Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Diaphragmatic Movement at Rest and After Exertion: A Non-Invasive and Easy to Obtain Prognostic Marker in COPD
Authors Mekov E, Yanev N , Kurtelova N, Mihalova T, Tsakova A, Yamakova Y, Miravitlles M , Petkov R
Received 8 February 2022
Accepted for publication 30 April 2022
Published 5 May 2022 Volume 2022:17 Pages 1041—1050
DOI https://doi.org/10.2147/COPD.S361235
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Evgeni Mekov,1 Nikolay Yanev,2 Nedelina Kurtelova,2 Teodora Mihalova,2 Adelina Tsakova,3 Yordanka Yamakova,4 Marc Miravitlles,5 Rosen Petkov2
1Department of Occupational Diseases, Medical University Sofia, Sofia, Bulgaria; 2Department of Pulmonary Diseases, Medical University Sofia, Sofia, Bulgaria; 3Central Clinical Laboratory, Medical University Sofia, Sofia, Bulgaria; 4Department of Anesthesiology and Intensive Care, Medical University Sofia, Sofia, Bulgaria; 5Pneumology Department, Hospital Universitari Vall d´Hebron/Vall d’Hebron Institut de Recerca (VHIR), Vall d’Hebron Hospital Campus; CIBER de Enfermedades Respiratorias (CIBERES), Barcelona, Spain
Correspondence: Marc Miravitlles, Pneumology Department, Hospital Universitari Vall d´Hebron, Pg. Vall d’Hebron 119-129, Barcelona, 08035, Spain, Email [email protected]
Introduction: Diaphragmatic dysfunction is common in patients with chronic obstructive pulmonary disease (COPD). This study aimed to assess the prognostic significance of impaired diaphragmatic movement at rest and after exercise.
Methods: This was a prospective study of patients with stable COPD. Diaphragmatic movements were examined at rest and after a 6-minute walking test (6MWT) with a convex transducer with a frequency of 3.5-5-7.5 MHz. Maximal movement of the diaphragm was measured in both right and left diaphragm, and the side with higher amplitude was selected for further analysis. Measurements obtained were evaluated for their prognostic value for a composite endpoint of moderate and severe COPD exacerbations and death in 1 year time period was assessed. In addition, postbronchodilator spirometry, symptoms, quality of life, and demographic and clinical information were collected.
Results: A total of 96 patients were analyzed (62.5% male, mean age 65.1 years (standard deviation (SD): 8.1), mean FEV1 (% predicted): 55.8%, SD: 18.3%, mean CAT: 15.6 units, SD: 9.2). Sixty-four patients (67%) presented the composite endpoint. In the multivariate Cox analysis, FVC (HR = 0.944, p = 0.005), CAT score (HR = 1.133, p = 0.011), previous severe exacerbations (HR = 5.446, p = 0.004) and diaphragmatic movement at rest (HR = 0.932, p = 0.033) were found to be predictors of the composite endpoint. This model correctly classified 86.5% (83/96) of the patients.
Conclusion: Non-invasive assessment of diaphragmatic movement by ultrasound measurement both at rest and after exercise could contribute to the assessment of disease severity and prognosis of COPD.
Keywords: COPD, diaphragmatic dysfunction, comorbidities, thoracic ultrasound, exacerbations
Introduction
Patients with chronic obstructive pulmonary disease COPD have reduced exercise capacity, which is a consequence of both impaired lung function and the extrapulmonary or systemic effects of the disease.1 Airway obstruction, reduced elastic forces of the lung parenchyma, which result in an expiratory collapse of small airways with auto-positive end-expiratory pressure, high ventilatory stimulus, and shortened expiration time (tachypnea) lead to an increase in air trapping and dynamic hyperinflation of the lungs with subsequent deterioration of diaphragmatic function.
Non-invasive assessment of diaphragmatic function by ultrasound measurement of diaphragm movement may contribute to the assessment of disease severity.2,3 Few studies have examined diaphragmatic movement in COPD, with no complete description of their relationship with the course of the disease. Moreover, to the best of our knowledge, no studies have examined the change in diaphragmatic movement after exertion and its relationship with relevant COPD outcomes.
