Back to Journals » Infection and Drug Resistance » Volume 16
Does the Microflora of Surgery Site Infection Change After Prophylactic Use of Vancomycin Powder in the Spine Surgery
Authors Hu W, Wang H , Wu X, Shi X, Ma H, Zhang K, Gao Y
Received 27 September 2022
Accepted for publication 22 December 2022
Published 5 January 2023 Volume 2023:16 Pages 105—113
DOI https://doi.org/10.2147/IDR.S390837
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Weiran Hu,1,2,* Hongqiang Wang,1,2,* Xiaonan Wu,1,3 Xinge Shi,1,2 Haohao Ma,1,2 Kai Zhang,1,2 Yanzheng Gao1,2
1Department of Spine and Spinal Cord Surgery, Henan Provincial People’s Hospital, Zhengzhou, People’s Republic of China; 2Department of Spine and Spinal Cord Surgery, People’s Hospital of Zhengzhou University, Zhengzhou, People’s Republic of China; 3Department of Spine and Spinal Cord Surgery, People’s Hospital of Henan University, Zhengzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanzheng Gao, Department of Spine and Spinal Cord Surgery, Henan Provincial People’s Hospital, No. 7, Wei Wu Road, Zhengzhou, 450003, People’s Republic of China, Email [email protected]
Study Design: Retrospective cohort study.
Objective: This study aimed to investigate the characteristics of microflora in patients with deep spinal surgical site infection (SSI) after prophylactic use of vancomycin powder (VP).
Methods: A retrospective analysis was performed on patients after spinal surgery. Patients were grouped according to whether VP use and only patients with deep SSI were included in this study. General information of the patients, the dose of vancomycin, bacterial culture results, drug sensitivity test results, and SSI treatment methods were recorded. The differences of microflora between the two groups were analyzed, and the sensitivity of bacteria in the +VP group to antibiotics was analyzed.
Results: The infection rate in the +VP group was 4.9% (56/1124) vs 6.3% (93/1476) in the No-VP group (P < 0.05). The proportion of Gram-positive bacteria (GPB) in the +VP SSIs was 55.4% vs.74.1% in the No-VP group (P < 0.05). The percentage of Gram-negative bacteria (GNB) in the +VP SSIs was 46.4% vs.30.1% in the No-VP group (P < 0.05). More dose of VP cannot decrease the SSI, but the proportion of GNB in VP > 1g SSIs was higher (59.0% vs 32.4%, P < 0.05). In the +VP SSIs, all of the GNB cultured were sensitive to meropenem, and linezolid covered most of the GPB cultured.
Conclusion: Local use of vancomycin powder can reduce the incidence of SSI, but this may lead to changes in the bacterial flora. Once the SSI occurs, the case of GNB infection may be increased. The more dose of VP cannot decrease SSI but may increase the rate of GNB in the +VP SSIs. Once infections still occur after VP use, antibiotics covering GNB may be added. These findings may help guide choice of empiric antibiotics while awaiting culture data.
Keywords: surgery site infection, microflora, spine, vancomycin
Introduction
Surgical site infection (SSI) is a serious complication of spinal surgery, which can lead to failure of internal fixation, spinal instability, neurological dysfunction, sepsis, death, and increased medical costs.1–3 Vancomycin is a glycopeptide antibiotic that acts mainly by destroying the cell walls of sensitive bacteria. Topical use of vancomycin powder in spinal surgery not only creates a higher drug concentration at the surgical site but also reduces drug diffusion in blood, so it has the dual advantages of improving antimicrobial efficiency and reducing the side effects.3 Many studies have shown that prophylactic use of vancomycin powder can effectively reduce the incidence of SSI.1,4–7
However, SSI still occurs after prophylactic use of vancomycin. Many studies reported that the SSI rate after VP use is 0.9–3.1%, which shows that VP dose did not completely eliminate SSI.4,5,7 Previous studies have shown that GPB are the main pathogenic bacteria, followed by GNB and anaerobes in SSIs,8 but all the studies of microflora were based on patients without VP use. Whether vancomycin alters the microflora of SSIs remains unknown.
