Back to Journals » Advances in Medical Education and Practice » Volume 13
Doctors’ and Nurses’ Knowledge and Perceived Barriers Regarding Acute Oxygen Therapy in a Tertiary Care Hospital in Nigeria
Authors Desalu OO , Ojuawo OB , Adeoti AO , Oyedepo OO, Aladesanmi AO, Afolayan OJ, Ibraheem RM , Suleiman ZA , Opeyemi CM
Received 15 June 2022
Accepted for publication 16 November 2022
Published 19 December 2022 Volume 2022:13 Pages 1535—1545
DOI https://doi.org/10.2147/AMEP.S378533
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Olufemi O Desalu,1 Olutobi B Ojuawo,1 Adekunle O Adeoti,2 Olanrewaju O Oyedepo,3 Adeniyi O Aladesanmi,1 Oluwafemi J Afolayan,4 Rasheedah M Ibraheem,5 Zakari A Suleiman,3 Christopher Muyiwa Opeyemi1
1Department of Medicine, University of Ilorin Teaching Hospital, Ilorin, Nigeria; 2Department of Medicine, Ekiti State University Teaching Hospital, Ado Ekiti, Nigeria; 3Department of Anesthesiology, University of Ilorin, Ilorin, Nigeria; 4Department of Medicine, Goulburn Valley Health, Shepparton, Victoria, Australia; 5Department of Child Health, University of Ilorin Teaching Hospital, Ilorin, Nigeria
Correspondence: Olufemi O Desalu, Department of Medicine, University of Ilorin Teaching Hospital, Ilorin, Nigeria, Email [email protected]
Purpose: Oxygen may cause serious consequences when administered wrongly. This study aimed to assess doctors’ and nurses’ knowledge of acute oxygen therapy and perceived delivery barriers.
Participants and Methods: We conducted a cross sectional study among 202 healthcare providers (134 doctors and 68 nurses) in a Nigerian hospital. The validated Acute Oxygen Therapy Questionnaire (AOTQ), which consisted of 21 knowledge assessment questions, was self administered by participants. Provider’s knowledge was classified as good if the score was≥ 80% and poor if < 60%.
Results: Overall, 26.7% (37.3% doctors and 5.9% nurses) had good knowledge of acute oxygen therapy (AOT), 35.9% were aware, and 19.3% used the AOT guidelines. The commonest source of knowledge on oxygen therapy was medical /nursing school (75.2%). The participants’ mean knowledge score was 14.75 ± 2.83(possible score of 0– 21). Doctors in postgraduate (PG) training obtained the highest score (15.96± 2.48) among the participants (F=12.45, df=4, p< 0.001). Most doctors (62%) and 23.5% of nurses considered oxygen as a drug. More doctors (52.2%) than nurses (14.7%) believed that a doctor’s order was mandatory before oxygen administration, contrary to guidelines recommendations. Most nurses did not know that breathlessness does not always signify hypoxemia and that asymptomatic anemia was not an indication for oxygen. Concerning oxygen prescription, 39.7% of nurses and 64.2% of doctors knew that it should be prescribed to achieve a target saturation range rather than a fixed dose. In acute oxygen delivery in COPD, doctors and nurses exhibited poor knowledge of the appropriate device and flow rate. The reported barriers to oxygen delivery were: a shortage of oxygen supply, inadequate delivery devices, power outages and out of pocket costs.
Conclusion: A significant proportion of doctors and nurses had poor knowledge of acute oxygen therapy, poor awareness and infrequently used AOT guidelines, and reported pertinent delivery barriers that warrant educational and administrative interventions.
