Back to Journals » Neuropsychiatric Disease and Treatment » Volume 17
Differences in the Association of Anxiety, Insomnia and Somatic Symptoms between Medical Staff and the General Population During the Outbreak of COVID-19
Authors Huang Y , Zhou Y, Wei Y, Zeng L, Yang J, Li Y, Song X, Li H, He H, Li T, Wu K , Yang M, Wu F , Ning Y, Zhang X
Received 6 January 2021
Accepted for publication 27 April 2021
Published 14 June 2021 Volume 2021:17 Pages 1907—1915
DOI https://doi.org/10.2147/NDT.S300719
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jun Chen
Yuanyuan Huang,1,* Yongjie Zhou,2,* Yi Wei,1 Lingyun Zeng,2 Jiezhi Yang,3 Yi Li,2 Xiuli Song,4 Hehua Li,1 Hongbo He,1 Ting Li,1 Kai Wu,5 Mingzhe Yang,1 Fengchun Wu,1,6,7 Yuping Ning,1,7 Xiangyang Zhang1,8
1Department of Psychiatry, The Affiliated Brain Hospital of Guangzhou Medical University (Guangzhou Huiai Hospital), Guangzhou, People’s Republic of China; 2Department of Psychiatry, Shenzhen Kangning Hospital, Shenzhen, People’s Republic of China; 3Department of Psychiatry, Shenzhen Health Development Research Center, Shenzhen, People’s Republic of China; 4Clinical Psychology, Yantai Affiliated Hospital of Binzhou Medical University, Yantai, People’s Republic of China; 5Department of Biomedical Engineering, School of Materials Science and Engineering, South China University of Technology (scUT), Guangzhou, People’s Republic of China; 6Department of Psychiatry, Guangdong Engineering Technology Research Center for Translational Medicine of Mental Disorders, Guangzhou, People’s Republic of China; 7The First School of Clinical Medicine, Southern Medical University, Guangzhou, People’s Republic of China; 8CAS Key Laboratory of Mental Health, Institute of Psychology, Chinese Academy of Sciences, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yuping Ning
Department of Psychiatry, The Affiliated Brain Hospital of Guangzhou Medical University (Guangzhou Huiai Hospital), 36 Mingxin Road, Liwan District, Guangzhou, 510370, People’s Republic of China
Email [email protected]
Xiangyang Zhang
CAS Key Laboratory of Mental Health, Institute of Psychology, Chinese Academy of Sciences, Beijing, People’s Republic of China
Email [email protected]
Background: During the outbreak of coronavirus disease 2019 (COVID-19), occupational differences were recognized with respect to psychological issues, but there are no reports regarding the insomnia and anxiety comorbidities and their related factors among the general public and medical staff. Our study aimed to compare the prevalence of anxiety and anxiety with insomnia, as well as the relationship between different psychological symptoms between the two groups.
Methods: A total of 605 medical staff and 1091 public respondents were assessed through an online questionnaire survey, including the 7-item Insomnia Severity Index (ISI), the somatization subscale of Symptom Checklist 90-Revised (SCL-90-R), and the 7-item Generalized Anxiety Disorder scale (GAD-7).
Results: Compared with the general public, medical staff had a higher incidence of anxiety (45.5% vs 32.4%). The incidence of insomnia in anxious participants was 52.7% in medical staff and 44.6% in the general public, and the difference was significant (p < 0.05). The GAD-7 score and somatization subscore of the SCI-90 were independently associated with insomnia among anxiety participants in both groups (all p < 0.001).
Conclusion: Our findings suggest that during the epidemic period of COVID-19, medical staff experienced more anxiety and anxiety with insomnia. Somatization, anxiety and insomnia are highly correlated among medical staff and the general public.
