Back to Journals » Infection and Drug Resistance » Volume 16
Development of a Risk Prediction Model of Subsequent Bloodstream Infection After Carbapenem-Resistant Enterobacteriaceae Isolated from Perianal Swabs in Hematological Patients
Authors Liu J, Zhang H, Feng D, Wang J, Wang M, Shen B, Cao Y, Zhang X, Lin Q, Zhang F, Zheng Y, Xiao Z, Zhu X, Zhang L, Wang J, Pang A, Han M, Feng S, Jiang E
Received 21 December 2022
Accepted for publication 21 February 2023
Published 6 March 2023 Volume 2023:16 Pages 1297—1312
DOI https://doi.org/10.2147/IDR.S400939
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Jia Liu, Haixiao Zhang, Dan Feng, Jiali Wang, Mingyang Wang, Biao Shen, Yigeng Cao, Xiaoyu Zhang, Qingsong Lin, Fengkui Zhang, Yizhou Zheng, Zhijian Xiao, Xiaofan Zhu, Lei Zhang, Jianxiang Wang, Aiming Pang, Mingzhe Han, Sizhou Feng, Erlie Jiang
State Key Laboratory of Experimental Hematology, National Clinical Research Center for Blood Diseases, Haihe Laboratory of Cell Ecosystem, Institute of Hematology & Blood Diseases Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Tianjin, People’s Republic of China
Correspondence: Sizhou Feng; Erlie Jiang, State Key Laboratory of Experimental Hematology, National Clinical Research Center for Blood Diseases, Haihe Laboratory of Cell Ecosystem, Institute of Hematology & Blood Diseases Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, No. 288 Nanjing Road, Tianjin, 300020, People’s Republic of China, Email [email protected]; [email protected]
Purpose: Patients with hematological diseases are at high risk of carbapenem-resistant Enterobacteriaceae (CRE) infection, and CRE-related bloodstream infection (BSI) is associated with high mortality risk. Therefore, developing a predictive risk model for subsequent BSI in hematological patients with CRE isolated from perianal swabs could be used to guide preventive strategies.
Methods: This was a single-center retrospective cohort study at a tertiary blood diseases hospital, including all hematological patients hospitalized from 10 October 2017 to 31 July 2021. We developed a predictive model using multivariable logistic regression and internally validated it using enhanced bootstrap resampling.
Results: Of 421 included patients with CRE isolated from perianal swabs, BSI due to CRE occurred in 59. According to the multivariate logistic analysis, age (OR[odds ratio]=1.04, 95% CI[confidence interval]: 1.01– 1.06, P=0.004), both meropenem and imipenem minimal inhibitory concentration (MIC) of the isolate from perianal swabs> 8ug/mL (OR=5.34, 95% CI: 2.63– 11.5, P< 0.001), gastrointestinal symptoms (OR=3.67, 95% CI: 1.82– 7.58, P< 0.001), valley absolute neutrophil count (109/L)> 0.025 (OR=0.07, 95% CI: (0.02– 0.19, P< 0.001) and shaking chills at peak temperature (OR=6.94, 95% CI: (2.60– 19.2, P< 0.001) were independently associated with CRE BSI within 30 days and included in the prediction model. At a cut-off of prediction probability ≥ 21.5% the model exhibited a sensitivity, specificity, positive predictive value and negative predictive value of 79.7%, 85.6%, 96.27% and 47.47%. The discrimination and calibration of the prediction model were good on the derivation data (C-statistics=0.8898; Brier score=0.079) and enhanced bootstrapped validation dataset (adjusted C-statistics=0.881; adjusted Brier score=0.083). The risk prediction model is freely available as a mobile application at https://liujia1992.shinyapps.io/dynnomapp/.
Conclusion: A prediction model based on age, meropenem and imipenem MIC of isolate, gastrointestinal symptoms, valley absolute neutrophil count and shaking chills may be used to better inform interventions in hematological patients with CRE isolated from perianal swabs.
