Back to Journals » Open Access Journal of Contraception » Volume 14
Discontinuation Rate of Intrauterine Device and Associated Factors Among Women in the Last One Year in Angacha District, Southern Ethiopia
Authors Mulatu A, Mathewos Oridanigo E , Markos M
Received 24 March 2023
Accepted for publication 21 June 2023
Published 5 July 2023 Volume 2023:14 Pages 119—128
DOI https://doi.org/10.2147/OAJC.S382973
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Alemu Mulatu,1 Eyassu Mathewos Oridanigo,2 Melese Markos3
1Kembata Tembaro Zone Health Department, Durame, Ethiopia; 2Department of Nursing, College of Medical and Health Sciences, Wachemo University, Durame Campus, Durame, Ethiopia; 3Department of Midwifery, College of Medical and Health Sciences, Wachemo University, Durame Campus, Durame, Ethiopia
Correspondence: Eyassu Mathewos Oridanigo, Tel +251911598052 ; +251986973832, Email [email protected]
Background: Discontinuation of intrauterine contraceptive device is the phenomenon of starting a contraceptive method and then ending it within one year of its use. Discontinuation of an intrauterine contraceptive method often leads to unintended pregnancy; this tips to potentially unsafe abortions and unintended births. Even though Ethiopian government gives an attention to long acting reversible contraceptives, especially IUCD, there are no recent studies conducted in the study area. Thus, this study aimed to assess the discontinuation rate of IUCD and associated factors among women in the last one year in Angacha District, southern Ethiopia.
Methods: A community-based cross-sectional study was conducted from June 22 to July 22, 2020. Multistage sampling was used to select a total of 596 women who used IUCD during the last year in the Angacha district. Data were collected using pre-tested structured questionnaires. The collected data were entered into Epidata version 3.1 and exported to SPSS version 23 for analysis. Multivariate logistic regression analysis was carried out to identify factors independently associated with discontinuation IUCD. The significance level was set at a p-value of < 0.05 and AOR with 95% CI was used to interpret the association.
Results: In this study, 116(19.5%) women discontinued the use of IUCD in the last year with a 95% CI of 16.3%– 22.5%. Counseling before IUCD insertion [AOR (95% CI) = 2.5(1.03, 6.03)], marital status [AOR (95% CI) = 0.23(0.08, 0.69)], access to IUCD service [AOR (95% CI) = 0.29(0.12, 0.72)], and parity [AOR (95% CI) = 3.69(1.97, 8.84)] were significant with discontinuation of IUCD.
Conclusion: The overall magnitude of IUCD discontinuation in the study area was found to be high. Counseling before IUCD insertion and parity were positively associated while marital status of mothers and access to IUCD services were negatively associated with the discontinuation of IUCD.
Keywords: Angacha district, discontinuation, intrauterine device, Kembata Tembaro zone
Background
Discontinuation of Intra Uterine Contraceptive Device (IUCD) is the phenomenon of starting a contraceptive method and then ending it within one year of its use.1 IUCD is the world’s most widely used method of reversible birth control.2 Efficacy with the IUCD device is high, with a failure rate of less than 1% per year with prolonged use.3,4 Unlike other contraceptive methods like pills, IUCD does not need to think about taking it every day or using it every time they have sex, and its utilization results in fewer unintended pregnancies and fewer clinic visits as compared to other methods.5
For many women, the IUCD is an excellent choice since the method was safe, highly effective, reversible, and inexpensive.6 In countries with high fertility rates and unmet need for contraceptives, shifting towards long-acting reversible contraception is a vital strategy to make sure continuity of services. It also helps to satisfy the necessity for spacing and limiting births which have the potential to forestall thousands of cases of maternal mortality and further by preventing 80 million unintended pregnancies occurring annually.7
