Back to Journals » International Journal of General Medicine » Volume 16
Differences in the Proportion of CYP2C19 Loss-of-Function Between Cerebral Infarction and Coronary Artery Disease Patients
Authors Shi Y, Yang Y, Feng M, Ling W, Wei T, Cao Y, Zhong R, Wu H
Received 30 May 2023
Accepted for publication 3 August 2023
Published 14 August 2023 Volume 2023:16 Pages 3473—3481
DOI https://doi.org/10.2147/IJGM.S420108
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Yuliang Shi,1,2 Yuxian Yang,1,2 Miaoling Feng,1,2 Weihan Ling,1,2 Tongguo Wei,1,2 Yumin Cao,1,2 Rui Zhong,1,2 Heming Wu2
1Department of Neurology, Meizhou People’s Hospital, Meizhou Academy of Medical Sciences, Meizhou, People’s Republic of China; 2Center for Precision Medicine, Meizhou People’s Hospital, Meizhou Academy of Medical Sciences, Meizhou, People’s Republic of China
Correspondence: Heming Wu, Center for Precision Medicine, Meizhou People’s Hospital, Meizhou Academy of Medical Sciences, No. 63 Huangtang Road, Meijiang District, Meizhou, People’s Republic of China, Email [email protected]
Background: Cytochrome P450 2C19 (CYP2C19) genotypes and metabolic phenotypes (extensive metabolizer (EM), intermediate metabolizer (IM), and poor metabolizer (PM)) are related to the metabolism of therapeutic drugs for cardiovascular and cerebrovascular diseases. This study aimed to investigate the differences of CYP2C19 gene polymorphism distribution between coronary artery disease (CAD) patients and cerebral infarction (CI) patients.
Methods: We identified 413 CI patients, 509 CAD patients, and 241 CI+CAD patients from 2016 to 2020 and studied genotypes of CYP2C19 rs4986893 (636G>A) and rs4244285 (681G>A) polymorphisms using PCR-gene chip detection method. Differences in CYP2C19 genotypes and metabolic phenotypes between the groups were compared. To analyze the efficacy of CYP2C19 metabolic phenotypes in discriminating between cerebral infarction and coronary artery disease, multiple logistic regression analysis was conducted after adjusting for gender, age, smoking history, drinking history, hypertension, and diabetes.
Results: There were significant differences in the distribution of CYP2C19 genotypes and metabolic phenotypes between CI and CAD patients. The results of multivariate logistic regression (adjusted for sex, age, smoking, drinking, hypertension, and diabetes) indicated that CYP2C19 IM phenotype (IM vs EM: OR 1.443, 95% CI: 1.086– 1.918, P=0.011) and CYP2C19 IM+PM phenotype (IM or PM vs EM: OR 1.440, 95% CI: 1.100– 1.885, P=0.008) may be indicators of CI from CAD.
Conclusion: CYP2C19 EM metabolic phenotype was dominant in CAD patients, and CYP2C19 IM metabolic phenotype was dominant in CI patients. After adjusting for other confounding factors, patients with the CYP2C19 IM metabolic phenotype were more likely to develop CI than CAD.