Keywords: somatic symptom, anxiety, insomnia, medical staff, COVID-19
Introduction
The 2019 novel coronavirus disease (COVID-19) pandemic is continuing to affect people around the world and poses a huge challenge to the global public health security. It is not only a serious public health problem,1 but has also caused increased great mental health problems.2 The outbreak of COVID-19 has had a negative impact on people’s daily lives and threatens both physical and mental health. For example, although family isolation measures can quickly and effectively prevent the rapid spread of this epidemic, they also affect people’s normal lives and work and even further endanger social and economic development.3 During the period of outbreak, people’s mental health and psychological distress have changed accordingly.4 Severe conditions can lead to mental health problems, including depressive symptoms, anxiety, fear, insomnia or somatic symptoms.5,6 Preliminary evidence indicates that during the COVID-19 pandemic, approximately 16–28% of the public have shown anxiety symptoms, which are the most common psychological reaction.5 In addition, it is well known that mental state plays a key role in epidemic management and the success of epidemic public health strategies.7
During the pandemic, occupational differences have been recognized with respect to psychological problems. Increasing evidence shows that medical staff are more likely to have mental health problems during the sudden outbreak of COVID-19.8,9 A recent study of 2182 Chinese subjects showed that medical staff had a significantly higher incidence of anxiety (13.0% vs 8.5%), insomnia (38.4% vs 30.5%), and somatization (1.6% vs 0.4%) than nonmedical health workers.9 Another psychological survey demonstrated that the incidences of anxiety and insomnia symptoms among in frontline medical staff were as high as 50.7% and 36.1%, respectively.10 Moreover, a study of 7236 public volunteers found that the incidence of anxiety and insomnia symptoms was 35.1% and 18.2% respectively, and medical staff were more prone to insomnia than people with other occupations.11 Compared with college students, the scores of all items of psychological stress, including fear, worry, sleep quality, etc. in medical staff were significantly higher.10 With the increase in the number of asymptomatic infections and the increasing severity of the pandemic, medical staff will face more pressure on treatment, and the public will also be under increasing pressure due to delays in returning to work and study.
As demonstrated in previous literature, there is a high rate of comorbidity between anxiety and insomnia with a bidirectional relationship.12 According to the diagnostic criteria of the DSM-5, sleep disturbance is part of generalized anxiety disorder (GAD). Mood disorders, especially anxiety are viewed as a common cause of insomnia.13 Conversely, a lack of sleep may increase the risk of anxiety-related symptoms, such as emotional disorders14 and impaired cognitive function.15 More than half of GAD patients have insomnia.12,16 A German health survey of 4181 participants found that patients with GAD were seven to eight times more likely to suffer insomnia than those in the control group.17 Moreover, increasing evidence supports the relationship between psychological stress and somatization during the COVID-19 pandemic. One study conducted in the Chinese general population showed that anxiety and insomnia were both independently associated with somatic symptoms.18 Similarly, our previous research revealed that insomnia and anxiety symptoms of Chinese medical staff during the COVID-19 pandemic were independently related to somatic symptoms.19 Taken together, during the COVID-19 pandemic, most studies reported each individual mental state and related factors of the general public or medical staff, while few studies have focused on the combination of anxiety and insomnia symptoms.
In view of the occupational differences in psychological health problems during the pandemic and the relationship between different mental states, it is of great significance to explore different mental states of the general public and medical staff, as well as the comorbidity of insomnia and anxiety and their relationships with somatization, which have not yet been reported. Therefore, our survey aimed to explore the different mental health statuses and related factors of medical staff and the general public in China through self-assessment of anxiety, insomnia and somatic symptoms to provide a theoretical basis for psychological intervention in different groups.
Methods
Participants and Procedures
We adopted a snowball sampling strategy to conduct an online and anonymous questionnaire survey to assess the psychological conditions of medical staff and the public from February 14 to March 29, 2020 (during the COVID-19 pandemic). Participants were invited through WeChat or email, and they completed the survey questionnaire with Ranxing Technology “SurveyStar”. Only after they completed all the questions could responses be submitted. All participants provided informed consent before entering the survey. They answered this question after being informed of the purpose of the study: “Do you agree to participate in the questionnaire?”. When the participants answered “yes”, they agreed and continued to complete the survey. Otherwise, they withdraw from the survey, and also, they could withdraw from the survey at any time. Inclusion criteria were as follows: (1) completed questionnaire; (2) 18–60 years old; and (3) Chinese people living in mainland China.
All procedures were performed in accordance with the Declaration of Helsinki promulgated by the National Institute of Health. This study was approved by the Ethics Committee of the Institute of Psychology of the Chinese Academy of Sciences.
