Back to Journals » Infection and Drug Resistance » Volume 16
Distribution and Antibiotic Resistance Analysis of Blood Culture Pathogens in a Tertiary Care Hospital in China in the Past Four Years
Received 30 May 2023
Accepted for publication 10 August 2023
Published 22 August 2023 Volume 2023:16 Pages 5463—5471
DOI https://doi.org/10.2147/IDR.S423660
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Kun Li,* Long Li,* Jie Wang*
Department of Clinical Laboratory Medicine, Suining Central Hospital, Suining, Sichuan, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Kun Li, Department of Clinical Laboratory Medicine, Suining Central Hospital, Suining, Sichuan, 629000, People’s Republic of China, Tel +86-13698355569, Email [email protected]
Purpose: This study aimed to investigate the antibiotic resistance patterns and clinical distribution of blood culture-positive isolates at Suining Central Hospital between 2018 and 2021. The findings of this study can provide a basis for ensuring rational and effective use of antibiotic therapy in clinical settings.
Methods: This retrospective study analyzed the data of 3660 non-repeating strains that tested positive for clinical blood culture, collected from the microbiology laboratory of Suining Central Hospital between January 2018 and December 2021. The identification of bacterial species and their antibiotic resistance patterns were analyzed.
Results: The study found that 76.7% of the bacterial strains identified were Gram-negative bacteria, while 23.3% were Gram-positive bacteria. Escherichia coli (44.8%), Klebsiella spp. (19.2%), Staphylococcus aureus (9.2%), Enterococcus spp. (5.3%), and Enterobacter spp. were the top five bacterial ratios observed. These bacteria were detected most frequently in the Digestion Center, intensive care unit (ICU), Neurology Center, Urology Department, and Hematology Department. Among the Staphylococcus spp., methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-resistant coagulase-negative staphylococci (MRCNS) were detected at rates of 39.3% and 71.8%, respectively. However, no vancomycin- or linezolid-resistant staphylococci were identified. Enterococcus faecalis showed higher susceptibility to most antibiotic than Enterococcus faecium, except for tetracycline. The resistance rates of E. coli and Klebsiella spp. to meropenem and imipenem were low, but the resistance rates for other antibiotic were above 40%.
Conclusion: The results of this study show a rising incidence of bacterial antibiotic resistance in positive blood culture specimens at Suining Central Hospital. Clinicians should carefully consider the importance of blood culture antibiotic susceptibility testing to ensure effective treatment. The Department of Microbiology at Suining Central Hospital should regularly analyze the distribution of pathogenic bacteria and antibiotic resistance in blood cultures to ensure the most effective treatment possible.
Keywords: blood stream infection, antibiotic resistance, antibacterial drugs
Introduction
Bloodstream infection (BSI) is a serious and potentially life-threatening systemic infectious disease caused by pathogenic microorganisms invading the bloodstream and releasing toxins and metabolites that can lead to infection, poisoning, and a systemic inflammatory response.1 Although molecular approaches have been explored for pathogen diagnosis, blood culture (BC) remains the gold standard tool for identifying BSI and sepsis.2 It provides an accurate and reliable basis for clinical diagnosis and rational antibiotic administration.3 The pathogenic spectrum and pattern of antibiotic resistance of BSI vary among affected regions due to distinct epidemiological and geographic factors.4,5 Monitoring data from Dalian, China, from 2015 to 2019 showed that Gram-positive cocci were the most prevalent BSI pathogens in blood cultures.6 In contrast, antibiotic resistance surveillance data from Korea and Europe revealed that E. coli and S. aureus were the most common pathogens of, BSI.7,8 According to studies, incorrect empiric antibiotic therapy is an independent risk factor for increased mortality, particularly in individuals with S. aureus or Enterobacter spp. In addition relevant studies have shown that bloodstream infections are associated with various risk factors, such as advanced age, comorbidities, previous infections, neutropenia, long-term use of immunosuppressive medications, and the presence of indwelling venous catheters.9,10 Therefore, to provide clinicians with a reference for rational antibiotic use in treating BSI, this retrospective study aimed to examine the main pathogenic species and resistance patterns in blood cultures of inpatients at Suining Central Hospital between 2018 and 2021. In summary, bloodstream infection is severe, and blood culture remains the most reliable diagnostic tool. Antimicrobial resistance patterns vary across regions, highlighting the need for region-specific surveillance and treatment guidelines. This study investigates the pathogenic species and resistance patterns of BSI in Suining Central Hospital, aiming to guide the rational use of antibiotics in the treatment of BSI.
