Back to Journals » Journal of Hepatocellular Carcinoma » Volume 8
Drug-Eluting Bead Transarterial Chemoembolization versus Conventional Transarterial Chemoembolization Both Combined Apatinib for Hepatocellular Carcinoma: A Retrospective, Propensity-Score Matched Study
Authors Ouyang T , Liu J, Shi C, Zhu L, Guo X
Received 10 September 2021
Accepted for publication 5 November 2021
Published 26 November 2021 Volume 2021:8 Pages 1459—1471
DOI https://doi.org/10.2147/JHC.S338309
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Imam Waked
This paper has been retracted.
Tao Ouyang,1,* Junxia Liu,2,* Chengyang Shi,3 Lisheng Zhu,4 Xiaopeng Guo1
1Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 2Cancer Medical Center, The Second Affiliated Hospital of Nanjing Medical University, Nanjing, People’s Republic of China; 3Department of Orthopaedics, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China; 4Cancer Center, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tao Ouyang
Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, People’s Republic of China, Tel +86 18720931226, Email [email protected]
Xiaopeng Guo
Department of Radiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, 430022, People’s Republic of China, +86 13667216827, Email [email protected]
Purpose: This study aims to compare the efficacy of drug-eluting bead transarterial chemoembolization (DEB-TACE) versus conventional TACE (cTACE), both combined with apatinib, and to establish predictive nomograms to support individualized survival prediction in hepatocellular carcinoma (HCC) patients.
Patients and Methods: This retrospective study assessed HCC patients from June 2015 to December 2019. Patients were classified as DEB-TACE plus apatinib (D-apatinib) and cTACE plus apatinib (c-apatinib). The endpoints were overall survival (OS) and progression-free survival (PFS). The nomograms were constructed, and the C-index, receiver operating characteristic (ROC) curve, and calibration curves were used to validate the nomograms. Propensity score matching (PSM) analysis was applied to reduce patient selection bias.
Results: A total of 174 patients were included. After PSM analysis, 58 pairs of patients were selected. Before PSM analysis, the median OS and PFS were 21.0 and 8.0 months in the D-apatinib group, respectively, which were better than the 18.0 and 5.0 months observed in the c-apatinib group (P < 0.05). The complete response (CR) rate and objective response rate (ORR) of the D-apatinib group were higher than those of the c-apatinib group. The C-index values of the nomograms in the D-apatinib group and the c-apatinib group were 0.826 and 0.802, and the area under the curve (AUC) values in the ROC curve were 0.934 and 0.892. After PSM analysis, the survival of patients treated with D-apatinib was better than that of patients treated with c-apatinib (P < 0.05). The C-index values were 0.854 and 0.794 in the D-apatinib group and the c-apatinib group, respectively, and the AUC values were 0.960 and 0.890. The incidence of adverse events was higher in the c-apatinib group.
Conclusion: DEB-TACE in combination with apatinib showed better treatment effectiveness for unresectable HCC. The nomograms can identify HCC patients who may benefit most from the treatment.
Keywords: hepatocellular carcinoma, DEB-TACE, cTACE, apatinib, nomogram, PSM
Introduction
Hepatocellular carcinoma (HCC) is one of the most common cancers and the fourth leading cause of cancer death worldwide, and over 300,000 people in China die each year of HCC.1,2 HCC lacks clinical symptoms in the early stages, and most patients are diagnosed in the intermediate and advanced stages.3 Transarterial chemoembolization (TACE) was the standard therapy for intermediate stage HCC based on the guidelines.4 For patients with advanced HCC, sorafenib and lenvatinib are recommended as first-line treatments.5 However, their application in advanced HCC has not achieved satisfactory long-term survival efficacy.
TACE could effectively inhibit tumor progression and prolong the survival time of patients.6 Conventional TACE (cTACE) consists of intra‐arterial infusion of an emulsion of lipiodol and chemotherapeutic drugs, followed by embolic materials to block the tumor blood vessels. Drug-eluting bead TACE (DEB-TACE) uses microspheres that load chemotherapy agents to deliver drugs and embolize vessels, which can not only provide a slow release of chemotherapeutic drugs in tumors but also embolize the tumor‐feeding vessels permanently. Several studies have suggested the favorable safety and tolerability profile of DEB-TACE.7–9 However, the hypoxic microenvironment induced by TACE can increase the risk of tumor angiogenesis and tumor recurrence or metastasis.10,11 The combination of TACE and systemic antiangiogenic drugs is considered an effective combination therapy to reduce tumor angiogenesis after TACE administration.