Keywords: carbapenem-resistant Enterobacteriaceae, bloodstream infection, risk prediction model, hematological patients, perianal colonization
Introduction
The emergence and spread of carbapenem-resistant Enterobacteriaceae (CRE) have become a serious global public health problem.1 Patients with hematological malignancies, whose immune functions are suppressed or even deficient, are at high risk of CRE infection and have a higher mortality rate due to receiving radiotherapy, chemotherapy, immunosuppressants or hematopoietic stem cell transplantation (HSCT).2–4 Among all types of CRE infection, bloodstream infection (BSI) was shown to be the independent risk factor for mortality.5 Furthermore, patients with CRE BSI had a median of 52 hours from culture collection until receipt of active therapy and they had a higher BSI-related mortality rate than those who received appropriate antibiotic therapy within the first 24 h of blood culture collection.6,7 Fortunately, CRE-active empirical therapy was associated with a lower 30-day mortality rate.6,7 Therefore, early identification of patients with CRE BSI and rapid initiation of empiric CRE-targeted therapy should be considered to improve prognosis.
However, some predictive features appear to be ineffective for patient identification. Given that CRE colonization was an independent risk factor for CRE infection,8 CRE asymptomatic carriers and previously infected patients are usually at increased risk of having a subsequent CRE infection. Thus, clinicians are often compelled to initiate early empiric CRE-targeted therapy. However, most CRE carriers did not develop CRE infection at a later stage. A systematic review analyzed 1806 CRE-colonized patients from 10 studies and found that the subsequent cumulative rate of infection was only 16.5%.9 For patients that are in fact unlikely to have a true CRE infection, active CRE-targeted empirical treatment may cause antibiotics abuse and increase the economic burden. Therefore, developing a quantified risk prediction model based on the risk factors of subsequent BSI in CRE carriers will help clinicians better identify specific individuals who would truly benefit from early empiric CRE-targeted treatment.
Some risk prediction models of subsequent infection in patients with CRE colonization have been developed. However, the subjects of these studies were mainly patients in intensive care units,8 patients undergoing liver transplantation,10 or hospitalized patients containing only a small number of participants from the hematology department.11,12 Other studies constructed the models for carbapenem-resistant Klebsiella pneumoniae (CRKP) strain only.11 However, unlike CRKP which is the main strain of CRE infection in patients with hematological tumors in Europe and the United States, carbapenem-resistant Escherichia coli (CREC) and CRKP account for almost half of the strains of CRE infection in Chinese patients with hematological tumor.3,13 This justifies the need to develop another model suitable for diagnosing and treating patients with hematological diseases with different disease characteristics and treatment approaches.
In summary, given the high risk of CRE infection in patients with hematological diseases and the high mortality of CRE BSI, this study aimed to develop a predictive risk model for subsequent BSI in hematological patients with CRE isolated from perianal swabs to identify patients at high risk of CRE BSI who are eligible to receive appropriate empirical antibiotic therapy.
Materials and Methods
Study Design and Patients
This was a single-center real-world retrospective cohort study at a 769-bed tertiary blood diseases hospital in Tianjin, China. The number of admissions to the hematology ward of the hospital is nearly 30,000 per year. Data of hematological patients hospitalized from 10 October 2017 to 31 July 2022 were collected, and patients with CRE isolated from perianal swabs were included in this study. Patients were divided into the case group and control group based on the occurrence of subsequent CRE BSI in the following 30 days. The exclusion criteria were: 1) occurrence of CRE BSI before the first CRE isolated from perianal swabs; 2) urinary or pulmonary CRE infection within 30 days after the first CRE isolated from perianal swabs; 3) death or loss to follow-up within 30 days in the control group. The follow-up time of patients was considered from the time of the first perianal CRE positive to CRE BSI onset (cases), or 30 days after the first isolation of CRE from perianal swabs (controls). The clinical outcome was the occurrence of CRE BSI occurred within 30 days after the first isolation of CRE from perianal swabs. Each case was included only once at the time of the first CRE isolation from blood cultures, even if more than one CRE BSI was reported. The onset of BSI was defined as the date of collection of the positive blood culture sample. The presence or absence of clinical outcome was decided blinded to the predictors under study.
