Back to Journals » Infection and Drug Resistance » Volume 16
Diagnostic Performance of Metagenomic Next⁃Generation Sequencing in the Diagnosis of Prosthetic Joint Infection Using Tissue Specimens
Authors Yu Y, Wang S, Dong G, Niu Y
Received 18 November 2022
Accepted for publication 21 February 2023
Published 28 February 2023 Volume 2023:16 Pages 1193—1201
DOI https://doi.org/10.2147/IDR.S397260
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Yali Yu,1,* Shaohua Wang,2,* Guixiang Dong,1 Yanli Niu3
1Department of Clinical Laboratory, Zhengzhou Orthopaedics Hospital, Zhengzhou, People’s Republic of China; 2Department of Joint Surgery, Zhengzhou Orthopaedics Hospital, Zhengzhou, People’s Republic of China; 3Laboratory of Cell Signal Transduction, School of Basic Medical Sciences, Henan University, Kaifeng, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanli Niu, Laboratory of Cell Signal Transduction, School of Basic Medical Sciences, Henan University, Kaifeng, People’s Republic of China, Email [email protected]
Purpose: The purpose of this study was to evaluate the ability of metagenomic next-generation sequencing (mNGS) diagnosing prosthetic joint infection (PJI) using tissue from hip/knee rapidly and precisely, especially in patients who had received antibiotic treatment within the preceding two weeks.
Methods: From May 2020 to March 2022, 52 cases with suspected PJI were enrolled. mNGS was performed on surgical tissue samples. The sensitivity and specificity of mNGS in diagnosis was evaluated using culture in conjunction with MSIS criteria. This study also looked at how antibiotic use affected culture and mNGS efficacy.
Results: According to MSIS criteria, 31 of the 44 cases had PJI, and 13 were classified in the aseptic loosening group. Sensitivity, specificity, positive/negative predictive value (PPV/NPV), positive/negative likelihood ratio (PLR/NLR), and area under the curve (AUC) of mNGS assay were 80.6% (71.9– 91.8%), 84.6 (73.7– 97.9%), 92.6 (84.2– 98.7%), 64.7 (58.6– 74.7%), 5.241 (4.081– 6.693), 0.229 (0.108– 0.482) and 0.826 (0.786– 0.967), respectively, with MSIS as a reference. When MSIS was used as a reference, the results of culture assay were 45.2% (40.8– 51.5%), 100 (100.0– 100.0%), 100 (100.0– 100.0%), 43.3 (39.1– 49.5%), +∞, 0.548 (0.396– 0.617) and 0.726 (0.621– 0.864), respectively. The AUC values for mNGS and culture were 0.826 and 0.731, respectively, and the differences were insignificant. mNGS demonstrated higher sensitivity than culture in PJI subjects who had previously received antibiotic treatment within 2 weeks (69.5% vs 23.1%, P = 0.03).
Conclusion: In our series, mNGS yield a higher sensitivity for diagnosis and pathogen detection of PJI compared to microbiological culture. Additionally, mNGS is less affected by prior antibiotic exposure.
Keywords: prosthetic joint infection, metagenomic next⁃generation sequencing MSIS criteria, antibiotic treatment
Introduction
PJI is the most common fatal complication after joint arthroplasty, with mean 1-year prevalence rates of 0.25–1.0% and 0.4–2% for primary THR and TKR, respectively1,2 and rates of up to 15% in revision surgeries.3,4 PJI has imposed enormous costs on patients and the global medical industry.5 Every year, the incidence of PJI rises as more primary and revision arthroplasty operations are performed worldwide.6,7
A good prognosis requires prompt detection and identification of harmful microorganisms. Early and timely diagnosis of PJI and identification of pathogenic microorganisms remain the key to successful treatment. Because identifying pathogenic bacteria can not only select effective antibiotics for specific pathogenic microorganisms, but also play a crucial role in the selection of treatment plan.8,9 Although various biochemical indications and clinical signs can be used to diagnose PJI, reliably identifying pathogenic microorganisms remains a significant difficulty. Traditional microbial culture has clear flaws, such as a high false negative rate.10,11 About 40% of PJI cases still have negative culture results using synovial fluid and tissue samples,12,13 which may be due to inappropriate culture conditions for particular microorganisms and widespread antibiotic use. Existing pathogenic microorganism diagnostic techniques are largely based on polymerase chain reaction (PCR), including multiplex PCR and 16S rRNA gene PCR.14,15 However, it has limitations, such as limited detection of species of pathogenic microorganisms and low resolution for multiple infections.16,17 Therefore, it is important to seek new diagnostic tools to accurately and precisely identify and treat PJI. It also termed massively parallel sequencing, that allows for thousands to billions of DNA sequences to be simultaneously sequenced.