Apatinib, a novel antiangiogenic small molecule, has ten times the binding affinity of VEGFR-2 tyrosine kinase than sorafenib.12 The combination of TACE with apatinib has revealed superior efficacy over apatinib and TACE monotherapy in HCC.13–16 Moreover, compared with TACE combined with sorafenib, TACE with apatinib exhibited a comparable prognosis for advanced HCC.17,18 Compared with c-TACE plus apatinib, DEB-TACE plus apatinib may increase the intratumor drug concentration and result in more sustained drug release, resulting in a better treatment response and long-term survival. Few studies are currently reporting differences in the treatment of DEB-TACE and c-TACE combined with apatinib for HCC patients, and there is no research developing and validating the predictive model for these patients.
Thus, this research aims to compare the effectiveness and safety of DEB-TACE and cTACE combined with apatinib in unresectable HCC and establish predictive nomograms to support individualized survival prediction.
Patients and Methods
Study Design and Patient Selection
This was a retrospective study conducted in a single-center, approved by the Ethics Committee of Tongji Medical College, Huazhong University of Science and Technology, and in accordance with the Declaration of Helsinki. In this retrospective study, we included 174 eligible patients who received DEB-TACE or cTACE combined with apatinib as the first-line treatment of HCC between June 2015 and December 2019. Based on the disease and after discussion with the physician, all patients chose one of the treatments: DEB-TACE plus apatinib or cTACE plus apatinib.
The inclusion criteria for this study were as follows: (a) patients were over 18 years, (b) patients diagnosed with primary HCC according to guidelines of the European Association for the Study of Liver and the American Association for the Study of Liver Disease,19 (c) Eastern Cooperative Oncology Group (ECOG) performance score of 0 or 1, (d) Child-Pugh class A or B, and (e) patients with HCC in stage B or C according to the BCLC staging system. The exclusion criteria for this study were as follows: (a) patients who had received liver transplantation, (b) patients who had a history of other malignancies, (c) patients with severe liver failure, severe renal failure, and severe infection, (d) patients without complete clinical records before the end of follow-up, (e) patients who received both treatments of DEB-TACE plus apatinib and cTACE plus apatinib, and (f) patients with resectable HCC and those treated by local ablative therapy (thermal ablation).
Every patient signed a consent form before receiving treatment for the first time. Based on the disease and after discussion with the physician, all patients chose one of the treatments: DEB-TACE plus apatinib or cTACE plus apatinib.
DEB-TACE Operation
The DEB-TACE operation was conducted by three experienced interventional physicians. The beads used in the study were CalliSpheres® Beads (Jiangsu Hengrui Medicine Co. Ltd., Jiangsu Province, China) with diameters of 100–300 µm or 300–500 µm. Before the operation, the beads were loaded with 60–80 mg pirarubicin. The procedure was performed in the digital subtraction angiography (DSA) operating room. Under local anesthesia, transfemoral access was gained, and a catheter was advanced into the coeliac artery for hepatic angiography to detect the tumor-supplying vessels. The embolization was conducted with a coaxial superselective, a subsegmental technique using a 5F cobra, followed by the positioning of a 2.4F microcatheter (Merit Maestro, Merit Medical System, Inc., Utah, USA). Then, the DEBs were injected through the microcatheter. When the contrast agent stopped flowing, the embolism was over. Finally, angiography was performed again to detect whether there were remaining blushed tumors.
cTACE Operation
The cTACE procedure is similar to the DEB-TACE operation. After percutaneous femoral arterial puncture was conducted, the catheter was superselectively inserted into the blood supply artery of the tumor through the hepatic artery. Then, the chemotherapy drug solution (pirarubicin 60–80 mg) was mixed with lipiodol in equal proportions. The mixed drug was injected into the tumor blood vessel by a 2.4F microcatheter (Merit Maestro, Merit Medical System, Inc., Utah, USA). Subsequently, the tumor blood vessel was embolized with 300~700 μm absorbable gelatin sponge particles (Cook, USA). Finally, angiography was performed again to ensure complete embolization.
