Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 15
Does Hepatitis C Virus Treatment by Directly Acting Antivirals Obligate Shifting Patients with Type 2 Diabetes from Oral Hypoglycemic Drugs to Insulin Therapy?
Authors Hagag RY, Selim AF, Darrag OM, Zied H, Aboelnasr MS
Received 25 December 2021
Accepted for publication 6 April 2022
Published 26 April 2022 Volume 2022:15 Pages 1261—1268
DOI https://doi.org/10.2147/DMSO.S354023
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Video abstract of "DAAs HCV treatment shift from hypoglycemic drugs to insulin therapy" [ID 354023].
Views: 147
Rasha Youssef Hagag,1,* Ahmed Fawzy Selim,1,* Omneya Mohamed Darrag,1 Hassan Zied,2 Mohamed Sabry Aboelnasr1
1Department of internal medicine, Faculty of medicine, Tanta University, Tanta, Egypt; 2Kafr-Elsheikh Liver Institute, Kafr-Elsheikh, Egypt
*These authors contributed equally to this work
Correspondence: Mohamed Sabry Aboelnasr, Elgeish Street, Aboelelasorour Building, Floor 6, Kafrelzayat, Gharbia Governorate, 31611, Egypt, Tel +20 1066276267, Email [email protected]; [email protected]
Purpose: The aim of the present work was to investigate whether hepatitis C virus treatment by directly acting antivirals obligate shifting patients with type 2 diabetes from oral hypoglycemic drugs to insulin therapy.
Methods: This was a prospective study including 92 treatment-naïve patients with chronic hepatitis C virus infection and type 2 diabetes who were eligible for treatment with directly acting antivirals (sofosbuvir + daclatasvir ± ribavirin). Patients in the study were divided into two groups; group 1 included 22 patients on insulin therapy and group 2 included 70 patients on oral antidiabetic medications. Patients were advised to keep on their anti-diabetic treatment.
Results: All our patients achieved sustained virologic response with significantly lower HbA1c 12 weeks after the end of therapy (p. values 0.001 for group 1 and group 2). There was no statistically significant difference in HbA1c level post-treatment between both groups (p. value 0.352).
Conclusion: Achievement of sustained virologic response using interferon free, directly acting antivirals-based regimen was associated with significantly lower HbA1c 12 weeks after the end of therapy. The type of treatment used for type 2 diabetes (oral drugs or insulin) did not affect improved glycemic control observed after achieving sustained virologic response.
Keywords: directly acting antivirals, hepatitis C virus, sustained virologic response, type 2 diabetes
Introduction
The prevalence of chronic hepatitis C virus (HCV) infection is higher in patients with type 2 diabetes mellitus (T2DM) compared to those without diabetes.1 On the other hand, T2DM is considered as one of the most common extrahepatic manifestations of chronic HCV infection;2 the prevalence of T2DM among patients with chronic HCV infection is 13%-33%. Strict control of blood glucose levels could improve survival in HCV patients.3
Chronic HCV infection is associated with increased insulin resistance (IR); a hallmark in pathogenesis of T2DM.2 Achievement of sustained virologic response (SVR) led to decreasing incidence and prevalence of T2DM during the interferon (IFN) era of HCV treatment.4 The new era of treatment of HCV infection depends on IFN-free regimens. Direct-acting antivirals (DAAs) target non-structural proteins of HCV resulting in arrest of viral replication5 with highly encouraging results.6 The impact of viral eradication on IR was observed even in patients without diabetes treated with DAAs.7 In chronic HCV patients with T2DM, DAAs therapy is associated with both better fasting blood glucose (FBG) and HbA1c controls.4
Both T2DM and HCV infection represent major health problem in Egypt. The international diabetes federation (IDF) listed Egypt among the world top 10 countries in the number of patients with diabetes.8 Regarding HCV prevalence, Egypt has been widely regarded as having an epidemic, with the highest recorded prevalence of HCV infection in the world with an overall anti-HCV antibody prevalence of 14.7%.9,10
Potential interactions could exist between DAAs and oral hypoglycemic medications11 and it is not known whether this interaction could affect glycemic control in patients with T2DM undergoing treatment with DAAs to a degree that necessitates shift to insulin therapy.