In recent years, metagenomic next-generation sequencing (mNGS) has been a rapidly developing diagnostic tool for pathogenic microorganisms.18,19 mNGS, also known as massively parallel sequencing, allow thousands to billions of DNA sequences to be sequenced simultaneously, identifying all nucleic acid sequences in a sample and searching them in a dedicated database of pathogenic microbes. Unlike multiplex polymerase chain reaction (PCR), primer extension, or bait probe enrichment methods, mNGS have high throughput, are independent of pre-detection, and have detection efficacy against practically all pathogenic microorganisms such as fungi, bacteria, parasites, and viruses. It is crucial in diagnosing genetic disorders, infectious diseases, and malignant tumors.20,21 It has been shown that mNGS is extremely accurate in diagnosing PJI; Many articles have performed mNGS using articular fluid or implant sonicate,22,23 whereas just a few used tissues. Results of mNGS from different sample types of the same disease may differ.24,30 For example, Miao et al observed a higher positivity in BALF than that in sputum for NTM but not MTB, Aspergillus, or Cryptococcus.30 Thus, the goals of this study were to (1) determine whether the mNGS assay was accurate in detecting PJI with tissues and (2) determine how antibiotic administration influenced culture and mNGS efficacy.
Materials and Methods
Study Design, Patient Inclusion, and Exclusion Criteria
We conducted this prospective cohort study at our facility. The Board Review Committee of Zhengzhou Orthopaedics Hospital approved our study protocols. Each partaker provided informed consent for participation. From May 2020 to March 2022, all surgically treated cases with primary knee or hip joint PJIs were included in the study. The diagnosis of PJI was made at our facility following the Musculoskeletal Infection Society (MSIS) diagnostic criteria.25 All cases were classified into two groups based on the MSIS diagnostic criteria: PJI and non-PJI.
Exclusion criteria were as follows: (1) all patients who refused to provide tissue for NGS evaluation; (2) all patients who underwent joint replacement after resection of bone tumors or patients with rheumatoid arthritis; (3) all patients who did not receive histology or had unclear outcomes; and (4) all patients who did not follow-up (<1 month). (5) patients whose sample sequencing failed. The inability to adequately execute comprehensive sequencing analysis due to poor DNA extraction and sequencing library formation was called sequencing failure.
Data Source and Collection
The electronic medical record system was used to collect all cases’ demographic data, clinical information, and test results.
Sample Collection
Before surgery, one clinical practitioner took a rigorously sterile aspiration of synovial fluid from a probably affected joint. Synovial fluid was collected before the surgical joint capsule incision for individuals with preoperative puncture failure.
Tissue sampling around the prosthesis: Immediately after joint opening, “fresh” instruments were used to extract tissues from 3 different sites around the hip/knee (inflammatory sites), which was then placed in the sterile sample containers and sent for NGS and culture.
Smear and Cultures
Intraoperative periprosthetic tissue samples were homogenized for 1 min with BHI broth (3 mL) using a homogenizer (JXFSTPRP-24L, JingXin, China) under aseptic conditions. The Gram and Ziehl-Neelsen method was used to stain treated sample sediments and examined at 100x magnification. Tissue homogenate (0.1 mL) was inoculated onto Columbia blood agar supplemented with chocolate agar and 5% sheep blood for 7 days at 35 °C, aerobic and anaerobic conditions. Another 1 mL homogenate was subjected to 14-day incubation in BD BACTEC aerobic/anaerobic/fungal and acid-fast bacilli bottles.