This study aimed to assess the prognostic significance of diaphragmatic movement at rest and after exercise in predicting a composite endpoint of moderate and severe COPD exacerbations or death over one year. We also analyzed the association of the diaphragmatic movement with the quality of life and the severity of the disease.
Methods
This was an observational, prospective study. Patients were recruited from an outpatient clinic of one university hospital in Bulgaria, Sofia. The primary outcome was a composite endpoint consisting of time to the first moderate or severe exacerbation or death of any cause.
Moderate exacerbation was defined as an acute increase in respiratory symptoms requiring ambulatory treatment with antibiotics and/or systemic corticosteroids. When the episode required treatment in a hospital setting or assistance in the emergency room for at least 24 hours it was considered severe.4 Frequent exacerbator was considered any patients who suffered 2 or more moderate exacerbations or at least one severe exacerbation in the previous year.5
The present study complies with the requirements of the Helsinki declaration for studies with human beings. The study was approved by the Ethics Committee of the Specialized Hospital for Active Treatment of Pulmonary Diseases “Sveta Sofia” (Sofia, Bulgaria) and all the participants provided signed informed consent and received the usual treatment schedule according to the criteria of the attending physician.
Patients over 40 years of age, current or former smokers with more than 10 pack-years of smoking and diagnosed with COPD with a postbronchodilator FEV1/FVC <0.7 were included. They had to be in a stable condition with no exacerbation at least for the previous month. Exclusion criteria were the presence of other lung diseases (cystic fibrosis, severe bronchiectasis, cancer, or restrictive lung disease), systemic inflammatory disease, and lack of compliance with the procedures (eg quality of life questionnaires, 6-minute walking test (6MWT)).
During the inclusion visit demographic characteristics, such as age and sex, and clinical characteristics of the disease – post-bronchodilator spirometry, and the number of exacerbations in the previous year were collected. Shortness of breath was assessed with the modified Medical Research Council (mMRC) dyspnea scale and quality of life with the COPD Assessment Test (CAT) questionnaire. Patients with 2 or more moderate exacerbations or 1 or more severe exacerbations (hospitalization) were considered “frequent exacerbators”.
For assessment of the inspiratory movement of the diaphragm, a convex transducer with a frequency of 3.5-5-7.5 MHz was used. Maximal movement of the diaphragm was measured at rest in both right and left diaphragm and the side with higher amplitude was selected for further analysis. Afterward, patients performed a 6MWT according to the American Thoracic Society guidelines6 and the measurement of diaphragmatic movement was repeated right after the test. The ultrasound examinations and measurements were performed by one investigator (RP) who is a certified expert in thoracic ultrasound with more than 20 years of experience. Direct measurement of the motion of the diaphragm is performed using a B-mode. Probe location on the lower intercostal spaces between anterior and posterior axillary lines allows a perpendicular ultrasound beam direction to the diaphragm movement and minimizes bowel gas interference in the left hemidiaphragm. The highest point of the cupola is marked at its highest location during maximal expiration and at its lowest location during maximal inspiration.7
Patients were followed for 12 months with clinical visits scheduled at 6 and 12 months, during which information was collected about the number and severity of exacerbations suffered during that period with a structured questionnaire. A patient was considered lost to follow-up if data could not be obtained for the one-year prospective observation time.