Antibiotics are the mainstay treatment for deep site infections after spinal surgery. It is important to know the type of infection, and broad-spectrum antibiotics should be administered as soon as possible when SSI occurs.9,10 Whether the use of vancomycin powder causes changes in bacterioflora is still unknown, this will affect the treatment strategy for the secondary infection. Therefore, we retrospectively analyzed SSIs after topical use of VP. The change of microflora and treatment strategy of the secondary infections were analyzed, aiming to help guide the choice of empiric antibiotics while awaiting culture data and improve the antimicrobial prophylaxis strategies for SSI after topical use of VP.
Method
A retrospective analysis was performed on patients who underwent spinal surgery in our institution between January 2015 and December 2020. Patients with intraoperative local use of VP were included in the +VP group, and those without were included in the No-VP group. The patient consent to review their medical records was waived due to the retrospective nature of this study by the Institutional Review Board and the Ethics Committee of Henan Provincial People’s Hospital. We pledge to respect the privacy of all participants, and all data involved in this study were anonymous and kept in a confidential manner. The study was based on the Declaration of Helsinki, as revised in 1983.
Diagnostic Criteria for SSI
Only deep SSIs were included in this study. The diagnosis of SSI was based on standards set by the Center for Disease Control and Prevention.11 Which is at least one of the following conditions must be met: (1) abscess formation or outflow of pus from the deep site; (2) accompanied by fever (over 38°C), local pain, or tenderness; (3) intraoperative diagnosis or postoperative histopathological confirmation of debridement; (4) abscess at the depth of the surgery site demonstrated by imaging examination; (5) deep SSI diagnosed by the surgeon.
Inclusion Criteria
The inclusion criteria were as follows: (1) patients underwent spinal surgery, degenerative diseases, fractures, deformities, or tumors are all included; (2) complete treatment record which included whether vancomycin was prophylactic used intraoperatively, the dose of vancomycin and specific treatment methods when SSI occurred; (3) only primary surgery was included in this study.
Exclusion Criteria
The exclusion criteria were as follows: (1) superficial SSI; (2) spinal infections such as tuberculosis and fungal infections; (3) patients with immunodeficiency or taking immunosuppressive drugs; (3) allergy to cephalosporin antibiotics or vancomycin; (4) incomplete medical records; (5) non-acute infection cases which means SSI occurred over 3 months postoperatively.12
Prophylactic Antibiotic Use Protocol
All patients receive pre-operative washes with chlorhexidine. A routine prophylactic use of antibiotics was applied in both groups, including intravenous application of 1.5g cefuroxime 1 h before surgery, an additional group every 4h during surgery, and 1.5g Q8h within 24h after surgery. In the +VP group, VP was sprayed into the wound during the operation, and the powder was evenly distributed in the sub-fascia and outer fascia according to the types of the surgery and the judgment of the surgeon.
Observational Index
Demographic characteristics of the patients, the dose of topical vancomycin, the type of postoperative infection, bacterial culture results, drug sensitivity test results, and the treatment of SSI were recorded. The bacterial culture specimen included blood, wound secretions and specimen obtained during the surgery. The culture methods mainly included smear identification of common bacteria and fungi, culture, drug sensitivity tests and drug sensitivity tests of anaerobic and aerobic bacteria.
Statistical Analysis
SPSS17.0 statistical software was used for the analysis. Quantitative data are expressed as mean ± standard deviation (x ± s). t-test of independent samples was used for comparison between the VP and the No-VP groups. The qualitative data were compared by chi-square test. Multiple comparisons were performed using Bonferroni’s method on the basis of chi-square test. P < 0.05 were considered statistically significant.
Results
Local vancomycin powder was used in 1124 patients, SSI occurred in 56 patients, and the infection rate was 4.9%. A total of 1476 patients were included in the No-VP group, and 93 patients developed SSI, the infection rate was 6.3%. There was a significant difference in infection rates between the two groups (P < 0.05). There were 56 patients in the +VP group, including 24 males and 32 females, with an average age of 56.7 ± 14.2 years. Vancomycin powder was used during the operation, with an average dose of 1.7 ± 0.8g. There were 1476 patients in the No-VP group, 93 patients developed SSIs including 57 males and 36 females, with an average age of 64.9±10.3 years. We included date from fracture, degenerative disease, scoliosis and tumor cases, and there was no significant difference in the distribution of disease types between the two groups (P > 0.05). In the VP group, there were 1008 instrumented cases and 106 no-instrumented cases. In the No-VP group, there were 1334 instrumented cases and 142 no-instrumented cases. There was no significant difference in the two groups (Table 1).
