observation and control groups, 95% and 90% of doctors were satisfied with the teaching, but the difference was not statistically significant (P > 0.05). The ability improvement rate of students in the two groups was 92.5% and 75%, respectively, and the difference was highly statistically significant (P < 0.001) (Table 2). The survey questionnaire on how to appraise this teaching method revealed the following: the awareness rate of “know how to study” and “know how to work in emergency” in the observation group was 90% and 90%, respectively, the rate of doctors that considered “missed diagnosis and misdiagnosis can be reduced” was 85%, and the rate of doctors that considered “help to learn in other departments in the future” was 80% (Table 3).
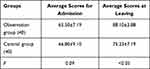 |
Table 1 Comparison of the Test Scores Between the Two Groups |
 |
Table 2 Results of Questionnaires on Teaching Satisfaction and Self-Assessment of Doctors in the Standardized Residents Training in Hospital |
 |
Table 3 Results of Questionnaires on Teaching Method Evaluation (Observation Group) |
Discussion
Emergency medicine has an extensive scope and is highly random and unpredictable Identifying and treating emergency and critical diseases is an essential part of in-hospital first aid and is the basic ability of each specialized clinician. After years of clinical practice, the results revealed that de-escalation is the core thinking of emergency situations. De-escalation thinking refers to a manner of thinking in which the differential diagnosis is carried out from severe disease to general disease and from rapid fatal disease to slow progressive disease. All patients should initially undergo the evaluation of “ABCs.” The process is selected according to the high-risk and low-risk symptomatology, and further diagnosis and differential diagnosis are made according to the list of the symptom’s causes. This deepens the understanding of emergency thinking and the process of ST doctors, preventing them from making mistakes in their initial decisions, which is conducive to the future work practice of different professional ST doctors. Experienced emergency doctors are still cautious, and new ST doctors feel more difficult to adapt to this. Determining how to enable ST doctors to adapt to emergency learning in a short time is worth exploring. The present study focused on training the emergency de-escalation thinking of ST doctors and used the template case report method to help them gradually master the core thinking of emergency treatment.
Surveys have revealed that there are still some limitations in the training of clinical thinking ability by teaching doctors, daily general rounds, standard diagnosis and treatment videos, clinical skills training, medical document writing, typical case analysis, and other teaching methods.9–13 In the present study, the ST doctors reported the cases according to the case template. It was used to record the initial judgment and treatment process of an emergency. The template is based on emergency experts’ experience in dealing with emergency problems, which is equivalent to ST doctors repeating the process of experienced doctors to help beginners grasp the thinking characteristics of an emergency quickly. In the case discussion, students asked questions, and experts interacted with them to solve problems, allowing the trainees to master the basic knowledge and theory of emergency treatment. This teaching model conforms to case teaching and problem-based teaching, which is welcomed by ST doctors. The present study results revealed that the difference in scores at admission between the observation and control groups was not statistically significant. However, the scores at departure were significantly higher in the observation group than in the control group, and the difference was statistically significant (Table 1). The survey revealed that the rate of doctors that considered “missed diagnosis and misdiagnosis can be reduced” was 85%, and the rate of doctors that considered “help to learn in other departments in the future” was 80% (Table 3).
Patients in any specialty are initially diagnosed based on symptoms rather than on disease. Previous clinical courses were disease-centered, and the order of learning was from disease, etiology, and pathophysiology to clinical manifestation, while the process of clinical practice is the opposite. Furthermore, medical students should re-evaluate and summarize the contents of the medical theory in the order of etiology-clinical manifestation-diagnosis and conversely use this in clinical practice. This kind of thinking mode and the complex types of acute diseases make it difficult for most doctors to construct urgent thinking. In 1988, the Cumming School of Medicine at the University of Calgary in Canada used a method to teach medicine and achieved good results. Similar subsequent reports have revealed high evaluation results.14 The present study started from the simulation of the actual reception situation, which was in line with the characteristics of “real combat” case discussions based on actual issues. The simulation of a real doctor’s reception was in line with the situational teaching mode, the real-world theory of patients, and the clinical practice of emergency diagnosis and treatment. The idea of differential diagnosis starting from symptomatology expands the lateral thinking of emergency treatment, thereby minimizing omissions.14 This may be one of the reasons why the students welcome it. Training ST doctors in clinical and emergency differentiation thinking based on symptom and differential diagnoses would be helpful for ST doctors not to panic and be in a hurry, and be busy but not messy when encountering emergencies, to avoid thinking loss, and improve their initial recognition and treatment ability in an emergency.15–18 In the present study, good teaching effects and practical values were also achieved through training. In the observation and control groups, 95% and 90% of the doctors were satisfied with the teaching, respectively, but the difference was not statistically significant. Furthermore, the ability improvement rate of students was 92.5% and 75%, respectively, and the difference was highly statistically significant (Table 2). Moreover, the awareness rate of “know how to study” and “know how to work in emergency” in the observation group was 90% and 90%, respectively (Table 3).
The biggest difference is in the real admission process template for reporting cases, not in the traditional way of reporting cases. In this way, by reporting cases, students will master the emergency admission process, keep a case report completely unified, report a case of not understanding disease, and understand and be familiar with the admissions process and way of thinking. The idea of symptoms as the breakthrough of disease diagnosis is not only practical in emergency clinical practice but also other specialties.