Statistical Analysis
An exploratory analysis was performed on the impact of diaphragmatic movement at rest and after exertion on disease parameters. All results are expressed as mean ± SD. Quantitative variables were analyzed with Student’s t-test. Qualitative variables were analyzed with frequencies and proportions. Kaplan-Meier survival analysis was used for the time to the primary endpoint. Receiver-operating characteristic (ROC) curves were used for performance evaluation of the diaphragmatic movement at rest and after 6MWT and area under the curve (AUC) were calculated. The selection of optimal cut-off points for diaphragmatic movement was done using the cutpointr package (https://cran.r-project.org/web/packages/cutpointr/vignettes/cutpointr.html) with a target to maximize the metric function “accuracy” (method = maximize_metric, metric = accuracy). The calculated cut-off value was used for dividing the groups and performing analysis for the remaining parameters. Univariate and multivariate analyses were performed for examining the predictive value of the movement. Variables with a significance <0.2 in the univariate analysis were included as independent variables. A multivariate Cox model was developed using backward stepwise logistic regression analysis. The data were analyzed with RStudio v1.4.1103.
Results
Population Characteristics
A total of 96 patients with COPD were included. The mean age was 65.1 (standard deviation (SD): 8.1) years, the mean FEV1 was 55.8% (SD: 18.3%). Table 1 summarizes the characteristics of the patients included. No patients were lost and 3 patients (3/96, 3.1%) died during the follow-up.
 |
Table 1 Patient and Disease Characteristics |
Diaphragmatic Movement
The results for maximal movement between the left and right diaphragms did not differ significantly. Mean diaphragmatic movement at rest was 48.1 mm (SD: 11.4 mm) and after 6MWT was 41.9 mm (SD:14.8 mm). The difference of 6.1 mm was significant, p <0.0001 (Figure 1). Mean diaphragmatic movement for the left diaphragm at rest was 47.6 mm (SD: 11.9 mm) and after 6MWT was 41.1 mm (SD:15.5 mm). The results will be presented only for the movement of the right diaphragm. Diaphragmatic movement correlates positively with FEV1 (Figure 2).
Diaphragmatic Movement and the Primary Endpoint
Sixty-four patients (67%) presented the composite endpoint. They were older, with worse pulmonary function and quality of life compared with those without the endpoint (Table 1).
The patients with the primary endpoint had significantly lower diaphragmatic movement at rest. The optimal cut-off points which provide the maximum accuracy were 55 mm for diaphragmatic movement at rest (accuracy 72.9%) and 53 mm after exertion. ROC curves are shown in Figure 3. Patients with diaphragmatic movement <55 mm were at increased risk for developing the primary endpoint (77.9% vs 39.3% patients, HR: 1.98, p= 0.00024, Figure 4).
 |
Figure 3 ROC curves for diaphragmatic movement at rest (left) and after 6MWT (right). |
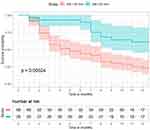 |
Figure 4 Survival curve for reaching the primary endpoint (time to exacerbation or death) stratified by diaphragmatic movement at rest (≥55 vs <55 mm). Abbreviation: DM, diaphragmatic movement. |
The diaphragmatic movement after 6MWT possesses the same accuracy (72.9%). Patients with diaphragmatic movement after 6MWT <53 mm were also at increased risk for developing the primary endpoint (75% vs 35% patients, HR: 2.14, p=0.0013) (Figure 5).
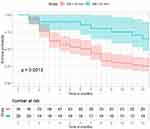 |
Figure 5 Survival curve for reaching the primary endpoint (time to exacerbation or death) stratified by diaphragmatic movement after 6MWT (≥53 vs <53 mm). Abbreviation: DM, diaphragmatic movement. |
Diaphragmatic Movement and Frequency of Exacerbations
Diaphragmatic movements at rest and after 6MWT were higher in infrequent exacerbators (50.0 ± 12.2 and 44.9 ± 15.6 mm, respectively) compared to frequent exacerbators (45.4 ± 10.1 and 37.7 ± 12.5 mm, respectively, p = 0.047 in rest and p = 0.01 after 6MWT) (Figure 6). Moreover, patients with reduced diaphragmatic movement had a higher incidence of moderate exacerbations both at rest (1.06 ± 0.93 vs 0.39 ± 0.63, p = 0.0001) and after 6MWT (0.97 ± 0.89 vs 0.45 ± 0.83, p = 0.019). In addition, patients with reduced diaphragmatic movement after 6MWT experienced more severe exacerbations (0.54 ± 0.94 vs 0.1 ± 0.31, p = 0.0009).
