Back to Journals » Breast Cancer: Targets and Therapy » Volume 15
Diagnostic Value of a Combined Serum α-Hydroxybutyrate Dehydrogenase, Carcinoembryonic Antigen and Glycoantigen 125 Test for Early-Stage Breast Cancer
Received 14 March 2023
Accepted for publication 27 July 2023
Published 15 August 2023 Volume 2023:15 Pages 617—623
DOI https://doi.org/10.2147/BCTT.S410500
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Pranela Rameshwar
Chuan-Hua Zhan,1 Guo-Jun Liu2
1Department of Clinical Laboratory, Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University, Huangshi, People’s Republic of China; 2Department of Breast Cancer Surgery, Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University, Huangshi, People’s Republic of China
Correspondence: Guo-Jun Liu, Department of Breast Cancer Surgery, Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University, No. 141, Tianjin Road, Huangshi, Hubei, 435000, People’s Republic of China, Tel +86 714 6323922, Email [email protected]
Objective: To investigate the diagnostic value of the combined detection of α-hydroxybutyrate dehydrogenase (α-HBDH), carcinoembryonic antigen (CEA) and cancer antigen 125 (CA125) in early-stage breast cancer (ESBC).
Methods: This was a retrospective analysis of 169 patients with ESBC, 138 patients with benign breast disease (BBD) and 200 normal healthy controls (NHCs). The levels of serum α-HBDH, CEA and CA125 in the two groups were detected. The receiver operating characteristic (ROC) curve and area under the curve (AUC) were used to analyse the diagnostic value of the above indicators alone and in combination for ESBC.
Results: The levels of α-HBDH, CEA and CA125 in the ESBC group were significantly higher than those in the BBD and NHC groups ([118.18 ± 11.19 vs 91.24 ± 9.17 vs 89.38 ± 9.01, F = 6.189, p = 0.004], [2.39 ± 1.12 vs 1.48 ± 0.76 vs 1.58 ± 0.58, F = 5.362, p = 0.017] and [14.44 ± 6.78 vs 11.19 ± 3.17 vs 7.18 ± 4.71, F = 8.912, p = 0.001], respectively). In the ESBC group, the positive rate of combined detection was higher than that of single detection (96.12% vs 72.64% vs 53.67% vs 42.41%, X2 = 27.174, p < 0.05). ROC curve analysis showed that serum α-HBDH, CEA, CA125 alone and combined detection in the diagnosis of ESBC. The sensitivity was 48.1%, 63.6%, 44.2% and 54.5%, the specificity was 75.4%, 75.4%, 86.0% and 91.2% and the AUC was 0.654, 0.715, 0.636 and 0.772, respectively. The diagnostic value of combined detection was the highest.
Conclusion: The levels of serum α-HBDH, CEA and CA125 in ESBC are high, and the combined detection of the three has a high diagnostic value for ESBC.
Keywords: breast cancer, α-hydroxybutyrate dehydrogenase, CA125, carcinoembryonic antigen, diagnosis
Introduction
Breast cancer is the most widespread malignant tumour that seriously threatens the health of women worldwide. In 2021, the World Health Organization’s International Agency for Research on Cancer released the global cancer burden data for 2020. There were 2.26 million new cases of breast cancer worldwide, exceeding the 2.2 million cases of lung cancer and making it the world’s most common cancer.1 In 2022, breast cancer accounted for 429,105 new cancer cases in China, showing a clear upward trend, and the number of cancer deaths in China was 124,002, indicating that the growth rate of breast cancer has significantly accelerated, posing a serious threat to the health of residents.2 Approximately 10–15% of patients with breast cancer also have other serious diseases or distant metastasis for 3 years or more after the first diagnosis. Distant tissue and organ metastasis is closely related to the treatment and prognosis of patients with breast cancer and is their main cause of death.