Keywords: CYP2C19, genotype, metabolic phenotype, cerebral infarction, coronary artery disease
Introduction
Cardiovascular and cerebrovascular diseases are the general terms for ischemic or hemorrhagic diseases of the heart, brain, and other related tissues and organs caused by hypertension, atherosclerosis, hyperlipidemia, and so on.1 The incidence of cardiovascular and cerebrovascular diseases has increased in recent years and has become an important global health burden.2,3 Ischemic cardiovascular and cerebrovascular diseases mainly include coronary artery disease (CAD) and cerebral infarction (CI).1 CAD is a disease in which plaque is caused by the accumulation of lipids in the blood on the intima of the artery, and the increasing amount of plaque causes narrowing of the arterial cavity, blocks blood flow, and leads to heart ischemia.4 CI is a disease in which ischemic hypoxic lesion and necrosis of brain tissue are caused by regional blood supply disorder of brain tissue, and produces corresponding loss of nerve function.5
Clopidogrel is a widely used antiplatelet therapy drug in clinical practice and has important application value in the prevention and treatment of patients with platelet aggregation diseases and arterial circulation disorders.6,7 Many factors affecting the difference of individual reactivity to clopidogrel, and gene polymorphisms play an important role, and these studies mainly focused on Cytochrome P450 2C19 (CYP2C19) gene polymorphisms.8,9 It was found that clopidogrel resistance was associated with CYP2C19 gene polymorphisms.10 CYP2C19 polymorphisms have a significant impact on the clinical outcomes of clopidogrel therapy in patients with stenting procedure for cerebral artery stenosis.11 As a precursor drug, clopidogrel needs to be metabolized by cytochrome P450 (CYP) isoenzymes in vivo to be transformed into active metabolites with platelet inhibition, especially CYP2C19 enzyme, and CYP2C19 function-related gene polymorphisms may affect the platelet inhibitory effect of clopidogrel.12 CYP2C19 rs4986893 (636G>A) and CYP2C19 rs4244285 (681G>A) are the most common polymorphisms in CYP2C19 gene and are defined as loss-of-function (LOF) variants related to decreased platelet response to clopidogrel or increased incidence of clopidogrel resistance.13 Based on the different genotypes of CYP2C19, the metabolic phenotype of individuals can be classified as extensive metabolizers (EM) (CYP2C19 636G/G complicated with 681G/G), intermediate metabolizers (IM) (CYP2C19 636G/G complicated with 681G/A, or 636G/A complicated with 681 G/G), and poor metabolizers (PM) (CYP2C19 636G/G complicated with 681A/A, or 636G/A complicated with 681 G/A, or 636A/A complicated with 681G/G).14
To date, to our knowledge, there have been no reports of differences in the distribution of CYP2C19 gene polymorphisms between patients with cardiovascular disease and patients with cerebrovascular disease. This study aimed to investigate the distribution of CYP2C19 gene polymorphisms in patients with cardiovascular and cerebrovascular diseases (CAD, and CI, CAD combined with CI) and whether there are differences between patients with CAD and CI. The results of this study will provide valuable reference for clinicians.
Materials and Methods
Study Population
This retrospective, observational study was approved by the Ethics Committee of the Meizhou People’s Hospital. A total of 1163 unrelated patients with cardiovascular and cerebrovascular diseases were included in this study, including 413 patients with CI, 509 patients with CAD, and 241 patients with CI combined with CAD, collected from Meizhou People’s Hospital, between January 2016 and June 2020.
The CAD diagnosis was confirmed using coronary angiography based on the American College of Cardiology/American Heart Association (ACC/AHA) classification.15 Patients with CI are diagnosed by at least two neurologists based on clinical symptoms and computed tomography (CT)/magnetic resonance imaging (MRI) and other findings. The inclusion criteria were as follows: (1) Clinically diagnosed as atherosclerosis; (2) The clinical data of the patients were complete; (3) Adults. The exclusion criteria were as follows: (1) Incomplete clinical data of the patients; (2) Atherosclerosis patients with severe infectious diseases, autoimmune diseases, organ insufficiency, and other diseases. Information on age, sex, history of smoking, history of alcohol consumption, hypertension, and diabetes was collected from the Hospital Information System (HIS) of Meizhou People’s Hospital.
Detection of CYP2C19 Gene Variants
Genomic DNA was extracted from the whole blood of these patients using the QIAamp DNA extraction kit (Qiagen, Germany), according to the manufacturer’s instructions. CYP2C19 rs4986893 (636G>A) and CYP2C19 rs4244285 (681G>A) variants were detected using a CYP2C19 Genotyping Kit with PCR-gene chip detection method (BaiO Technology Co, Ltd, Shanghai, China). The PCR procedure was as follows: pre-denaturation at 94°C for 5min, 35 cycles (94°C for 25s, 48°C for 40s, and 72°C for 30s) were amplified, and 72°C for 5min for the final elongation on the Veriti™ Dx 96-Well Thermal Cycler (Thermo Fisher Scientific, America).16 The method of gene chip hybridization method was used to detect PCR products on an automatic nucleic acid molecular hybridization instrument (BaiO Technology Co, Ltd, Shanghai, China). The wild-type fragments and the mutant fragments in the PCR amplification products were hybridized with the corresponding wild-type probes and mutant probes fixed on the chip, respectively, and the specific hybridization signal was chromogenic through an enzyme chromogenic reaction. The chip hybridization signal was read by a biochip reader (BaiO Technology Co., Ltd, Shanghai, China).16
Statistical Analysis
Data analysis in this study was performed using SPSS statistical software version 21.0 (IBM, USA). The significance of the Hardy-Weinberg equilibrium (HWE) of the CYP2C19 polymorphisms in the patients was analyzed by the χ2 test. Differences in the composition ratios and frequencies of CYP2C19 genotypes and metabolic phenotypes among different patients were analyzed using the χ2 test. To analyze the efficacy of CYP2C19, metabolic phenotypes in discriminating between CI and CAD, a multiple logistic regression analysis was conducted after adjusting for sex, age, smoking history, drinking history, hypertension, and diabetes. P<0.05 was used as the level of statistical significance for all statistical analyses in this study.