Microbiology
All patients routinely received perianal screening for CRE within 48 hours of each hospital admission. In addition, some patients received perianal bacterial culture tests when they were suspected of infection by a competent physician during hospitalization. Perianal skin and throat swab samples were collected and submitted for examination by specially trained medical staff. Bacterial culture, identification and drug sensitivity test were conducted by special technicians in the microbiology laboratory, and the target bacteria were CRE. All CRE strains were isolated from perianal skin swabs and blood samples. Blood culture was performed using an automatic blood culture system (BD, USA). The isolation and identification of bacteria were carried out strictly following the relevant provisions of the National Clinical Laboratory Procedures. VITEK 2 compact (bioMérieux, France) was used to identify the isolates and MALDI-TOF MS (bioMérieux, France) was used for further confirmation. Antibiotic susceptibility testing was performed in the microbiology laboratory of the hospital using an automated system (VITEK 2 Compact) with the broth microdilution and disk diffusion methods. The following antibiotics were tested: penicillins (ticarcillin, piperacillin), β-lactamase inhibitor combinations (amoxicillin/clavulanic acid, piperacillin/tazobactam, cefoperazone/sulbactam), cephalosporins (cefazolin, cefuroxime, ceftazidime, cefepime, cefotaxime, cefotetan, cefpodoxime, ceftizoxime), quinolones (levofloxacin, moxifloxacin, ciprofloxacin, norfloxacin), carbapenems (imipenem, meropenem, doripenem), aminoglycosides (amikacin, tobramycin), tetracyclines (tetracycline, minocycline), aztreonam, trimethoprim/sulfamethoxazole and tigecycline. The minimum inhibitory concentration (MIC) was measured according to the guidelines of the 31st Edition of the Clinical and Laboratory Standards Institute (CLSI) M100-Performance Standards for Antimicrobial Susceptibility Testing.14 The detection of carbapenemases in CRE according to the modified carbapenem inactivation assay (mCIM and eCIM) provided by the CLSI 31th Edition.
Data Collection and Definition
Baseline characteristics were collected, such as: demographic data (age and sex), diagnosis of hematologic diseases, level of the disease risk, Charlson Comorbidity Index, prior 30-day antibiotic use before first isolation of CRE, microbiological characteristics (strain type and site, carbapenemases production and carbapenems MIC of isolate in the first perianal CRE positive), hematopoietic stem cell transplantation, treatment (radiotherapy, chemotherapy, immunosuppressive therapy and invasive catheter) and complications (emergence or progression of lung infection, oral mucositis, perianal infection, gastrointestinal symptoms and infections caused by other bacteria) after first isolation of CRE. Data on the valley absolute neutrophil count, the peak body temperature, blood pressure at peak body temperature, heart rate at peak body temperature, and the presence or absence of shaking chills during the observation period were also collected.
CRE were Enterobacteriaceae bacteria that meet any of the following conditions: 1) Drug resistance to any carbapenems (The MIC of imipenem, meropenem and doripenem was ≥ 4 mg/L, or the MIC of ertapenem was ≥2 mg/L); 2) producing carbapenemase; 3) if it is a bacteria that is naturally resistant to imipenem, such as Morganella morganii, Proteus genus, Provenice genus, it must also be resistant to other carbapenems like meropenem, ertapenem, doripenem.15 The onset of BSI was defined as the date of collection of the positive blood culture sample. Acute leukemia (AL), including acute myeloid leukemia and acute lymphoblastic leukemia in complete remission (CR), lymphoma in CR or partial remission, refractory anemia of myelodysplastic syndrome (MDS) and untreated severe aplastic anemia (SAA) were defined as standard risk. Meanwhile, AL in induction failure or relapse, lymphoma in stable disease or progression and MDS/SAA transfusion dependence with no response to treatment were classified as high risk.13,16 Chemotherapy or radiation therapy was defined as the prescription of cytotoxic antineoplastic drugs or ionizing radiation for cancer cure or palliation. Pulmonary infection was diagnosed when patients had an acute respiratory disorder and new onset of pulmonary infiltration on chest computed tomography.17 Gastrointestinal symptoms included the presence of abdominal pain, diarrhea, or lower gastrointestinal bleeding. Perianal infections included perianal pain, perianal abscess, anal fistula, perianal gangrene or scrotal infection. Shaking chills were defined as feeling extremely cold with rigors and generalized bodily shaking, even under a thick blanket.18
Statistical Analysis
R (Version 4.0.4) was used for statistical analysis. The Shapiro–Wilk test was used to check the normal distribution of continuous data. Normally distributed continuous data were expressed as means ± standard deviation (SD) and tested using the Student’s t-test. Non-normally distributed continuous data were expressed as medians (first quartile, third quartile) and tested using the Mann–Whitney U-test. Categorical data were expressed as number (n) and percentage (%) and tested using the Chi-square test or Fisher’s exact test.