 |
Table 1 General Conditions of Patients and Distribution of Infected Sites in 2 Groups |
In the +VP SSIs, there were 5 cases (8.1%) of cervical spine infection, 13 cases (23.2%) of thoracic spine infection, and 38 cases (67.9%) of lumbar spine infection. In the No-VP group, there were 12 (12.9%) cervical vertebra infections, 19 (20.4%) thoracic vertebrae infections, and 62 (66.7%) lumbar vertebrae infections. There was no statistical difference in the distribution of infection sites between the two groups (P > 0.05) (Table 1).
In the +VP group, the positive detection rate of bacteria was 80.4% (45/56) and 11 patients were cultured negative, which was diagnosed by the clinical diagnostic criteria. In the No-VP group, the positive detection rate of bacteria was 79.6% (74/93) and 19 patients were cultured negative. In the +VP group, 31 cases of GPB, 2.8% (31/1124) in total patients, 26 cases of GNB, 2.3% (26/1124) in total patients, 3 cases of fungi, and 8 cases of mixed infection with multiple bacteria were cultured. In the No-VP group, 69 cases of GPB, 4.7% (69/1476) in total patients, 28 cases of GNB, 1.9% (28/1476) in total patients, 1 case of fungus, and 10 cases of mixed bacterial infection were cultured, and the proportion of Gram-positive bacteria was 55.4% and 63.4% in the 2 groups (P < 0.05). Among all cases, the total rate of GPB infection is 2.8% in the +VP group and 4.7% in the No-VP group (P < 0.05), meanwhile the rate of GNB is 2.3% in the +VP group and 1.9% in the No-VP group (P > 0.05) (Table 2 and Figure 1).
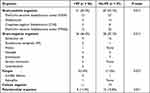 |
Table 2 Bacterial Culture Results of Wound Infections in 2 Groups |
When subgroup analysis was performed on SSI cases, the proportion of GPB in the +VP SSIs was 55.4% vs.74.1% in the No-VP group (P < 0.05). The GNB rate in the +VP SSIs was 46.4% and 30.1% in the No-VP (P < 0.05). The fungal proportion in the +VP SSIs was significantly higher than that in the No-VP group (5.4% vs.1.0%) (P < 0.05) (Table 2).
The sensitivity test results of GPB and GNB cultured in the +VP group were analyzed. The GNB cultured showed higher sensitivity to cefixime, ceftazidime and ceftriaxone, reaching 60% to 95%, and all of the cultured bacteria were sensitive to meropenem. The sensitivity of GPB cultured to vancomycin, teicoplanin and macrodantin as 80% to 90%, and linezolid has the highest sensitivity (Table 3).
 |
Table 3 Drug Sensitivity Test Results of Bacteria Cultured in the +VP Group |
Of the +VP SSIs, the treatment methods were analyzed, and the days between the debridement and first procedure were 13.4 ± 7.1 days. And 15 cases of fracture, 30 cases of degenerative disease, 6 cases of scoliosis and 5 cases of tumor were included. Among which including 6 cases of debridement, 32 cases of debridement and closed irrigation, 18 cases of debridement and vacuum sealing drainage (VSD). Whether a vacuum device was applied depends on the size of the wound, this was decided by the surgeon. The average number of procedures was 3.7 ± 2.1. Multiple comparisons were performed on the infection rate of different disease, and no significant difference was found (P > 0.05). But the infection rate in the scoliosis (7.7%) and tumor (10.2%) is higher than that in fracture (4.7%) and degenerative disease (4.4%) (Table 4).
 |
Table 4 Clinical Characteristics and Treatment Methods in the +VP SSIs |
Subgroup analysis was performed on VP dose, and patients were divided into VP ≤1g and VP >1g group. The amount of VP used in the two groups was 0.8 ± 0.4 and 1.6 ± 0.7g, respectively. There was no significant difference in the total infection rate between the two groups (P > 0.05), and no significant difference in the GPB infection in VP ≤1g and VP >1g SSIs and fungal infection in VP ≤1g and VP >1g SSIs (P > 0.05), but the proportion of GNB in VP >1g SSIs was higher than that in VP ≤1g SSIs (59.0% vs 32.4%, P < 0.05) (Table 5 and Figure 2).