Keywords: healthcare professionals, knowledge, barriers, oxygen therapy, training needs
Introduction
Oxygen accounts for about 21% of atmospheric air and is required by human body cells for function and survival. Inadequate blood oxygen can result in cellular dysfunction, organ failure, and death.1 Oxygen is like any other medical drug administered by doctors, nurses, and other healthcare workers; it can reduce mortality when used appropriately. When administered wrongly, it may be harmful with severe consequences.2 Acute oxygen therapies are often instituted when there is hypoxemia or respiratory distress, suspicion of tissue hypoxia in conditions like severe anemia, severe sepsis, tissue poisoning, and shock. Too much oxygen was erroneously believed to have no untoward effect.3 However, recent clinical data from systematic reviews and randomized clinical trials on using acute oxygen therapy in patients with stroke and acute myocardial infarction have disapproved of this notion.4–6 Excessive oxygen administration can be harmful, especially in those pulmonary conditions associated with hypercapnic respiratory failure like COPD and pneumonitis from bleomycin or paraquat exposure.7 Inappropriate administration can also lead to increased length of hospital stay, higher admission rates to high dependency units, and an increased risk of death.8–10 Uncontrolled oxygen administration, mainly when delivered at high concentrations, can worsen hypercapnia, primarily caused by hypoxic vasoconstriction.11,12 As a result of these documented harmful effects, safety agencies and several international respiratory societies have advocated for titrated oxygen therapy in this vulnerable patient group.7,13–16 For safety reasons and accurate administration, the experts have opined that oxygen should be treated like any other prescription drug. The orders for therapy are included on a treatment (medication) chart. The prescription must include dose specification, delivery methods, therapy duration, monitoring, and a target arterial oxygen saturation range (SaO2)and discontinued when arterial oxygenation is adequate with the patient breathing room air (Pao2 >8 kPa, Sao2 > 90%.2,7,13–17 A previous study in Nigeria reported doctors’ and other healthcare workers’ prescription and administration of emergency oxygen as inappropriate and poor.18 A recent systematic review that explored international prescribing and delivery practices of oxygen therapy found no study in sub Saharan Africa.19 Therefore, the conclusions from the two previous studies informed the decision of the current research to ascertain healthcare providers’ knowledge of the use of supplemental oxygen. In addition, to identify specific knowledge gaps for educational needs. To the best of our knowledge, there is little information on doctors’ and nurses’ understanding of the optimal administration of oxygen in emergencies in low income countries (LMIC). The primary objective of this study was to determine the doctors’ and nurses’ overall knowledge of acute oxygen therapy. The secondary objective was to determine the perceived delivery barriers among health providers.
Methods
Study Setting and Design
This survey was a cross sectional study that involved 202 doctors and nurses working in a public tertiary hospital in the Middle Belt region in Nigeria.
Ethical Consideration
The institutional approval for the study was obtained from the ethics and research committee of the University of Ilorin Teaching Hospital (ERC Protocol No: PAN/2017/03/1649). Informed written consent was obtained from the doctors and nurses, and the data collected were analyzed anonymously. Our team developed and validated the acute oxygen therapy questionnaire (AOTQ).20 All methods were carried out following relevant guidelines and regulations, notably the Declaration of Helsinki.
Sample Size
The minimum sample size of 297 was obtained using the Raosoft online sample calculator,21 from a suitable population size of 1300 doctors and nurses, with a response distribution of 50%, a margin of error of 5%, and a standard deviation set at 1.96 for a 95% confidence interval. Considering the expected response rate based on previous studies, which was 90%,20 the adjusted sample was 335.
Sampling Design
We recruited our sample from doctors and nurses working in hospitals involved in the clinical management of patients. The random number function (RAND) in Microsoft Excel generated random numbers, and the participants were selected by simple random sampling.