Because the 5-year survival rate of patients with stage I breast cancer is almost 100%,2 the early diagnosis of breast cancer is particularly important. Imaging examination is the main method of detecting breast cancer; however, there are some problems with this technique, such as the high cost of equipment and instruments, potential radiation, operator experience, professional interpretation of the results and a high false positive rate.3 Therefore, blood markers that can be quickly detected, are economically practical, highly specific, easily interpreted and minimally invasive have the potential to be used as auxiliary imaging examinations to detect breast cancer more effectively.
Carcinoembryonic antigen (CEA) and cancer antigen 125 (CA125) are extensively used serum tumour markers for monitoring the occurrence, development and therapeutic effects of carcinoma.4 A recent cohort study of 10,836 Chinese patients with breast cancer revealed a negative correlation between preoperative CA153 and CEA expression on survival and tumour progression.5 Lactate dehydrogenase (LDH) is a glycolytic enzyme that converts pyruvate into lactic acid. The growth, invasion and metastasis of cancer cells require of cancer cells. Lactate dehydrogenase is elevated in many malignant tumours. Serum LDH levels can be used as a prognostic indicator of breast cancer,4–6 and α-hydroxybutyrate dehydrogenase (α-HBDH) is an isoenzyme of LDH that reflects the overall level of LDH1 and LDH2 in vivo. Relevant studies have reported that serum α-HBDH levels are significantly increased in patients with malignant tumours such as leukaemia, lymphoma and ovarian cancer, and the prognosis of patients with malignant tumours with different α-HBDH levels is also different.7,8 However, there are few studies on the relationship between breast cancer and α-HBDH in clinical practice. To further improve the diagnosis rate of early-stage breast cancer (ESBC), this study explored the diagnostic value of the combined detection of α-HBDH, CEA and CA125 in ESBC.
Materials and Methods
Study Participants
The convenience sampling method was used to retrospectively identify patients with ESBC, those with benign breast disease (BBD) and normal healthy controls (NHCs) who had been diagnosed and treated in the hospital between January 2020 and December 2022. The inclusion criteria were (1) breast cancer patients diagnosed by puncture or surgery and pathological examination and (2) patients with benign breast lesions diagnosed as BBD by puncture or surgery and pathological examination. The exclusion criteria were (1) patients with breast cancer in pathological stages III and IV, (2) patients with other malignant tumours or malignant tumour histories, (3) patients with extensive tumour metastasis not suitable for surgery, (4) patients with coagulation dysfunction or a history of thrombotic diseases, (5) patients with serious heart, liver, kidney and other vital organ diseases and (6) patients with acute infection, blood disease, high fever and other signs before operation. This study was approved by the Hospital Medical Ethics Committee [(2022) -15]. This was a retrospective study and was exempt from the signing of informed consent.
Test Method
Patients with ESBC and patients with benign breast lesions were tested before treatment. Healthy participants were tested on the day of physical examination. After fasting, a 2–3 mL venous blood sample was extracted from members of each group in the morning and centrifuged within 1 h (centrifuged for 10 mins at 3000 revs/min). All laboratory tests, including blood collection, handling and quantitative analysis, were performed in accordance with standard operating procedures. The serum levels of α-HBDH, CEA and CA125 were detected by electrochemiluminescence immunoassay in serum using an automatic Roche Cobas E602 analyser (Roche Diagnostics, IN, United States). Quantitative analysis of the markers with enzyme-linked immunosorbent assay (ELISA) was performed by following the manufacturer’s instructions. The ELISA kits used were the α-HBDH ELISA Kit (Thermo Fisher, MA, United States), CEA Human ELISA Kit (Thermo Fisher) and CA125 Human ELISA Kit (Thermo Fisher). The normal reference values of α-HBDH, CEA and CA125 are 71–182 U/L, 0–5 ng/mL and 0–35 U/mL, respectively. If any index in the combined detection is positive, the result is judged as positive.