 |
Table 5 Distribution of Infected Rate in VP ≤1g and VP >1g Groups |
 |
Figure 2 The bacterial flora distribution between the VP≤1g and VP>1g SSIs. Abbreviations: VP, vancomycin powder; GPB, gram-positive bacteria; GNB, gram-negative bacteria. |
Discussion
Vancomycin reduces infection by increasing the local concentration of the drug and reducing the chance of bacterial biofilm production. Hovis et al2 created a rabbit surgical model with fixation of implants at a tibial surgical site seeded with MRSA. They found that VP could decrease the risk of infection and biofilm formation on the implants, and the vancomycin levels in serum were minimally increased at the same time. A total of 2600 patients were enrolled in this study, and postoperative infections were analyzed. Local use of vancomycin powder can reduce the incidence of SSI, but this may lead to changes in the bacterial flora. The case of GNB infection may be increased in the secondary SSIs. The more dose of VP cannot decrease SSI but may increase the rate of GNB in the +VP SSIs at the same time.
Many studies came to a conclusion that topical use of VP can effectively reduce SSI.4,5,13 Dodson et al4 conducted a systematic review and found that VP significantly reduced the relative risk of SSI (RR = 0.55, P < 0.0001). In this study, compared to the No-VP group, the SSI in the +VP group decreased from 6.3% to 4.9%. In the previous study, the SSI rate is 0.9–3.1%, the SSI rate in the +VP group in this study is higher than previous date, this may be due to the inclusion of scoliosis and tumor cases.
Many previous studies focused on the change of infections caused by Staphylococcus aureus after vancomycin use.1,14 In this study, we also found a decrease in Staphylococcus infections, which is 1.1% (13/1124) in the +VP group and 1.8% (27/1476) in the control. Besides, by analyzing the bacterial flora distribution, we found that the overall infection rate was reduced by reducing the rate of GPB infection (2.8% vs 4.7%, P < 0.05), while the rate of GNB infection did not change (2.3% vs 1.9%, P > 0.05), which means that the most important reason for the decrease of SSI is the decrease of GPB infections after topical use of VP.
Vancomycin is a glycopeptide antibiotic widely used for the treatment of infections caused by GPB but is inefficient against GNB.15 The cellular integrity and morphology of most GNB are maintained by peptidoglycan, which consists of glycan strands cross-linked by peptides, whose arrangement determines cell shape and prevents lysis due to turgor pressure.16 Vancomycin is inherently inactive toward GNB because of its inability to cross the outer membrane.17 However, the GNB rate of total patients was equal in the groups. But of the SSI cases, the GNB rate in the +VP group was 46.4% and 30.1% in the No-VP group (P < 0.05). Many studies conducted the same conclusion. Ghobrial et al18 compared the causative pathogens among the patients who developed SSI. They found that 31 of 51 (60.7%) vancomycin-treated SSI patients were positive for GNB, while only 12 of 57 patients were found to be positive for GNB in the control. Adogwa et al7 demonstrated that over half of the secondary SSIs after VP use were positive for GNB.
Since the rate of GPB infection decreases, the percentage of SSI caused by GNB would increase. At the same time, the flora disequilibrium may increase opportunistic infections. The changes in commensal communities alter the interaction between pathogens, enhancing not only the production of certain T cell subsets but also altering the cytokine expression in immune innate and adaptive cells.19 Scheithauer et al20 conducted that short-term vancomycin treatment increases the abundance of Gram-negative opportunistic pathogens and immunogenic bacterial components. Rosa et al19 indicate that the bacterial community found in vancomycin-induced dysbiosis increased opportunistic infections.
The effect of VP dose on SSI subgroup was analyzed. We found that VP dose did not affect the incidence of SSI, nor did it affect the rate of GPB and fungi in the SSI cases, but the GNB infection rate in SSI cases increased in the VP >1g group (59.0% vs 32.4%), which was consistent with the higher GNB infection rate in the +VP SSIs. Dodson et al4 conducted a systematic review, and they demonstrated that the more dose of VP cannot significantly reduce SSI but may inhibit bone remodeling. What is impressive is that the rate of GNB SSI in the VP >1g SSIs is higher than that in the VP ≤1g (59.0% vs 32.4%); this also confirms that vancomycin inhibits the growth of GPB, and the flora disequilibrium may increase opportunistic infections.