Following established laboratory procedures, isolated bacteria were tested for the antibiotic susceptibility of positive culture using the Phoenix 100 (BD) automated system.
Metagenomic Next-Generation Sequencing (mNGS)
The intraoperatively obtained tissue was sliced into pieces before being shipped to the laboratory for mNGS. The initial step was to isolate total tissue DNA using the TIANamp Micro DNA Kit (DP316, TIANGEN BIOTECH). After that, Qubit 2.0 (Invitrogen, USA) was used to quantify DNA content, and 200 ng was used in the following step. The second step was to create and identify a DNA library. Initially, DNA fragmentation, end-repair adaption, dA-tailing addition, adapter ligation and PCR amplification were used to create a DNA library. The Agilent 2100 Bioanalyzer (Agilent Technologies, Canada) and qPCR were used to identify the DNA library. To manufacture DNA nanospheres for NGS, the library was cyclized to form a single-stranded ring structure and then rolled to replicate.
After loading on the chip, samples were sequenced at 20 M 50 bp using the BGISEQ-50 platform (BGI Genomics Co., Ltd.). Low quality, adaptor contamination, repeat sequence number, and short (<35 bp) reads were eliminated to obtain high-quality sequencing data. Human reference genome (hg19)-mapped human host sequences were afterward computationally subtracted using the Burrows-Wheeler alignment technique. Meanwhile, the remaining data were classified using simultaneous alignment against four NCBI Microbial Genome Databases (ftp://ftp.ncbi.nlm.nih.gov/genomes/), including bacteria, viruses, fungi, and parasites. They covered 6350 bacterial genomes/scaffolds, 1798 whole genome sequences, 1064 human infection-associated fungi, and 234 human disease-related parasites.
Statistical Analysis
SPSS17.0 was used in this study to analyze sensitivity, specificity, positive/negative predictive value (PPV/NPV), AUC, likelihood ratio (LR), and related 95% confidence intervals (CIs) in culture and NGS techniques. Basic characteristics were displayed using descriptive statistics. To compare continuous data in both groups, the nonparametric Mann–Whitney U-test or t-test was used, while the chi-square test was used to analyze categorical variables. The McNemar test was used to compare both approaches. P < 0.05 stood for statistical significance.
Results
General Characteristics and Comorbidities of Patients
This study included 52 cases with clinically suspected PJI, 5 of which were excluded according to our exclusion criteria. Synovial fluid was obtained from 3 patients, and among the 44 cases in which biopsies were taken for investigation. Among these cases, 31 (70.5%) were confirmed with PJI, and 13 (29.5%) were non-PJI cases based on MSIS criteria. There were 21 (47.7%) males and 23 (52.3%) females. The average ages of patients in the PJI and non-PJI groups were 66.4±6.7 and 67.3±8.2, respectively, and the PJI group had significantly higher ESR levels [41.5±18.2 mm/h] than the non-PJI group [14.4±6.1 mm/h)] (P = 0.00). The difference in CRP levels between the two groups was not statistically significant [22.1±53.1 mg/L vs 17.2 13.8±2.5 mg/L, P = 0.08]. PCT levels in the PJI group were 1.3 ±0.7 ng/mL, significantly higher than in the non-PJI group [0.2±0.1 ng/mL, P = 0.00]. D-dimer levels did not differ substantially between groups [1.6±0.2 mg/L vs 1.4±0.1 mg/L, P = 0.41]. Figure 1 and Table 1 show our enrolled cases’ demographic and clinical features.
 |
Table 1 Demographic Characteristics of Patients |
 |
Figure 1 Flowchart of patient inclusion. |
Periprosthetic Tissue Microbial Culture and mNGS Results
Our enrolled cases yielded two positive findings from the culture with the same organism. Microbiological culture detected 9 types of bacteria, while mNGS detected 15 types of bacteria and 2 types of fungi. There were 13 patients with positive mNGS and culture results, including 7 completely matched, 4 slightly matched (one of pathogens is the same), and 2 completely mismatched. There were no results from polymicrobial cultures. The bacteria with the highest abundances were S. epidermidis (6/13 [46.2%]), together with S aureus (3/13 [23.1%]). The most commonly identified bacteria by NGS are S. epidermidis (9/25 [30.0%]) and S. aureus (6/25 [24.0%]) (Table 2).