Materials and Methods
Data Collection
This retrospective study aimed to analyze blood cultures conducted between January 1, 2018, and December 31, 2021, at Suining Central Hospital in China. The dataset was obtained from the esteemed microbiology department, encompassing crucial information such as the date of blood culture, outcomes, AST results, patient demographics (age and sex), and the respective ward. To ensure the elimination of any potential bias arising from duplicate isolates, our analysis solely focused on the initial pathogen isolated from each patient and exclude positive outcomes from blood cultures containing single vials of coagulase-negative staphylococci and treating it as contamination.
Pathogen Identification and Antimicrobial Susceptibility Test
Blood samples were collected from patients using commercially available media bottles (bioMérieux, France) in accordance with established protocols. For adult patients, a combination of both aerobic and anaerobic bottles was utilized, whereas children were subjected to blood culture using exclusively aerobic bottles. The volumes of the blood samples collected were approximately 8–10 mL and 2–5 mL per bottle for adults and children, respectively. These samples were subsequently processed for blood culture analysis utilizing the BACT/ALERT 3D system (bioMérieux, France). The incubation cycle is five days. Positive blood samples were subjected to meticulous microscopic examination and subsequently subcultured on appropriate media. The suspected pathogens were then identified utilizing conventional biochemical tests, and an automatic identification instrument (Vitek-2 Compact system, bioMérieux, France). Ensuring accurate detection and characterization.11,12 Bacterial identification and antibiotic sensitivity identification were performed using a fully automated Vitek 2 compact. Instrument from Mérieux, France, with reagents for GN and GP identification cards matched with GN13 and GP67antimicrobial susceptibility testing cards, Antimicrobial drug susceptibility testing (AST) was conducted in accordance with the guidelines outlined by the Clinical and Laboratory Standards Institute (CLSI). The testing methods employed included the disk diffusion method, gradient diffusion method, and Vitek-2 Compact system. Antimicrobial susceptibility test discs and ETEST test strips were procured from Wenzhou Kangtai Biotechnology Co. in accordance with the manufacturer’s instructions. To control the quality of results, all laboratory activities were strictly conducted in accordance with ISO 15189.13 Antibiotic sensitivity testing followed the method recommended by the American Clinical and Laboratory Standardization Institute (CLSI) in 2021. The quality control strains used included E. coli ATCC25922, S. aureus ATCC25923 (for paper method) and ATCC29213 (for Minimum Inhibitory Concentration (MIC) method), Pseudomonas aeruginosa ATCC27853, E. faecalis ATCC29212, Streptococcus pneumoniae ATCC49619, and Haemophilus influenzae ATCC49247.
Statistical Analysis
The antibiotic sensitivity test results were interpreted according to the CLSI 20219 guidelines. Analysis of the data was performed using WHONET 5.6 software and version standards. The chi-square test was performed to compare the differences in the proportion of positive blood cultures among the sex, age, and hospital ward groups. Furthermore, to evaluate the significance of the annual trend, the Mann-Kendall trend test was employed on the linear trend. This statistical analysis allowed for a robust assessment of the temporal patterns observed in the data. Statistical analysis was performed using SPSS Statistics 28.0 (IBM Corp, NY, USA) and R software version 4.2.3.
Results
Blood Culture
A total of 29,283 blood culture tests were conducted from 2018 to 2021, with 3660 tests (12.5%) yielding positive results. Among these positive blood culture results, males accounted for 47.0% (1721/3660) and females accounted for 53.0% (1939/3660). The blood culture positivity rate was found to be significantly higher in individuals aged 60 years and above, with a rate of 60.7% (2223/3660)(P < 0.05), compared to those in the age groups of 0–17 years, where the rate was 3.4% (125/3660), and 18–59 years, where the rate was 35.8% (1312/3660). Patients’general information is presented in Table 1. This stark disparity in blood culture positivity rates across different age groups highlights the increased susceptibility and potential severity of infections among elderly individuals. The top five departments in this study were found to be Digestion Center, ICU, Neurology Center, Urology Department, and Hematology Department. The positive rate of blood culture of Digestion Center was significantly higher than that of other hospital wards (P < 0.05). Please refer to Figure 1 Distribution of clinical departments with positive blood culture bacteria, 2018–2021.