Linezolid is an anti-infective drug with GPB SSI after VP use. According to the experimental results, the sensitivity to linezolid was over 90%. Many previous studies have confirmed that linezolid is superior to vancomycin.15,21–24 Fernandes et al15 compared the efficacy of linezolid and vancomycin on MRSA burden and found that treatment with linezolid has a greater beneficial effect. Moreover, linezolid was found to be more effective in patients complicated with underlying diseases. Among diabetic patients with MRSA infection, linezolid is clinically more effective than vancomycin.25 The authors found that all of the GNB SSIs were sensitized to meropenem. Carbapenems have a wider antimicrobial spectrum and lower sensitization. Samuel et al26 studied the bioactivity of meropenem and meropenem was biologically active against S. aureus, P. aeruginosa, E. coli, and K. pneumoniae. In the treatment of polymicrobial SSIs, meropenem was found to be the most effective single agent (90–95%), and its efficacy was even improved by adding vancomycin (97–98%).27,28
It was also worth noting that the higher rate of GNB infections in the +VP SSIs, which means in high-risk patients antibiotics covering GNB should be considered in primary surgery. This will help reduce the incidence of SSI, either GPB infection or GNB infection. Salimi26 and Gande29 hold the same opinion, they conducted that the strategy of vancomycin use needs to be individualized and antibiotic use strategies for GNB need to be improved.
At the same time, our study has limitations. Firstly, this was a single-center retrospective study, the flora in different regions and different seasons have different manifestations and nasal swabs for bacterial culture did not apply before surgery which may influence the research results.30,31 Secondly, the effect of vancomycin can be influenced by many uncontrollable factors, although the two groups showed no difference in patient age, sex, and diagnosis, but the ambulatory status, bowel/bladder incontinence, chronic respiratory insufficiency nutritional issues which are confounding factors influencing experimental results.32,33 Finally, although the effect of vancomycin dosage on postoperative SSI was initially discussed in this paper, the method of surgery, operation timing, and the fixed segments would affect the results.34,35
Conclusion
Local use of vancomycin powder can reduce the incidence of SSI, but this may lead to changes in the bacterial flora. Once the SSI occurs, the cases of GNB infection may be increased. The more dose of VP cannot decrease SSI but may increase the rate of GNB in the +VP SSIs. Once infections still occur after topical use of VP, antibiotics covering GNB may be added. These findings may help guide the choice of empiric antibiotics while awaiting culture data.
Data Sharing Statement
All of the data are described in the manuscript. The datasets used and/or analyzed in the present study are available from the corresponding author upon reasonable request.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Henan Provincial Medical Science and Technology Tackling Program Joint Project (LHGJ20200047), the Henan Provincial Medical Science and Technology Tackling Program Provincial-Ministerial Co-construction Project (SB201901085), and the Henan Provincial Medical Science and Technology Tackling Program Provincial-Ministerial Co-construction Project (SBGJ2018076).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Horii C, Yamazaki T, Oka H, et al. Does intrawound vancomycin powder reduce surgical site infection after posterior instrumented spinal surgery? A propensity score-matched analysis. Spine J. 2018;18(12):2205–2212. doi:10.1016/j.spinee.2018.04.015
2. Hovis JP, Montalvo R, Marinos D, et al. Intraoperative vancomycin powder reduces Staphylococcus aureus surgical site infections and biofilm formation on fixation implants in a rabbit model. J Orthop Trauma. 2018;32(5):263–268. doi:10.1097/BOT.0000000000001136
3. Park HY, Hegde V, Zoller SD, et al. Progress not panacea: vancomycin powder efficacy and dose evaluated in an in vivo mouse model of spine implant infection. Spine J. 2020;20(6):973–980. doi:10.1016/j.spinee.2019.12.007
4. Dodson V, Majmundar N, Swantic V, Assina R. The effect of prophylactic vancomycin powder on infections following spinal surgeries: a systematic review. Neurosurg Focus. 2019;46(1):E11. doi:10.3171/2018.10.FOCUS18470
5. Sweet FA, Roh M, Sliva C. Intrawound application of vancomycin for prophylaxis in instrumented thoracolumbar fusions: efficacy, drug levels, and patient outcomes. Spine. 2011;36(24):2084–2088. doi:10.1097/BRS.0b013e3181ff2cb1
6. Van Hal M, Lee J, Laudermilch D, Nwasike C, Kang J. Vancomycin powder regimen for prevention of surgical site infection in complex spine surgeries. Clin Spine Surg. 2017;30(8):E1062–E1065. doi:10.1097/BSD.0000000000000516
7. Adogwa O, Elsamadicy AA, Sergesketter A, et al. Prophylactic use of intraoperative vancomycin powder and postoperative infection: an analysis of microbiological patterns in 1200 consecutive surgical cases. J Neurosurg Spine. 2017;27(3):328–334. doi:10.3171/2017.2.SPINE161310
8. Guzek A, Rybicki Z, Tomaszewski D. Changes in bacterial flora and antibiotic resistance in clinical samples isolated from patients hospitalized in the Military Institute of Medicine in Warsaw, Poland, between 2005–2012. Przegl Epidemiol. 2017;71(2):165–176.