Discontinuation of an IUCD often leads to unintended pregnancy; this tips to potentially unsafe abortions and unintended births that expose a risk to the health of the women.8 The higher discontinuation rate of the IUCD is a public health concern and it is also a failure of the program.9 Along with their health impact, the economic impact of discontinuing IUCD is very high.10 A significant proportion of women discontinue the service within one year even without any side effects.11 Globally, nearly, 20–50% of reversible modern methods users discontinue employing IUCD during the primary 12 months of initiating it, and another 7–27% stop employing birth control for reasons linked to the standard of service use.12 According to a report based on developing countries, 13.1% of IUCD users discontinue its use during the first 12 months, 26.3% within 24 months, and 36.7% by the third year of its use.13 Similarly, Ethiopian 2016 EDHS reports showed that 13.2% of IUCD users discontinued its use during the first 12 months and also 35% of them discontinued in five years.14 Different studies also indicated that the discontinuation of IUCD users in Ethiopia within the first 12 months ranges from 8% to 19.2%.1,6,13
From the available limited research, it was indicated that side effects and health concerns like irregular bleeding, lower abdominal pain, and vaginal discharge play an important role in the discontinuation of the IUCD.15 Socio-demographic variables (Level of parity or need for more children, preferred family size, sex preference, and religious concern) along with healthcare-related variables (appointment for follow-up, quality of care, satisfaction, and counseling) also contributed to discontinuation.1 Thus, understanding these factors behind the IUCD discontinuation may help in developing a strategy that can help in improving the continuation of IUCD in the study area and thereby contributing towards decreasing the number of unintended pregnancies and adverse outcomes. There were also no similar studies conducted in the study area. Therefore, this study aimed to conduct the discontinuation of the IUCD and its associated factors in Angacha District, Southern Ethiopia.
Methodology
Study Setting
The study was conducted in Angacha District, Kembata Tembaro Zone, southern Ethiopia, which is located 290-km southwest of Addis Ababa, the capital of Ethiopia. The district is bounded by the Hadiya Zone in the east, the Doyogena District in the west and the south, and the Damboya District in the north. According to the 2007 national population and housing census projections, the district has a total population of 117,826, among which 51% were females, with a total of 23,165 households residing in 22 Kebeles (the kebele being the smallest administrative unit). According to the District Administrative Report, there is one primary hospital, five public health centres, six private clinics, three drug shops and one rural drug vendor. There are also various different non-governmental organizations working in different areas, such as those focused on transforming primary health care units, gender health, Communicable Disease Control (CDC), HIV/AIDS prevention and control, and Medan Act. A prominent example is Food for Hungry (FH) Ethiopia. According to the 2019 Report of the Angacha District Health Office, the estimated reproductive age group is 27,454. The contraceptive acceptance rate of the district was 94%, with Long Act Family Planning (LAFP) at 50%, of which 15% was IUCD (Ethiopian Financial Year, Personal Communication, July 2019).
Study Period and Design
The study was carried out between June 22 and July 22, 2020. A community-based cross-sectional study design was employed.
Population
The source population comprised all women in Angacha District with prior experience of IUCD use. The study population included participants selected from women who had used IUCD within the preceding one year (from June 2018 to June 2019) and were living in randomly selected 14 Kebeles in Angacha. IUCD users who were unable to speak and hear at the time of data collection were excluded from the study.
Sample Size Determination
The sample size was calculated by using a single population proportion formula for a cross-sectional study with the assumption of a 95% confidence level, a 5% margin of error, and by obtaining p=50%, ie the proportion of the discontinuation rate of IUCD since there was no study conducted in the study areas or in homogenous population.
Since the multistage sampling technique was employed, a design effect 1.5 was used and by considering a 10% non-response rate, the final actual sample size was n= 634.
Sampling Procedure
Out of 22 kebeles in the study area, 14 kebeles were selected using Simple Random Sampling (SRS). After allocating the sample size proportionally to each selected kebele, systematic random sampling was used to select study subjects. A list of IUCD users is taken from the family planning registration book, and chart review of each selected kebele from health centers. The study subjects from each kebele were achieved through house-to-house interview. The first sample included was identified using the lottery method. When two or more eligible women were present in one household, only one woman was considered.