Apatinib Administration
Apatinib was administered orally within 5–7 days after every DEB-TACE or cTACE operation. Apatinib administration stopped before the day of every TACE operation. The starting dose per patient was 500 mg each day. The dose of apatinib was reduced to 250 mg/day, or apatinib was stopped, if severe adverse events occurred in patients. Until the toxicity was alleviated or eliminated, apatinib was given at 250 mg/day or 500 mg/day.
Follow Up and Treatment Assessment
Patients underwent follow up, and the treatment response was assessed by enhanced magnetic resonance imaging (MRI) or computed tomography (CT) every 1 to 3 months. The primary endpoint of this research was overall survival (OS), which was defined as the date from the first DEB-TACE or cTACE procedure until mortality or the last follow-up. The last follow-up date was December 31, 2020. Progression-free survival (PFS) was defined as the time from the date of the first DEB-TACE or cTACE procedure until the time of disease progression or death. The treatment response assessment was evaluated by experienced radiologists based on the modified response evaluation criteria in solid tumors (MRECIST), which include four treatment responses: complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD).20 The objective response rate (ORR) was defined as (CR+PR)/all patients, and the disease control rate (DCR) was defined as (CR+PR+SD)/all patients. Treatment toxicity was continuously assessed during the study and graded according to the National Cancer Institute Common Toxicity Criteria for Adverse Events version 4.0.
PSM Analysis
Patients with D-Apatinib were matched with c-Apatinib using PSM analysis to reduce patient selection bias. The baseline variables entered into the model included age, sex, ascites, tumor size, number of tumors, tumor location, PVTT, AFP, Child–Pugh class, BCLC stage, ALP, AST, bilirubin, hemoglobin, and platelets. PSM was performed at a 1:1 ratio, and the caliper width was 0.05.
Statistics Analysis
Categorical variables are shown as frequencies with percentages, and continuous variables are presented as the mean ± standard deviation (SD). The difference in variables between the two treatments was compared with the chi-squared test and the Mann–Whitney U-test. The comparison of OS and PFS was performed by the Kaplan–Meier method and analyzed by two-sided Log rank tests. Variables with a p value < 0.05 in the univariable Cox regression analysis were enrolled in the multivariable Cox regression analysis. The nomogram was established based on the results of multivariate analysis and by the rms package in R version 4.0.4. The performance of nomograms was quantified by the concordance index (C-index). The calibration curve was used to identify the differences between the nomogram-predicted risks and the observed risks estimated by the Kaplan–Meier method. In addition, the precision of the prognosis prediction was evaluated using the area under the receiver operating characteristic (ROC) curve (AUC). All statistical analyses were performed using SPSS software (SPSS version 25.0) and R software (version 4.0.4, http://www.r-project.org). A p value of < 0.05 was considered statistically significant.
Results
Baseline Characteristics
A total of 299 HCC patients received treatment with either D-apatinib or c-apatinib. In all, 125 patients were excluded from this study. Of the 174 patients included in the study, 82 patients underwent treatment with D-apatinib, and 92 patients underwent c-apatinib treatment. The flow chart of the patient selection process presented in Figure 1. Before the PSM analysis, there was an almost significant difference in tumor size and tumor location between the two groups (P = 0.172 and P = 0.057). After the PSM analysis, 58 pairs of patients were selected, and the baseline variables of tumor size and tumor location were balanced between the two groups (P = 0.444 and P = 0.575). Other detailed patient characteristics are presented in Table 1, and there were no significant differences in other variables between the two groups (all P > 0.05). Most patients received a dosage of apatinib of 500 mg/day, and the mean dosage was 393.3 ± 84.8 mg/day in the D-Apatinib group and 377.7 ± 101.2 mg/day in the c-Apatinib group.