Statistical Methods
The SPSS 19.0 software package was used for statistical analysis of the data. The measurement data conforming to a normal distribution and homogeneity of variance were expressed as mean ± standard deviation. Analysis of variance was used for comparison between groups, and the least significant difference test was used for pairwise comparisons. Measurement data with a non-normal distribution were expressed as a median and interquartile range (M[P25, P75]), and the Wilcoxon rank sum test was used for comparison between groups. The count data were expressed as the number of cases and rate (%), and the X2 test was used for comparison between groups. A receiver operating characteristic (ROC) curve was drawn, and the area under the curve (AUC) was used to evaluate the diagnostic value of single and combined detection of α-HBDH, CEA and CA125 in breast cancer. A value of p < 0.05 was considered statistically significant.
Results
Basic Information and Characteristics
The study included a total of 169 patients with ESBC aged 29–76 years, with an average age of 52.08 ± 7.34 years. According to the American Joint Committee on Cancer (Eighth Edition) tumour–node–metastasis (TNM) staging system, these patients were in the early stages of pathological TNM staging, including TNM 0, IA, IB, IIA and IIB. The 169 patients included 31 with carcinoma in situ (TNM stage 0) and 138 with invasive carcinoma.
The control group included 138 patients with BBD and 200 NHCs. A total of 138 patients with BBD were treated in the hospital, including 118 with breast fibroadenoma and breast adenosis and 20 with breast hyperplasia (see Figure 1). An NHC is an individual with a regular physical examination and no abnormal laboratory and imaging results. There was no significant difference in age, height or body mass index among the three groups (p > 0.05) (see Table 1).
 |
Table 1 Comparison of Serum α-HBDH, CEA and CA125 Levels in Three Groups of Patients |
 |
Figure 1 A detailed figure of samples. |
Comparison of Serum α-HBDH, CEA and CA125 Levels
The levels of α-HBDH, CEA and CA125 in the ESBC group were significantly higher than those in the BBD and NHC groups ([118.18 ± 11.19 vs 91.24 ± 9.17 vs 89.38 ± 9.01, F = 6.189, p = 0.004], [1.99 ± 1.12 vs 1.28 ± 0.76 vs 1.38 ± 0.58, F = 3.362, p = 0.047] and [14.44 ± 6.78 vs 11.19 ± 3.17 vs 7.18 ± 4.71, F = 8.912, p = 0.001], respectively). The level of CA125 in the BBD group was higher than that in the NHC group (11.19 ± 3.17 vs 7.18 ± 4.71, p < 0.05) (see Table 1).
Comparison of Positive Rates of Single and Combined Detection of Various Indicators Between Groups
The positive rates of single and combined detection of each index in the ESBC group were significantly higher than those in the BBD and NHC groups, and the differences were statistically significant (p < 0.05). In the ESBC group, the positive rate of combined detection was higher than that of single detection (96.12% vs 72.64% vs 53.67% vs 42.41%, X2 = 27.174, p < 0.05). In the ESBC group, the positive rate of α-HBDH was significantly higher than that of CEA and CA125 (p < 0.05) (see Table 2).
 |
Table 2 Comparison of Positive Rates of Single and Combined Detection of Various Indicators Between Groups |
Diagnostic Value of Single and Combined Detection of Serum α-HBDH, CEA and CA125 in Early-stage Breast Cancer
The results revealed that the sensitivity of serum α-HBDH, CEA and CA125 alone and combined detection in the diagnosis of ESBC was 48.1%, 63.6%, 44.2% and 54.5%, respectively, and the specificity was 75.4%, 75.4%, 86.0% and 91.2%, respectively. The AUC were 0.654 (95% confidence interval [CI]: 0.560–0.747), 0.715 (95% CI: 0.629–0.801), 0.636 (95% CI: 0.542–0.729) and 0.772 (95% CI: 0.695–0.849), respectively. The diagnostic value of combined detection was the highest (see Figure 2).