Data Collection
Data was collected using interviewer-administered structured questionnaires, which were designed to collect data concerning socio-demographic factors (Age, education, occupation, number of children, residence, and monthly income), health facility and service-related factors (accessibility, availability of method mix, previous history of FP use and the level of HF in which women received IUCD), healthcare provider-related factors (counseling before IUCD insertion, and follow-up after IUCD insertion), reproductive history-related factors (previous history of pregnancy, age at first pregnancy, parity, who decided to have more children), and individual health concern-related factors (reason for removal, date of insertion of IUCD and its duration). Data was collected from house to house in a place where the participants felt free to express their feelings and ideas. For women who were absent in their homes at the time of the data collection, repeated visits were done to decrease the non-response rate. Five nurses and 2 health officers were involved as data collectors and supervisors, respectively. They were selected outside the study area to minimize interviewer bias. It takes nearly 57 minutes as average interview time during data collection.
Data Quality Assurance
The quality of data was assured by proper designing of the questionnaires and training the data collectors and supervisors before data collection. The data collectors and supervisors were trained intensively for two days on the aim of the study, the contents of the questionnaires, and the procedures to be followed by principal investigator. All the questionnaires were translated from English to Amharic (local language) and then re-translated back to English by language experts to check their consistencies. They were pre-tested on 5% of the calculated sample size in the kebele, which was found outside of the study area. Every day after data collection, questionnaires were reviewed and checked to maintain their accuracy and completeness by data collectors and supervisors.
Data Analysis
The collected data was entered into Epidata version 3.1 and then exported to SPSS version 23 for analysis. The data were cleaned for inconsistencies and missing values. Frequency distributions, diagrams, cross-tabulations, and percentages were used to present the findings as appropriate. Bivariate analysis was used to identify factors associated with the discontinuation of IUCD and variables with a p-value of less than 0.25 were considered as candidate variables for multivariable analysis. Multivariable analysis was performed using the backward LR method to identify factors independently associated with the discontinuation of IUCD. The significance level was set at 5% and AOR (Adjusted Odds Ratio) and 95% CI (Confidence Interval) were used to interpret the results. Hosmer and Lemeshow’s goodness-of-fit test was used to check the consistency of the given observed values with the model assumed under the null hypothesis. Multicollinearity was checked and VIF was less than 10.
Operational Definitions
Contraceptive: An agent or device intended to prevent conception.
Physical accessibility of IUCD: If a woman walked less than 6 km to reach the health facility from her home, IUCD was physically accessed, otherwise not.
Counseling: Making the women aware of its long protection, side effects, and effectiveness of IUCD utilization.13
IUCD discontinuation: When IUCD was removed due to health concerns, accidental loss from the inserted site, or any other reason by a health worker within 1 year of its use following insertion.1
Ethical Clearance
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance was obtained from the ethical review committee of Wolaita Sodo University, College of Health Sciences, and Medicine (with letter number: ERC/202 and date: 5/06/2020). A letter of cooperation was obtained from the Kembata Tembaro Zone Health Department and Angacha District Health Office. After a clear discussion about the actual study or explaining the purpose of the study, verbal informed consent was obtained from each study subject and this consent process was accepted and approved by the Wolaita Sodo University ethics committee. Confidentiality was maintained and they were informed that they had the full right to discontinue or refuse to participate in the study.
Results
Socio-Demographic Characteristics of the Respondent
In this study, 596 women participated with a response rate of 94%. More than half, 331(55.5%) were in the age range of 25–34. The mean and SD age of the women was 32.1 and ± 5.74 years respectively. Among the respondents, 217(36.4%) had no formal education but 31(5.2%) had some diploma or higher education level. Regarding the occupation of respondents, nearly two-thirds, 397(66.7%) were housewives and only 33(5.5%) were government employees (Table 1).
 |
Table 1 Socio-Demographic Related Factors Among IUCD Users Among Women in Angacha District, Southern Ethiopia, September 2020 |
Health Facility and Service-Related Factors
Among the IUCD acceptors, almost all, 567(95.1%) had access to the IUCD insertion service site. Regarding the type of contraceptives, more than half, 342(57.4%) used short-acting contraceptives (pills and injectables), 111(18.6%) used IUCD, and 118(20.0%) used implants previously. But 22(3.7%) never used contraceptives previously. In this study, 390(65.4%), 115(19.3%), and 91(15.3%) women utilized IUCD in Health Centers (HCs), hospitals, and health posts, respectively.