Candidate variables, selected based on statistical significance in univariate logistic analysis (P<0.05), clinical experience and published data were included in the multivariate logistic analysis using stepwise methods. The final variables in the prediction model were selected by the clinical significance, principle of statistics19 and the results of the multivariate logistic analysis (P<0.05). The final regression model was visualized by a nomogram to predict the CRE BSI. Furthermore, the receiver-operating characteristic (ROC) curve (area under the curve [AUC]) and the C-statistic were used to assess the discrimination ability of this nomogram. The calibration curves and Brier score were used to assess the calibration ability of this nomogram. In addition, enhanced bootstrap internal validation was performed to verify the diagnostic efficiency of the model. Furthermore, decision curve analysis (DCA) was performed to determine the model’s clinical usefulness. P<0.05 was considered statistically significant. An online prediction tool (Shiny App) was prepared using the DynNom package in R. The construction process was conducted according to the Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis guidelines.20
Results
Study Population and Baseline Characteristics
A total of 478 patients were screened, and 421 were finally included in the study according to the study’s exclusion criteria. CRE BSI occurred in 59 patients (Figure 1). The median time from the first positive perianal CRE to the onset of CRE BSI was 11 (1–30) days. The mortality rate within 30 days was 20.34% among CRE BSI patients (Figure 2A). The first three strains isolated from perianal swabs were CREC (39.7%), CRKP (33.7%) and carbapenem-resistant Enterobacter cloacae (CREL) (18.3%), and the other isolated strains are shown in Table 1. Of all the species detected from blood, 45.9% were CRKP, 42.6% were CREC, and 11.5% were CREL (Table 2). Among these 59 patients, the coincidence rate of strains isolated from perianal swabs and blood samples was 96.61% and only two patients (3.39%) had differences between the colonization strain and infection strain (Figure 2B). In addition, the trend of drug resistance of perianal skin swabs and blood isolates to imipenem, meropenem, piperacillin-tazobactam, levofloxacin, amikacin, aztreonam and tigecycline was highly consistent (Figure 2C).
 |
Table 1 Distribution of Carbapenem-Resistant Enterobacteriaceae Strains in Perianal Swabs from 421 Patients |
 |
Table 2 Characteristics of All Patients (n = 421) |
 |
Figure 1 Participant flow diagram. Abbreviations: CRE, carbapenem-resistant Enterobacteriaceae; BSI, bloodstream infection. |
Before November 2019, our hospital laboratory could only identify whether CRE strains were carbapenemase-producing, and could not further determine whether the carbapenemases were serine carbapenemases or metallo-carbapenemases. Among 228 perianal swabs from patients after November 2019, 112 perianal isolates were carbapenemase-producing CRE (CP-CRE), of which 78.57% (88/112) were metallo-carbapenemases and 21.43% (24/112) were serine-carbapenemases. Similarly, among the 35 CRE isolates from blood samples included after November 2019, 32 were CP-CRE, of which 71.87% (23/32) were metallo-carbapenemases and 28.13% (9/23) were serine-carbapenemases.
Detailed characteristics of all patients are presented in Table 2. CRE BSI and non-CRE BSI patients differed significantly by age, multi-site colonization, carbapenemases production, both meropenem and imipenem MIC of isolate>8ug/mL, chemotherapy, radiotherapy, perianal skin infection, gastrointestinal symptoms, valley absolute neutrophil count, peak body temperature, heart rate at peak body temperature and shaking chills at peak body temperature after the first CR-positive perianal test (all P<0.05).