Methods
Patients
This was a prospective study included patients attending at outpatient clinic of Tanta University Hospitals in the period from April 2018 to April 2019. Out study included 100 patients with T2DM and chronic HCV infection who were eligible for treatment with DAAs. Eight patients did not attend at follow up; so finally a total of 92 patients were included. After careful analysis of clinical and laboratory parameters of our patients, they were prescribed IFN-free, DAAs-based regimen for HCV eradication. All our patients were advised to continue their regular anti-diabetic medications.
Inclusion Criteria
- Age between 18 and 75 years.
- Naïve patient of chronic HCV infection.
- Positive results for HCV RNA by polymerase chain reaction (PCR).
- T2DM: patients with known T2DM on oral drugs or on insulin.
- Thyroid stimulating hormone (TSH) levels within normal limit (0.5˗4.5 mIU/L).
Exclusion Criteria
- Co-infection with hepatitis B virus (HBV) or human immunodeficiency virus (HIV).
- Patients with other causes of liver disease (Hemochromatosis,
- Wilson’s disease, Budd Chiari, auto-immune hepatitis, drug related liver disease).
- Immunologically mediated diseases eg ulcerative colitis, crohn’s disease, idiopathic thrombocytopenic purpura, systemic lupus erythematosus.
- Patients with Child Pugh B or C.12
- Pregnancy.
- Active malignancy (hepatic or extrahepatic).
- Patients with recent ischemic cardiovascular events over the past 6 months.
- Lack of written informed consent.
- Patients with intravenous drug abuse or with unhealthy alcohol use (includes unhealthy alcohol consumption and risky drinking behaviors; the later term means drinking amounts of alcohol that exceed recommended limits without meeting diagnostic and statistical manual of mental Disorders (DSM-5) criteria for alcohol use disorder).13,14
- Estimated glomerular filtration rate (eGFR) below 30 mL/hour according to Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.15
- Patients on other medications known to have interactions with DAAs.
All Patients in the Study Were Subjected to the Following
- Thorough history taking and complete physical examination.
- Laboratory investigations:
- Fasting and postprandial glucose.
- Alanine amino transferase (ALT), aspartate amino transferase.(AST).
- Bilirubin.
- Serum albumin.
- Prothrombin time, activity and international normalized ratio.
- Serum creatinine and eGFR using CKD-EPI equation.15
- HbA1c.
- TSH
- Full blood count.
- Fib 4 index calculation.16
- PCR for HCV RNA:
RNA Isolation from Plasma
Automatic extraction of viral RNA was done according to the manufacturer’s protocol using the QIAamp1 Viral RNA Mini-Kit (cat#1048147, QIAGEN1, Qiagen, Hilden, Germany).
Detection of HCV-RNA in Plasma by Quantitative Real-Time PCR
Detection of HCV viral load in the plasma was performed with the Artus1HCV-RG RT-PCR Kit (cat no. 4518265, QIAGEN1, Qiagen) by standardized quantitative real-time PCR according to the manufacturer’s protocol, and amplification was done by the ABI 7500 Fast Real-Time PCR Thermal cycler (Applied Biosystems, Foster City, CA, USA). Negative and positive controls were obtained from healthy volunteers and HCVinfected patients, respectively.
Pelvic abdominal ultrasonography to assess liver (size, border, hepatic veins and echogenicity), spleen size, portal vein diameter and ascites.