Survey Instruments
The acute oxygen therapy questionnaire (AOTQ) was developed by a panel of pulmonologists, anesthesiologists, pediatricians, epidemiologists, and health educationists.21 It is a reliable and validated English language questionnaire to evaluate doctors’ and nurses’ knowledge of acute oxygen administration.21 The global content validity index (S-CVI) was 0.85. The test retest reliability statistics showed a kappa coefficient of 0.546–0.897 (P<0.001) and a percentage agreement of 80–98.3%, indicating high temporal stability in the target population. The AOTQ has a total of 37 questions in eight sections consisting of 21 on knowledge; three on awareness and three on sources of information about oxygen therapy, two on time of last prescription and administration of oxygen therapy) and eight on demographics and professional profiles. The final five-section of this questionnaire included the following: four questions on general knowledge of oxygen as a medical gas(Q17-Q20), five questions on recognition of hypoxemia and tissue hypoxia(Q21-Q25), four questions about indications for oxygen therapy(Q26-Q29) with response options consisting of “true”, or “false”. In addition, two other sections on oxygen prescription (Q30-Q33) and delivery practices (Q34-Q37) contain four multiple-choice questions with one correct item, respectively. The weight for a correctly answered option is 1 point, and a “missing option” is considered an incorrect answer and scored 0. An optional self-reported open-ended question asks participants to describe their experiences or feelings on the challenges of oxygen administration in the hospital ward and emergency room. Questions about demographic and professional characteristics (Q1-Q8), time of last prescription and administration of oxygen (Q9-Q10), and sources of information about oxygen therapy (Q11-Q13) had no assigned scores. Likewise, the questions about awareness and use of an oxygen therapy guideline (Q14-Q16) and the open-ended questions have no scores. Instead, the score assigned to each respondent depends on the number of correct responses provided in the scoring. The AOTQ and its scoring are available in the Supplementary Materials.
Measured Outcome
The outcome measured was 1) knowledge of acute oxygen therapy (AOT), 2) awareness of AOT guidelines, 3) self reported barriers to AOT, and 4) sources of AOT knowledge which were reported as a number, frequency, percentage, and mean score where appropriate. We calculated mean and percentage scores for total and individual domains measuring oxygen therapy and compared scores by professional characteristics. The knowledge score for the survey population for each question was calculated by dividing the total number of correct responses by the number of respondents who answered the particular question. Each respondent’s complete knowledge score was calculated by dividing the number of correct responses to the survey questions by the maximum possible score. The total knowledge score per respondent was classified based on the original Bloom’s cut-off points into poor (<60%), fair (60%-79%), and good (≥80%).22,23 We also analyzed answers in absolute numbers and percentages of correct responses to each question to determine what percentage of the population knows a specific question. This analysis is crucial because it provides a better understanding of the overall knowledge, which would not be apparent with the mean score without a more detailed breakup of the data.
Data Collection
Eligible participants were approached by the survey team and provided with the acute oxygen therapy questionnaire (AOTQ) containing the study information note. The inclusion criteria were doctors and nurses actively working in the hospital who agreed to participate by giving verbal and written consent. Consenting participants were requested to voluntarily self administer the hard copy of the questionnaire based on their perception of the topic, and the confidentiality of their responses was assured. Exclusion criteria included declining participation, previous participation in validating AOTQ or failing to return the questionnaire after two weeks.
Statistical Analysis
The data entry clerk performed data cleaning operations to guarantee integrity by deleting duplicates, correcting spelling and wrong codes, and deleting or completing fields not filled out. After cleaning the data, the IBM/SPSS statistical software version 22 (SPSS Inc., Chicago, IL, USA) was used to analyze the data. We excluded respondents whose questionnaires contained less than 70% of answers or missing professional data. Univariate and bivariate statistics were performed to compare categorical and continuous variables among doctors and nurses. When normally distributed, the data were presented as mean (SD) and median (interquartile range) for skewed data. The statistical significance level was set at a p-value < 0.05 and was considered statistically significant.
Operational Definition
A junior hierarchy was defined as any doctor below a consultant rank and nurses below the position of a matron or principal nursing superintendent.
Results
During the study period, 325 participants were approached to participate, of which 202 (134 doctors and 68 nurses) were recruited, giving a response rate of 62.5% (73% doctors and 62% nurses).Forty nine were excluded because of lack of consent,43 failed to return the questionnaire, and 35 had an incomplete demographic or professional profile. Most of the doctors and nurses excluded were specialist consultants and matrons.
