Back to Journals » International Journal of General Medicine » Volume 10
Early in-hospital clinical deterioration is not predicted by severity of illness, functional status, or comorbidity
Authors Wang J, Hahn SS, Kline M , Cohen RI
Received 10 July 2017
Accepted for publication 22 August 2017
Published 29 September 2017 Volume 2017:10 Pages 329—334
DOI https://doi.org/10.2147/IJGM.S145933
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Janice Wang,1 Stella S Hahn,1 Myriam Kline,2 Rubin I Cohen1
1Division of Pulmonary, Critical Care and Sleep Medicine, Hofstra Northwell School of Medicine, New Hyde Park, 2Biostatistics Unit, Feinstein Institute for Medical Research, Northwell Health, Manhasset, NY, USA
Background: Prior studies concentrated on unplanned intensive care unit (ICU) transfer to gauge deterioration occurring shortly following hospital admission. However, examining only ICU transfers is not ideal since patients could stabilize with treatment, refuse ICU admission, or not require ICU evaluation. To further explore etiologies of early clinical deterioration, we used rapid response team (RRT) activation within 48 hours of admission as an index of early clinical worsening.
Methods: A retrospective analysis of prospectively gathered admissions from the emergency department in an academic medical center was done. Data were reviewed independently by two physicians. We assessed severity of illness, functional status, comorbidity, the frequency of ICU and palliative care consultations, and changes in advance health care directives.
Results: Of 655 rapid responses (RRs) within the study period, 24.6% occurred within 48 hours of admission. Disease trajectory was the most frequent perceived reason for RRs (55.6% and 58.9%, reviewer 1 and 2, respectively) followed by medical error (15.6% and 15.2%). Acute physiology and chronic health evaluation II (APACHE-II) and modified early warning scores (MEWS) were higher at the time of RR compared to admission (p<0.0001). However, admission APACHE-II, MEWS, functional status, and comorbidity scores did not predict early RRs. One third of RRs resulted in ICU consultation and 95% were accepted. Palliative care consults were requested for 15%, the majority (65%) after RR and all resulting in advance directive change.
Conclusion: Disease trajectory accounted for most clinical deterioration and medical error contributed to 15%. Our data suggest that it is difficult to predict early clinical deterioration as none of the measured parameters were associated with RRT activation.
Keywords: clinical deterioration, rapid response team, hospital admission, triage, medical error, palliative care
Introduction
Clinical deterioration occurring shortly following hospital admission occurs frequently despite patients undergoing multiple evaluations by several health care professionals. Hypothetically, given the number of evaluations that a patient undergoes upon admission, clinical deterioration soon after hospitalization should hardly take place. Realistically, disease progression or response to treatment is not predictable. Even so, early deterioration could represent deficiencies in care and understanding the reasons for early deterioration could improve patient care. Accordingly, prior studies sought to clarify reasons for early clinical deterioration by assessing transfer to an intensive care unit (ICU), the so-called unplanned transfer.1–7 However, to improve care, it is important to fully understand any potentially preventable errors. Examining ICU transfers occurring soon after admission provides a glimpse of events occurring in the wards, as it ignores those who had a critical care consult but were denied ICU admission and those who deteriorated and improved following treatment. Indeed, in a previous study we prospectively assessed all ICU consults requested within 48 hours of admission to determine factors associated with early deterioration.8 However, our prior study, as well as those of others, cannot account for patients who experienced an adverse event and on whom an ICU consult was not requested. More importantly, prior studies did not evaluate early deterioration in the present-day context of the rapid response team (RRT).
Over the past decade, the RRT has become an integral component in many hospitals. This team is activated for multiple reasons, any of which may suggest clinical deterioration. The goal of the RRT is to stabilize the patient, avoid further deterioration, and, if need be, transfer the care to a more monitored setting such as an ICU. Indeed, RRTs have become such an integral aspect of inpatient care that their activation precedes ICU evaluation and transfer.9,10 Consequently, to better clarify reasons for early clinical deteriorations, we assessed all rapid responses (RRs) within 48 hours of hospital admission from the emergency department (ED). We determined the reasons for RRT activation and examined whether factors such as severity of illness, the number of comorbidities, or functional status could predict early deterioration and RRT activation. Finally, we assessed those transferred to an ICU following evaluation by a critical care team, the presence of advance directives, and the outcome of these patients.