 |
Table 1 Baseline Characteristics of Patients in Two Groups |
Treatment Outcome
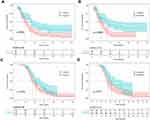
One month after treatment, the D-Apatinib group achieved a higher CR than the c-Apatinib group (32.9% versus 19.3%, P = 0.045), and the ORR was 76.8% in the D-Apatinib group, which was higher than the 62.0% observed in the c-Apatinib group (P = 0.034). After PSM, the CR and ORR were 36.2% and 81.0% in the D-Apatinib group and 19.0% and 60.3% in the c-Apatinib group, respectively (P = 0.038 and P = 0.014). In addition, the CR rate at three months was also higher in the D-Apatinib group than in the c-Apatinib group (before PSM, 28.0% versus 15.2%, P = 0.039; after PSM, 32.8% versus 15.5%, P = 0.030), while there was no significant difference in the ORR between the two groups (Table 2). At the cutoff date, the D-Apatinib group (median PFS: 8.0 months, 95% CI: 6.8–9.2 months) had a longer PFS than the c-Apatinib group (median PFS: 5.0 months, 95% CI: 3.8–6.2 months) (P < 0.001) (Figure 2A). After PSM, the median PFS was 8.0 months (95% CI: 6.1–9.9 months) in the D-Apatinib group, and 5.0 months (95% CI: 3.8–6.2 months) in the c-Apatinib group (Figure 2B). Similarly, D-Apatinib treatment (median OS: 21.0 months, 95% CI: 17.0–25.0 months) was associated with a prolonged OS compared with c-Apatinib treatment (median OS: 18.0 months, 95% CI: 15.7–20.3 months) (P = 0.024) (Figure 2C). After PSM, the median OS was 21.0 months (95% CI: 16.6–25.4 months) in the D-Apatinib group and 17.0 months (95% CI: 15.5–18.5 months) in the c-Apatinib group (Figure 2D).
 |
Table 2 Response Rates According to the Modified Response Evaluation Criteria in Solid Tumors at Different Times |
Independent Prognostic Factors
All significant factors associated with overall survival identified from the univariate analysis were included in the multivariate Cox analysis (Table 3). For the D-Apatinib group, before PSM, factors affecting OS included a BCLC of stage C (HR = 6.17, 95% CI: 2.45–15.56, P < 0.001), number of tumors of more than 3 (HR = 3.63, 95% CI: 1.75–7.52, P < 0.001), hemoglobin less than 130 g/L (HR = 2.49, 95% CI: 1.15–5.40, P = 0.021), and platelets less than 125 G/L (HR = 2.40, 95% CI: 1.24–4.67, P = 0.010) (Figure 3A). After PSM, the existence of more than 3 tumors (HR = 7.05, 95% CI: 2.42–20.56, P < 0.001), 130 g/L hemoglobin (HR = 9.03, 95% CI: 3.01–26.70, P < 0.001), and 125 G/L platelets (HR = 4.31, 95% CI: 1.71–10.87, P = 0.002) were predictive factors associated with OS (Figure 3B). In the c-Apatinib group, before PSM, a number of tumors greater than 3 (HR = 2.48, 95% CI: 1.35–4.56, P = 0.003), platelets less than 125 G/L (HR = 2.19, 95% CI: 1.18–4.04, P = 0.013), the presence of ascites (HR = 2.46, 95% CI: 1.40–4.34, P = 0.002), and an ALP level greater than 150 U/l (HR = 3.87, 95% CI: 2.27–6.62, P < 0.001) were independently associated with poor survival (Figure 3C). After PSM, more than 3 tumors (HR = 3.63, 95% CI: 1.78–7.43, P < 0.001), the presence of ascites (HR = 2.89, 95% CI: 1.45–5.78, P = 0.003), and an ALP level of more than 150 U/l (HR = 4.81, 95% CI: 2.29–10.09, P < 0.001) were independent predictive factors (Figure 3D).
 |
Table 3 Multivariable Analyses of Significant Prognostic Factors |
Prognostic Nomogram for Overall Survival
Independent prognostic factors based on multivariate analysis for the two groups were applied to establish predictive nomograms. For survival estimation of HCC after D-Apatinib treatment, BCLC stage (stage B or stage C), number of tumors (≥ 3 or < 3), hemoglobin level (≥ 130 g/L or < 130 g/L), and platelet level (≥ 125 G/L or < 125 G/L) were enrolled (Figure 4A). Moreover, the c-Apatinib predictive nomogram included ascites (present or absent), number of tumors (≥ 3 or < 3), ALP level (> 150 U/l or ≤ 150 U/l), and platelet level (≥ 125 G/L or < 125 G/L) (Figure 4B). After the PSM analysis, two prognostic nomograms of D-Apatinib group and c-Apatinib group were developed (Figure 4C and D). Before PSM, the C-index of the two nomograms for predicting overall survival was 0.826 (95% CI, 0.779–0.873) and 0.802 (95% CI, 0.767–0.837), respectively. After PSM, the C-index was 0.854 (95% CI, 0.815–0.863) and 0.794 (95% CI, 0.745–0.843). In addition, before and after the PSM analysis, the calibration curves showed good agreement between prediction and observation in the probability of 2-year survival (Figure 5A–D). The AUC values of the nomogram for 2-year OS were 0.934 and 0.892 in the D-Apatinib group and c-Apatinib group, respectively before PSM, and 0.960 and 0.890 after PSM (Figure 6A–D).