Diaphragmatic Movement and Symptoms
The mean CAT score was 15.6 points and the mMRC scores of 0, 1, 2, 3 and 4 had 11 (11.5%), 15 (15.6%), 28 (29.2%), 41 (42.7%) and 1 (1%) patients, respectively (Table 1). The dyspnea level was associated with diaphragmatic movement at rest and after 6MWT (Figure 7). The presence of more symptoms (CAT ≥10) was also associated with impaired diaphragmatic movement after exertion (87.3% specificity).
 |
Figure 7 Diaphragmatic movement at rest (left) and after 6MWT (right) according to mMRC group. |
Univariate and Multivariate Analysis
In the univariate analysis age, pack-years of smoking, FEV1 (% predicted), FVC (% predicted), 6MWT distance, CAT score, moderate and severe exacerbations in the previous year, and diaphragm amplitude at rest and after exertion were predictors for the primary outcome (Table 2).
 |
Table 2 Cox Multivariate Analysis to Determine Factors Associated with the Primary Outcome (Exacerbation or Death) |
In the multivariate Cox analysis, FVC, CAT score, previous severe exacerbations, and diaphragmatic movement at rest were found to be predictors of the primary outcome during follow-up (Table 2). This model correctly classified 86.5% of the patients.
Discussion
Skeletal and respiratory muscle dysfunction is considered to be a major effect influencing disease progression.8,9 Systemic inflammation, sedentary lifestyle, oxidative stress, eating disorders, heart failure, hypoxemia, and hypercapnia lead to muscle loss.10 In addition, hyperinflation causes displacement from the optimal position of the diaphragm, which reduces the movement and generated pressure during work. The long-term use of corticosteroids (even in low doses) for COPD could also contribute to respiratory muscle dysfunction, particularly of the diaphragm.11,12
One of the first ultrasound (US) studies reported mean right diaphragm movement in healthy subjects of 53 mm.13 Patients with COPD had a smaller amplitude of diaphragmatic excursions compared to the control group (36 mm versus 46 mm), depending on the distance at 6MWT.14 Corbellini et al15 showed that diaphragmatic movement during tidal breathing was higher in patients with COPD compared with healthy individuals (2.09 ± 0.8 cm versus 1.27 ± 0.3 cm), but it was lower during deep inspiration (4.75 ± 1.58 cm versus 6.93 ± 1.15 cm). On the other hand, one study reported that the diaphragm thickness, movement, and zone of apposition were significantly reduced in mild to moderate COPD but increased in severe COPD.16 The authors could not explain these results but suggested that severe airflow obstruction could lead to hypoxia with hyperventilation and subsequent increase in diaphragmatic movement.
Our study found that diaphragmatic movement at rest and after 6MWT was a significant predictor of developing an exacerbation or death. Moreover, reduced diaphragmatic movement (<53 mm) after 6MWT had 89.1% sensitivity of classifying the patients into this risk group. This could change the disease management with subsequent improvement of the clinical outcomes. Diaphragm US assessment demonstrated to be a useful prognostic marker of pulmonary rehabilitation outcomes in COPD patients.17
The relationship between diaphragmatic movement, its decrease after exercise, and FEV1 was expected and already described in relation with the dynamic hyperinflation.13,14 In addition, we have observed that exacerbations are more frequent in patients with impaired diaphragmatic function and therefore, diaphragmatic movement at rest could be used as a prognostic marker for increased risk of exacerbations or death. Although diaphragmatic movement after exertion may provide some complementary information, it was not a better predictor than diaphragmatic movement at rest, and in most cases does not justify the additional performance of a 6MWT to obtain this variable.