Methods
We conducted this study in a 600-bed US-based academic tertiary hospital in the New York city metropolitan area. The hospital is neither a trauma nor burn center. It has medical intensive care units (MICUs), surgical intensive care units (SICUs), and coronary intensive care units. Since ours is a teaching medical center, all admit decisions are made by residents following review with an attending physician. ED physicians can admit directly to a medical service, but require a surgical consult prior to admitting to any of the surgical services. ED physicians also require critical care consultations if they believe that a patient should be admitted directly to any of the ICUs. Should the patient be denied admission by the critical care team, the patient will be admitted to the ward.
We examined all RTTs requested in the wards for patients admitted through the ED. The RRT comprises a senior medical resident, an ICU nurse, and a respiratory therapist, and is activated by any health care provider or family member. The RRT is independent from the ICU consultation service. Since we studied only those admitted by ED physicians to a ward service, be it a medical or surgical ward, we excluded patients who were transferred from another hospital and those who were admitted directly to an ICU from the ED. The project was approved by the North Shore-Long Island Jewish Institutional Review Board, which waived the need for informed consent because this project entailed only data extraction from charts. The study team was trained in maintaining privacy and confidentiality in research. Furthermore, no personal identifiable data were recorded or collected. Data were collected for 9 consecutive months.
We determined whether critical care and palliative care consultations followed RRs and whether advance directives were in place prior to or following the RR. We also determined whether residents or physician assistants (PA) provided care for the patients and whether the RRs occurred during the day (0700 to 1900 hours) or night (1900 to 0700 hours) nursing shifts. Severity of illness was assessed by the acute physiology and chronic health evaluation II (APACHE-II) score and the modified early warning score (MEWS), which has been useful in reducing in-hospital mortality and cardiac arrest.11–13 We determined whether there were differences in APACHE-II scores and MEWS at admission compared to RR time.
We used the modified Elixhauser score to determine whether the patient’s comorbidity burden was associated with early RRs. The modified Rankin scale (MRS) was used to assess patients’ prehospital functional status in terms of disability and dependence. MRS scores range from 0 to 5, with 0 indicating a fully functional person to 5 denoting severe disability.14–16
Two intensivists referred to as reviewer 1 and reviewer 2 conducted independent chart reviews of RRs occurring within 48 hours of hospital admission. Reviewers considered the following categories in determining the primary reason for RRT activations.
- Triage error – admitting a patient to the ward when in fact the ICU was more appropriate (eg, a hypotensive patient is admitted to the ward).
- Disease trajectory – clinical deterioration secondary to progression of the admitting diagnosis despite appropriate medical management (eg, a patient admitted for seizures who then develops status epilepticus while on treatment).
- Iatrogenic complication – adverse effect of a medical intervention (eg, a patient develops anaphylaxis to a drug that was not known to be an allergen).
- Medical error – error in diagnosis or disease management, including untimely or inadequately addressed abnormal laboratory values or vital signs resulting in clinical deterioration.
- Unrelated – an event unrelated to the admitting diagnosis (eg, a patient admitted for pneumonia has a mechanical fall).
Statistical analysis
Descriptive data are reported as mean ± standard deviation (SD) or median (q1, q3), as appropriate. Gwet’s AC1 was used to measure agreement between reviewers’ perceived reasons for RR calls. Associations between categorical variables were tested using Fisher’s exact test. In tables larger than 2 rows by 2 columns, the cell chi-square was used to identify cells with the largest contribution to the overall significant result. Multiple testing was adjusted with a Bonferroni correction. Differences between or among groups were compared using the two-sample Student’s t-test, the Mann–Whitney test, or Kruskall–Wallis test, as appropriate. The paired t-test, or the Wilcoxon signed rank test, as appropriate was used to determine change in scores from admission to post-admission. Spearman’s correlation was used to evaluate the relationship between continuous or ordinal data. Findings were considered significant if p<0.05. The data analysis for the bulk of this paper was generated using SAS/STAT version 9.4 (SAS Institute Inc, Cary, NC, USA); Gwet’s AC1 and the percentage agreement were calculated using AgreeStat version 2011.3 (Advanced Analytics, Gaithersburg, MD, USA).
Results
Characteristics of RRs
There were 13,325 admissions from the ED to the wards during the study period. The RRT was activated 655 times, with 24.6% (161) occurring within 48 hours of admission. Patients’ age was 64±20 years and 65% were female. Twenty percent (33/161) of RRs occurred within 12 hours following admission, 29.8% (48/161) occurred between 12 and 24 hours, and 49.7% (80/161) occurred between 24:01 and 48 hours following ward admission. Fifty-five percent (88/161) of RRs occurred during the day shift.