Comparison of Treatment-Related Adverse Events
All 174 patients enrolled in the safety analysis. Most toxicities were tolerable, and there were no treatment-related deaths in either group. The incidences of vomiting (27.2% versus 9.8%, P = 0.003), hyperbilirubinemia (59.8% versus 42.7%, P = 0.024), ALT increase (69.6% versus 54.9%, P = 0.046), and AST increase (76.1% versus 61.0%, P = 0.031) were higher in the c-Apatinib group than the D-Apatinib group for all-grade treatment-related adverse events (trAEs), while the incidence of other trAEs was not different between the two groups. The detailed results of the safety analysis are presented in Table 4.
 |
Table 4 Treatment-Related Adverse Events |
Discussion
This retrospective study found that DEB-TACE plus apatinib treatment seemed to elicit a better treatment response than c-TACE plus apatinib in HCC patients. In addition, the survival time of PFS and OS was longer in the D-Apatinib group than in the c-Apatinib group. Conversely, the incidence of adverse events was higher in the c-Apatinib group. Moreover, based on the evaluation of different survival risk factors for OS in the two groups, predictive nomograms were established to predict the individual outcomes accurately and may be helpful in selecting between DEB-TACE plus apatinib and c-TACE plus apatinib in the treatment of patients with HCC.
Considering some limitations of cTACE, such as the fluidity of lipiodol reducing the concentration of chemotherapeutic agents and leading to weakened antitumor efficacy, DEB-TACE was developed to address the disadvantages of cTACE in the past decade.21 DEB-TACE can not only locally release loaded drugs but can also effectively block the blood supply to tumor tissues, which allows it to retain higher drug concentrations at tumor lesions. Therefore, DEB-TACE can improve the therapeutic effect by increasing antitumor activity. Ping et al conducted a prospective cohort study, comparing the treatment efficacy of DEB-TACE and cTACE in Chinese HCC patients. The results suggested that compared with cTACE treatment, DEB-TACE treatment attained a higher ORR and longer long-term survival time.8 Nevertheless, regardless of cTACE or DEB-TACE treatment, permanent chemoembolization cannot destroy these tumor lesions, and the ischemic and hypoxic microenvironment caused by TACE easily motivates neovascularization in local tumors.
As a highly selective VEGFR-2 inhibitor, apatinib can restrain endothelial cell migration and proliferation, thus decreasing tumor microvascular density, and accelerating cell apoptosis.22 A Phase 2 randomized study revealed that apatinib monotherapy was effective as the initial-line treatment for advanced HCC.23 Another multicenter, randomized, Phase 3 study showed that apatinib as second-line or later therapy significantly improved OS in advanced HCC patients.24 In addition, previous studies also demonstrated that TACE combined with apatinib exhibited a better treatment response and survival profiles than TACE alone.13,15 Moreover, Hu et al performed an analysis to compare the efficacy and safety of DEB-TACE plus apatinib, cTACE plus apatinib, and apatinib alone in advanced intrahepatic cholangiocarcinoma (ICC) patients and found that DEB-TACE plus apatinib has superior therapeutic efficacy compared with the other two treatments.25 In our study, the median PFS and OS were 8.0 and 21.0 months in patients treated with DEB-TACE plus apatinib, respectively, which were longer than those in patients who received cTACE plus apatinib. A possible explanation may be that D-Apatinib increases the intratumor chemotherapeutic drug concentration, and has a more sustained drug release than c-Apatinib, thereby leading to a better treatment response and long-term survival. Furthermore, compared with cTACE plus apatinib by lipiodol embolism, a more durable ischemic and hypoxic tumor microenvironment formed by microsphere embolization of DEB-TACE plus apatinib could enhance the antitumor effect of apatinib, leading to prolonged survival of HCC patients.