The mean age of the study sample population was 35 ± 9 years, the median year of professional practice was 8(IQR 4–13, range 1–31), and 110 (55.5%) respondents were females. The general characteristics of the participants are presented in Table 1
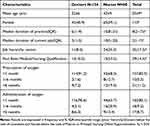 |
Table 1 General Characteristics of the Respondents |
Knowledge Level of Acute Oxygen Therapy
On classifying the total knowledge score of the entire study participants by the mean percentage score, 54 (26.7%) had good knowledge (score ≥80%), 41 (20.3%) had poor knowledge (score <60%), while the remaining 107(53.0%) had moderate knowledge of AOT. Figure 1 illustrates healthcare professionals’ knowledge level of acute oxygen therapy; 50 (37.3%) doctors had a good total knowledge score than four 4(5.9%) nurses.
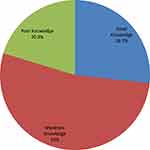 |
Figure 1 Knowledge of Acute Oxygen Therapy of respondents. |
Knowledge of Acute Oxygen Therapy by Professional Characteristics
The total knowledge of acute oxygen therapy by professional characteristics is expanded in Table 2. The mean knowledge score of the respondents in the study was 14.75±2.83 (possible score range 0–21), and the mean percentage score was 70.24%±13.48%. There was variation in overall mean scores for different categories of doctors and nurses (F=12.45, df=4, p<0.001), and mean scores for the domains assessing general knowledge of oxygen as a medical gas and recognition of hypoxeamia were significant (p<0.05). There were no significant differences in the mean scores for domains assessing the indications, prescription, and oxygen delivery. Generally, doctors significantly had a higher total knowledge score (15.60±2.61) than the nurses (13.07±2.48). Doctors in postgraduate training recorded a higher score (15.96±2.48) than the specialist consultant (15.55±3.17) and nurses with a bachelor’s degree (12.38±2.25).
 |
Table 2 Knowledge of Acute Oxygen Therapy by Professional Characteristics |
Similarly, junior doctors and nursing staff and those who have practiced <less than 10 ten years, respectively, had significantly higher scores than the senior doctors and nursing staff, and those who practiced more than 10 ten years p<0.05. Participants obtained a good knowledge score in domain testing for hypoxemia recognition (4.21±0.85), the maximum possible score of 5, and a poor score in the domain assessing for acute oxygen delivery(2.16±1.05) out of 4. The Specialist Consultants significantly had the highest score in general knowledge of oxygen as medical gas and recognition of hypoxemia, while the postgraduate trainee doctors led the score in the domain testing indication for oxygen therapy and oxygen prescription.
Responses to Questions Related to the Knowledge of Oxygen Therapy
To better understand the population’s knowledge, we analyzed the knowledge in terms of the absolute number and percentages of correct responses to a question. Almost 62%(83/134) of the doctors knew that oxygen was like any other medication/drug compared to 23.5%(16/68) among the nurses. This belief was corroborated by another question in which 91.2%(62/68) of nurses reported: “that oxygen is not a medication but a supportive therapy”. More than half of the doctors, 52.2%(70:134), said that oxygen could be given only after ‘doctors’ prescriptions, compared to 14.7%(10/68) among the nurses. Concerning hypoxemia recognition, 95.5% significantly knew that arterial blood gas analysis is useful for confirming hypoxemia compared to 69.1% of nurses. The majority (78.4%) of the doctors significantly knew that “breathlessness is not always a sign of hypoxemia”, which was higher than 38.2%(26/68) among the nurses. Regarding oxygen indications, most doctors, compared to nurses, significantly knew less that oxygen is indicated in Eclampsia (69.4% vs.82.4%).However, 82.8% of doctors, compared to 27.9% of nurses, significantly knew that asymptomatic anemia is not an indication for oxygen. Only 39.7% of the nurses knew that oxygen prescription should be to a target saturation range rather than a fixed dose, which is significantly less than 64.2% (86/134) among the doctors. In the oxygen delivery practice, both doctors and nurses exhibited poor knowledge concerning acute oxygen delivery of oxygen in COPD as only 44.0% (59/134) doctors and 32.4%(22/68) nurses, respectively, knew the appropriate device with the flow rate (Table 3).