Figure 1 illustrates causes for RRT activation. The three most frequent medical reasons were neurologic instability 45.3% (73/161), hemodynamic or cardiac instability 23% (37/161), and respiratory instability 18.6% (30/161). Eighty-eight percent (142/161) of patients with RRs within 48 hours of admission were discharged from the hospital while 9% (15/161) expired. Of the 15 patients who expired, 12 had been admitted to the MICU, of whom five were intubated during the RR.
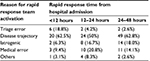
All charts were accessible to reviewers, except for one. The most frequent reason for early RR was disease trajectory (reviewer 1: 56% [89/160]; reviewer 2: 58% [93/160]) followed by medical error (reviewer 1: 16% [25/160]; reviewer 2: 15% [24/160]). An iatrogenic complication accounted for 11% (18/160) and 15% (24/160) of early RRs as determined by reviewer 1 and reviewer 2, respectively. Triage error was perceived to account for only 5% (8/160) by reviewer 1 and 6% (10/160) by reviewer 2. Triage error was responsible for only 5% of RRs and was associated with RRs occurring <12 hours from admission (p=0.05) (Table 1). There was substantial agreement between both reviewers (inter-rater reliability coefficient 0.62).
Critical care consultations
Most patients (108/161 or 67%) remained in the ward. Slightly over a third of RRs (36% [59/161]) led to a critical care consultation. Most critical care consults were to the MICU 80% (47/59), 12% (7/59) to the CCU, and 8% (5/59) to the SICU. Most patients (95%) were accepted by a critical care unit, with 96% (45/47) admitted to the MICU, 80% (4/5) to the SICU, and 100% (7/7) to the CCU. Severity of illness and disability and Elixhauser scores for those admitted or rejected from an ICU are illustrated in Table 2.
We observed that most MICU consultations followed RRT activation. Indeed, of the patients accepted by an ICU, only 15% (9/59) were evaluated by the MICU prior to the RR and all had been denied admission on initial consultation. Of those that were admitted to the MICU (45 patients), 12 expired, including three who consented to do-not-resuscitate (“DNR”) following MICU transfer. Perceived reasons (ie, triage error, disease trajectory, iatrogenic, medical error) leading to RR were not associated with MICU acceptance or denial.
Multiple RRT activations
Three patients had multiple RRs within 48 hours of admission. A 68-year-old male admitted with gastrointestinal bleeding had three RRs for seizure and hypotension. Palliative care consultation followed the first RR; however, he remained “full code” and expired in the MICU. A 90-year-old male with congestive heart failure had two RRs for acute respiratory distress. MICU denied admission due to poor prognosis and the patient consented to “DNR” and comfort care after meeting with the palliative care team. A 96-year-old female who underwent hip fracture repair had an RR called for lethargy. A second RR was called for a hemoglobin of 4 g/dL due to a hematoma. She was transferred to the SICU and subsequently discharged from the hospital. Palliative care was not consulted.
Timing of RRT activation
Time of RR following hospital admission was associated with MICU acceptance or denial (p=0.04). MICU acceptance was higher in RRs occurring <12 hours from admission (24.4%) and between 24:01 and 48 hours (51.1%) compared to rejection in these two groups (14.3% and 14.3%, respectively). On the other hand, rejection (71.4%) was higher than acceptance (24.4%) for RRs occurring between 12 and 24 hours.
Palliative care
Palliative care consultations were requested in only 14% (22/161) of patients, the majority following RR (15/22) and all resulted in advance directive change from “full code” to “DNR”. Of the 15 patients who expired, six had their advance directives changed to “DNR”. Of the 6 patients with changes to “DNR” status, palliative care was consulted in only 2 cases before the RR. In the remaining four patients, palliative care consultation followed the RR.
Covering service
Residents and PAs cared for 63% and 37% of the patients, respectively. APACHE-II scores did not differ by covering service (p=0.07); 12.2 (SD 7.1) in resident-covered patients versus 10.2 (SD 4.9) in PA-covered patients. Covering service was not associated with any perceived reason for RR (eg, medical error) (reviewers 1 or 2; p=0.75 and 0.54, respectively) or medical reasons for RRT activation (eg, neurologic instability, respiratory emergency). Covering service was not associated with code status change (p=0.08). Full code to DNR status change was 4.1% under resident service and 12.5% under PA service; however, this was not significant.