Self-Measurement
The sociodemographic data included: occupation (medical staff or others), gender, age, body mass index (BMI), ethnicity, marital status, education, daily working hours, history of physical diseases, infection with COVID-19 in friends or relatives, and experience with the SARS pandemic. According to the policy on the division of responsibilities of the hospital during COVID-19, medical staff in the infection or emergency department were classified as front-line workers in terms of occupational classification because they had more opportunities to be exposed to patients with COVID-19, while others were considered second-line medical staff.
All participants completed the 7-item Insomnia Severity Index (ISI), the somatization subscale of Symptom Checklist 90-Revised (SCL-90-R), and the 7-item Generalized Anxiety Disorder (GAD-7) scale. These scales have been widely used in the study of psychological state measurement in China and have high reliability and validity.20–23
The GAD-7 was used to evaluate the presence of anxiety and the severity of symptoms, with a total score of 0 (not present) to 21 (extremely severe). According to previous literature, people with a total score of ≥5 on GAD-7 can be considered as the existence of anxiety symptoms.19,24,25 The ISI was used to assess insomnia symptoms, with a score from 0 to 28 points (not present to severe). A total score of ≥8 (cut-off score) can be identified as insomnia.25 The somatization subscale of the SCL-90-R was used to estimate somatic symptoms: the total score ranges from 12 to 60 points, corresponding to not present to extremely, and higher scores indicate more severe symptoms. The subscale contains 12 items with a five-point (none to severe) Likert scale (Cronbach’s α = 0.83). According to the results of the Chinese norm, a single item with a score greater than or equal to 2 points is considered a potential problem, and patients with SCL-90-R somatization subscale score ≥ 24 points are considered to have somatic symptoms.9,26
Statistical Analysis
Data analysis was performed using SPSS 18.0 statistical software. The Kolmogorov–Smirnov test was performed to test for normality. Continuous variables including age, BMI and scale scores, are expressed as the mean ± standard deviation, and analysis of variance (ANOVA) was used for comparisons between groups. Since the scores of all scales were not normally distributed, all data were first logarithmically transformed. Then, analysis of covariance (ANCOVA) was used to control for confounding factors. Other demographic and clinical variables are expressed as percentages (%) and the χ2 test was used for comparison between groups. Also, the incidence of anxiety comorbid with insomnia among different occupations was compared by χ2 test. Furthermore, Spearman correlation coefficients were performed to explore the relationship between ISI scores and demographic and clinical variables. Finally, multivariate logistic regression analysis (stepwise forward entry models) was used to assess factors associated with insomnia in anxiety subjects. A P-value less than 0.05 was defined as statistically significant (two-tailed).
Results
Differences in Sample Characteristics
Table 1 shows the sociodemographic data and the measured scores of medical staff and the general population. In total, we recruited 1696 subjects (605 medical staff and 1091 public respondents) in mainland China. Among the medical staff, 45.5% (275/605) participants had anxiety symptoms and the percentage of insomnia symptoms in participants with anxiety was 52.7% (145/275). Among the general public, 32.4% (354/1091) participants had anxiety symptoms, while 44.6% (158/354) participants with anxiety suffered from insomnia symptoms. Compared with the general public, medical staff had significantly higher prevalences of anxiety (p < 0.001, OR = 1.735) and anxiety with insomnia (p < 0.05, OR = 1.384). Furthermore, there were significant differences in GAD-7 scores, somatization subscores of SCL-90 and ISI scores between medical staff and general public. When gender, marital status, education attainment, and history of physical disease were added as covariates, there were still significant differences in GAD-7 scores (F = 2.472, p < 0.001, r 2 = 0.136), somatization subscores of SCL-90 (F = 3.391, p < 0.001, r 2 = 0.151), and ISI scores (F = 1.505, p = 0.044, r 2 = 0.131) between the two groups.
 |
Table 1 Sociodemographic Data and Measurement Scores Between Medical Staff and the General Public Group |
Differences in the Non-Insomnia vs Insomnia Groups with Anxiety
The psychological status of participants with anxiety in the subgroups with and without insomnia subgroups is shown in Table 2. Among anxious medical staff, the SCI-90 somatization subscale the scores of the ISI, and GAD-7 were significantly higher in participants with insomnia than in those without insomnia (all p< 0.001). When daily working hours and physical disease history were added as covariates, there were still significant differences in GAD-7 score, SCL-90 somatization subscore, and ISI score (all p< 0.05). Next, Spearman correlation analysis showed that the ISI score was significantly positively correlated with history of physical diseases (r = 0.172, p = 0.035), daily working hours (r = 0.125, p = 0.038), somatization subscores of the SCL-90 (r = 0.424, p < 0.001) and GAD-7 score (r = 0.451, p < 0.001).