The present study characterizes for the first time the impact of diaphragmatic dysfunction in the course of COPD. Moreover, this is the first study to examine the change in diaphragmatic movement on exertion and its relationship to several disease parameters. Nevertheless, our study has some limitations. It should be noted that the “optimal cut-off point” was calculated based on the sample in the study. Thus, the calculated values may not be optimal in other populations; this urges subsequent studies to validate the presented results in other populations. In addition, exacerbations were self-reported by the patients during clinical visits, and this may be subjected to some recall bias; however, this bias, if it really existed, should not affect differently the two subgroups of study, and should not significantly influence the results.
Skeletal muscle dysfunction is frequent in patients with COPD18 and diaphragmatic dysfunction may be a good marker of a more generalized dysfunction that can be assessed by means of a non- invasive technique. Other authors have proposed the evaluation of muscle function by means of the computed tomography scans,19 but they produce radiation, are more expensive and their availability is reduced compared with echography. Therefore, the simple evaluation of diaphragmatic excursion at rest in COPD patients may be a simple, cheap, and safe prognostic measurement in clinical practice. It remains to be demonstrated whether it can be improved with rehabilitation of exercise20 and if this improvement may result in a reduction in the risk of future exacerbations.
Conclusions
Diaphragmatic dysfunction is common in patients with COPD. Diaphragmatic movement at rest and the drop in diaphragmatic movement after exertion show a significant relationship with the probability of exacerbation or death in a one-year follow-up. Non-invasive assessment of diaphragmatic movement by ultrasound at rest could be included in the complex assessment of disease severity.
Abbreviations
AUC, Area under the curve; CAT, COPD Assessment Test; COPD, Chronic obstructive pulmonary disease; DM, Diaphragmatic movement; FEV1, Forced expiratory volume in one second; FVC, Forced vital capacity; GOLD, Global Initiative for Obstructive Lung Disease; HR, Hazard ratio; MHz, Megahertz; IQR, Interquartile range; mMRC, Modified Medical Research Council; Q, Quartile; ROC, Receiver-operating characteristics; SD, Standard deviation; US, Ultrasound; 6MWT, Six-minute walking test.
Funding
There is no funding to report.
Disclosure
Evgeni Mekov has received grants and personal fees from Chiesi, and speaker or consulting fees from Astra Zeneca and Chiesi. Nikolay Yanev has received speaker or consulting fees from Astra Zeneca, Boehringer Ingelheim, Berlin Chemie and Chiesi. Nedelina Kurtelova has received speaker or consulting fees from Astra Zeneca, Boehringer Ingelheim, and Chiesi. Marc Miravitlles has received speaker or consulting fees from AstraZeneca, Atriva Therapeutics, Bial, Boehringer Ingelheim, Chiesi, Cipla, CSL Behring, Laboratorios Esteve, Ferrer, Gebro Pharma, GlaxoSmithKline, Grifols, Kamada, Menarini, Mereo Biopharma, Novartis, ONO Pharma, Palobiofarma SL, pH Pharma, Rovi, Sanofi, Sandoz, Spin Therapeutics, Takeda, TEVA, Verona Pharma and Zambon, and research grants from Grifols. Rosen Petkov has received speaker or consulting fees from Astra Zeneca and Boehringer Ingelheim. The authors report no other conflicts of interest in this work.
References
1. Mekov E, Slavova Y. Diabetes mellitus and metabolic syndrome in COPD – part 3: consequences. Thorac Med. 2014;6(4):23–36.
2. Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by M-mode ultrasonography: methods, reproducibility, and normal values. Chest. 2009;135(2):391–400. doi:10.1378/chest.08-1541
3. Testa A, Soldati G, Giannuzzi R, et al. Ultrasound M-mode assessment of diaphragmatic kinetics by anterior transverse scanning in healthy subjects. Ultrasound Med Biol. 2011;37(1):44–52. doi:10.1016/j.ultrasmedbio.2010.10.004
4. Wedzicha JA, Miravitlles M, Hurst JR, et al. Management of COPD exacerbations: an European Respiratory Society/American Thoracic Society (ERS/ATS) guideline. Eur Respir J. 2017;49:1600791. doi:10.1183/13993003.00791-2016
5. Miravitlles M, Calle M, Molina J, et al. Spanish COPD guidelines (GesEPOC) 2021: updated pharmacological treatment of stable COPD. Arch Bronconeumol. 2022;58:68–91. doi:10.1016/j.arbres.2021.03.026
6. American Thoracic Society. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi:10.1164/ajrccm.166.1.at1102
7. Haji K, Royse A, Tharmaraj D, Haji D, Botha J, Royse C. Diaphragmatic regional displacement assessed by ultrasound and correlated to subphrenic organ movement in the critically ill patients-an observational study. J Crit Care. 2015;30(2):
8. Agusti A, Soriano JB. COPD as a systemic disease. COPD. 2008;5:133–138. doi:10.1080/15412550801941349
9. Kim HC, Mofarrahi M, Hussain SN. Skeletal muscle dysfunction in patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2008;3:637–658. doi:10.2147/COPD.S4480
10. Decramer M, De Benedetto F, Del Ponte A, Marinari S. Systemic effects of COPD. Respir Med. 2005;99(suppl B):S3–S10. doi:10.1016/j.rmed.2005.09.010
11. Decramer M, Lacquet LM, Fagard R, Rogiers P. Corticosteroids contribute to muscle weakness in chronic airflow obstruction. Am J Respir Crit Care Med. 1994;150:11–16. doi:10.1164/ajrccm.150.1.8025735
12. Koerts-de Lang E, Schols AM, Rooyackers OE, Gayan-Ramirez G, Decramer M, Wouters EF. Different effects of corticosteroid-induced muscle wasting compared with undernutrition on rat diaphragm energy metabolism. Eur J Appl Physiol. 2000;82(5–6):493–498. doi:10.1007/s004210000231
13. Houston JG, Morris AD, Howie CA, Reid JL, McMillan N. Technical report: quantitative assessment of diaphragmatic movement–a reproducible method using ultrasound. Clin Radiol. 1992;46(6):405–407. doi:10.1016/S0009-9260(05)80688-9
14. Paulin E, Yamaguti WP, Chammas MC, et al. Influence of diaphragmatic mobility on exercise tolerance and dyspnea in patients with COPD. Respir Med. 2007;101(10):2113–2118. doi:10.1016/j.rmed.2007.05.024
15. Corbellini C, Boussuges A, Villafañe JH, Zocchi L. Diaphragmatic mobility loss in subjects with moderate to very severe COPD may improve after in-patient pulmonary rehabilitation. Respir Care. 2018;63(10):1271–1280. doi:10.4187/respcare.06101
16. Jain S, Nair G, Nuchin A, Uppe A. Study of the diaphragm in chronic obstructive pulmonary disease using ultrasonography. Lung India. 2019;36(4):299–303. doi:10.4103/lungindia.lungindia_466_18
17. Crimi C, Heffler E, Augelletti T, et al. Utility of ultrasound assessment of diaphragmatic function before and after pulmonary rehabilitation in COPD patients. Int J Chron Obstruct Pulmon Dis. 2018;13:3131–3139. doi:10.2147/COPD.S171134
18. Cruthirds CL, van der Meij BS, Wierzchowska-McNew A, Deutz NEP, Engelen MPKJ. Presence or absence of skeletal muscle dysfunction in Chronic Obstructive Pulmonary Disease is associated with distinct phenotypes. Arch Bronconeumol. 2021;57(4):264–272. doi:10.1016/j.arbres.2019.12.034
19. Ezpondra A, Casanova C, Cabrera C, et al. Psoas muscle density evaluated by chest CT and long-term mortality in COPD patients. Arch Bronconeumol. 2021;57:533–539.
20. Galdiz JB, Gómez A, Rodriguez D, et al. Telerehabilitation programme as a maintenance strategy for COPD patients: a 12-month randomized clinical trial. Arch Bronconeumol. 2021;57(3):195–204. doi:10.1016/j.arbres.2020.03.034
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