 |
Table 3 Responses to Questions Related to the Knowledge of Oxygen Therapy |
Awareness and Use of Oxygen Therapy Guidelines
Out of 202 participants, 70(35.9%) were aware of either the British Thoracic Society (BTS) or the World Health Organization (WHO) guidelines on acute oxygen therapy, 43(22.8%) have read and been familiar with these guidelines, and only 39(19.3%) have used it to change their practice behavior (Table 4). The majority of the participants, 152 (75.2%), reported that medical/nursing school was the most common source of knowledge on oxygen therapy, followed by postgraduate training/ in-service training in 11 (23.4%),3(1.5%) mentioned internet websites and medical textbooks and journals respectively. Only 41(20.5%) have had professional education/CME on oxygen therapy.
 |
Table 4 Awareness and Use of Oxygen Therapy Guidelines |
Barriers to Oxygen Therapy
Overall, the shortage of oxygen supply, 106 (52.5%) was the most significant barrier to the acute administration of oxygen, followed by the shortage of delivery devices and systems reported by 19(9.4%) and 18(8.9%) cited patients out of the pocket cost of oxygen and 17(8.4%) reported electrical power failure (Figure 2).
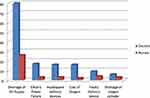 |
Figure 2 Heading: Doctors and Nurses reported barriers to acute oxygen therapy. |
Discussion
The main findings show that less than one third of participants had good knowledge of acute oxygen therapy (score ≥80%) and doctors significantly had a higher score than the nurses. Residents in PG training recorded higher scores than other categories of doctors and nurses. The main knowledge gaps were identified in the domain assessed for acute oxygen delivery, an essential aspect of oxygen therapy.
Our results show that less than one-third (26.7%) of the participants had good knowledge of acute oxygen therapy (AOT). This result is supported by other studies showing significant knowledge gaps among healthcare staff.24–28 These findings could affect the assessment and optimal delivery of oxygen and the outcome of acutely ill patients. The poor understanding of AOT in this study was because most doctors and nurses lack awareness of and familiarity with the available international AOT guidelines and perhaps the absence of a local protocol and national guideline for oxygen administration. Another explanation for the unsatisfactory performance was the lack of sufficient attendance for continuing professional development (CPD), as 20% of the participants in this study had attended training focused on acute oxygen therapy.
Notably, only 5% of nurses had a good knowledge of oxygen therapy, which is an abysmal performance. The observation is worrying, given the standard recommendation that nurses are required to know the indications and target oxygen saturation ranges based on various age groups and disease conditions.29
Doctors in PG training scored significantly higher than any other staff category. Considering that doctors in postgraduate training had the highest knowledge score, it is imperative to promote post-graduation or continuing professional development (CPD) training in healthcare facilities in the country. The importance of educating healthcare professionals on AOT cannot be overemphasized. A previous report by Considine et al revealed that specific education related to oxygen administration increases factual knowledge regarding the use of supplemental oxygen in emergency settings.30
Most (62%) doctors knew that oxygen was like any other medication, compared to 23.5% among nurses. This finding is comparable to a previous study among clinicians in Australia.29 However, the figure obtained for nurses was lower than 59% among Nepalese nurses.31 A significant proportion of doctors recorded a high score than the nurses in the domain of recognition of hypoxemia. For example, 78.4% of doctors and 38.2% of nurses knew that breathlessness might not signify hypoxemia, indicating the use of supplemental oxygen. These findings are of particular concern, considering how frequently nurses administer oxygen in an acute hospital setting. It implies that oxygen may be administered in the absence of hypoxemia. Like any other medication, oxygen may cause harm if the delivery is uncontrolled; as a result, there is a need for adequate oxygen therapy training for healthcare professionals.