Results
Characteristics of Patients
This study included 1163 patients with cardiovascular and cerebrovascular diseases, including 800 (68.8%) men and 363 (31.2%) women, respectively. There were 354 (30.4%) cases aged <65 years old and 809 (69.6%) cases aged ≥65 years old. There were 413 CI patients, 509 CAD patients, and 241 CI combined with CAD patients in this study. There were no significant differences in the proportion of patients with a history of alcohol consumption (P=0.376) and proportion of patients with diabetes (P=0.179) among the different groups. The proportion of patients with history of smoking in CAD patients was significantly higher than that in patients with CI complicated with CAD, and the proportion of hypertension history in CI patients and patients with CI complicated with CAD was significantly higher than that in CAD patients, respectively (Table 1).
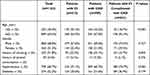 |
Table 1 Clinical Characteristics of Patients Among Different Groups in This Study |
Frequencies of CYP2C19 636G>A and CYP2C19 681G>A Genotypes in All Subjects and Patients Among Different Groups
The χ2 test was used to test the significance of the Hardy-Weinberg equilibrium of the CYP2C19 polymorphisms in the CI patients, CAD patients, and CI combined with CAD patients. Genotype distributions of CYP2C19 636G>A (χ2=0.696, P=0.404) and CYP2C19 681G>A (χ2=0.244, P=0.621) polymorphisms were consistent with the Hardy-Weinberg equilibrium in all participants. Genotype distributions of CYP2C19 636G>A and CYP2C19 681G>A polymorphisms were also consistent with Hardy-Weinberg equilibrium in patients with different diseases (all P>0.05) (Table 2).
 |
Table 2 Frequencies of CYP2C19 636G>A and CYP2C19 681G>A Genotypes in All Subjects and Patients Among Different Groups |
The frequencies of CYP2C19 636G>A and CYP2C19 681G>A genotypes and alleles were compared among patients with different diseases. The proportion of CYP2C19 636G>A alleles was significantly different among all groups (P=0.041). Specifically, the proportion of CYP2C19 636G>A G allele in the CAD group was significantly lower than that in the CI group (93.9% vs 96.2%, P=0.024). The proportion of CYP2C19 681G>A alleles was significantly different among all the groups (P<0.001). Specifically, the proportion of CYP2C19 681G>A G allele in the CAD group was significantly higher than that in the CI group (73.7% vs 65.7%, P<0.001) and CI complicated with the CAD group (73.7% vs 66.2%, P=0.003) (Table 2).
The Distributions of Different Genotypes’ Combinations and Metabolic Phenotypes of CYP2C19 in Different Groups
The proportion of different genotypes’ combinations was significantly different among all groups (P=0.006). The proportion of CYP2C19 636G/G + 681G/G in CAD group was significantly higher than that in the CI group (46.6% vs 37.5%, P=0.006), whereas the proportion of CYP2C19 636G/G + 681G/A in CAD group was significantly lower than that in the CI group (34.4% vs 43.8%, P=0.003). The proportion of CYP2C19 636G/G + 681G/G in CAD group was significantly higher than that in CI complicated with CAD group (46.6% vs 36.9%, P=0.014), the proportion of CYP2C19 636G/G + 681G/A in CAD group was significantly lower than that in CI complicated with CAD group (34.4% vs 46.5%, P=0.002). In addition, the proportion of different metabolic phenotypes was significantly different among all groups (P=0.035). The proportion of EM phenotype in CAD group was significantly higher than that in CI group (46.6% vs 37.5%, P=0.006), the proportion of IM phenotype in the CAD group was significantly lower than that in the CI group (42.0% vs 48.9%, P=0.039). The proportion of EM phenotype in CAD group was significantly higher than that in CI complicated with CAD group (46.6% vs 36.9%, P=0.014), the proportion of IM phenotype in CAD group was significantly lower than that in CI complicated with CAD group (42.0% vs 50.6%, P=0.028) (Table 3). The results of the pairwise comparisons of the distributions of CYP2C19 genotypes’ combinations and metabolic phenotypes among the three groups are shown in Table 4. These results indicate that CYP2C19 EM metabolic phenotype was dominant in CAD patients, and CYP2C19 IM metabolic phenotype was dominant in CI patients.