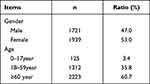 |
Table 1 Baseline Data of Patients |
 |
Figure 1 Distribution of clinical departments with positive blood culture bacteria, 2018–2021. |
Distribution of Bacteria
From 2018 to 2021, our hospital collected a total of 3660 clinical, non-repeated strains that yielded positive blood cultures. Among these, 76.7% (2807 strains) were identified as Gram-negative, while the remaining 23.3% (853 strains) were Gram-positive. The most frequently isolated strains during this period were E. coli(44.8%), Klebsiella spp. (19.2%), S. aureus (9.2%), Enterococcus spp. (5.3%), and Enterobacter spp. (3.4%). Please refer to Table 2 for a detailed breakdown of the major species distribution.
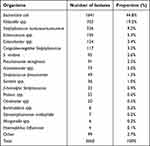 |
Table 2 Distribution of Clinically Isolated Bacteria, 2018–2021 |
Antibiotic Resistance Characteristics of Gram-Positive Bacteria
In the period spanning from 2018 to 2021, a comprehensive survey of blood culture-positive isolated specimens yielded a total of 336 S. aureus and 117 coagulase-negative Staphylococcus (CoNS)strains. The detection rates of MRSA and MRCNS were 39.3% and 71.8%, respectively. Notably, there were no isolated Staphylococci strains that exhibited resistance to either vancomycin or linezolid, a finding that is presented in Table 3. This dataset represents a valuable resource for future investigations into antibacterial treatment modalities.
 |
Table 3 Rates (%) of Staphylococcus spp Resistance to Antimicrobial Agents from 2018 to 2021 |
Enterococci spp. were isolated from blood culture-positive specimens during the period spanning 2018 to 2021. A total of 195 Enterococcus spp. were identified, with 79 (40.5%) and 93 (47.7%) being E. faecalis and E. faecium, respectively. E. faecalis exhibited higher rates of resistance to antibiotics, with the exception of tetracycline, compared to other Enterococcus spp. Notably, vancomycin-resistant E. faecium strains were identified (all confirmed by E-test strips), while no enterococci resistant to linezolid were detected in the isolates. Antibiotic sensitivity data is presented in Table 4.
 |
Table 4 Rates (%) of Enterococcus spp. Resistance to Antimicrobial Agents from 2018 to 2021 |
Antibiotic Resistance Characteristics of Gram-Negative Bacteria
In common gram-negative bacilli, high detection rates of extended-spectrum β-lactamase (ESBL) were observed for E. coli (47.5%, 779/1641) and Klebsiella pneumoniae (14.8%, 104/703). Notably, ESBL-producing strains exhibited higher resistance rates to most antimicrobial treatments compared to non-ESBL producing strains. However, it is noteworthy that E. coli demonstrated low resistance rates to meropenem (0.2%) and imipenem (0.4%), respectively. Similar trends were observed for Klebsiella spp., with resistance rates to meropenem and imipenem at 2.4% and 3.0%, respectively. These specific antibiotic sensitivity findings are presented in Table 5.