The present study still has the following limitations. First, although the teaching template completely simulated the clinical diagnosis and treatment process, the heavy workload of establishing standardized templates remains at a disadvantage. Second, although the test scores and the evaluation of all ST doctors were significantly higher at departure than at admission, it is difficult to eliminate some confounding factors in this study due to the complexity of medical education. For example, differences in residents’ cognitive abilities and skills can affect research results. Third, there was no comparison with other teaching methods. Hence, further comparative studies are needed.
Conclusion
Although most data are not significantly different between groups, we can still see a trend that the teaching method of a template case report based on the CTA integrates a variety of advanced teaching methods, allows for the training of emergency thinking of ST doctors, and helps improve their ability to analyze and solve problems in emergencies.
Funding
This study was supported by Medical Science Research Key Project Plan of Hebei Province in 2017 [No.20170273, 20170008], Medical Science Research Project Plan of Hebei Province in 2019 [No.20190202], and 2021 Traditional Chinese Medicine Research Project [No.2021160].
Disclosure
All of the authors had no any personal, financial, commercial, or academic conflicts of interest.
References
1. Bryan J, Rawi FA, Bhandari T, Chu J, Hansen S, Klaiman MZ. P026: need for training in medical education: staff emergency physician perspectives. CJEM. 2017;19(S1):S86.
2. King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas. 2006;18:391–397. doi:10.1111/j.1742-6723.2006.00872.x
3. Heidari M, Ebrahimi P. Examining the relationship between critical-thinking skills and decision-making ability of emergency medicine students. Indian J Crit Care Med. 2016;20:581–586. doi:10.4103/0972-5229.192045
4. Russ AL, Militello LG, Glassman PA, Arthur KJ, Zillich AJ, Weiner M. Adapting cognitive task analysis to investigate clinical decision making and medication safety incidents. J Patient Saf. 2019;15:191–197. doi:10.1097/PTS.0000000000000324
5. Chan TM, Van Dewark K, Sherbino J, Schwartz A, Norman G, Lineberry M. Failure to flow: an exploration of learning and teaching in busy, multi-patient environments using an interpretive description method. Perspect Med Educ. 2017;6(6):380–387. doi:10.1007/s40037-017-0384-7
6. Liu JH, Yu XZ, Guo SB, et al. [Emergency triage system design and implementation based on cognitive task analysis]. Chin J Crit Care Med. 2013;33:664–668. [Article in Chinese].
7. Ross JG, Beckmann B, Goumas C. Baccalaureate nursing students’ perceptions of the use of a facebook case study as a teaching strategy. Nurs Educ Perspect. 2019;40:174–175. doi:10.1097/01.NEP.0000000000000359
8. Kelly M, Feeley I, Boland F, O’Byrne JM. Undergraduate clinical teaching in orthopedic surgery: a randomized control trial comparing the effect of case-based teaching and bedside teaching on musculoskeletal OSCE performance. J Surg Educ. 2018;75:132–139. doi:10.1016/j.jsurg.2017.06.024
9. Krupat E, Sprague JM, Wolpaw D, Haidet P, Hatem D, O’Brien B. Thinking critically about critical thinking: ability, disposition or both? Med Educ. 2011;45:625–635. doi:10.1111/j.1365-2923.2010.03910.x
10. Eyre HA, Mitchell RD, Milford WJ. Growing the clinical academic workforce: the case for structured academic training programs for junior doctors. Med J Aust. 2014;200:389. doi:10.5694/mja13.00204
11. Beyeler C, Villiger PM, Tekian A. Postgraduate training program. Swiss Med Wkly. 2007;137:373–382.
12. Chang MJ, Chang YJ, Kuo SH, Yang YH, Chou FH. Relationships between critical thinking ability and nursing competence in clinical nurses. J Clin Nurs. 2011;20:3224–3232. doi:10.1111/j.1365-2702.2010.03593.x
13. Pavlish C. A model for situational patient teaching. J Contin Educ Nurs. 1987;18:163–167. doi:10.3928/0022-0124-19870901-07
14. Woloschuk W, Harasym P, Mandin H, Jones A. Use of scheme-based problem solving: an evaluation of the implementation and utilization of schemes in a clinical presentation curriculum. Med Educ. 2000;34:437–442. doi:10.1046/j.1365-2923.2000.00572.x
15. Whiting AS, Johnson LN. Papilledema: clinical clues and differential diagnosis. Am Fam Physician. 1992;45:1125–1134.
16. Martin BA, Peacock JG, Warner LL, et al. A novel metric and feedback template improves differential diagnosis formation capabilities in pre-clinical medical students. Med Sci Educ. 2014;24:189–194. doi:10.1007/s40670-014-0043-0
17. Smith EM, Anderson B. The effects of symptoms and delay in seeking diagnosis on stage of disease at diagnosis among women with cancers of the ovary. Cancer. 1985;56:2727–2732. doi:10.1002/1097-0142(19851201)56:11<2727::AID-CNCR2820561138>3.0.CO;2-8
18. Luo X, Chang Y, Yang J. An automatic disease diagnosis method based on big medical data.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