More doctors (52.2%) than nurses (14.7%) reported that oxygen could only be given after doctors’ orders. In previous studies, roughly 60% of nurses knew oxygen could be administered without “a doctor”s prescription.31,32 The BTS oxygen guideline stated that in life threatening emergencies, oxygen should be administered first by staff (paramedics, nurses, doctors, physiotherapists, and others) trained in oxygen administration and the standard prescription documented later.7 In either local protocols or national guidelines, it is essential to emphasize that oxygen must be given to patients immediately without a formal prescription considering its role as a lifesaving therapy. The lack of a prescription should never preclude oxygen administration by other trained healthcare providers who are not doctors when needed in an emergency.
Remarkably, over 80% of participants recognized the usefulness of pulse oximetry in detecting and monitoring hypoxemia and cutoff SpO2-defining hypoxia. This result is higher than the reported figures in previous studies.26,31 A SpO2 <90% is the most clinically useful definition of hypoxemia, and most clinicians consider this an appropriate indication for giving oxygen. In some clinical situations, such as severe anemia, cardiac failure, and brain injury, providing oxygen to patients with SpO2of <94% is more appropriate. Specifying the cutoff needed to initiate oxygen therapy is essential because hypoxemia is a common complication in acute lower respiratory infection (ALRI) and a risk factor for death.17
Only 39.7% of the nurses knew that oxygen prescription should be to a target saturation range rather than a fixed dose, which was lower than 64.2% obtained among the doctors. This finding is perhaps not surprising as a previous audit of the pattern of acute oxygen therapy in our center found that 40.7% of acute oxygen administration shad a prescription to target oxygen saturation. Only 31.3% achieved their target saturation. This outcome is not satisfactory and contrasts with the recommendation of the oxygen therapy guidelines. Uncontrolled oxygen administration leads to supra-physiological oxygen levels, increased reactive oxygen species, tissue damage, vasoconstriction, and worse outcomes in myocardial infarction and stroke.2,7 High oxygen concentration can also mask a significant deterioration in the patient’s clinical condition, causing dangerous delays in treatment.7 These consequences informed several international oxygen guidelines recommendations of prescription to a target saturation range.13–17
Another significant finding from this study was in a vignette on acute oxygen delivery in COPD. We found that only 44.0% of doctors and 32.0% of nurses knew the appropriate device with the flow rate. This finding has important implications for the current practice of acute oxygen therapy. Inadequate oxygen can deprive the tissue and lead to more deaths and permanent disability.2 Too much oxygen, especially in type 2 respiratory failure, can cause life threatening hypercapnia, respiratory acidosis, organ dysfunction, coma, and death.13–17 To avoid these harmful effects, healthcare professionals should be highly knowledgeable in oxygen delivery and devices.
Irrespective of the healthcare professions, shortages of oxygen supply and delivery devices were the most significant barrier to the acute administration of oxygen. Previous publications in our setting have reported that available infrastructures for standard oxygen delivery systems were inadequate18,33 and that 78.2% of patients and 87.2% of caregivers considered oxygen therapy expensive and a possible barrier to treatment.34
We are baffled that none of the respondents mentioned poor knowledge as a barrier to oxygen delivery. It shows their lack of insight and awareness of the fundamentals of oxygen therapy.
Most respondents reported the medical/nursing school as the most common source of knowledge on oxygen therapy. We suggest that copies of the available oxygen therapy guidelines, such as the WHO or BTS, be sent to all hospital chief executives, medical directors, nursing heads, and all primary care and paramedics for better understanding.
Study Limitations
There were a few limitations associated with this study. Firstly, the study was conducted in a tertiary hospital, and the results may not be generalized to primary care settings. Secondly, outcomes were measured by self-report and may be subjected to bias. Despite these limitations, we used a validated instrument that is reliable.
Conclusion
A significant proportion of doctors and nurses had poor knowledge of acute oxygen therapy, poor awareness and infrequently used AOT guidelines and reported pertinent delivery barriers. This study has highlighted the knowledge gaps and perceived barriers regarding acute oxygen therapy. It underscores the need for tailored continuing professional development (CPD) and administrative interventions. Hospital clinical leads should widely disseminate available oxygen therapy guidelines or local protocols to improve awareness and familiarity. There is no national guideline for oxygen therapy in Nigeria; there is a need to develop local protocols and national guidelines or policies on oxygen therapy to improve knowledge and change our practice behavior.