 |
Table 5 Rates (%) of Common Gram-Negative Bacilli. Resistance to Antimicrobial Agents from 2018 to 2021 |
Discussion
Bloodstream infection (BSI) is a grave systemic infectious malady typified by the infiltration of deleterious microorganisms, including bacteria and fungi, into the bloodstream.14 Annually, a staggering 31 million cases of sepsis are reported globally.15 During the designated study period, a noteworthy 3660 cases (equivalent to 12.5%) of blood cultures exhibited positive results. A considerable 60.7% of these blood stream infections (BSIs) were observed in patients aged ≥60 years, demonstrating a notably higher culture positivity rate within this age bracket compared to other groups. These findings substantiate prior study outcomes and lend further credence to the observations made.16–18 Gram-negative bacteria (76.7%) were the dominant isolated pathogen group compared to gram-positive bacteria (23.3%). This result is consistent with those reported by reputable organizations in China such as the China Antimicrobial Drug Surveillance Network (CHINET),19 Vietnam Antimicrobial Resistance Network (VINARES),20 and Korea Global AMR Surveillance System (Kor-GLASS).21,22 However, this study diverges from the findings of numerous studies conducted in various regions, including Europe and Africa, as well as within our own country. These studies consistently identified Gram-positive bacteria as the prevailing culprits responsible for BSI.5,23,24 According to the findings of this investigation, E. coli (44.8%) emerged as the predominant causative agent, followed closely by K. pneumoniae (17.5%, 639/3660) and S. aureus (9.2%). This discovery aligns with previous reports from diverse countries and regions.20,22 However, this stands in stark contrast to investigations conducted in Italy and certain hospitals in Africa, where Coagulase-Negative Staphylococci (CoNS) and Salmonella have been consistently identified as the prevailing culprits responsible for bloodstream infections (BSIs).24,25 The reasons for these differing results may be multifaceted and could arise from dissimilar amounts of specimen collections, disparities in geographical locations, and distinctive community lifestyles. Among all the Gram-negative organisms identified, E. coli ranked foremost with a notable detection rate of broad-spectrum-lactamase ESBLs at an impressive 47.5%, surpassing the rate reported in Vietnam, which stood at 45%,26 Relevant studies show that patients who were infected with ESBL-producing Enterobacteriaceae should be firstly treated with carbapenems.27 The preponderance of E. coli as the primary causative agent for bloodstream infections (BSIs) is a worldwide phenomenon.28 The incidence of carbapenem resistance in this study was found to be less than 1%, which is notably lower than the 3.5% reported in Vietnam. Furthermore, the VINARES report from 2016–2017 revealed that E. coli strains isolated from blood and cerebrospinal fluid samples exhibited a carbapenem resistance rate of 8%, surpassing the resistance rate observed in this study.16,20 In addition, a comprehensive analysis (focusing on bloodstream infections (BSIs)) conducted from 2017 to 2019 showed that E. coli resistance to carbapenems ranged from 0.1% to 0.2%, which is consistent with the results of the present study, consistently low rates of E. coli resistance to carbapenems.22 Meanwhile, the resistance rates for piperacillin/tazobactam and cefoperazone/sulbactam remain at a low level, which indicates that these antibacterial medications containing enzyme inhibitors could still be viable treatment options for E. coli-caused bloodstream infections. K. pneumoniae, a member of the Enterobacteriaceae family, is another common causative agent for bloodstream infections, following only E. coli in terms of its frequency. However, the detection rate of broad-spectrum extended-spectrum beta-lactamases (ESBLs) was found to be relatively low at 14.8%, which stands in stark contrast to the higher percentage of 72% documented in India.29 Within the scope of our investigation, it was determined that the resistance rate of K. pneumoniae to carbapenem antibiotics persisted at approximately 3%. In contrast, several studies conducted in China have reported a considerably higher resistance rate of 26.5% for K. pneumoniae towards carbapenem antibiotics, thus highlighting a notable discrepancy when compared to our study findings.30 However, it should be noted that while the resistance rate of K. pneumoniae towards carbapenems remains low, there has been a gradual increase in the detection rate of Carbapenem-resistant Klebsiella pneumoniae (CR-KP) over the years. The key mechanisms underlying carbapenem resistance in enterobacteria include the production of carbapenemases, deficits in outer membrane protein expression, elevated expression levels of efflux pumps, and altered target locations of antimicrobial antibiotic action. Antimicrobial resistance in non-fermentable, Gram-negative bacilli (such as Acinetobacter baumannii) presents a serious challenge. Bacteremia