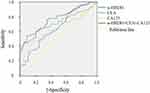 |
Figure 2 ROC curve of serum α-HBDH, CEA, CA125 alone and combined detection in the diagnosis of early breast cancer. |
Discussion
The stage of breast cancer at the time of diagnosis is closely related to the long-term survival of patients. There is still a lack of simple, effective molecular markers that allow the clinical detection of patients with ESBC, either alone or with auxiliary imaging diagnostic applications. Because blood samples are easy to obtain, it is wise to continue to explore new blood biomarkers.9
Lactate dehydrogenase is a key enzyme of glucose metabolism. It is involved in the energy metabolism of tumour cells and is highly expressed in breast cancer.10 As it is an isoenzyme of LDH, α-HBDH is closely related to the metabolism of LDH and plays a key role in a variety of malignant tumours.11 Tumour tissue metabolism is disordered, and α-HBDH and LDH also enter the patient’s circulatory system with the metabolism of the body. α-HBDH can be used as a tumour-related index to evaluate the progression of patients with breast cancer and provide a reference for the early screening, diagnosis, treatment and prognosis evaluation of breast cancer. The results of this study revealed that the serum α-HBDH level in patients with ESBC was significantly higher than that of patients in the BBD and NHC groups. The positive rate of α-HBDH in the ESBC group was significantly higher than that of CEA and CA125, indicating that the serum α-HBDH level can be used for the early diagnosis of breast cancer.
The antigenic proteins produced by breast cancer during metabolism in vivo can be used as serum markers in clinical practice. At present, breast cancer-related tumour markers include CEA, CA125 and CA153.12 Carcinoembryonic antigen is a carbohydrate–protein formed during the growth of malignant tumours. In healthy people, CEA is expressed at a low concentration on the surface of the tissue. When malignant tumours occur in the body, the tumour tissue will highly express CEA; therefore, CEA can be used as a tumour marker. CA125 is a glycoprotein detected by the epithelial ovarian cancer antigen, which does not exist in normal ovarian tissue. It is common in epithelial ovarian cancer and has a high diagnostic sensitivity. Some studies have confirmed that the detection of CA125 level is helpful for the differential diagnosis of breast cancer.13 In the process of breast cancer recurrence and metastasis, the serum CA125 level is higher, and there is an upward trend. However, the limitation of CA125 detection is poor specificity. CA125 levels are higher in patients with endometrial cancer, fallopian tube adenocarcinoma, breast cancer, cervical cancer, pancreatic cancer, colorectal cancer and lung cancer.14 CA153 has high specificity in the detection of breast cancer. It is a specific tumour marker for breast cancer and has a significant effect on the dynamic detection of recurrence after treatment in patients with stage II and III breast cancer.15 Breast cancer is often accompanied by elevated CA153 levels, but the sensitivity is low in the early stages of the disease. Therefore, this study did not select this indicator.
The ROC curve can be used to evaluate the diagnostic efficacy and help to find the best diagnostic markers,16 and the curve drawn in this study demonstrated that serum α-HBDH, CEA and CA125 were independently detected and diagnosed. Thus, the combined detection of three indicators has a higher diagnostic efficacy for ESBC. It shows that the diagnostic effect of α-HBDH combined with CEA and CA125 is more effective, which can make up for the lack of sensitivity and specificity of a single marker.
This study has some limitations. Because it was a retrospective case-control study and the blood samples were obtained from a single centre, the results were easily affected by the selection bias of the study participants. At the same time, the sample size was not large enough, and there were no in-depth molecular functional mechanism experiments to verify the role of the target molecule in breast cancer. Therefore, in the future, we should make greater efforts, especially in the research design, to prospectively include a multi-centre design with a larger sample size to promote the diagnostic performance of the validated factors in the general population and further study the biological function of their corresponding proteins. In subsequent studies, more tumour markers and more parameters will be included to predict the classification and prognosis of breast cancer.