HbA1c and PCR for HCV RNA were assessed 12 weeks after the end of treatment. This is to assess for SVR and because of the known hemolytic effect of ribavirin with possible impact on HbA1c.17
Statistical Analysis of Data
The data was collected, presented and statistically analyzed with the computer program SPSS version 19 (SPSS Inc., Chicago, IL, USA). For quantitative data, the Kolmogorov test for normality was performed. For normally distributed data, values were expressed as mean (±SD) and independent samples t test (t) was performed for comparison between two groups. For data that were not normally distributed median and interquartile range (IQR) (expressed as 25th-75th percentiles) were calculated and MannWhitney test (ZMW), and Spearman’s rank-order correlation were used. For qualitative data, Pearson’s Chi square (X2ChS) test was used to examine association between two variables. Significance was adopted at probability (p) value < 0.05 for interpretation of results of tests.18
Results
This study was a prospective study that included 92 patients with chronic HCV infection and T2DM, attending outpatient clinic at Tanta University Hospitals during the period from 1st of September 2017 to the end of August 2018. The patients were divided into 2 groups; group 1 including 22 patients on insulin therapy and group 2 including 70 patients on oral hypoglycemic drugs. Baseline clinical and demographic characteristics of both groups are shown in Table 1. Baseline laboratory characteristics of both groups are shown in Table 2. Half of our patients had liver cirrhosis assessed by pelviabdominal US (11/22 patients in group 1 and 35/70 patients in group 2). Fib4 index was not significantly different between both groups (p. value 0.470) at study beginning (Table 3).
 |
Table 1 Baseline Clinical and Demographic Characteristics of the Studied Groups |
 |
Table 2 Baseline Laboratory Characteristics of the Studied Groups |
 |
Table 3 Comparison of Liver Status (by Pelviabdominal US) and Fib4 Index Between Both Groups |
Patients were advised to continue their usual anti-diabetic medications. Types of anti-diabetic medications used in both groups are shown in Table 4. All our patients received DAAs-based regimen (sofosbuvir + daclatasvir ± ribavirin). All of them achieved SVR 12 weeks after the end of therapy. We found that HbA1c levels were significantly reduced in both groups at 12 weeks after the end of treatment (p. values 0.001 for group 1 and group 2), with no difference in HbA1c level post treatment between both groups (p. value 0.352) (Table 5).
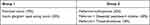 |
Table 4 Types of Anti-Diabetic Medications in Both Groups |
 |
Table 5 Comparison of HbA1c Before and After Treatment in Both Groups |
Discussion
A large number of studies reported an increased risk for T2DM in patients with chronic HCV infection. There was a higher prevalence of T2DM in those patients.19–21
Chronic HCV infection is associated with increased IR.2 A metaanalysis showed that patients with IR had lower rate of SVR. Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) was lower in patients who achieved SVR.22
We found that achievement of SVR, 12 weeks after end of therapy, is associated with improved glycemic control indicated by significant reduction of HbA1c 12 weeks post-treatment.
This positive impact of SVR on glycemic control was proved during the IFN era of HCV treatment.23–25 The use of DAAs therapy for treatment of patients with chronic HCV infection is now widely adopted, achieving SVR in nearly all patients.26 Our study showed that achievement of SVR was associated with improved glycemic control post-treatment with IFN-free, DAAs-based anti-HCV therapy; an effect that was independent on the type of treatment received for T2DM whether insulin or oral drugs. Butt et al found that DAAs-treated patients had longer diabetes-free survival rates, compared to untreated and PEG/RBV-treated persons; an effect that was more pronounced in persons with more advanced liver fibrosis. In that study, there was no significant difference in diabetes-free survival rates between untreated and PEG/RBV-treated persons.27
In our study, we used HbA1c as a marker for glycemic control. Some of the studies evaluated impact of SVR on glycemic control using HbA1c alone,28,29 others assessed both FBG and HbA1c,30–32 while some studies used FBG only.33 In many studies, improved glycemic control was also evident by a reduction in the use of anti-diabetic medications, significant reduction in the dose of insulin or the occurrence of hypoglycemic episodes in patients who achieved SVR.21,28,30,33–36 We did not record change in antidiabetic medications after treatment or the number of patients who had hypoglycemic episodes.