 |
Table 2 Sociodemographic Data and Self-Measurement Scores of Anxiety Participants without or with Insomnia Symptoms |
In the general public, compared to the anxiety without insomnia subgroup, the anxiety with insomnia subgroup had significantly higher scores on the ISI, SCI-90 somatization subscale and GAD-7 (all p< 0.001). When a history of physical disease was added as a covariate, there were still significant differences in GAD-7 score, SCL-90 somatization subscores, and ISI scores (all p< 0.05). Furthermore, Spearman correlation analysis showed that ISI score was significantly positively correlated with a history of physical diseases (r = 0.202, p < 0.001), somatization subscores of the SCL-90 (r = 0.459, p< 0.001), and GAD-7 score (r = 0.368, p< 0.001) (Table 2).
Relationship Between Anxiety with Insomnia and Somatization Symptoms
Multiple logistic regression analysis was performed to examine the relationship between anxiety and insomnia in medical staff and the general public. Insomnia in anxious participants was the dependent variable, and the covariates included variables that inhibited statistical significance in univariate analyses, including history of physical diseases, daily working hours, somatization subscore of SCL-90 and GAD-7 score.
In medical staff, somatization subscores of SCL-90 (OR=1.115; 95% CI: 1.052–1.182; p< 0.001) and GAD-7 score (OR=1.198; 95% CI: 1.098–1.307; p< 0.001) were independent contributors to insomnia in the participants with anxiety (Table 3).
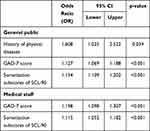 |
Table 3 Factors Associated with Insomnia in Participants with Anxiety |
In the general public, physical disease history (OR=1.608; 95% CI: 1.025–2.522; p = 0.039), GAD-7 score (OR=1.127; 95% CI: 1.069–1.188; p< 0.001) and somatization subscore of SCL-90 (OR=1.154; 95% CI: 1.109–1.202; p< 0.001) were independent contributors to insomnia in the participants with anxiety (Table 3).
Discussion
To our best knowledge, this study is the first to compare anxiety with insomnia symptoms and related factors (especially the relationship with somatic symptoms) between medical staff and the general public during the COVID-19 outbreak in China. Our primary results included the following: (1) Compared with the general public, medical staff had a higher incidence of anxiety (45.5% vs 32.4%). (2) Compared with the general public, medical staff had a higher insomnia rate in anxious participants (52.7% vs 44.6%). (3) The GAD-7 score and somatization subscore of the SCI-90 were factors related to insomnia in the anxious participants in both medical staff and the general public.
First, medical staff exhibited a higher incidence of anxiety symptoms than nonmedical staff, consistent with most of previous studies,9,10,27 but both were much higher than the proportion of psychological symptoms in the general public during the nonepidemic period in China.28,29 Similar to previous reports on the incidence (20–50%) of anxiety and insomnia,20,30,31 this study demonstrated that both medical staff and the general public were under greater psychological stress during the epidemic. The fact that medical staff suffer from more psychological problems may be attributed to the following: (1) The most influential factor may be the working environment of medical personnel,9,32 including a high risk of exposure to confirmed or suspected cases of COVID-19, long-term workload, lack of specific drugs, shortage of protective equipment, etc. Our study also found that medical workers who worked more than 8 hours a day were more likely to have insomnia symptoms. (2) After the end of work, first-line medical staff spent more time alone and had no face-to-face interpersonal communication, which led to an increase in negative emotions (anxiety, depression, fear, etc.).33 Medical workers may be prevented from going home because there is a public misunderstanding that they may come back with the virus, increasing the chances of people around them becoming infected. (3) Some medical staff were unable to participate in clinical first-line work due to specific personal circumstances (such as pregnancy or physical discomfort), which may have increased their sense of guilt.34 In the current pandemic period, the psychological status of medical staff cannot be ignored. A recent review on healthcare workers during the COVID-19 pandemic further suggested that psychiatric teams should be invited to evaluate the mental states of front-line medical health workers.35