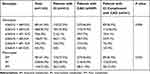 |
Table 3 The Distributions of Different Genotypes’ Combinations and Metabolic Phenotypes of CYP2C19 in Different Groups |
 |
Table 4 Pairwise Comparison of CYP2C19 Genotypes and Metabolic Phenotypes Distribution Among Three Groups |
Association of the CYP2C19 Metabolic Phenotypes with CI and CI Complicated with CAD Compared with CAD
Logistic regression analysis was performed to analyze the role of differential distribution of CYP2C19 metabolic phenotypes in differentiating CI from CAD. The results of multivariate logistic regression (adjusted for sex, age, smoking, drinking, hypertension, and diabetes) indicated that CYP2C19 IM phenotype (IM vs EM: OR 1.443, 95% CI: 1.086–1.918, P=0.011) and CYP2C19 IM+PM phenotype (IM or PM vs EM: OR 1.440, 95% CI: 1.100–1.885, P=0.008) may be indicators in differentiating CI from CAD. And CYP2C19 IM phenotype (IM vs EM: OR 1.409, 95% CI: 1.004–1.979, P=0.048) and CYP2C19 IM+PM phenotype (IM or PM vs EM: OR 1.389, 95% CI: 1.006–1.920, P=0.046) may be an indicator for differentiating CI complicated with CAD from CAD (Table 5). It means that patients with the CYP2C19 IM metabolic phenotype were more likely to develop CI than CAD.
 |
Table 5 Association of the CYP2C19 Metabolic Phenotypes with CI and CI Complicated with CAD Compared with CAD |
Discussion
Are there differences in the distribution of CYP2C19 genotypes and metabolic phenotypes between patients with CAD and CI? Whether the distribution of CYP2C19 genotypes and metabolic phenotypes can be used as an indicator to distinguish CAD from CI? However, these issues have not yet been resolved. The results of this study show that CAD patients mainly have EM metabolic phenotypes, while CI patients mainly have IM metabolic phenotypes. After adjusting for other confounding factors, patients with the CYP2C19 IM metabolic phenotype were more likely to develop CI than CAD.
In this study, the proportion of the percentages of CYP2C19 EM, IM, and PM phenotypes were 41.4%, 46.3%, and 12.4%, respectively. There have been some corresponding studies in other populations. CYP2C19 EM, IM, and PM phenotypes accounted for 33.2%, 47.1%, and 14.7%, respectively, in South-East Asian patients with acute coronary syndrome (ACS).17 CYP2C19 EM, IM, and PM phenotypes accounted for 39.9%, 45.6%, and 13.4%, respectively, in a Han Chinese population.18 These phenotypes accounted for 38.8%, 42.4%, and 15.3%, respectively, in Chinese Hui patients with coronary atherosclerotic heart disease; and 38.9%, 36.1%, and 7.1%, respectively, in Chinese Uygur patients with coronary atherosclerotic heart disease.13 In Taiwanese patients with ischemic stroke, the prevalence of CYP2C19 EM, IM, and PM phenotypes was 40.3%, 45.8%, and 13.8%, respectively.19 The percentages of CYP2C19 EM, IM, and PM phenotypes was 58%, 36%, and 6% in the Vietnamese population, respectively.20 The percentages of CYP2C19 EM, IM, and PM phenotypes was 48.22%, 42.98%, and 6.64% in a Thai population,21 41.20%, 24.07%, and 4.17% in the population of the Republic of Srpska.22 The prevalence of CYP2C19 EM, IM, and PM phenotypes was 75.97%, 21.91%, and 2.21% in a Greek population.23 In Moroccan population, the percentages of CYP2C19 EM, IM, and PM phenotypes was 83.45%, 14.14%, and 2.41%, respectively,24 the percentages was 75.8%, 21.1%, and 3.1% in Lebanese population.25 In the populations from Americas, the percentages of CYP2C19 EM, IM, and PM phenotypes were 85.3%, 13.6%, and 1.0%, respectively, in a Bolivian population,26 71.1%, 14.2%, and 0.5% in a Nicaraguan Mestizo population.27 In general, the frequencies of CYP2C19 IM and PM phenotypes are relatively high in Southeast Asian populations.