The impact of SVR on glycemic control was observed early during development of DAAs. An example was observed in 3a stage of chronic HCV, genotype 1, treated with 3D combo paritaprevir/ritonavir + dasabuvir + ombitasvir; where post hoc analysis of 6 studies showed a significant drop in FBG in the group of patients who received treatment compared to the group that received placebo.37 This effect was also evident in two Japanese studies on patients infected with genotype 1b on sofosbuvir and ledipasvir.28,29 Similar results were observed in studies involving the use of different DAAs regimens35,36,38 and also in patients who received DAAs after liver transplantation.39 Drazilova et al found that a significant decrease of fasting glycemia occurred in patients who achieved SVR after treatment with different DAAs-based regimens. In their study, 30 patients were on antidiabetic medication before the start of DAA therapy (13 were on oral antidiabetics, and 17 were on insulin). Three insulin treated patients needed to reduce insulin dose due to documented hypoglycemia.21
Data from studies on patients from other countries cannot be simply extrapolated to our population due to variation in social and environmental factors as well as difference in the prevalent HCV genotype. It is known that genotype 4 is the most common HCV genotype in Egypt representing 90% of infections.40
A study in Egypt that found a positive impact of SVR on IR manifested by a significant reduction of fasting insulin, and HOMA-IR. The study excluded patients with diabetes and included exclusively patients with genotype 4.33 Another study involved 460 Egyptian patients with chronic HCV infection who received sofosbuvir+daclatasvir ± ribavirin for 12 weeks showed that SVR was associated with better glycemic control indicated by a composite end-point given by the reduction of FBG (of a minimum of 20 mg/dL) or HbA1c (of a minimum of 0.5%), with the need to reduce the dose of anti-diabetic medications in 26% of patients who achieved a SVR.32 Similar findings were shown in another study that included 60 chronic HCV patients with diabetes, who received different sofosbuvir-based regimens (majority of patients had genotype 4).31
Our study showed that viral eradication was associated with improved glycemic control, however, few studies failed to show this correlation.41,42 Montenegro et al found an association between the presence of anti-HCV antibodies at baseline and a higher incidence of T2DM in the following 20 years only in patients with elevated ALT.43 A retrospective study concluded that the incidence of glucose abnormalities was not significantly different between patients with long-term SVR and those with persistently positive HCV- RNA.44 Another prospective study involving patients with genotype 1a/b failed to find a positive impact of SVR on HbA1c (31% of patients had HIV and 17% had T2DM). Patients were treated with different DAAs regimens (sofosbuvir, ledipasvir, beclabuvir, daclatasvir, and asunaprevir) and one patient was treated with IFN, ribavirin, and telaprevir. The result of that study should be taken cautiously because of low number of patients with T2DM comorbidity, and different DAAs regimens used.45
Whether to use insulin or oral drugs for treatment of T2DM in patients with chronic HCV infection remains a question for active research. Some oral drugs have beneficial effects in patients with liver disease independent on their impact on glycemia. For example, thiazolidinediones showed improvement in ALT and liver histology in patients with non-alcoholic fatty liver disease46 and IR;47 two major problems in patients with T2DM and chronic HCV infection. However this class is not recommended in patients with advanced liver cirrhosis.48
It is not known whether the type of antidiabetic medication could affect the improved glycemic control obtained after achievement of SVR in our patients. In our study, all patients were advised to continue their usual antidiabetic medications whether oral drugs or insulin. We found that the type of anti-diabetic medication did not affect SVR or improved glycemic control that occurred with achieving SVR. Abdel Alem et al showed that a decline in FBG occurred after SVR regardless of the treatment received in a group of 60 patients with T2DM and chronic HCV infection.31
In conclusion, we found that achievement of SVR in patients with T2DM and chronic HCV infection under treatment with DAAs was associated with significant reduction of HbA1c. This effect was observed whether patients were on oral drugs or on insulin; so no need to change anti-diabetic regimen in patients with T2DM and chronic HCV infection on starting treatment with DAAs.