Associated Factors of CRE BSI
To screen for factors associated with subsequent BSI after CRE isolation from perianal swabs, we performed univariate logistic analyses of patients with and without CRE BSI (Table 3). In total, 17 candidate variables, selected based on clinical and statistical significance in univariate logistic analysis (P<0.05), clinical experience and published data, were included in the multivariate logistic analysis. Multivariate analysis found that age, carbapenemases production, both meropenem and imipenem MIC of isolate>8ug/mL, hematopoietic stem cell transplantation, perianal skin infection, gastrointestinal symptoms, valley absolute neutrophil count (109/L) ≤0.025, peak body temperature ≥38 °C, heart rate at peak body temperature > 100 bpm and shaking chills at peak temperature (P<0.05) were independently associated with CRE BSI (Table 3).
 |
Table 3 Univariate and Multivariate Logistic Analysis for the CRE BSI Within 30 Days |
Development of the Prediction Model
Considering the clinical significance, stability and limited number of the variable, in addition to the convenience of clinical application, the following five variables were included in the prediction model: age, carbapenem resistance level, gastrointestinal symptoms, valley absolute neutrophil count and shaking chills at peak temperature within 30 days after first CRE-positive perianal test. The results of the logistic analysis are shown in Table 4. According to the logistic analysis, age (OR [odds ratio]=1.04, 95% CI [confidence interval]: 1.01–1.06, P=0.004), both meropenem and imipenem MIC of isolate>8ug/mL (OR=5.34, 95% CI: 2.63–11.5, P<0.001), gastrointestinal symptoms (OR=3.67, 95% CI: 1.82–7.58, P<0.001), valley absolute neutrophil count (109/L)>0.025 (OR=0.07, 95% CI: (0.02–0.19, P<0.001) and shaking chills at peak temperature (OR=6.94, 95% CI: (2.60–19.2, P<0.001) were independently associated with CRE BSI within 30 days. As described in Figure 3, the operation of the model was based on the nomogram in which all five factors described above correspond to values obtained during the multivariate analysis. The risk prediction model is freely available as a mobile application at https://liujia1992.shinyapps.io/dynnomapp/.
 |
Table 4 Final Multivariable Analysis for Predicting Risk of CRE BSI Within 30 Days |
Performance of the Prediction Model
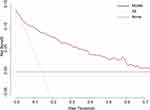
Discrimination was assessed using the ROC curve, and the AUC for predicting BSI by the nomogram model was 0.890 (95% CI:0.846–0.934) (Figure 4A). Risk stratification was performed in all patients based on the optimal cut-off value (0.215) of the ROC curve. The incidence of CRE BSI in the high-risk patients was higher than that in the low-risk patients (47.5% vs 3.7%, P<0.001) (Figure 5). At a cut-off of prediction probability ≥ 21.5%, the model exhibited a sensitivity, specificity, positive predictive value and negative predictive value of 79.7%, 85.6%, 96.27% and 47.47%. A calibration curve was used to assess the consistency between predictions by the model and observed risks across of the population. The Hosmer-Lemeshow goodness of fit test was used to evaluate the degree of calibration of the proposed logistic regression model, and the test results indicated that the model had a good test efficiency (P=0.534) (Figure 4B).
Internal Validation and Clinical Usefulness of Model
Internal validation of this proposed prediction model was performed using the 500 times resampling enhanced bootstrap method to estimate the C-Statistic and Brier Score. The apparent C-statistic and apparent Brier score was 0.8898 and 0.079, respectively. The optimism of the C-statistic and Brier score was 0.0088 and −0.0039, respectively. The adjusted C-statistic and Brier score was 0.881 and 0.083, respectively.
The DCA showed that if the threshold probability of the patient was 5–70%, using this theoretical risk-model guided strategy (ie, empiric administration of CRE-active antibiotics) adds more benefit than either the treat-all-patients scheme or the treat-none scheme (Figure 6).