As presented in our study, each treatment type had different prognostic factors, which were included in the predictive nomograms. Patients with stage C and multiple tumors have a shorter survival time, which may be due to the more highly aggressive tumors in these patients. In addition, patients with poor liver function and primary status have worse therapeutic effects and shorter survival times. The independent prognostic factors found in this study were similar to previous research conducted by Chen, who evaluated the therapeutic effectiveness between DEB-TACE and cTACE in HCC.26 In predictive analysis, the regression models and nomograms showed moderate accuracy in predicting D-Apatinib treatment and c-Apatinib treatment. The contributions of our study are that it provides an accurate and convenient method for predicting survival that applies to HCC patients who receive D-Apatinib or c-Apatinib treatment and may be helpful in selecting between the two treatments.
In terms of adverse events, the most frequent treatment-related adverse events were postembolization syndrome, including fever, abdominal pain, vomiting, and an increase in liver enzymes. For DEB-TACE plus treating HCC, one previous study showed that common apatinib-related adverse reactions consist of bone marrow suppression, fatigue, hypertension, hand-foot syndrome, proteinuria and diarrhea, and these adverse events are mild without toxicity-induced death occurring.27 In this study, the incidence of adverse events such as vomiting, hyperbilirubinemia, and elevated ALT and AST was higher in the c-Apatinib group than in the D-Apatinib group. The reason for this is that DEB-TACE has a better treatment effect, which can reduce the number of TACEs.
There are several significant limitations in our research. Although the PSM analysis was conducted, there is still the risk of selection bias as this research was a single-center retrospective study. In addition, the sample size of this study was relatively small, and hence additional large-scale multicenter prospective studies are required to validate the results.
In conclusion, DEB-TACE combined with apatinib has superior effectiveness and safety in the treatment of HCC. Predictive nomograms are helpful for identifying HCC patients who benefit most from combination treatment and for making decisions in clinical practice.
Data Sharing Statement
The datasets used in this study are available from the corresponding author on reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
All authors have no conflicts of interest.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. Xu X, Chen J, Wei Q, et al. Clinical practice guidelines on liver transplantation for hepatocellular carcinoma in China (2018 edition). Hepatobiliary Pancreat Dis Int. 2019;18(4):307–312. doi:10.1016/j.hbpd.2019.06.010
3. Meyer T, Palmer DH, Cheng AL, Hocke J, Loembe AB, Yen CJ. mRECIST to predict survival in advanced hepatocellular carcinoma: analysis of two randomised phase II trials comparing nintedanib vs sorafenib. Liver Int. 2017;37(7):1047–1055. doi:10.1111/liv.13359
4. Bruix J, Sherman M. American association for the study of liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–1022. doi:10.1002/hep.24199
5. European Association for the Study of the Liver. Electronic address eee, European Association for the Study of the L. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi:10.1016/j.jhep.2018.03.019
6. Zhang J, Li H, Gao D, et al. A prognosis and impact factor analysis of DC-CIK cell therapy for patients with hepatocellular carcinoma undergoing postoperative TACE. Cancer Biol Ther. 2018;19(6):475–483. doi:10.1080/15384047.2018.1433501
7. Albrecht KC, Aschenbach R, Diamantis I, Eckardt N, Teichgraber U. Response rate and safety in patients with hepatocellular carcinoma treated with transarterial chemoembolization using 40-microm doxorubicin-eluting microspheres. J Cancer Res Clin Oncol. 2021;147(1):23–32. doi:10.1007/s00432-020-03370-z
8. Wen P, Chen SD, Wang JR, Zeng YH. Comparison of treatment response and survival profiles between drug-eluting bead transarterial chemoembolization and conventional transarterial chemoembolization in Chinese hepatocellular carcinoma patients: a prospective cohort study. Oncol Res. 2019;27(5):583–592. doi:10.3727/096504018X15368325811545