To date, to our knowledge, there have been no reports of differences in the distribution of CYP2C19 gene polymorphisms between patients with cardiovascular disease and patients with cerebrovascular disease. In this study, CYP2C19 EM metabolic phenotype was dominant in CAD patients, and CYP2C19 IM metabolic phenotype was dominant in CI patients. A study has suggested that a poor metabolizer status was associated with a higher risk for ischemic stroke.28 Loss of function of CYP2C19 is associated with increased risk of ischemic stroke after transient ischemic attack in intracranial atherosclerotic disease.29 In mechanism, CYP2C19 is associated with the pathological features of CI and CAD. Arachidonic acid (AA) can be metabolized by CYP2C19 into endodermal hyperpolarized factor (EDHF),30 while EDHF is beneficial for vascular dilation and inhibits vascular calcification.31 In contrast, reactive oxygen species (ROS) produced by coronary endothelial cells in the process of CYP2C19-catalyzed reaction,32 is a risk factor for cardiovascular and cerebrovascular diseases.33,34 The differences between CYP2C19 genotypes and metabolic phenotypes found in CI and CAD in this study may be related to the differences in the role of CYP2C19 at different arterial vascular sites. The results of this study need to be verified in further basic researches.
Clinically, according to the status of CYP2C19 and other genes related to drug metabolism, timely adjustment of therapeutic measures and dosage can avoid the insufficient efficacy of therapeutic drugs and reduce the occurrence of adverse events. To the best of our knowledge, this study is the first to report the differences in CYP2C19 genotypes and metabolic phenotypes between patients with CAD and CI. This study has some limitations. First, the association between these genotypes, metabolic phenotypes, and disease severity was not investigated, because this was a retrospective study. Second, this study was conducted among patients with CAD and CI in one hospital; there may be some bias in the results, as the included subjects were not completely representative. Third, this study only examined the differences in common polymorphisms of the CYP2C19 gene in the two diseases and did not study the relationship between CYP2C19 protein levels and disease risk. Therefore, future studies with larger sample sizes, disease severity, and analysis of CYP2C19 protein levels are needed.
Conclusion
In the cohort of this study, we found that CYP2C19 EM metabolic phenotype was dominant in CAD patients, and CYP2C19 IM metabolic phenotype was dominant in CI patients. After adjusting for other confounding factors, patients with the CYP2C19 IM metabolic phenotype were more likely to develop CI than CAD.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
As this study was a retrospective study, all participants were informed on the study procedures and goals and the informed consent from all the participants was obtained in verbal form through the telephone communication, which was approved by the Ethics Committee of the Meizhou People’s Hospital. The study was performed under the guidance of the Declaration of Helsinki and approved by the Ethics Committee of Medicine, Meizhou People’s Hospital.
Acknowledgments
The authors would like to thank their colleagues who were not listed in the authorship of the Department of Neurology, Meizhou People’s Hospital, for their helpful comments on the manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Science and Technology Program of Meizhou (Grant No.: 2019B0202001).