Healthcare Provider Related Factors
In this study, 489(82%) women received counseling before IUCD insertion. Among them, nearly three-fourth of them, 370(62.1%) counseled individually, while nearly one-fourth 119(20.0%) were counseled together with their husbands. Almost all of them, 572(96.0%) revealed that the IUCD was the method of their choice (Table 2).
 |
Table 2 IUCD Acceptors’ Responses Regarding Service Provider and Facilities Related Factors in Angacha District, Oct 2020 |
Reproductive History Related Factors
Almost all, 586(98.3%) respondents had previous history of pregnancy, and only 42(7%) married before the age of 18 years. Of the respondents, more than two-third, 414(69.8%) desired to have additional children. Regarding decision on the number of children, more than half, 339(56.9%) decided with their husbands (Table 3).
 |
Table 3 Reproductive History-Related Factors Among IUCD Acceptors in Angacha District, Southern Ethiopia, September 2020 |
The Magnitude of the IUCD Discontinuation Rate Among Women in the Angacha District
Out of 596 women who used IUCD during the last 1 year, 116(19.5%) discontinued it with a 95% CI of 16.3%–22.5%. The mean and SD of utilization of IUCD before discontinuation was 7.97 ± 3.024 months respectively. Among them, nearly half, 59(50.9%) discontinued between 7 and 12 months, 38(32.2%) discontinued between 3 and 6 months and 19(16.1%) discontinued within 3 months. Of the women who discontinued IUCD, 40(34.6%) reported misconception as the main reason for discontinuation (Figure 1).
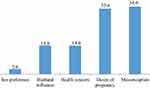 |
Figure 1 Reasons for discontinuation of IUCD among mothers in Angacha district, Southern Ethiopia, 2020. |
Factors Affecting IUCD Discontinuation Rate Among Women in Angacha District, Southern Ethiopia
Among 15 variables in bivariate analysis, 8 of them had a p-value of less than 0.25; hence they were candidates for multivariable logistic regression analysis. Bivariate analysis revealed that marital status, maternal education and occupation, monthly income, physical accessibility of IUCD, follow-up, counseling before IUCD insertion, and parity had p-values of <0.25 and they were candidates for multivariable logistic regression analysis. The candidate variables were again entered into multiple logistic regression models with backward LR methods to obtain variables, which were independently associated with the discontinuation of IUCD. Multivariable analysis revealed that marital status, parity, physical accessibility of IUCD, and counseling before IUCD insertions were significant with discontinuation of IUCD.
In this study, married women were 77% times less likely to discontinue the IUCD than single mothers [AOR (95% CI) = 0.23(0.08, 0.69)]. Women who did not receive counseling before IUCD insertion were 2.5 times more likely to discontinue the IUCD than their counterparts [AOR (95% CI) = 2.5(1.03, 6.03)] (Table 4).
 |
Table 4 Multivariate Analysis of Factors Associated with IUCD Discontinuation Among Women in Angacha District, Southern Ethiopia, September 2020 |
Discussion
The finding of this study revealed that 19.5% [95% CI: 16.5–22.8%] of women in Angacha District discontinued the use of IUCD in the past 12 months. The magnitude of IUCD discontinuation observed in this study was in line with an earlier study performed in Indonesia.16 However, the finding was higher than studies conducted in Tanzania, Ghana, and Egypt, which found 13.9%, 11.2 and, 14.3%, respectively.4,15,17 The probable reasons for the discrepancy might be due to socio-cultural differences among the different populations. This is confirmed by difference in age structure of the population of this study and previous studies. Most women included in this study were young than previous studies. Moreover, it might be due to the lower educational status of the population in this study than others. In this study, more than one-third of women did not join any formal education, which limits them to obtain and follow-up on new information from the Medias.
The finding from this study revealed that married women were less likely to discontinue IUCD than single women. This finding was supported by the study conducted in Northwest Ethiopia and Kenya.6,18 This could be due to the reason that unmarried or single women are not a good candidate for IUCD as they could have multiple sexual partners, which consequently lead to sexually transmitted infection and it may expose for discontinuation. In this study, parity was found to be another predictor of discontinuation of IUCD. The study revealed that the majority of women requesting discontinuation of the IUCD were grand multiparous. Women who gave 4–6 births were more likely to discontinue IUCD than women who gave 1–3 births. The finding was supported by a study conducted in Nigeria.19 This could be because the grand multiparous women are close to menopausal age considering the preponderance age of grand multiparty in the study area.