Second, we found that medical workers had a higher incidence of insomnia among anxious participants than among the general public (52.7% vs 44.6%). This is the first study to compare the incidence of insomnia among anxious subjects between different occupations. However, our results and all previous studies showed that the incidence of insomnia was relatively high in anxious subjects.16,36,37 A study of 5692 Chinese respondents reported that approximately 45% of insomniacs coexisting anxiety symptoms.37 Maher et al found that the incidence of insomnia in anxious patients was as high as 70%.36 A previous study reported that patients with generalized anxiety disorder had different types of insomnia, indicating that 47.7% of patients had difficulty falling sleep, 63.6% of patients had difficulty maintaining sleep, and 56.8% of patients woke up too early.16 Moreover, our study found that medical workers who work more than 8 hours a day were more likely to have insomnia symptoms. The long-term heavy workload of medical staff caused circadian rhythm disturbance and reduced rest time, which led to sleep rhythm disorder and insomnia.38 People who work in an isolated environment are 1.71 times more likely to suffer from insomnia than ordinary people.34 The high prevalence of comorbidities is attributed to the interaction between insomnia and anxiety. On the one hand, acute insomnia increases anxiety symptoms,39 which may be caused by hypothalamic-pituitary axis (HPA) dysfunction and deficits in executive function.40 Neuroimaging studies have further shown that sleep deprivation for one night decreases functional connectivity between the medial-prefrontal cortex and the amygdala and increases the amygdala response to negative stimuli,41 resulting in anxiety. Additionally, lack of sleep increases cortisol output, and elevated cortisol may cause anxiety.42 On the other hand, heightened anxiety may in turn impair sleep, which might be related to anxiety symptoms and processes.43 Anxiety increases cortisol levels and decreases melatonin synthesis, reducing sleep quality.44 A previous study also reported that sleep disorders or insomnia symptoms were associated with an increased risk of anxiety for 2–4 years.45 Because of the higher incidence of insomnia in medical staff with anxiety, it is necessary to explore factors related to comorbidities between different occupations.
Our study also identified potential risk factors for the development of insomnia in anxious participants. We found that the GAD-7 and SCI-90 somatization subscale scores were influential factors for the coexisting insomnia and anxiety in both the general public and medical workers, and SCL-90 somatization score was positively correlated with the insomnia score. Similar to our results, a cross-sectional study of 2008 people showed that all types of anxiety disorders were independently related to somatic symptoms, while GAD had the strongest correlation with cardiopulmonary symptoms.46 A longitudinal survey of 2239 participants showed that anxiety symptoms partially mediated the link between occasional pain and insomnia symptoms.47 However, a few studies have reported the opposite relationship between these three symptoms; that is, anxiety and insomnia are considered to be important stressors and risk factors for somatic symptoms.48 Although the results are different, current studies have shown that anxiety, insomnia and somatization are closely related, which can be explained by symptomatology and biology.48 The symptom criteria of anxiety include fatigue, muscle tension and restlessness. In contrast, the severity of somatization symptoms reflects the severity of anxiety. Pain caused by anxiety may be related to muscle tension.49 Hoehn-Saric et al reported that patients with anxiety have higher scores of physical and psychological symptoms, which is attributed to these patients being more sensitive to physical changes.50 Several previous studies have also shown that increased anxiety causes an increase in visceral allergies, blood pressure or heart rate, resulting in physical discomfort.51,52 For example, gastrointestinal discomfort may be related to the promotion of corticotropin-releasing hormone release and autonomic nervous system activity in response to anxiety and stress, which may increase colonic motility and reduce gastric peristalsis.51 Changes in heart rate or blood pressure are associated with activation of sympathetic nerves and inactivation of parasympathetic nerves under anxiety conditions.52 In addition, as mentioned above, anxiety and insomnia interact closely, so insomnia may affect physical symptoms through anxiety. Moreover, as front-line medical staff, long-term wearing of protective equipment and working in a closed environment can increase physical symptoms, such as dizziness, fatigue, nausea, chest tightness and other issues, which also increase the incidence of somatization.32 Therefore, any improvement in these symptoms is likely to improve other symptoms.48 Unlike medical staff, our study found that somatic disease is an influencing factor of public anxiety comorbid with insomnia, which was similar to a previous result revealing that somatic symptoms were highly associated with chronic diseases.53 This may be because medical workers have a special understanding that they can better distinguish between physical and psychological discomfort, an important reminder that maintaining good physical condition is beneficial to mental health.