There are several limitations to our study. First, we did not assess the impact of SVR on IR. Second, we did not include other factors that could have led to improvement of glycemic control eg diet, sport, and changing lifestyle. The study included one ethnic group in one treatment center. The length of the analysis was limited. A larger multicenter study is needed to confirm the results. This study should include other parameters that might be affected with SVR eg improvement in ALT, liver histology, cardiovascular risk, lipid profile and HOMA-IR. Long-term follow up of patients is recommended to evaluate long-term impact of SVR on parameters of glycemic control.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The present study was conducted in accordance with the Declaration of Helsinki. Permission obtained from Research Ethics Committee, faculty of medicine, Tanta University, Egypt (approval code: 17/07/31636). An informed written consent was obtained from all participants in this research. Privacy of all patients’ data was granted by a special code number for every patient’s file that includes all investigations. The results of the research were used only in scientific purposes and not in any other aims.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclosure
The authors declare that they have no conflicts of interest for this work. This work formed the base of an abstract introduced as an E-poster at Asian Pacific Digestive Week (APDW) held at Kolkata (in India) on December 2019.
References
1. Fabiani S, Fallahi P, Ferrari SM, et al. Hepatitis C virus infection and development of type 2 diabetes mellitus: systematic review and meta-analysis of the literature. Rev Endocr Metab Disord. 2018;19(4):405–420. doi:10.1007/s11154017-9440-1
2. Vanni E, Bugianesi E, Saracco G. Treatment of type 2 diabetes mellitus by viral eradication in chronic hepatitis C: myth or reality? Dig Liver Dis. 2016;48(2):105–111. doi:10.1016/j.dld.2015.10.016
3. Kwon S, Kim S, Kwon O, et al. Prognostic significance of glycaemic control in patients with HBV and HCV related cirrhosis and diabetes mellitus. Diabetic Med. 2005;22(11):1530–1535. doi:10.1111/j.14645491.2005.01687.x
4. Drazilova S, Gazda J, Janicko M, et al. Chronic hepatitis C association with diabetes mellitus and cardiovascular risk in the era of DAA therapy. Can J Gastroenterol Hepatol. 2018;(2018:11. doi:10.1155/2018/6150861
5. Schinazi R, Halfon P, Marcellin P, et al. HCV direct acting antiviral agents: the best interferon free combinations. Liver Int. 2014;34:69–78. doi:10.1111/liv.12423
6. Pawlotsky JM. New hepatitis C therapies: the toolbox, strategies, and challenges. Gastroenterology. 2014;146(5):1176–1192. doi:10.1053/j.gastro.2014.03.003
7. Gastaldi G, Gomes D, Schneiter P, et al. Treatment with direct-acting antivirals improves peripheral insulin sensitivity in non-diabetic, lean chronic hepatitis C patients. PLoS One. 2019;14(6):e0217751. doi:10.1371/journal.pone.0217751
8. Guariguata L, Whiting DR, Hambleton I, et al. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149. doi:10.1016/j.diabres.2013.11.002
9. El-Zanaty F, Way A. Egypt demographic and health survey (2008). Ministry of Health, El-Zanaty and Associates, and Macro International; 2009: 431.
10. Alter MJ. Epidemiology of hepatitis C virus infection. World J Gastroenterol. 2007;13(17):2436. doi:10.3748/wjg.v13.i17.2436
11. Sicras Mainar A, Navarro Artieda R, Hernández I, et al. Prevalence of the potential drug–drug interactions between pangenotypic direct-acting antivirals and the concomitant medications associated with patients with chronic hepatitis C virus infection in Spain. Gastroenterol Hepatol. 2019;42(8):465–475. doi:10.1016/j.gastre.2019.09.001
12. Durand F, Valla D. Assessment of prognosis of cirrhosis. Semin Liver Dis. 2008;28(1):110–122. doi:10.1055/s-2008-1040325
13. Pace CA, Uebelacker LA. Addressing unhealthy substance use in primary care. Med Clin. 2018;102(4):567–586. doi:10.1016/j.mcna.2018.02.004
14. Jonas DE, Garbutt JC. Screening and counseling for unhealthy alcohol use in primary care settings. Med Clin. 2017;101(4):823–837. doi:10.1016/j.mcna.2017.03.011
15. Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi:10.7326/0003-4819-150-9-200905050-00006
16. Sterling RK, Lissen E, Clumeck N, et al. Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology. 2006;43(6):1317–1325. doi:10.1002/hep.21178
17. Unnikrishnan R, Anjana RM, Mohan V. Drugs affecting HbA1c levels. Indian J Endocrinol Metab. 2012;16(4):528–531. doi:10.4103/22308210.98004