Acknowledgments
The authors thank the doctors and nurses that participated in the study.
Funding
This research did not receive any specific funding from any authority or body.
Disclosure
The authors report no conflicts of interest in relation to this work and declare that there is no conflict of interest regarding the publication of this article.
References
1. American Thoracic Society (ATS). Oxygen Therapy. Clinical Resources. Available from: http://www.thoracic.org/clinical/index.php.
2. Bateman NT, Leach RM. ABC of oxygen: acute oxygen therapy. BMJ. 1998;317::798801.
3. Martin DS, Grocott MP III. Oxygen therapy in anaesthesia: the yin and yang of O2. Br J Anaesth. 2013;111(6):867–871.
4. Cabello JB, Burls A, Emparanza JI, Bayliss S, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. 2010;6:CD007160.
5. Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Weatherall M, Beasley R. Routine use of oxygen in the treatment of myocardial infarction: systematic review. Heart. 2009;95:198–202.
6. Ronning OM, Guldvog B. Should stroke victims routinely receive supplemental oxygen? A quasi-randomized controlled trial. Stroke. 1999;30:2033–2037.
7. O’Driscoll BR, Howard LS, Davison AG;;British Thoracic Society. BTS guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl 6):vi1e68.
8. Joosten SA, Koh MS, Bu X, Smallwood D, Irving LB. The effects of oxygen therapy in patients presenting to an emergency department with exacerbation of chronic obstructive pulmonary disease. Med J Aust. 2007;186(5):235–238.
9. Austin MA, Willis KE, Blizzard L, Walters EH, Wood-Baker R. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ. 2010;341:c5462.
10. Wijesinghe M, Perrin K, Healy B, et al. Pre-hospital oxygen therapy in acute exacerbations of chronic obstructive pulmonary disease. Intern Med J. 2011;41(8):618–622. doi:10.1111/j.1445-5994.2010.02207.x
11. Abdo WF, Heunks LMA. Oxygen-induced hypercapnia in COPD: myths and facts. Critical Care. 2012;16(5):4. doi:10.1186/cc11475
12. Aubier M, Murciano D, Milic-Emili J, Touaty E, Daghfous J, Pariente R. Effects of the Administration of O 2 on Ventilation and Blood Gases in Patients with Chronic Obstructive Pulmonary Disease During Acute Respiratory Failure 1– 3. American Review of Respiratory Disease. 1980;122(5):747–754. doi:10.1164/arrd.1980.122.5.747
13. Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, management, and Prevention of Chronic Obstructive Pulmonary Disease. Am J Respir. 2016;1:111.
14. Beasley R, Chien J, Douglas J, et al. <atl>T horacic S ociety of A ustralia and N ew Z ealand oxygen guidelines for acute oxygen use in adults: ‘Swimming between the flags’. Respirology. 2015;20(8):1182–1191. doi:10.1111/resp.12620
15. O’Driscoll BR, Howard L, Earis J, Mak V; BTS Emergency Oxygen Guideline Group. BTS Guidelines for oxygen use in adults in healthcare and emergency settings [Public consultation draft]; 2015. Available from: https://www.brit-thoracic.org.uk/document-library/clinical-information/oxygen/emergency-oxygen-guideline-2015/bts-full-guideline-for-oxygen-use-in-adults-in-healthcare-and-emergency-settings–2015/.
16. Lamont T, Luettel D, Scarpello J, O’Driscoll BR, Connew S. Improving the safety of oxygen therapy in hospitals: summary of a safety report from the National Patient Safety Agency. BMJ. 2010;340:313–314.
17. Trevor D. The Clinical Use of Oxygen in Hospitals with Limited Resources: Guidelines for Healthcare Workers, Hospital Engineers and Managers. World Health Organization; 2011.