 |
Table 2 Microbial Results of mNGS and Culture in PJI Group |
There were 17 patients that tested positive for MSIS but had negative cultures. Within 12 patients (81.8%), mNGS could detect an organism, including known pathogens such as Mycobacterium tuberculosis, Streptococcus agalactiae, and Pseudomonas stutzeri. No infectious organism was isolated from culture or NGS in the remaining 5 patients.
Accuracy of mNGS and Culture Assays in Diagnosing PJI Compared with MSIS
The mNGS assay confirmed 25 of the 31 PJI cases found with MSIS, yielding a sensitivity of 80.6% (71.9–91.8%), which was significantly higher than culture (χ2 = 41.812, P < 0.001). Specificity, PPV, NPV, PLR, NLR, and AUC were determined to be 84.6% (73.7–97.9%), 92.6% (84.2–98.7%), 64.7% (58.6–74.7%), 5.241 (4.081–6.693), 0.229 (0.108–0.482), and 0.826 (0.786–0.967), respectively. Culture had sensitivity, specificity, PPV, NPV, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and AUC of 45.2% (40.8–51.5%), 100.0% (100.0–100.0%), 100.0% (100.0–100.0%), 43.3% (39.1–49.5%), 0.726 (0.621–0.864), 0.548 (0.396–0.617), and 0.5 (0.39–0.61), respectively, with MSIS as a reference (Table 3).
 |
Table 3 Performance of mNGS and Culture Compared to the MSIS Criteria |
mNGS Performance in Diagnosis with Diverse Reference Standards
Using culture as a control, mNGS achieved sensitivity, specificity, PPV, NPV, PLR, NLR, and AUC of 92.9% (87.7–99.6%), 53.3% (44.8–71.1%), 48.1.7% (41.2–59.6%), 94.1% (83.9–99.1%), 1.989 (1.504–2.814), and 0.152 (0.085–0.292) and 0.731 (0.654–0.897), respectively.
Using MSIS as a reference, mNGS achieved the following sensitivity, specificity, PPV, NPV, PLR, NLR, as well as AUC values: 84.6% (73.7–97.9%), 92.6% (84.2–98.7%), 64.7% (58.6–74.7%), 5.241 (4.081–6.693), 0.229 (0.108–0.482), and 0.826 (0.786–0.967), respectively (Table 4, Figure 2).
 |
Table 4 Comparison of Diagnostic Efficacies Using MSIS and Culture as the Reference Standard |
Effects of Antibiotic Exposure on the Positive Rate of mNGS and Culture
13 of the 31 patients in the PJI group (62%) received antibiotics two weeks before mNGS and microbial cultures. In the case of antibiotic exposure, mNGS achieved a sensitivity of 69.5%, which was significantly higher than microbial culture (21.3%, P = 0.001). Among non-antibiotic exposed patients, mNGS had a sensitivity of 66.7%, and microbial culture had a sensitivity of 44.4%, with no significant difference (P = 0.34) (Table 5).
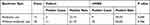 |
Table 5 Comparison of Antibiotic Use on the Efficacy of mNGS and Culture |
Discussion
PJI represents a fatal complication of hip/knee arthroplasty that can result in multiple surgical interventions, revision arthroplasty, long-term disability, and poor functional rehabilitation. Infection is responsible for more than 25% of revision surgeries, and its prevalence is increasing. Aseptic failure is distinguished from septic failure during revision arthroplasty. Clinical symptoms of PJI include affected joint swelling and discomfort, which can arise with aseptic failure. Existing diagnostic techniques, such as culture, radiographic test, and smear, are time-consuming and have low sensitivity and specificity, resulting in inaccurate or missing diagnoses. NGS can sequence all DNAs within a single sample, thus, yielding more thorough microbial profiles. Numerous recent studies show that the mNGS had a high sensitivity (61.9–95.6%) and specificity (73.0–100%) in the diagnosis of PJI.26,27 However, such studies were mostly based on synovial fluid or did not study how antibiotic use impacts the efficacy of culture and mNGS. Only a few studies discuss tissue samples as having diagnostic value. According to our results, mNGS is extremely sensitive and specific for diagnosing PJI in tissues.