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Tapeinos C, Gao H, Bauleth-Ramos T, Santos HA. Progress in stimuli-responsive biomaterials for treating cardiovascular and cerebrovascular diseases. Small. 2022;18(36):e2200291. doi:10.1002/smll.202200291
2. Turana Y, Tengkawan J. Hypertension and stroke in Asia: a comprehensive review from HOPE Asia. J Clin Hypertens. 2021;23(3):513–521. doi:10.1111/jch.14099
3. Ji E, Lee S. Antibody-based therapeutics for atherosclerosis and cardiovascular diseases. Int J Mol Sci. 2021;22(11):5770. doi:10.3390/ijms22115770
4. Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S. A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol. 2019;234(10):16812–16823. doi:10.1002/jcp.28350
5. Zhao Y, Zhang X, Chen X, Wei Y. Neuronal injuries in cerebral infarction and ischemic stroke: from mechanisms to treatment (Review). Int J Mol Med. 2022;49(2):15. doi:10.3892/ijmm.2021.5070
6. Passacquale G, Sharma P, Perera D, Ferro A. Antiplatelet therapy in cardiovascular disease: current status and future directions. Br J Clin Pharmacol. 2022;88(6):2686–2699. doi:10.1111/bcp.1522
7. Akkaif MA, Sha’aban A. Coronary Heart Disease (CHD) in elderly patients: which drug to choose, ticagrelor and clopidogrel? A systematic review and meta-analysis of randomized controlled trials. J Cardiovasc Dev Dis. 2021;8(10):123. doi:10.3390/jcdd8100123
8. Lee CR, Luzum JA, Sangkuhl K, et al. Clinical pharmacogenetics implementation consortium guideline for CYP2C19 genotype and clopidogrel therapy: 2022 update. Clin Pharmacol Ther. 2022;112(5):959–967. doi:10.1002/cpt.252
9. Akkaif MA, Daud NAA, Noor DAM, et al. Platelet reactivity index after treatment of clopidogrel versus ticagrelor based on CYP2C19 genotypes among patients undergoing percutaneous coronary intervention: results of a randomized study. Eur Heart J. 2023;44(Supplement_1). doi:10.1093/eurheartj/ehac779.120
10. Akkaif MA, Daud NAA, Sha’aban A. The role of genetic polymorphism and other factors on Clopidogrel Resistance (CR) in an Asian Population with Coronary Heart Disease (CHD). Molecules. 2021;26(7):1987. doi:10.3390/molecules26071987
11. Li YJ, Chen X, Tao LN, Hu XY, Wang XL, Song YQ. Association between CYP2C19 polymorphisms and clinical outcomes in patients undergoing stent procedure for cerebral artery stenosis. Sci Rep. 2021;11(1):5974. doi:10.1038/s41598-021-85580-0
12. de Lara DV, de Melo DO. Pharmacogenetics of clopidogrel and warfarin in the treatment of cardiovascular diseases: an overview of reviews. Pharmacogenomics. 2022;23(7):443–452. doi:10.2217/pgs-2021-0158
13. Ma L, Yuan Y, Li J, Yu C, Zhao J. Distribution of CYP2C19, ABCB1 and PON1 polymorphisms in Chinese Han, Hui, Uygur and Kazak patients with coronary atherosclerotic heart disease. Int J Immunogenet. 2020;47(6):539–545. doi:10.1111/iji.12511
14. Yang E, Kim S, Kim B, et al. Night-time gastric acid suppression by tegoprazan compared to vonoprazan or esomeprazole. Br J Clin Pharmacol. 2022;88(7):3288–3296. doi:10.1111/bcp.15268
15. Han D, Beecy A, Anchouche K, et al. Risk reclassification with coronary computed tomography angiography-visualized nonobstructive coronary artery disease according to 2018 American College of Cardiology/American Heart Association Cholesterol Guidelines (from the Coronary Computed Tomography Angiography Evaluation for Clinical Outcomes: an International Multicenter Registry [CONFIRM]). Am J Cardiol. 2019;124(9):1397–1405. doi:10.1016/j.amjcard.2019.07.045
16. Cai N, Li C, Gu X, et al. CYP2C19 loss-of-function is associated with increased risk of hypertension in a Hakka population: a case-control study. BMC Cardiovasc Disord. 2023;23(1):185. doi:10.1186/s12872-023-03207-w
17. Tan DS, Aw JWX, Winther M, et al. CYP2C19 phenotype in South-East Asian Acute Coronary Syndrome patients and impact on major adverse cardiovascular events. J Clin Pharm Ther. 2020;45(1):52–58. doi:10.1111/jcpt.13062