Discussion
Similar to previous studies,9 only 14% of patients developed BSI after CRE was isolated from swabs in this study, and the vast majority of patients developed CRE BSI within 30 days. However, the mortality rate of about a quarter still grim. Whether and when CRE carriers need to be de-colonization is uncertain, and the potential risk factors of infection vary between different populations. Due to the critical consequences of CRE BSI, this study aimed to develop a BSI prediction model in hematological patients with CRE to identify high risk patients who are eligible for appropriate empirical antibiotic therapy. This single-center retrospective cohort study, conducted in patients with hematological diseases and positive CRE anal swab has found that age, meropenem and imipenem MIC of isolate from perianal swabs, gastrointestinal symptoms, valley neutrophil value (109/L) ≤ 0.025 and shaking chills at peak temperature within 30 days of the first positive perianal test were independently associated with the occurrence of CRE BSI. The developed prediction model based on the above risk factors demonstrated acceptable specificity and sensitivity and was validated using the enhanced bootstrap method. To the best of our knowledge this is the first prediction model proposed for the risk evaluation of subsequent CRE BSI after CRE perianal swab positive among hematological patients and obtained results that may contribute to guiding risk stratification of CRE in clinical practice.
Although CRE strains are resistant to carbapenems, when meropenem or imipenem MIC of isolated CRE strains ≤ 8ug/mL, meropenem or imipenem can still be used in combination with another drug with in vitro anti-CRE activity to treat CRE infection under the conditions of increased dosage and prolonged administration time.20,21 Interestingly, our study found that when both meropenem and imipenem MIC of isolates from perianal swabs >8ug/mL, meaning isolates had a relatively high resistance to carbapenems, patients were more likely to develop subsequent BSI. The results were similar to the study of Wang et al who used carbapenem resistance score to evaluate the carbapenem resistance of isolates according to the inhibition zone diameters of meropenem and imipenem.12 They found that high carbapenem resistance score was an independent risk factor for subsequent CRE BSI in rectal carriers. Thus, CRE strains with high resistance to carbapenems isolated from carriers might be associated with the occurrence of BSI. Meanwhile, their funding also suggest that the commonly used carbapenems may not be a good selection for patients with CRE BSI.
Gastrointestinal mucositis caused by radiotherapy and chemotherapy is a complex reaction of the mucous membranes, accompanied by a series of gastrointestinal symptoms, and its severity is difficult to assess.22 Patients with malignant hematological diseases and hematopoietic stem cell transplantation recipients have a high risk of developing invasive infections due to enteric bacteria because of chemotherapy-induced gastrointestinal mucositis.3,23,24 Wang et al found that gastrointestinal injury with definite diagnosis, including gastrointestinal bleeding or perforation, ostomy or excision of stomach and intestine, gastroenteritis, cholecystitis and pancreatitis was an independent risk factor of subsequent CRE BSI.12 Likewise, our study found that hematological patients with gastrointestinal symptoms, including abdominal pain, diarrhea and gastrointestinal bleeding, after CRE colonization were independent risk factors for subsequent CRE BSI and could be included in the model for risk assessment of CRE BSI in CRE carriers. The damage to gastrointestinal barrier is a potential entry for CRE, which reasonably explains the occurrence of subsequent BSI. Hence, paying attention to reducing gastrointestinal injury for hematological patients may help to prevent the occurrence of BSI.
Patients with neutropenia were highly related to BSI.25,26 Most hematological patients will develop neutropenia due to immune deficiency, radiotherapy and chemotherapy, but only some developed subsequent CRE BSI. It is worthwhile to further explore the relationship between the time and value of neutropenia and CRE BSI. Cao et al found that agranulocytosis time ≥21 days was a risk factor for BSI in hematopoietic stem cell transplantation recipients.26 However, there is a lack of relevant research. Hence, we analyzed the neutropenia value and found that patients were more likely to develop subsequent CRE BSI when their valley neutrophil value (109/L) was less than 0.025. This result may contribute to the further risk stratification of patients with neutropenia in clinical practice.