Despite the fact that a few articles suggest that mNGS assay is clinically useful in PJI using bone tissues, there is no agreement on sensitivity or specificity. For starters, mNGS has many detection steps, and the detection results are affected by many factors, including reagents, sample types, detection platforms, biological information analysis, and so on.28 Additionally, it may be related to the disparate reference standards used in these studies. Inadequate reference standards may cause sample misclassification, lowering test sensitivity and specificity. MSIS and culture have been the most commonly utilized reference standards for diagnosing PJI. We found that using the MSIS standard mNGS yielded 80.6% sensitivity and 84.6% specificity, whereas culture yielded 92.9% sensitivity and 53.3% specificity. Using culture as a diagnostic criterion, mNGS achieved lower specificity than traditional MSIS (53.3% vs 84.6%; P < 0.001). This could be attributed to PJI’s paucibacillary nature, which results in low culture specificity. When culture was used as the reference standard, mNGS assay-based positive results were deemed false negative, underestimating the actual specificity. Hence, culture is yet another imperfect diagnostic standard. MSIS, based on several assessment indices, may be the more appropriate standard. Furthermore, the AUC values of both diagnostic standards were not substantially different (0.731 vs 0.826; P > 0.05). As a result, regardless of the diagnosis criterion, mNGS performed well in diagnosing PJI using tissues.
Our results showed a 45.2% positive microbial culture rate, which was lower than the results of similar studies.11,29 One possible explanation is that the PJI patients included had a high rate of antibiotic utilization prior to enrollment. In comparison, the positive rate of mNGS in the antibiotic exposure group was significantly higher than in the microbial culture group (69.5% vs 15.4%, P < 0.05), which was consistent with a previous study involving 347 patients with cerebrospinal fluid, alveolar lavage fluid, sputum, ascites, and tissues. In terms of mNGS, its positive rate in antibiotic exposure cases was significantly higher than in microbial culture (52.7% vs 23.1%, P<0.01).30 These results suggest that antibiotic exposure may have less of an effect on mNGS detection than microbial culture.
For our patients, the turnaround time for DNA-Seq was 32–36 h, which should be reduced to roughly 24 h because the sequencing platform was housed on-site in our center. In comparison, the mean pathogen culture feedback durations for bacteria, fungi, and mycobacteria were ≥3, 7, and 45 days, respectively. Therefore, mNGS has a time advantage in detection.
mNGS also poses certain issues and challenges in the diagnosis of PJI. To begin with, there is no perfect or uniform technique for identifying background microorganisms, and interpreting sequencing results has become a big challenge.31 The integration of microbial genetic sequences during sampling and laboratory testing seems unavoidable, making identifying the actual pathogenic organism challenging, especially when opportunistic pathogens are present. For example, Propionibacterium acnes is part of the typical bacterial flora of the skin, sometimes referred to as background bacteria. However, PJI induced by P. acnes has been documented frequently.32,33 Secondly, mNGS can only detect drug sensitivity in the presence of pathogenic microorganisms, and its ability to guide reasonable antibiotic screening should be improved. In addition, the expensive cost of mNGS detection limits the use of this technology in PJI diagnosis.
Limitations of this study (1) As a Unicenter investigation, this study contained a small number of patients, which may impair the reliability of the conclusions. In the future, multi-center studies should be conducted to corroborate findings. (2) There is no certainty that all physicians and surgeons for sampling are the same.
In conclusion, this study suggests that mNGS is valuable for etiological PJI diagnosis, improves PJI detection, and challenges PJI identification by culture. It can reduce detection time and is less susceptible to antibiotics. It is an excellent supplemental approach for detecting bacterial cultures. There is a need for a multi-center, large sample, and multi-type mNGS diagnostic efficacy studies.