Women who did not receive counseling before IUCD insertion were more likely to discontinue IUCD than their counterparts. This finding was in agreement with studies done in Ethiopia, Ghana, South Africa, and Pakistan.12,15,20,21 This may be explained by the fact that in the absence of counseling, IUCD users are exposed to rumors and misconceptions which leads to premature removal. As part of the provision of quality services for IUCD during the initiation of its use, women were thought to be provided with information on potential side effects and options to consider including method switching, when they experience intolerable side effects.22 Pre-insertion counseling regarding possible side effects might decrease the fear of women for potential side effects.23 Furthermore, IUCD users who did not have access to IUCD service are less likely to discontinue IUCD than those who had access to the service. This finding was also supported by previous studies done in Brazil.24
Limitations of the Study
The interviews were retrospective and the data on indicators related to side effects were self-reported by the respondents, and not verified or confirmed by healthcare professionals. Due to the cross-sectional study design, no causal inferences can be made regarding the temporal association between the potential factors and discontinuation.
Conclusion
The overall magnitude of IUCD discontinuation in the study area was found to be high. Counseling before intrauterine contraceptive device insertion and parity were positively associated while marital status of women and access to IUCD service were negatively associated with the discontinuation of IUCD. Healthcare providers should provide counseling strictly before insertion and after proper follow-up, they should take corrective action at the right time and emphasis should be given for training of service providers regarding method of family planning and counseling in collaboration with supportive organizations.
Abbreviation
CDC, communicable disease control; CI, confidence interval; EDHS, Ethiopian Demographic and Health Survey; FP, family planning; HH, household; HIV, human immune deficiency virus; IUCD, inter uterine contraceptive device; LAPM, long-acting and permanent contraceptives methods; MPH, master of public health; RH, reproductive health; SPSS, Statistical Package for Social Sciences; SSA, sub-Saharan Africa; SNNPR, South Nations and Nationalities of People’s Regional; WHO, World Health Organization.
Data Sharing Statement
Data can be made available upon reasonable request from the corresponding author.
Acknowledgments
We would like to express our sincere gratitude to Wolaita Sodo University, the College of Medicine and Health Sciences, and the School of Public Health for technical support. Our thanks go to the managers of health facilities for their permission to conduct the study in their facilities. The authors also acknowledge their study participants for providing the necessary information and the data collectors for collecting the data carefully.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Wolde TF, AYana K, Bekele F. Determinants of intrauterine contraceptive device discontinuation among women using family planning, in Southwest Ethiopia: unmatched case–control study. Open Access J Contracept. 2022;13(April):39–47. doi:10.2147/OAJC.S351930
2. Franklin SG, O’Neal M, Arneus A, Colvin C, Aung M, Jolly PE. Effectiveness of an intrauterine device informative intervention among post-natal women in Western Jamaica. Reprod Health. 2021;18(1):1–6. doi:10.1186/s12978-021-01075-1
3. Goldstuck ND, Cheung TS. The efficacy of intrauterine devices for emergency contraception and beyond: a systematic review update. Int J Womens Health. 2019;11:471–479. doi:10.2147/IJWH.S213815
4. Rwegoshora FJ, Muganyizi PS, Kimario GF, Paul PP, Makins A. A one-year cohort study of complications, continuation, and failure rates of postpartum TCu380A in Tanzania. Reprod Health. 2020;17(1):1–10. doi:10.1186/s12978-020-00999-4
5. United Nations D of E and SA. Contraceptive use by method 2019 - data booklet [Internet]; 2019. Available from: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2019_contraceptiveusebymethod_databooklet.pdf.
6. Gashaye KT, Tsegaye AT, Abebe SM, Woldetsadik MA, Ayele TA, Gashaw ZM. Determinants of long acting reversible contraception utilization in Northwest Ethiopia: an institution-based case control study. PLoS One. 2020;15(10 October):1–19. doi:10.1371/journal.pone.0240816
7. Haakenstad A, Angelino O, Irvine CMS, et al. Measuring contraceptive method mix, prevalence, and demand satisfied by age and marital status in 204 countries and territories, 1970–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2022;400(10348):295–327. doi:10.1016/S0140-6736(22)00936-9
8. United Nations Department of Economics and Social Affairs PD. World family planning 2022 [Internet]. Meeting the changing needs for family planning: contraceptive use by age and method; 2022:43. Available from: https://www.un.org/en/development/desa/population/publications/pdf/family/WFP2017_Highlights.pdf.