Several limitations are worth mentioning in this survey study. First, the cross-sectional design of this study makes it difficult to explain the internal causal relationship between different mental states. Second, this survey was conducted using an online questionnaire to avoid possible infections, so the possible biases in selecting research samples should be considered. Due to network limitations, we only included participants who submitted the questionnaires. Participants who dropped out or did not complete the questionnaire had no records. Therefore, the selection of research samples may be biased. Third, all clinical symptoms were assessed not via standardized psychiatric interviews and diagnoses, but by self-assessment scales. However, in order to avoid errors to the greatest extent, we used questionnaires with good reliability and validity. Fourth, our sample size is relatively smaller than that of other studies on mental state during the COVID-19 outbreak. Fifth, subjects of this study come from online surveys and this research mainly explore the psychological state of medical staff, so it cannot be generalized to other populations. Due to the limitations of cross-sectional and web-based surveys, our results should be confirmed in a larger sample with longitudinal studies in this field to support their causal relationship.
In summary, this study was the first to compare the anxiety, insomnia symptoms and related factors between medical staff and the general public during the COVID-19 pandemic. We demonstrated that medical staff had a higher incidence of anxiety and anxiety comorbid with insomnia than nonmedical staff. Moreover, somatization and anxiety were independently associated with insomnia in anxious participants, both in medical staff and the general public. Therefore, we need to pay attention to the psychological state of high-risk occupational workers during the COVID-19 outbreak, as well as the relationship between different psychological states. In addition, medical staff should strike a balance between rest and working hours, while the general public should maintain good physical condition.
Acknowledgments
The authors thank all the participants who shared their experiences for this survey. Yuanyuan Huang and Yongjie Zhou are co-first authors for this study.
Funding
This research was supported by the National Natural Science Foundation of China (Grant No.31771074), the Science and Technology Plan Project of Guangdong Province (Grant No.2019B030316001), the Guangdong Basic and Applied Basic Research Foundation Outstanding Youth Project (2021B1515020064), and the Science and Technology Plan Project of Guangzhou (Grant No.201807010064, 201704020168, 202103000032, and 201804010259).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Gudi SK, Tiwari KK. Preparedness and lessons learned from the novel coronavirus disease. Int J Occup Environ Med. 2020;11(2):108–112. doi:10.34172/ijoem.2020.1977
2. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–37e38. doi:10.1016/S0140-6736(20)30309-3
3. Callaway E, Cyranoski D, Mallapaty S, Stoye E, Tollefson J. The coronavirus pandemic in five powerful charts. Nature. 2020;579(7800):482–483. doi:10.1038/d41586-020-00758-2
4. Craske MG, Stein MB. Anxiety. Lancet. 2016;388(10063):3048–3059. doi:10.1016/S0140-6736(16)30381-6
5. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52:102066. doi:10.1016/j.ajp.2020.102066
6. Xiang YT, Yang Y, Li W, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi:10.1016/S2215-0366(20)30046-8
7. Moradian N, Ochs HD, Sedikies C, et al. The urgent need for integrated science to fight COVID-19 pandemic and beyond. J Transl Med. 2020;18(1):205. doi:10.1186/s12967-020-02364-2
8. Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. doi:10.1016/S2215-0366(20)30047-X
9. Zhang WR, Wang K, Yin L, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 Epidemic in China. Psychother Psychosom. 2020:1–9. doi:10.1159/000507639.