Conclusion
In summary, serum α-HBDH levels are higher in patients with ESBC. The combined detection of α-HBDH, CEA and CA125 showed the highest sensitivity for the diagnosis of breast cancer. These results can improve diagnostic efficiency and provide a reference for the diagnosis of ESBC.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the declaration of Helsinki. This study was approved by the Medical Ethics Committee of Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University. This clinical study is a retrospective study that only collects patient clinical data and does not interfere with the patient’s treatment plan. It does not pose any physiological risks to the patient. Patient’s privacy will be respected in accordance with the Declaration of Helsinki.
Consent for Publication
The manuscript is not submitted for publication or consideration elsewhere.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any funding support.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Xia C, Dong X, Li H, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J. 2022;135(5):584–590. doi:10.1097/CM9.0000000000002108
3. Jafari SH, Saadatpour Z, Salmaninejad A, et al. Breast cancer diagnosis: imaging techniques and biochemical markers. J Cell Physiol. 2018;233(7):5200–5213. doi:10.1002/jcp.26379
4. Sauerbrei W, Taube SE, McShane LM, et al. Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK): an abridged explanation and elaboration. J Natl Cancer Inst. 2018;110(8):803–811. doi:10.1093/jnci/djy088
5. Li J, Liu L, Feng Z, et al. Tumor markers CA15-3, CA125, CEA and breast cancer survival by molecular subtype: a cohort study. Breast Cancer. 2020;27(4):621–630. doi:10.1007/s12282-020-01058-3
6. Chen B, Dai D, Tang H, et al. Pre-treatment serum alkaline phosphatase and lactate dehydrogenase as prognostic factors in triple negative breast cancer. J Cancer. 2016;7(15):2309–2316. doi:10.7150/jca.16622
7. Bai Y, Zhu B, Zhu Y, Ma Y, Zhang J. Exploration on the application value of the expression level of alpha-hydroxybutyrate dehydrogenase in the diagnosis of ovarian cancer. Chin J Lab Med. 2019;42(7):529–534. doi:10.3760/cma.j.issn.1009-9158.2019.07.007
8. Wu J, Fu N. Detection level and clinical significance of serum α-hydroxybutyrate dehydrogenase in patients with bladder cancer. J Logist Univ CAPF. 2020;29(8):7–11.
9. Li J, Guan X, Fan Z, et al. Non-invasive biomarkers for early detection of breast cancer. Cancers. 2020;12(10):2767. doi:10.3390/cancers12102767
10. Becker LM, O’Connell JT, Vo AP, et al. Epigenetic reprogramming of cancer-associated fibroblasts deregulates glucose metabolism and facilitates progression of breast cancer. Cell Rep. 2020;31(9):107701. doi:10.1016/j.celrep.2020.107701
11. Nakamura T, Asanuma K, Hagi T, Sudo A. Is serum lactate dehydrogenase useful for predicting oncological outcome in patients with soft tissue sarcoma? Anticancer Res. 2019;39(12):6871–6875. doi:10.21873/anticanres.13905
12. Das V, Kalita J, Pal M. Predictive and prognostic biomarkers in colorectal cancer: a systematic review of recent advances and challenges. Biomed Pharmacother. 2017;87:8–19. doi:10.1016/j.biopha.2016.12.064
13. Wang H, Cai D, Luan Y, Luo X, Duan Z. Value of CEA, CA125, CA153 and CYFRA211 in diagnosis of triple negative breast cancer. J Trop Med. 2019;19(9):1082–1085. doi:10.3969/j.issn.1672-3619.2019.09.005
14. Yang W. The value of serum CA15-3, CA125 combined with MMP-1 and IL-10 in the diagnosis and prognosis evaluation of breast cancer. Label Immunoassays Clin Med. 2018;25(8):1107–1113. doi:10.11748/bjmy.issn.1006-1703.2018.08.006
15. Wang Q, Zhou Q, Qu Y. The clinical significance of combined detection of serum tumor markers CA153, CA125 and CEA in the diagnosis of breast cancer. Chin J Control Endem Dis. 2018;33(4):452.
16. Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010;5(9):1315–1316. doi:10.1097/JTO.0b013e3181ec173d
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