9. Wolde TF. Determinants of intrauterine contraceptive device discontinuation among women using family planning, in Southwest Ethiopia: unmatched case – control study. Open Access J Contracept. 2022;2022:39–47.
10. Khalifa M, Abdel Aziz Hussein W, Metwally S. The impact of method choice on the risk of contraceptive discontinuation: Egypt 2014. J Humanit Appl Soc Sci. 2022;4(1):39–56.
11. Chethan R, A GS, S C. Study on post partum intrauterine contraceptive device practices and causes for discontinuation of PPIUCD at follow up in a tertiary hospital. Int J Reprod Contracept Obstet Gynecol. 2018;7(6):2299. doi:10.18203/2320-1770.ijrcog20182339
12. Fekadu GA, Omigbodun AO, Roberts OA, Yalew AW. Factors associated with early long-acting reversible contraceptives discontinuation in Ethiopia: evidence from the 2016 Ethiopian demographic and health survey. Arch Public Health. 2020;78(1):1–10.
13. Weldekidan HA, Lemlem SB, Sinishaw Abebe W, Sori SA. Discontinuation rate of long-acting reversible contraceptives and associated factors among reproductive-age women in Butajira town, Central Ethiopia. Womens Health. 2022;18:17455057221104656.
14. Central Statistical Agency (CSA) and ICF Addis Ababa E. Demographic and health survey 2016: Ethiopia; 2016.
15. Gbagbo FY, Kayi EA. Use and discontinuation of intrauterine contraceptive device in the greater Accra region of Ghana. Contracept Reprod Med Res. 2018;3(8):1–17.
16. Id MG, Utomo B, Budiharsana M, Id GD. Pregnancy resumption following contraceptive discontinuation: hazard survival analysis of the Indonesia demographic and health survey data 2007. PLoS One. 2022;17(2):1–13. doi:10.1371/journal.pone.0264318
17. Mohamed N, El A, Ahmed H, Mostafa RH, Abuelghar W, Elbishry G. Discontinuation rates among copper intrauterine device users in primary healthcare unit and university clinic. Is there a difference ? Egypt J Hosp Med. 2018;72(July):5658–5665. doi:10.21608/ejhm.2018.11543
18. Ontiri S, Were V, Kabue M, Biesma-blanco R, Stekelenburg J. Patterns and determinants of modern contraceptive discontinuation among women of reproductive age: analysis of Kenya Demographic Health Surveys. PloS One. 2003;2020:e0241605.
19. Bello OO, Agboola AD. Discontinuation of intrauterine device: are the reasons changing ? Afr J Med Health Sci Full. 2020;19(May):15–21.
20. Azmat SK, Shaikh BT, Hameed W, Bilgrami M, Mustafa G. Rates of IUCD discontinuation and its associated factors among the clients of a social franchising network in Pakistan. BMC Womens Health. 2012;12(1):8. doi:10.1186/1472-6874-12-8
21. Hofmeyr GJ, Singata-madliki M, Lawrie TA, Bergel E, Temmerman M. Effects of the copper intrauterine device versus injectable progestin contraception on pregnancy rates and method discontinuation among women attending termination of pregnancy services in South Africa: a pragmatic randomized controlled trial. Reprod Health. 2016;1–8. doi:10.1186/s12978-015-0112-x
22. Daniele MAS, Cleland J, Benova L, Ali M. Provider and lay perspectives on intra- uterine contraception: a global review. Reprod Health. 2017;2017(14):1–11.
23. Schrumpf LA, Stephens MJ, Nsarko NE, et al. Side effect concerns and their impact on women s uptake of modern family planning methods in rural Ghana: a mixed methods study. BMC Womens Health. 2020;2020(20):1–8.
24. Borges C, Moreau C, Luiza A, Borges V. Contraceptive discontinuation: frequency and associated factors among undergraduate women in Brazil. Reprod Health. 2019;9:1–12.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