18. Desalu OO, Oyedepo OO, Ojuawo OB, et al. Acute Oxygen Therapy on Hospital Wards in Low Middle-Income Country: experience from a Referral Centre in Ilorin, Nigeria. West Afr J Med. 2019;36(2):122–128.
19. Cousins J, Wark P, McDonald V. Acute oxygen therapy: a review of prescribing and delivery practices. Int J Chron Obstruct Pulmon Dis. 2016;11(1):1067–1075. doi:10.2147/COPD.S103607
20. Desalu OO, Aladesanmi AO, Ojuawo OB, et al. Oxygen Study Group. Development and validation of a questionnaire to assess the doctors’ and nurses’ knowledge of acute oxygen therapy. PLoS One. 2019;14(2):e0211198. doi:10.1371/journal.pone.0211198.
21. Raosoft Incorporation: raosoft Sample Size Online Calculator; 2004. Available from: http://www.raosoft.com/samplesize.html.
22. Bloom BS. Learning for mastery. instruction and curriculum. Regional education laboratory for the Carolinas and Virginia. Evaluation Comment. 1968;1(2):1–12.
23. Zakaria K, Chuemchit M. Knowledge, attitude and practice of psychological first aid among health professionals working in accident & emergency department in Brunei Darussalam. J Health Res. 2017;31(Suppl.1):S99–105. doi:10.14456/jhr.2017.72
24. Ganeshan A, Hon LQ, Soonawalla ZF. Oxygen: can we prescribe it correctly? Eur J Intern Med. 2006;17(5):355–359.
25. Smith GB, Poplett N. Knowledge of aspects of acute care in trainee doctors. Postgrad Med J. 2002;78(920):335–338.
26. Esposito S, Brivio A, Tagliabue C, et al. knowledge of oxygen administration, aerosol medicine, and chest physiotherapy among pediatric healthcare workers in Italy. J Aerosol Med Pulm Drug Deliv. 2011;24(3):149–156.
27. Eastwood GM, Reade MC, Peck L, Baldwin I, Considine J, Bellomo R. Critical care nurses’ opinion and self-reported practice of oxygen therapy: a survey. Aust Crit Care. 2012;25(1):23–30.
28. Cousins JL, Wark PAB, Hiles SA, McDonald VM. Understanding Clinicians’ Perceived Barriers and Facilitators to Optimal Use of Acute Oxygen Therapy in Adults. Int J Chron Obstruct Pulmon Dis. 2020;15:2275–2287. doi:10.2147/COPD.S263696
29. Kane B, Decalmer S, Ronan O’Driscoll B. Emergency oxygen therapy: from guideline to implementation. Breathe. 2013;9:246–253.
30. Considine J, Botti M, Thomas S. The effect of a self-directed learning package on emergency nurses’ knowledge of respiratory physiology, assessment of oxygenation and use of supplemental oxygen. Nurs Health Sci. 2005a;7:199–208.
31. Biryani RM, Ma PR, Suneel P, Shama P, Jasmine G, Pooja S. Knowledge of Staff Nurses about Oxygen Therapy Working in Intensive Care Areas of Universal College of Medical Sciences Teaching Hospital Bhairahawa, Nepal. EC Em Med Critical Care. 2020;1:1–10.
32. Mahmoud AO, Alseed HH, Awad HA, Ahmed AH, Elhussein GM. Assessment of knowledge and practice of nurses regarding oxygen therapy in Elmak Nimir University Hospital. Eur J Pharmaceutical Med Res. 2016;3(4):30–35.
33. Desalu OO, Onyedum CC, Iseh KR, Salawu FK, Salami AK. Asthma in Nigeria: are the facilities and resources available to support internationally endorsed standards of care? Health Policy. 2011;99(3):250–254.
34. Adeoti AO, Desalu OO, Elebiyo T, Aremu OA. Misconception on oxygen administration among patients and their caregivers in Ado Ekiti, Nigeria. Ann Afr Med. 2022;21:269–273.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