Functional status
Patients’ functional status, as assessed by the MRS, was not different based on the time of early RR. Patients with RR <12 hours had a mean MRS of 2.3; between 12 and 24 hours, MRS of 1.9; and between 24:01 and 48 hours, MRS of 2.2. Moreover, functional status did not play a role in acceptance or denial to MICU.
Severity of illness
APACHE-II and MEWS scores increased at the time of RR when compared to hospital admission (p<0.0001). This indicates that patients had deteriorated. However, the APACHE-II score at RRT activation was associated with neither an increased likelihood of ICU consultation nor ICU acceptance. Similarly, MEWS was not associated with MICU acceptance or denial; MEWS scores for accepted and rejected patients were 5.1 and 4.3, respectively (p=0.56).
APACHE-II and MEWS scores at the time of admission did not differ with regard to RR timing (p=0.18 and 0.28, respectively). The APACHE-II and MEWS median scores were 10.5 and 2.0 for RRs occurring <12 hours since admission; 12.5 and 2.0 for RRs from 12 to 24 hours; and 10.0 and 1.0 for RRs between 24 and 48 hours.
Comorbidity
There were no associations between Elixhauser scores, an index of comorbidity burden, and the timing of RRs or MICU acceptance or rejection.
Discussion
Using RRT activation as an indicator of early clinical deterioration, we found that a quarter of all RRs occurred within 48 hours of hospital admission. Had we examined only ICU transfers, we would have missed most early deteriorations as 108/161 (67%) remained in the ward. RRT activation resulted in a critical care consult in 36% of patients, and the majority (95%) were accepted. Nevertheless, when we examine early RRT activation, we note that it occurred 161 times in over 13,000 admissions, or 1.2%.
The most commonly perceived reason for RRT activation, and hence clinical deterioration, was disease trajectory. Medical error and iatrogenic complication each accounted for ~15% of RRs, which represents an undeniable need for improvement. Triage error played a minor role in RRT activation and was mostly associated with RRs taking place within 12 hours of admission. This seems logical since a true triage error would become apparent earlier in the hospital course.
Our results demonstrate that it is difficult to determine a priori who is at higher risk for early clinical deterioration, since none of the scores we examined at the time of hospital admission, APACHE-II, MEWS, MRS, and Elixhauser, were associated with an increased likelihood for early RRT activation. Illness severity scores did indeed worsen at the time of the RRT activation when compared to those compiled at admission indicating that the patients’ clinical status had indeed deteriorated.
Our data show that only 15% of those admitted to an ICU had a critical care consult prior to RR, suggesting that for most patients, neither the ED physician nor the admitting team felt that an ICU consult was necessary. When we examined the data more closely, we found that ICU denial (71.4%) was significantly higher than acceptance (24.4%) only when the RR occurred between 12 and 24 hours of admission. The reasons for this are not entirely clear and it may be that medical management was already underway or the ICU consult was cautionary in nature. Additionally, due to the scarcity of critical care resources, the approach of initial denial of ICU admission followed by reevaluation of the patient’s condition after therapeutic measures is often practiced. For example, reassessing a hypotensive patient’s response to fluid administration or a hypercapnic patient’s response to noninvasive ventilation may lead to clinical improvement and subsequent ICU denial.
Palliative care consults were requested in 14% of all early RRs with the majority following the RR. Our data suggest that palliative care is underutilized in early hospitalization. All palliative care consultations requested following the RR resulted in a change of advance health care directives from full code to DNR status. This implies that some RRs could have been prevented had the goals of care been addressed earlier. Alternatively, an acute deterioration may compel patients and families to come to terms with the poor prognosis and become more accepting of comfort care measures.
Prior studies showed that the care delivered by mid-level practitioners was comparable to that provided by residents.17 Our data further reinforce these findings. The covering service did not play a role in either the activation of the RRT or the timing of the RR. Further, we found no difference in hospital course or change in advance health care directives when the patient was under resident or PA care.
This study does have limitations. It was a single-center study, thus limiting its generalizability to other medical centers. Moreover, we could not evaluate patients in real time and relied on documentation. Real-time evaluation would have been logistically very difficult, if not impossible. The retrospective study design may have shaped the conclusions of the two reviewers. Nevertheless, the strength and uniqueness of this study is that by evaluating RRT activation rather than unplanned ICU transfers, we fully captured and assessed early clinical deterioration following ward admission. Clearly, there could have been additional patients who received an ICU consultant and were either rejected or admitted and for whom RRT was not activated. However, in a previous study, we examined just this population and found similar results.8 Indeed, our purpose of examining RRT activation rather than ICU consults was to more adequately capture early deterioration. It is also possible that some patients had a change in code status to DNR, and as such the RRT was not activated. However, this in no way impacts our conclusion as DNR patients did not deteriorate per se. Finally, the possibility exists that as length of stay increases, the chance of an iatrogenic error also increases. Therefore, it can be argued that had we studied patients beyond 48 hours, iatrogenic error may have become prominent. However, the purpose of this study was to examine early worsening, and we found that iatrogenic error played a minor role in early deterioration.