10. Wu W, Zhang Y, Wang P, et al. Psychological stress of medical staffs during outbreak of COVID-19 and adjustment strategy. J Med Virol. 2020;92(10):1962–1970. doi:10.1002/jmv.25914
11. Huang Y, Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian J Psychiatr. 2020;51:102052. doi:10.1016/j.ajp.2020.102052
12. Huang Z, Zhan S, Chen C, et al. The effect of insomnia on cortical excitability in patients with generalized anxiety disorder. Front Psychiatry. 2018;9:755. doi:10.3389/fpsyt.2018.00755
13. Harvey AG. A cognitive model of insomnia. Behav Res Ther. 2002;40(8):869–893. doi:10.1016/s0005-7967(01)00061-4
14. Reddy R, Palmer CA, Jackson C, Farris SG, Alfano CA. Impact of sleep restriction versus idealized sleep on emotional experience, reactivity and regulation in healthy adolescents. J Sleep Res. 2017;26(4):516–525. doi:10.1111/jsr.12484
15. Cousins JN, Sasmita K, Chee M. Memory encoding is impaired after multiple nights of partial sleep restriction. J Sleep Res. 2018;27(1):138–145. doi:10.1111/jsr.12578
16. Bélanger L, Morin CM, Langlois F, Ladouceur R. Insomnia and generalized anxiety disorder: effects of cognitive behavior therapy for gad on insomnia symptoms. J Anxiety Disord. 2004;18(4):561–571. doi:10.1016/S0887-6185(03)00031-8
17. Ramsawh HJ, Stein MB, Belik SL, Jacobi F, Sareen J. Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. J Psychiatr Res. 2009;43(10):926–933. doi:10.1016/j.jpsychires.2009.01.009
18. Huang Y, Wang Y, Zeng L, et al. Prevalence and correlation of anxiety, insomnia and somatic symptoms in a chinese population during the COVID-19 Epidemic. Front Psychiatry. 2020;11:568329. doi:10.3389/fpsyt.2020.568329
19. Li H, Zhang Y, Wang H, et al. The relationship between symptoms of anxiety and somatic symptoms in health professionals during the coronavirus disease 2019 Pandemic. Neuropsychiatr Dis Treat. 2020;16:3153–3161. doi:10.2147/NDT.S282124
20. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi:10.1001/jamanetworkopen.2020.3976
21. Toussaint A, Hüsing P, Gumz A, et al. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7). J Affect Disord. 2020;265:395–401. doi:10.1016/j.jad.2020.01.032
22. Wei Y, Li H, Wang H, Zhang S, Sun Y. Psychological Status of Volunteers in a Phase I Clinical Trial Assessed by Symptom Checklist 90 (SCL-90) and Eysenck Personality Questionnaire (EPQ). Med Sci Monit. 2018;24:4968–4973. doi:10.12659/MSM.909524
23. Yu DS. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. 2010;66(10):2350–2359. doi:10.1111/j.1365-2648.2010.05394.x
24. Zhang YN, Jin C, Ning L, Gong S, Xiao Y, Yu GL. [Clinical characteristics and related factors of somatization symptoms in outpatients with psychiatric disorders of the department of cardiology in general hospitals]. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47(11):907–912. Chinese. doi:10.3760/cma.j.issn.0253-3758.2019.11.010
25. Kraepelien M, Svanborg C, Lallerstedt L, Sennerstam V, Lindefors N, Kaldo V. Individually tailored internet treatment in routine care: a feasibility study. Internet Interv. 2019;18:100263. doi:10.1016/j.invent.2019.100263
26. Chen X, Li P, Wang F, Ji G, Miao L, You S. Psychological results of 438 patients with persisting gastroesophageal reflux disease symptoms by symptom checklist 90-revised questionnaire. Euroasian J Hepatogastroenterol. 2017;7(2):117–121. doi:10.5005/jp-journals-10018-1230
27. Tian F, Li H, Tian S, Yang J, Shao J, Tian C. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288:112992. doi:10.1016/j.psychres.2020.112992
28. Huang Y, Wang Y, Wang H, et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. doi:10.1016/S2215-0366(18)30511-X
29. Kohlmann S, Gierk B, Hilbert A, Brähler E, Löwe B. The overlap of somatic, anxious and depressive syndromes: a population-based analysis. J Psychosom Res. 2016;90:51–56. doi:10.1016/j.jpsychores.2016.09.004
30. Liu S, Yang L, Zhang C, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–17e18. doi:10.1016/S2215-0366(20)30077-8
31. Wang C, Pan R, Wan X, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17(5). doi:10.3390/ijerph17051729