caused by A. baumannii is a prevailing cause of mortality amongst patients, with the associated mortality rate ranging from 32.5% to 63.5%.31,32 Research highlights that A. baumannii is predominantly multidrug-resistant, challenging to manage and spreads rapidly - causing bloodstream infections in critically unwell patients with potentially grave consequences. Alarming findings emerged from our investigation of A. baumannii, indicating that over 55% of the isolates exhibited resistance to carbapenem antimicrobials. This resistance rate closely aligns with the 56.5% reported by Wang et al,32 underscoring the consistent and concerning trend of carbapenem resistance in Acinetobacter baumannii strains,32 furthermore, it is noteworthy that the rate of carbapenem resistance observed in our investigation of A. baumannii bloodstream infections (BSIs) was comparatively lower than that reported in BSI studies conducted in other geographical regions.16,20,22 In contrast, P. aeruginosa exhibits a lower resistance rate than A. baumannii, with carbapenem resistance at only approximately 5%. Data obtained from a comprehensive study conducted at a tertiary care hospital in Beijing unveiled a concerning resistance rate of 27.8% among P. aeruginosa strains towards carbapenem antibiotics. This rate starkly contrasts with our study data, which demonstrates a significantly lower resistance rate.30 Apart from carbapenemase synthesis, P. aeruginosa strategy of resistance includes high bacterial antibiotic efflux pump expression, bacteriophage biofilm formation, and alterations to extracellular membrane permeability. The antibiotic resistance rates of common Gram-positive bacteria were investigated, indicating a MRSA detection rate of 39.3% - higher than the 19% rate reported by de Kraker ME28 Intriguingly, our results indicate a higher rate of resistance than that reported in an Italian study (28.1%).24 In cases where staphylococci induce bloodstream infections, vancomycin or linezolid may be used. Vancomycin and linezolid are preferred options for treating patients with some antimicrobial gram-positive bacteria, such as MRSA, because of their effectiveness against these bacteria.33
In this investigation, E. faecium was found to exhibit greater resistance to most antimicrobial antibiotic than E. faecalis - although tetracycline proved less resistant for the former. The rate of antibiotic resistance is high, except for vancomycin, which maintains a resistance rate to Enterococcus faecium of about 5%, Of note, our study found a higher prevalence of vancomycin resistance in enterococci compared to data from a study in Africa.23 When treating with vancomycin, it is recommended that vancomycin trough concentrations be ≥15 mg/L while trying not to exceed 20 mg/L to avoid excessive nephrotoxicity.34 Underscoring the importance of promptly sending microbiological specimens for early clarification of pathogenesis and antibiotic resistance when treating suspected bloodstream infections caused by E. faecium in order to avoid the use of ineffective antimicrobials.
Limitations of This Study
It should be noted that our evaluation and discussion was limited to instances from within our hospital, which may not fully represent broader patterns. Going forward, we aspire to conduct a multi-center study in order to obtain more comprehensive results.
Conclusions
To sum up, the prevalence of Enterobacteriaceae bacteria in bloodstream infections was found to be high in our hospital, especially among patients with liver disease, severe illness, urinary and hematologic disorders, as well as major medication resistance of A. baumannii. Bloodstream infection is a serious infectious condition that constitutes a risk factor for patient mortality. These findings might help the healthcare professionals to make informed decisions and provide better care for the patients.30
Data Sharing Statement
All data used for analyzing and generating the results of this study are included in this article.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of Suining Central Hospital (approval number: KYLLKS20230102), which waived the requirement of written informed consent from patients. All strains are part of the routine laboratory procedures of the hospital and do not involve any human genetic resources. This study was conducted in accordance with the principles outlined in the Declaration of Helsinki.
Consent for Publication
All authors have read the manuscript and consent to publish.
Acknowledgments
We would like to thank the staff of the Microbiology Department of Suining Central Hospital for their contribution.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors declare that they have not received any funding to carry out this study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Martinez RM, Wolk DM, Hayden RT, Wolk DM, Carroll KC, Tang Y-W. Bloodstream infections. Microbiol Spectr. 2016;4(4). doi:10.1128/microbiolspec.DMIH2-0031-2016
2. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock. Intensive Care Med. 2016;43:304e77.