18. Dawson B, Trapp R. Basic and clinical biostatistics. In: Lange Medical Books.
19. White DL, Ratziu V, El-Serag HB. Hepatitis C infection and risk of diabetes: a systematic review and meta-analysis. J Hepatol. 2008;49(5):831–844. doi:10.1016/j.jhep.2008.08.006
20. Burman BE, Bacchetti P, Ayala CE, et al. Liver inflammation is a risk factor for prediabetes in at risk latinos with and without hepatitis C infection. Liver Int. 2015;35(1):101–107. doi:10.1111/liv.12676
21. Drazilova S, Janicko M, Skladany L, et al. Glucose metabolism changes in patients with chronic hepatitis C treated with direct acting antivirals. Can J Gastroenterol Hepatol. 2018;(2018:6095097. doi:10.1155/2018/6095097
22. Deltenre P, Louvet A, Lemoine M, et al. Impact of insulin resistance on sustained response in HCV patients treated with pegylated interferon and ribavirin: a meta-analysis. J Hepatol. 2011;55(6):1187–1194. doi:10.1016/j.jhep.2011.03.010
23. Qing S, Ji D, Li B, et al. Improvement of glucose and lipid metabolism with pegylated interferon-α plus ribavirin therapy in Chinese patients chronically infected with genotype 1b hepatitis C virus. Ann Saudi Med. 2015;35(4):293–297. doi:10.5144/0256-4947.2015.293
24. Romero-Gómez M, Fernández-Rodríguez CM, Andrade RJ, et al. Effect of sustained virological response to treatment on the incidence of abnormal glucose values in chronic hepatitis C. J Hepatol. 2008;48(5):721–727. doi:10.1016/j.jhep.2007.11.022
25. Arase Y, Suzuki F, Suzuki Y, et al. Sustained virological response reduces incidence of onset of type 2 diabetes in chronic hepatitis C. Hepatology. 2009;49(3):739–744. doi:10.1002/hep.22703
26. Marshall AD, Cunningham EB, Nielsen S, et al. Restrictions for reimbursement of interferon-free direct-acting antiviral drugs for HCV infection in Europe. Lancet Gastroenterol Hepatol. 2018;3(2):125–133. doi:10.1016/S24681253(17)30284-4
27. Butt AA, Yan P, Aslam S, et al. Hepatitis C Virus (HCV) treatment with directly acting agents reduces the risk of incident diabetes: results from electronically retrieved cohort of HCV infected veterans (ERCHIVES). Clin Infect Dis. 2019;70(6):1153–1160.
28. Ikeda A, Ikeda K, Takai A, et al. Hepatitis C treatment with sofosbuvir and ledipasvir accompanied by immediate improvement in hemoglobin A1c. Digestion. 2017;96(4):228–230. doi:10.1159/000484237
29. Meissner EG, Lee YJ, Osinusi A, et al. Effect of sofosbuvir and ribavirin treatment on peripheral and hepatic lipid metabolism in chronic hepatitis C virus, genotype 1–infected patients. Hepatology. 2015;61(3):790–801. doi:10.1002/hep.27424
30. Pavone P, Tieghi T, d’Ettorre G, et al. Rapid decline of fasting glucose in HCV diabetic patients treated with direct-acting antiviral agents. Clin Microbiol Infect. 2016;22(5):
31. Abdel Alem S, Elsharkawy A, Fouad R, et al. Improvement of glycemic state among responders to Sofosbuvir based treatment regimens: single center experience. J Med Virol. 2017;89(12):2181–2187. doi:10.1002/jmv.24897
32. Dawood AA, Nooh MZ, Elgamal AA. Factors associated with improved glycemic control by direct-acting antiviral agent treatment in Egyptian type 2 diabetes mellitus patients with chronic hepatitis C genotype 4. Diabetes Metab J. 2017;41(4):316–321. doi:10.4093/dmj.2017.41.4.316
33. El Sagheer G, Soliman E, Ahmad A, et al. Study of changes in lipid profile and insulin resistance in Egyptian patients with chronic hepatitis C genotype 4 in the era of DAAs. Libyan J Med. 2018;13(1):1435124. doi:10.1080/19932820.2018.1435124