9. Farid K, Elalfy H, Abo El-Khair SM, et al. Prognostic value of vascular endothelial growth factor in both conventional and drug eluting beads transarterial chemoembolization for treatment of unresectable hepatocellular carcinoma in HCV patients. Expert Rev Gastroenterol Hepatol. 2020;14(12):1203–1214. doi:10.1080/17474124.2020.1823215
10. Wang B, Xu H, Gao ZQ, Ning HF, Sun YQ, Cao GW. Increased expression of vascular endothelial growth factor in hepatocellular carcinoma after transcatheter arterial chemoembolization. Acta Radiologica. 2008;49(5):523–529. doi:10.1080/02841850801958890
11. Ma P, Chen J, Qu H, et al. Hypoxic targeting and activating TH-302 loaded transcatheter arterial embolization microsphere. Drug Deliv. 2020;27(1):1412–1424. doi:10.1080/10717544.2020.1831102
12. Tian S, Quan H, Xie C, et al. YN968D1 is a novel and selective inhibitor of vascular endothelial growth factor receptor-2 tyrosine kinase with potent activity in vitro and in vivo. Cancer Sci. 2011;102(7):1374–1380. doi:10.1111/j.1349-7006.2011.01939.x
13. Lu W, Jin XL, Yang C, et al. Comparison of efficacy between TACE combined with apatinib and TACE alone in the treatment of intermediate and advanced hepatocellular carcinoma: a single-center randomized controlled trial. Cancer Biol Ther. 2017;18(6):433–438. doi:10.1080/15384047.2017.1323589
14. Li Z, Chen Q, Zhang W, et al. Efficacy and safety of the arsenic trioxide/lipiodol emulsion in the transcatheter arterial chemoembolization combined with apatinib in the treatment of advanced hepatocellular carcinoma. Can J Gastroenterol Hepatol. 2021;2021:5565793. doi:10.1155/2021/5565793
15. Kan X, Liang B, Zhou G, et al. Transarterial chemoembolization combined with apatinib for advanced hepatocellular carcinoma: a propensity score matching analysis. Front Oncol. 2020;10:970. doi:10.3389/fonc.2020.00970
16. Gu H, Li J, You N, et al. Efficacy and safety of apatinib combined with transarterial chemoembolization (TACE) in treating patients with recurrent hepatocellular carcinoma. Ann Transl Med. 2020;8(24):1677. doi:10.21037/atm-20-7244
17. Qiu Z, Shen L, Jiang Y, et al. Transarterial chemoembolization (TACE) combined with apatinib versus TACE combined with sorafenib in advanced hepatocellular carcinoma patients: a multicenter retrospective study. Ann Transl Med. 2021;9(4):283. doi:10.21037/atm-20-5360
18. Cao Y, Sun T, Guo X, et al. Sorafenib versus apatinib both combined transarterial chemoembolization for hepatocellular carcinoma with portal vein tumor thrombosis: a comparative retrospective study. Front Oncol. 2021;11:673378. doi:10.3389/fonc.2021.673378
19. Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208–1236. doi:10.1002/hep.20933
20. Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60. doi:10.1055/s-0030-1247132
21. Golfieri R, Giampalma E, Renzulli M, et al. Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer. 2014;111(2):255–264. doi:10.1038/bjc.2014.199
22. Wang E, Xia D, Bai W, et al. Tumor hypervascularity and hand-foot-skin reaction predict better outcomes in combination treatment of TACE and Sorafenib for intermediate hepatocellular carcinoma. BMC Cancer. 2019;19(1):409. doi:10.1186/s12885-019-5570-z
23. Qin S. Apatinib in Chinese patients with advanced hepatocellular carcinoma: a phase II randomized, open-label trial. J Clin Oncol. 2014;32(15_suppl):4019. doi:10.1200/jco.2014.32.15_suppl.4019
24. Qin S, Li Q, Gu S, et al. Apatinib as second-line or later therapy in patients with advanced hepatocellular carcinoma (AHELP): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Gastroenterol Hepatol. 2021;6(7):559–568. doi:10.1016/S2468-1253(21)00109-6
25. Hu Y, Hao M, Chen Q, Chen Z, Lin H. Comparison of the efficacy and safety among apatinib plus drug-eluting bead transarterial chemoembolization (TACE), apatinib plus conventional TACE and apatinib alone in advanced intrahepatic cholangiocarcinoma. Am J Transl Res. 2020;12(10):6584–6598.
26. Chen C, Qiu H, Yao Y, et al. Comprehensive predictive factors for CalliSpheres® microspheres (CSM) drug-eluting bead-transarterial chemoembolization and conventional transarterial chemoembolization on treatment response and survival in hepatocellular carcinoma patients. Clin Res Hepatol Gastroenterol. 2021;45(2):101460. doi:10.1016/j.clinre.2020.05.008
27. Liu J, Xu J, Zhang W, et al. Safety and efficacy of drug-eluting bead transarterial chemoembolization combined with apatinib in patients with advanced hepatocellular carcinoma. Acad Radiol. 2020;27(5):704–709. doi:10.1016/j.acra.2019.07.003
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.