3. Scheer CS, Fuchs C, Gründling M, et al. Impact of antibiotic administration on blood culture positivity at the beginning of sepsis: a prospective clinical cohort study. Clin Microbiol Infect. 2019;25(3):326–331. doi:10.1016/j.cmi.2018.05.016
4. Zhang X, Gu B, Mei Y, Wen Y, Xia W. Increasing resistance rate to carbapenem among blood culture isolates of Klebsiella pneumoniae, Acinetobacter baumannii and Pseudomonas aeruginosa in a university-affiliated hospital in China, 2004–2011. J Antibiot (Tokyo). 2015;68(2):115–120. PMID: 25182483. doi:10.1038/ja.2014.119
5. Gao J, Song J. Clinical analysis of distribution and drug resistance of pathogenic bacteria in blood culture of Dalian Municipal Central Hospital from 2015 to 2019. Pak J Med Sci. 2022;38(7):1931–1937. doi:10.12669/pjms.38.7.5377
6. Lee H, Yoon E-J, Kim D, et al. Antimicrobial resistance of major clinical pathogens in South Korea, May 2016 to April 2017: first one-year report from Kor-GLASS. Eurosurveillance. 2018;23(42). doi:10.2807/1560-7917.ES.2018.23.42.1800047
7. Gagliotti C, Balode A, Baquero F, et al. Escherichia coli and Staphylococcus aureus: bad news and good news from the European Antimicrobial Resistance Surveillance Network (EARS-Net, formerly EARSS), 2002 to 2009. Eurosurveillance. 2011;16(11):19819. PMID: 21435327. doi:10.2807/ese.16.11.19819-en
8. Aryee A, Rockenschaub P, Gill MJ, Hayward A, Shallcross L. The relationship between clinical outcomes and empirical antibiotic therapy in patients with community onset gram-negative bloodstream infections: a cohort study from a large teaching hospital. Epidemiol Infect. 2020;148:e225. doi:10.1017/S0950268820002083
9. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing[S]. M100-S30. Wayne, PA: CLSI; 2021.
10. Jamulitrat S, Meknavin U, Thongpiyapoom S. Factors affecting mortality outcome and risk of developing nosocomial bloodstream infection. Infect Control Hosp Epidemiol. 1994;15(3):163–170. doi:10.2307/30145555
11. Leber AL. Clinical Microbiology Procedures Handbook.
12. Garcia LS. Clinical Microbiology Procedures Handbook.
13. International Organization for Standardization. ISO 15189-Medical Laboratories - Requirements for Quality and Competence.
14. Kern WV, Rieg S. Burden of bacterial bloodstream infection-a brief update on epidemiology and significance of multidrug-resistant pathogens. Clin Microbiol Infect. 2020;26(2):151–157. doi:10.1016/j.cmi.2019.10.031
15. Lamy B, Sundqvist M, Idelevich EA; ESCMID Study Group for Bloodstream Infections, Endocarditis and Sepsis (ESGBIES). Bloodstream infections - standard and progress in pathogen diagnostics. Clin Microbiol Infect. 2020;26(2):142–150. doi:10.1016/j.cmi.2019.11.017
16. Van An N, Hoang LH, Le HHL, et al. Distribution and antibiotic resistance characteristics of bacteria isolated from blood culture in a teaching hospital in Vietnam during 2014–2021. Infect Drug Resist. 2023;16:1677–1692. doi:10.2147/IDR.S402278
17. Skogberg K, Lyytikäinen O, Ollgren J, et al. Population-based burden of bloodstream infections in Finland. Clin Microbiol Infect. 2012;18(6):E170–E176. doi:10.1111/j.1469-0691.2012.03845.x
18. Mehl A, Åsvold BO, Lydersen S, et al. Burden of bloodstream infection in an area of Mid-Norway 2002–2013: a prospective population-based observational study. BMC Infect Dis. 2017;17(1):205. doi:10.1186/s12879-017-2291-2
19. Hu F, Zhu D, Wang F, et al. Current status and trends of antibacterial resistance in China. Clin Infect Dis. 2018;67(suppl_2):S128–S134. doi:10.1093/cid/ciy657