18. He L, Chen S, Li J, et al. Genetic and phenotypic frequency distribution of CYP2C9, CYP2C19 and CYP2D6 in over 3200 Han Chinese. Clin Exp Pharmacol Physiol. 2020;47(10):1659–1663. doi:10.1111/1440-1681.13357
19. Lee YC, Liao YC, Chang FC, Huang HC, Tsai JY, Chung CP. Investigating CYP2C19 loss-of-function allele statuses and their association with stroke of different etiologies in a Taiwanese population. J Chin Med Assoc. 2019;82(6):469–472. doi:10.1097/JCMA.0000000000000101
20. Vu NP, Nguyen HTT, Tran NTB, et al. CYP2C19 genetic polymorphism in the Vietnamese population. Ann Hum Biol. 2019;46(6):491–497. doi:10.1080/03014460.2019.1687750
21. Sukprasong R, Chuwongwattana S, Koomdee N, et al. Allele frequencies of single nucleotide polymorphisms of clinically important drug-metabolizing enzymes CYP2C9, CYP2C19, and CYP3A4 in a Thai population. Sci Rep. 2021;11(1):12343. doi:10.1038/s41598-021-90969-y
22. Dorji PW, Wangchuk S, Boonprasert K, Tarasuk M, Na-Bangchang K. Pharmacogenetic relevant polymorphisms of CYP2C9, CYP2C19, CYP2D6, and CYP3A5 in Bhutanese population. Drug Metab Pers Ther. 2019;34(4). doi:10.1515/dmpt-2019-0020
23. Arvanitidis K, Ragia G, Iordanidou M, et al. Genetic polymorphisms of drug-metabolizing enzymes CYP2D6, CYP2C9, CYP2C19 and CYP3A5 in the Greek population. Fundam Clin Pharmacol. 2007;21(4):419–426. doi:10.1111/j.1472-8206.2007.00510.x
24. Afilal D, Basselam MA, Brakez Z, Chouham S, Brehm A, Izaabel EH. Genetic polymorphism of drug-metabolizing enzymes CYP2C9 and CYP2C19 in Moroccan population. Genet Test Mol Biomarkers. 2017;21(5):298–304. doi:10.1089/gtmb.2016.0304
25. Djaffar Jureidini I, Chamseddine N, Keleshian S, Naoufal R, Zahed L, Hakime N. Prevalence of CYP2C19 polymorphisms in the Lebanese population. Mol Biol Rep. 2011;38(8):5449–5452. doi:10.1007/s11033-011-0700-y
26. Bravo-Villalta HV, Yamamoto K, Nakamura K, Bayá A, Okada Y, Horiuchi R. Genetic polymorphism of CYP2C9 and CYP2C19 in a Bolivian population: an investigative and comparative study. Eur J Clin Pharmacol. 2005;61(3):179–184. doi:10.1007/s00228-004-0890-5
27. de Andrés F, Altamirano-Tinoco C, Ramírez-Roa R, Montes-Mondragón CF, Dorado P. Relationships between CYP1A2, CYP2C9, CYP2C19, CYP2D6 and CYP3A4 metabolic phenotypes and genotypes in a Nicaraguan Mestizo population. Pharmacogenomics J. 2021;21(2):140–151. doi:10.1038/s41397-020-00190-9
28. Gronich N, Lavi I, Lejbkowicz F, et al. Ischemic stroke and myocardial ischemia in clopidogrel users and the association with CYP2C19 loss-of-function homozygocity: a real-world study. Pharmacogenomics J. 2021;21(3):402–408. doi:10.1038/s41397-021-00218-8
29. Patel PD, Vimalathas P, Niu X, et al. CYP2C19 loss-of-function is associated with increased risk of ischemic stroke after transient ischemic attack in intracranial atherosclerotic disease. J Stroke Cerebrovasc Dis. 2021;30(2):105464. doi:10.1016/j.jstrokecerebrovasdis.2020.105464
30. Fisslthaler B, Fleming I, Busse R. EDHF: a cytochrome P450 metabolite in coronary arteries. Semin Perinatol. 2000;24(1):15–19. doi:10.1016/s0146-0005(00)80048-8
31. Chawengsub Y, Gauthier KM, Campbell WB. Role of arachidonic acid lipoxygenase metabolites in the regulation of vascular tone. Am J Physiol Heart Circ Physiol. 2009;297(2):H495–H507. doi:10.1152/ajpheart.00349.2009
32. Fleming I, Michaelis UR, Bredenkötter D, et al. Endothelium-derived hyperpolarizing factor synthase (Cytochrome P450 2C9) is a functionally significant source of reactive oxygen species in coronary arteries. Circ Res. 2001;88(1):44–51. doi:10.1161/01.res.88.1.44
33. Malekmohammad K, Sewell RDE. Antioxidants and atherosclerosis: mechanistic aspects. Biomolecules. 2019;9(8):301. doi:10.3390/biom9080301
34. Negre-Salvayre A, Guerby P, Gayral S, Laffargue M, Salvayre R. Role of reactive oxygen species in atherosclerosis: lessons from murine genetic models. Free Radic Biol Med. 2020;149:8–22. doi:10.1016/j.freeradbiomed.2019.10.011
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