We conclude that clinical deterioration occurring within 48 hours of hospitalization was mostly due to disease trajectory and may not be preventable since no factor could predict early clinical deterioration. Nonetheless, medical error was responsible for 15% of early RRT activation and presents an opportunity for improvement. Perhaps, it is this population that should be pursued to improve care. Finally, palliative care input is underutilized early in hospital admission.
Disclosure
The authors report no conflicts of interest in this work.
References
Bapoje SR, Gaudiani JL, Narayanan V, Albert RK. Unplanned transfers to a medical intensive care unit: causes and relationship to preventable errors in care. J Hosp Med. 2011;6(2):68–72. | ||
Delgado MK, Liu V, Pines JM, Kipnis P, Gardner MN, Escobar GJ. Risk factors for unplanned transfer to intensive care within 24 hours of admission from the emergency department in an integrated healthcare system. J Hosp Med. 2013;8(1):13–19. | ||
Escobar GJ, Greene JD, Gardner MN, Marelich GP, Quick B, Kipnis P. Intra-hospital transfers to a higher level of care: contribution to total hospital and intensive care unit (ICU) mortality and length of stay (LOS). J Hosp Med. 2011;6(2):74–80. | ||
Frost SA, Alexandrou E, Bogdanovski T, Salamonson Y, Parr MJ, Hillman KM. Unplanned admission to intensive care after emergency hospitalisation: risk factors and development of a nomogram for individualising risk. Resuscitation. 2009;80(2):224–230. | ||
Liu V, Kipnis P, Rizk NW, Escobar GJ. Adverse outcomes associated with delayed intensive care unit transfers in an integrated healthcare system. J Hosp Med. 2012;7(3):224–230. | ||
Dahn CM, Manasco AT, Breaud AH, et al. A critical analysis of unplanned intensive care unit transfer within 48 hours from ED admission as a quality measure. Am J Emerg Med. 2016;34(8):1505–1510. | ||
Keller AS, Kirkland LL, Rajasekaran SY, Cha S, Rady MY, Huddleston JM. Unplanned transfers to the intensive care unit: the role of the shock index. J Hosp Med. 2010;5(8):460–465. | ||
Cohen RI, Eichorn A, Motschwiller C, et al. Medical intensive care unit consults occurring within 48 hours of admission: a prospective study. J Crit Care. 2015;30(2):363–368. | ||
Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015;19:254. | ||
Solomon RS, Corwin GS, Barclay DC, Quddusi SF, Dannenberg MD. Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: a systematic review and meta-analysis. J Hosp Med. 2016;11(6):438–445. | ||
Alam N, Hobbelink EL, van Tienhoven AJ, van de Ven PM, Jansma EP, Nanayakkara PWB. The impact of the use of the early warning score (EWS) on patient outcomes: a systematic review. Resuscitation. 2014;85(5):587–594. | ||
Paterson R, MacLeod DC, Thetford D, et al. Prediction of in-hospital mortality and length of stay using an early warning scoring system: clinical audit. Clin Med. 2006;6(3):281–284. | ||
Moon A, Cosgrove JF, Lea D, Fairs A, Cressey DM. An eight year audit before and after the introduction of modified early warning score (MEWS) charts, of patients admitted to a tertiary referral intensive care unit after CPR. Resuscitation. 2011;82(2):150–154. | ||
van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–633. | ||
Cohen RI, Eichorn A, Silver A. Admission decisions to a medical intensive care unit are based on functional status rather than severity of illness. A single center experience. Minerva Anestesiol. 2012;78(11):1226–1233. | ||
de Haan R, Limburg M, Bossuyt P, van der Meulen J, Aaronson N. The clinical meaning of Rankin “handicap” grades after stroke. Stroke. 1995;26(11):2027–2030. | ||
Newhouse RP, Stanik-Hutt J, White KM, et al. Advanced practice nurse outcomes 1990–2008: a systematic review. Nurs Econ. 2011;29(5):230–250. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.