20. Vu TVD, Choisy M, Do TTN, et al. Antimicrobial susceptibility testing results from 13 hospitals in Viet Nam: VINARES 2016–2017. Antimicrob Resist Infect Control. 2021;10(1):78. doi:10.1186/s13756-021-00937-4
21. Lee H, Yoon EJ, Kim D, et al. Antimicrobial resistance of major clinical pathogens in South Korea, May 2016 to April 2017: first one year report from Kor-GLASS. Euro Surveill. 2018;23(42):1800047. doi:10.2807/1560-7917.ES.2018.23.42.1800047
22. Kim D, Yoon EJ, Hong JS, et al. Major bloodstream infection-causing bacterial pathogens and their antimicrobial resistance in South Korea, 2017–2019: Phase I report from Kor-GLASS. Front Microbiol. 2021;12:799084. doi:10.3389/fmicb.2021.799084
23. Deku JG, Dakorah MP, Lokpo SY, et al. The Epidemiology of bloodstream infections and antimicrobial susceptibility patterns: a Nine-Year Retrospective Study at St. Dominic Hospital, Akwatia, Ghana. J Trop Med. 2019;2019:6750864. doi:10.1155/2019/6750864
24. Licata F, Quirino A, Pepe D, et al. Antimicrobial resistance in pathogens isolated from blood cultures: a Two-Year Multicenter Hospital Surveillance Study in Italy. Antibiotics. 2020;10(1):10. doi:10.3390/antibiotics10010010
25. Tack B, Phoba MF, Van Puyvelde S, et al. Salmonella typhi from blood cultures in the Democratic Republic of the Congo: a 10-year surveillance. Clin Infect Dis. 2019;68(Suppl 2):S130–S137. doi:10.1093/cid/ciy1116
26. Dat VQ, Vu HN, Nguyen The H, et al. Bacterial bloodstream infections in a tertiary infectious diseases hospital in Northern Vietnam: aetiology, drug resistance, and treatment outcome. BMC Infect Dis. 2017;17(1):493. doi:10.1186/s12879-017-2582-7
27. Katip W, Yoodee J, Uitrakul S, et al. Efficacy of loading dose colistin versus carbapenems for treatment of extended spectrum beta lactamase producing Enterobacteriaceae. Sci Rep. 2021;11(1):18. doi:10.1038/s41598-020-78098-4
28. de Kraker ME, Jarlier V, Monen JC, Heuer OE, van de Sande N, Grundmann H. The changing epidemiology of bacteraemias in Europe: trends from the European antimicrobial resistance surveillance system. Clin Microbiol Infect. 2013;19(9):860. PMID: 23039210. doi:10.1111/1469-0691.12028
29. Hemalatha V, Padma M, Sekar U, Vinodh TM, Arunkumar AS. Detection of Amp C beta lactamases production in Escherichia coli & Klebsiella by an inhibitor based method. Indian J Med Res. 2007;126(3):220–223.
30. Zhu Q, Zhu M, Li C, et al. Epidemiology and microbiology of gram-negative bloodstream infections in a tertiary-care hospital in Beijing, China: a 9-year retrospective study. Expert Rev Anti Infect Ther. 2021;19(6):769–776. doi:10.1080/14787210.2021.1848544
31. Ballouz T, Aridi J, Afif C, et al. Risk factors, clinical presentation, and outcome of Acinetobacter baumannii bacteremia. Front Cell Infect Microbiol. 2017;7:156. doi:10.3389/fcimb.2017.00156
32. Wang X, Zhang L, Sun A, et al. Acinetobacter baumannii bacteremia in patients with haematological malignancy: a multicentre retrospective study from the infection working party of Jiangsu society of hematology. Eur J Clin Microbiol Infect Dis. 2017;36(7):1073–1081. doi:10.1007/s10096-016-2895-2
33. Birmingham MC, Rayner CR, Meagher AK, et al. Linezolid for the treatment of multidrug-resistant, gram-positive infections: experience from a compassionate-use program. Clin Infect Dis. 2003;36(2):159–168. doi:10.1086/345744
34. Katip W, Okonogi S, Oberdorfer P. The thirty-day mortality rate and nephrotoxicity associated with trough serum vancomycin concentrations during treatment of enterococcal infections: a propensity score matching analysis. Front Pharmacol. 2022;12:773994. doi:10.3389/fphar.2021.773994
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