Abbreviations
PJI, Periprosthetic joint infection; ESR, erythrocyte sedimentation rate; CRP, C-reactive protein; BMI, body mass index; PCT, Procalcitonin; mNGS, metagenomic next-generation sequencing; THR, total hip arthroplasty; TKR, total hip replacement.
Ethics Approval and Consent to Participate
The study protocol was approved by the Institutional Review Board of Zhengzhou Orthopaedics Hospital (202109). This study was conducted in accordance with the declaration of Helsinki and patient data were kept confidential.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Peersman G, Laskin R, Davis J, Peterson M. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res. 2001;392:15–23. doi:10.1097/00003086-200111000-00003
2. Meehan J, Jamali AA, Nguyen H. Prophylactic antibiotics in hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91(10):2480–2490. doi:10.2106/JBJS.H.01219
3. Blom AW, Brown J, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Infection after total knee arthroplasty. J Bone Joint Surg Br. 2004;86(5):688–691. doi:10.1302/0301-620x.86b5.14887
4. Laffer RR, Graber P, Ochsner PE, Zimmerli W. Outcome of prosthetic knee-associated infection: evaluation of 40 consecutive episodes at a single centre. Clin Microbiol Infect. 2006;12(5):433–439. doi:10.1111/j.1469-0691.2006.01378.x
5. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi:10.2106/JBJS.F.00222
6. Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty. 2012;27(8Suppl):61–5.e1. doi:10.1016/j.arth.2012.02.022
7. Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014;96(8):624–630. doi:10.2106/JBJS.M.00285
8. Benito N, Franco M, Ribera A, et al. Time trends in the aetiology of prosthetic joint infections: a multicentre cohort study. Clin Microbiol Infect. 2016;22(8):732.e1–732.e7328. doi:10.1016/j.cmi.2016.05.004
9. Gbejuade HO, Lovering AM, Webb JC. The role of microbial biofilms in prosthetic joint infections. Acta Orthop. 2015;86(2):147–158. doi:10.3109/17453674.2014.966290
10. Gatti G, Taddei F, Brandolini M, et al. Molecular approach for the laboratory diagnosis of periprosthetic joint infections. Microorganisms. 2022;10(8):1573. doi:10.3390/microorganisms10081573
11. Yoon HK, Cho SH, Lee DY, et al. A review of the literature on culture-negative periprosthetic joint infection: epidemiology, diagnosis and treatment. Knee Surg Relat Res. 2017;29(3):155–164. doi:10.5792/ksrr.16.034
12. Corvec S, Portillo ME, Pasticci BM, Borens O, Trampuz A. Epidemiology and new developments in the diagnosis of prosthetic joint infection. Int J Artif Organs. 2012;35(10):923–934. doi:10.5301/ijao.5000168
13. Van Diek FM, Albers CGM, Van Hooff ML, Meis JF, Goosen JHM. Low sensitivity of implant sonication when screening for infection in revision surgery. Acta Orthop. 2017;88(3):294–299. doi:10.1080/17453674.2017.1300021
14. Woo PC, Lau SK, Teng JL, Tse H, Yuen KY. Then and now: use of 16S rDNA gene sequencing for bacterial identification and discovery of novel bacteria in clinical microbiology laboratories. Clin Microbiol Infect. 2008;14(10):908–934. doi:10.1111/j.1469-0691.2008.02070.x
15. Wang CX, Huang Z, Fang X, Li W, Yang B, Zhang W. Comparison of broad-range polymerase chain reaction and metagenomic next-generation sequencing for the diagnosis of prosthetic joint infection. Int J Infect Dis. 2020;95:8–12. doi:10.1016/j.ijid.2020.03.055
16. Higgins E, Suh GA, Tande AJ, Humphries RM. Enhancing diagnostics in orthopedic infections. J Clin Microbiol. 2022;60(6):e0219621. doi:10.1128/jcm.02196-21