32. El-Hage W, Hingray C, Lemogne C, et al. [Health professionals facing the coronavirus disease 2019 (COVID-19) pandemic: what are the mental health risks?]. Encephale. 2020. French. doi:10.1016/j.encep.2020.04.008
33. Plaisier I, de Bruijn JG, de Graaf R, Ten Have M, Beekman AT, Penninx BW. The contribution of working conditions and social support to the onset of depressive and anxiety disorders among male and female employees. Soc Sci Med. 2007;64(2):401–410. doi:10.1016/j.socscimed.2006.09.008
34. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care. 2020;9:2048872620922795. doi:10.1177/2048872620922795
35. Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic-A review. Asian J Psychiatr. 2020;51:102119. doi:10.1016/j.ajp.2020.102119
36. Maher MJ, Rego SA, Asnis GM. Sleep disturbances in patients with post-traumatic stress disorder: epidemiology, impact and approaches to management. CNS Drugs. 2006;20(7):567–590. doi:10.2165/00023210-200620070-00003
37. Soehner AM, Harvey AG. Prevalence and functional consequences of severe insomnia symptoms in mood and anxiety disorders: results from a nationally representative sample. Sleep. 2012;35(10):1367–1375. doi:10.5665/sleep.2116
38. Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123–127. doi:10.1016/j.comppsych.2018.10.003
39. Pires GN, Bezerra AG, Tufik S, Andersen ML. Effects of acute sleep deprivation on state anxiety levels: a systematic review and meta-analysis. Sleep Med. 2016;24:109–118. doi:10.1016/j.sleep.2016.07.019
40. Cox RC, Olatunji BO. Sleep in the anxiety-related disorders: a meta-analysis of subjective and objective research. Sleep Med Rev. 2020;51:101282. doi:10.1016/j.smrv.2020.101282
41. Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep–a prefrontal amygdala disconnect. Curr Biol. 2007;17(20):R877–878. doi:10.1016/j.cub.2007.08.007
42. Wright KP
43. Tousignant OH, Taylor ND, Suvak MK, Fireman GD. Effects of Rumination and Worry on Sleep. Behav Ther. 2019;50(3):558–570. doi:10.1016/j.beth.2018.09.005
44. Cardinali DP, Srinivasan V, Brzezinski A, Brown GM. Melatonin and its analogs in insomnia and depression. J Pineal Res. 2012;52(4):365–375. doi:10.1111/j.1600-079X.2011.00962.x
45. Batterham PJ, Glozier N, Christensen H. Sleep disturbance, personality and the onset of depression and anxiety: prospective cohort study. Aust N Z J Psychiatry. 2012;46(11):1089–1098. doi:10.1177/0004867412457997
46. Bekhuis E, Boschloo L, Rosmalen JG, Schoevers RA. Differential associations of specific depressive and anxiety disorders with somatic symptoms. J Psychosom Res. 2015;78(2):116–122. doi:10.1016/j.jpsychores.2014.11.007
47. Dunietz GL, Swanson LM, Jansen EC, et al. Key insomnia symptoms and incident pain in older adults: direct and mediated pathways through depression and anxiety. Sleep. 2018;41(9). doi:10.1093/sleep/zsy125
48. Wong JY, Fong DY, Chan KK. Anxiety and insomnia as modifiable risk factors for somatic symptoms in Chinese: a general population-based study. Qual Life Res. 2015;24(10):2493–2498. doi:10.1007/s11136-015-0984-9
49. Pluess M, Conrad A, Wilhelm FH. Muscle tension in generalized anxiety disorder: a critical review of the literature. J Anxiety Disord. 2009;23(1):1–11. doi:10.1016/j.janxdis.2008.03.016
50. Hoehn-Saric R, McLeod DR, Funderburk F, Kowalski P. Somatic symptoms and physiologic responses in generalized anxiety disorder and panic disorder: an ambulatory monitor study. Arch Gen Psychiatry. 2004;61(9):913–921. doi:10.1001/archpsyc.61.9.913
51. Kreibig SD. Autonomic nervous system activity in emotion: a review. Biol Psychol. 2010;84(3):394–421. doi:10.1016/j.biopsycho.2010.03.010
52. Wilson PB. The psychobiological etiology of gastrointestinal distress in sport: a review. J Clin Gastroenterol. 2020;54(4):297–304. doi:10.1097/MCG.0000000000001308
53. Huijbregts KM, de Jong FJ, van Marwijk HW, Beekman AT, Adèr HJ, van der Feltz-cornelis CM. A high physical symptom count reduces the effectiveness of treatment for depression, independently of chronic medical conditions. J Psychosom Res. 2013;74(3):179–185. doi:10.1016/j.jpsychores.2013.01.004
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