9. Esposito S, Capuano A, Noviello S, et al. Modification of patients’ endogenous bacterial flora during hospitalization in a large teaching hospital in Naples. J Chemother. 2003;15(6):568–573. doi:10.1179/joc.2003.15.6.568
10. Sudduth JD, Moss JA, Spitler CA, et al. Open fractures: are we still treating the same types of infections? Surg Infect. 2020;21(9):766–772. doi:10.1089/sur.2019.140
11. Solomkin JS, Mazuski J, Blanchard JC, et al. Introduction to the Centers for Disease Control and Prevention and the Healthcare Infection Control Practices Advisory Committee Guideline for the prevention of surgical site infections. Surg Infect. 2017;18(4):385–393. doi:10.1089/sur.2017.075
12. Russo V, Leaptrot D, Otis M, Smith H, Hebden JN, Wright MO. Health care-associated infections studies project: an American Journal of Infection Control and National Healthcare Safety Network Data Quality Collaboration Case Study - chapter 9 surgical site infection event (SSI) case study. Am J Infect Control. 2022;50(7):799–800. doi:10.1016/j.ajic.2022.03.036
13. Khan NR, Thompson CJ, DeCuypere M, et al. A meta-analysis of spinal surgical site infection and vancomycin powder. J Neurosurg Spine. 2014;21(6):974–983. doi:10.3171/2014.8.SPINE1445
14. Garg S, Bloch N, Potter M, et al. Topical vancomycin in pediatric spine surgery does not reduce surgical site infection: a retrospective cohort study. Spine Deform. 2018;6(5):523–528. doi:10.1016/j.jspd.2018.01.010
15. Fernandes MM, Ivanova K, Hoyo J, Pérez-Rafael S, Francesko A, Tzanov T. Nanotransformation of vancomycin overcomes the intrinsic resistance of gram-negative bacteria. ACS Appl Mater Interfaces. 2017;9(17):15022–15030. doi:10.1021/acsami.7b00217
16. Turner RD, Hurd AF, Cadby A, Hobbs JK, Foster SJ. Cell wall elongation mode in Gram-negative bacteria is determined by peptidoglycan architecture. Nat Commun. 2013;4:1496. doi:10.1038/ncomms2503
17. Yarlagadda V, Manjunath GB, Sarkar P, et al. Glycopeptide antibiotic to overcome the intrinsic resistance of gram-negative bacteria. ACS Infect Dis. 2016;2(2):132–139. doi:10.1021/acsinfecdis.5b00114
18. Ghobrial GM, Thakkar V, Andrews E, et al. Intraoperative vancomycin use in spinal surgery: single institution experience and microbial trends. Spine. 2014;39(7):550–555. doi:10.1097/BRS.0000000000000241
19. Rosa CP, Pereira JA, Cristina de Melo Santos N, et al. Vancomycin-induced gut dysbiosis during Pseudomonas aeruginosa pulmonary infection in a mice model. J Leukoc Biol. 2020;107(1):95–104. doi:10.1002/JLB.4AB0919-432R
20. Scheithauer TPM, Bakker GJ, Winkelmeijer M, et al. Compensatory intestinal immunoglobulin response after vancomycin treatment in humans. Gut Microbes. 2021;13(1):1–14. doi:10.1080/19490976.2021.1875109
21. Karaman R, Jubeh B, Breijyeh Z. Resistance of gram-positive bacteria to current antibacterial agents and overcoming approaches. Molecules. 2020;25(12):2888. doi:10.3390/molecules25122888
22. Kaye KS, Devine ST, Ford KD, Anderson DJ. Surgical site infection prophylaxis strategies for cardiothoracic surgery: a decision-analytic model. Scand J Infect Dis. 2012;44(12):948–955. doi:10.3109/00365548.2012.700118
23. Yue J, Dong BR, Yang M, Chen X, Wu T, Liu GJ. Linezolid versus vancomycin for skin and soft tissue infections. Cochrane Database Syst Rev. 2016;(1):CD008056. doi:10.1002/14651858.CD008056.pub3
24. Li J, Zhao QH, Huang KC, et al. Linezolid vs. vancomycin in treatment of methicillin-resistant staphylococcus aureus infections: a meta-analysis. Eur Rev Med Pharmacol Sci. 2017;21(17):3974–3979.