17. Ivy MI, Thoendel MJ, Jeraldo PR, et al. Direct detection and identification of prosthetic joint infection pathogens in synovial fluid by metagenomic shotgun sequencing. J Clin Microbiol. 2018;56(9):e00402–e00418. doi:10.1128/JCM.00402-18
18. Indelli PF, Ghirardelli S, Violante B, Amanatullah DF. Next generation sequencing for pathogen detection in periprosthetic joint infections. EFORT Open Rev. 2021;6(4):236–244. doi:10.1302/2058-5241.6.200099
19. Cai Y, Fang X, Chen Y, et al. Metagenomic next generation sequencing improves diagnosis of prosthetic joint infection by detecting the presence of bacteria in periprosthetic tissues. Int J Infect Dis. 2020;96:573–578. doi:10.1016/j.ijid.2020.05.125
20. Kwon M, Seo SS, Kim MK, Lee DO, Lim MC. Compositional and functional differences between microbiota and cervical carcinogenesis as identified by shotgun metagenomic sequencing. Cancers. 2019;11(3):309. doi:10.3390/cancers11030309
21. Wilson MR, Sample HA, Zorn KC, et al. Clinical metagenomic sequencing for diagnosis of meningitis and encephalitis. N Engl J Med. 2019;380(24):2327–2340. doi:10.1056/NEJMoa1803396
22. Zhang C, Fang X, Huang Z, et al. Value of mNGS in sonication fluid for the diagnosis of periprosthetic joint infection. Arthroplasty. 2019;1(1):9. doi:10.1186/s42836-019-0006-4
23. Fang X, Cai Y, Shi T, et al. Detecting the presence of bacteria in low-volume preoperative aspirated synovial fluid by metagenomic next-generation sequencing. Int J Infect Dis. 2020;99:108–116. doi:10.1016/j.ijid.2020.07.039
24. Gu W, Miller S, Chiu CY. Clinical metagenomic next-generation sequencing for pathogen detection. Annu Rev Pathol. 2019;14(1):319–338. doi:10.1146/annurev-pathmechdis-012418-012751
25. Parvizi J, Zmistowski B, Berbari EF, et al. New definition for periprosthetic joint infection: from the workgroup of the musculoskeletal infection society. Clin Orthop Relat Res. 2011;469(11):2992–2994. doi:10.1007/s11999-011-2102-9
26. Street TL, Sanderson ND, Atkins BL, et al. Molecular diagnosis of orthopedic-device-related infection directly from sonication fluid by metagenomic sequencing. J Clin Microbiol. 2017;55(8):2334–2347. doi:10.1128/JCM.00462-17
27. Huang Z, Li W, Lee GC, et al. Metagenomic next-generation sequencing of synovial fluid demonstrates high accuracy in prosthetic joint infection diagnostics: mNGS for diagnosing PJI. Bone Joint Res. 2020;9(7):440–449. doi:10.1302/2046-3758.97.BJR-2019-0325
28. Schlaberg R, Chiu CY, Miller S, et al. Validation of metagenomic next-generation sequencing tests for universal pathogen detection. Arch Pathol Lab Med. 2017;141(6):776–786. doi:10.5858/arpa.2016-0539-RA
29. Palan J, Nolan C, Sarantos K, Westerman R, King R, Foguet P. Culture-negative periprosthetic joint infections. EFORT Open Rev. 2019;4(10):585–594. doi:10.1302/2058-5241.4.180067
30. Miao Q, Ma Y, Wang Q, et al. Microbiological diagnostic performance of metagenomic next-generation sequencing when applied to clinical practice. Clin Infect Dis. 2018;67(suppl_2):S231–S240. doi:10.1093/cid/ciy693
31. Simner PJ, Miller S, Carroll KC. Understanding the promises and hurdles of metagenomic next-generation sequencing as a diagnostic tool for infectious diseases. Clin Infect Dis. 2018;66(5):778–788. doi:10.1093/cid/cix881
32. Klement MR, Cunningham DJ, Wooster BM, et al. Comparing standard versus extended culture duration in acute hip and knee periprosthetic joint infection. J Am Acad Orthop Surg. 2019;27(9):e437–e443. doi:10.5435/JAAOS-D-17-00674
33. Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014;27(2):302–345. doi:10.1128/CMR.00111-13
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