34. Soriano V, Barreiro P, de Mendoza C. Hypoglycemia in a diabetic patient during hepatitis C therapy. Hepatology. 2016;63(6):2065–2066. doi:10.1002/hep.28137
35. Hum J, Jou JH, Green PK, et al. Improvement in glycemic control of type 2 diabetes after successful treatment of hepatitis C virus. Diabetes Care. 2017;40(9):1173–1180. doi:10.2337/dc17-0485
36. Ciancio A, Bosio R, Bo S, et al. Significant improvement of glycemic control in diabetic patients with HCV infection responding to direct acting antiviral agents. J Med Virol. 2018;90(2):320–327. doi:10.1002/jmv.24954
37. Tran T, Mehta D, Goldstein A, et al. Potential effect of hepatitis C treatment on renal, cardiovascular and metabolic extrahepatic manifestations: results from clinical trials of ombitasvir/paritaprevir/ritonavir and dasabuvir±ribavirin. J Hepatol. 2017;66(1):S302. doi:10.1016/S01688278(17)
38. Morales AL, Junga Z, Singla MB, et al. Hepatitis C eradication with sofosbuvir leads to significant metabolic changes. World J Hepatol. 2016;8(35):1557–1563. doi:10.4254/wjh.v8.i35.1557
39. Beig J, Orr D, Harrison B, et al. Hepatitis C virus eradication with new interferon free treatment improves metabolic profile in hepatitis C virus related liver transplant recipients. Liver Transpl. 2018;24(8):1031–1039. doi:10.1002/lt.25060
40. Blach S, Zeuzem S, Manns M, et al. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2(3):161–176. doi:10.1016/S24681253(16)
41. Svegliati-Baroni G, Bugianesi E, Bouserhal T, et al. Post-load insulin resistance is an independent predictor of hepatic fibrosis in virus C chronic hepatitis and in non-alcoholic fatty liver disease. Gut. 2007;56(9):1296–1301. doi:10.1136/gut.2006.107946
42. Elgouhari HM, Zein CO, Hanouneh I, et al. Diabetes mellitus is associated with impaired response to antiviral therapy in chronic hepatitis C infection. Dig Dis Sci. 2009;54(12):2699–2705. doi:10.1007/s10620-0080683-2
43. Montenegro L, De Michina A, Misciagna G, et al. Virus C hepatitis and type 2 diabetes: a cohort study in southern Italy. Am J Gastroenterol. 2013;108(7):1108. doi:10.1038/ajg.2013.90
44. Giordanino C, Bugianesi E, Smedile A, et al. Incidence of type 2 diabetes mellitus and glucose abnormalities in patients with chronic hepatitis c infection by response to treatment: results of a cohort study. Am J Gastroenterol. 2008;103(10):2481–2487. doi:10.1111/j.15720241.2008.02002.x
45. Chaudhury CS, Sheehan J, Chairez C, et al. No improvement in hemoglobin A1c following hepatitis C viral clearance in patients with and without HIV. J Infect Dis. 2017;217(1):47–50. doi:10.1093/infdis/jix517
46. Van Wagner LB, Rinella ME. The role of insulin-sensitizing agents in the treatment of nonalcoholic steatohepatitis. Ther Adv Gastrointest Endosc. 2011;4(4):249–263. doi:10.1177/1756283X11403809
47. Sumie S, Kawaguchi T, Kawaguchi A, et al. Effect of pioglitazone on outcome following curative treatment for hepatocellular carcinoma in patients with hepatitis C virus infection: a prospective study. Mol Clin Oncol. 2015;3(1):115–120. doi:10.3892/mco.2014.435
48. Bonkovsky HL, Azar R, Bird S, et al. Severe cholestatic hepatitis caused by thiazolidinediones: risks associated with substituting rosiglitazone for troglitazone. Dig Dis Sci. 2002;47(7):1632–1637. doi:10.1023/A:1015895925374
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