25. Equils O, da Costa C, Wible M, Lipsky BA. The effect of diabetes mellitus on outcomes of patients with nosocomial pneumonia caused by methicillin-resistant Staphylococcus aureus: data from a prospective double-blind clinical trial comparing treatment with linezolid versus vancomycin. BMC Infect Dis. 2016;16(1):476. doi:10.1186/s12879-016-1779-5
26. Salimi S, Khayat Kashani HR, Azhari S, et al. Local vancomycin therapy to reduce surgical site infection in adult spine surgery: a randomized prospective study. Eur Spine J. 2022;31(2):454–460. doi:10.1007/s00586-021-07050-5
27. Dybowski BA, Zapała P, Bres-Niewada E, et al. Catheter-associated bacterial flora in patients with benign prostatic hyperplasia: shift in antimicrobial susceptibility pattern. BMC Infect Dis. 2018;18(1):590. doi:10.1186/s12879-018-3507-9
28. Shetty HS, Mallela AR, Shastry BA, Acharya V. Parietal bone osteomyelitis in melioidosis. BMJ Case Rep. 2015;2015:bcr2014208612. doi:10.1136/bcr-2014-208612
29. Gande A, Rosinski A, Cunningham T, Bhatia N, Lee YP. Selection pressures of vancomycin powder use in spine surgery: a meta-analysis. Spine J. 2019;19(6):1076–1084. doi:10.1016/j.spinee.2019.01.002
30. Aleissa S, Parsons D, Grant J, Harder J, Howard J. Deep wound infection following pediatric scoliosis surgery: incidence and analysis of risk factors. Can J Surg. 2011;54(4):263–269. doi:10.1503/cjs.008210
31. Cahill PJ, Warnick DE, Lee MJ, et al. Infection after spinal fusion for pediatric spinal deformity: thirty years of experience at a single institution. Spine. 2010;35(12):1211–1217. doi:10.1097/BRS.0b013e3181c212d1
32. Warner SJ, Uppstrom TJ, Miller AO, et al. Epidemiology of deep surgical site infections after pediatric spinal fusion surgery. Spine. 2017;42(3):E163–E168. doi:10.1097/BRS.0000000000001735
33. Maesani M, Doit C, Lorrot M, et al. Surgical site infections in pediatric spine surgery: comparative microbiology of patients with idiopathic and nonidiopathic etiologies of spine deformity. Pediatr Infect Dis J. 2016;35(1):66–70. doi:10.1097/INF.0000000000000925
34. Glotzbecker M, Troy M, Miller P, et al. Implementing a multidisciplinary clinical pathway can reduce the deep surgical site infection rate after posterior spinal fusion in high-risk patients. Spine Deform. 2019;7(1):33–39. doi:10.1016/j.jspd.2018.06.010
35. Vandenberg C, Niswander C, Carry P, et al. Compliance with a comprehensive antibiotic protocol improves infection incidence in pediatric spine surgery. J Pediatr Orthop. 2018;38(5):287–292. doi:10.1097/BPO.0000000000000812
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