Previous studies failed to show that age may be associated with CRE BSI.27,28 However, this study found that age was one of the independent risk factors included into the prediction model, The differences listed above might be explained by the fact that previous studies were focused on children or adult patients of a certain age. In addition, prior antibiotic treatment was not significantly associated with BSI in our study, while previous studies found that tigecycline use before admission was associated with BSI.12 This may be because patients with hematological diseases often suffer from immune deficiency, resulting in high rates of antibiotics use. Furthermore, shaking chills were strong predictors of subsequent CRE BSI in our study, which is in line with our traditional understanding that chills and are often associated with severe infection and bacteremia.18,29,30 Those notions are worth continuing their verification in subsequent studies and potentially suggesting them for use in clinical practice.
A similar prediction model proposed by Giannella et al10 was based on chemotherapy, radiotherapy, invasive abdominal manipulation, and colonization at multiple sites, which showed less or no predictive value in our study. This may be related to different subjects. The patients included in the Giannella’s study were from large-scale tertiary nursing general hospitals, while our study subjects were only patients with hematological diseases, and most of them received radiotherapy and chemotherapy, making it difficult to appreciate any difference. Focusing on a specific population is also one of the strengths of this study. Unlike the above mentioned study, that only studied CRKP, this study included all CRE strains. In our study, CREC was the most frequently found strain (39.7%), followed by Klebsiella pneumoniae took (33.7%) and CREL (18.3%), which is reflective of the real clinical setting in China. In particular, the type of bacterial strains was not restricted in light of possible in vivo inter-species plasmid transfer.31–33
Based on this model, patients in the high-risk group with fever or other signs of infection can be considered strong anti-infective treatment, given that CRE strains and antibiotic susceptibility testing from perianal skin swabs and blood samples were highly consistent. Drug selection can refer to the sensitive drugs of previous bacteria in perianal swabs before the blood culture results.
This study had some limitations. Firstly, the sample size is relatively small, with fewer events but more variables were included in the analysis. Although this study had the largest number of hematological patients with BSI after a positive CRE perianal swabs (n=59) reported so far, the model should be further evaluated in larger studies to reach a conclusion regarding the proposed sensitivity. Secondly, this was a single center study without external validation. Finally, this study has inherited all limitations of a retrospective design, including the possibility of bias.
Conclusion
The proposed prediction model based on age, meropenem and imipenem MIC of isolate, gastrointestinal symptoms, valley absolute neutrophil count and shaking chills may be used for risk stratification of CRE BSI in hematological patients with CRE isolated from perianal swabs.
Ethics Statements
This study was approved by the ethical committee of the Institute of Hematology and Blood Diseases Hospital, Chinese Academy of Medical Sciences (QTJC2022012-EC-1). Written informed consent was waived by the ethics committee for research in health due to the anonymized retrospective analysis. In addition, this study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (82070192 & 81670171 & 82170217), the Haihe Laboratory of Cell Ecosystem Innovation Fund (HH22KYZX0034), the Fundamental Research Funds for the Central Universities (3332021055), the Key Project of Tianjin Natural Science Foundation (20JCZDJC00410) and the CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-073). The abstract of this paper was presented at the EHA2022 Hybrid Congress name development of a risk prediction model of subsequent bloodstream infection after carbapenem-resistant Enterobacteriaceae isolated from perianal swabs in patients with hematological diseases as a poster presentation with interim findings.
Disclosure
Dr Jianxiang Wang is an adviser for Abbvie, outside the submitted work. The authors declare no competing interests.
References
1. Logan LK, Weinstein RA. The epidemiology of carbapenem-resistant Enterobacteriaceae: the impact and evolution of a global menace. J Infect Dis. 2017;215(suppl_1):S28–S36. doi:10.1093/infdis/jiw282
2. Satlin MJ, Jenkins SG, Walsh TJ. The global challenge of carbapenem-resistant Enterobacteriaceae in transplant recipients and patients with hematologic malignancies. Clin Infect Dis. 2014;58(9):1274–1283. doi:10.1093/cid/ciu052
3. Pouch SM, Satlin MJ. Carbapenem-resistant Enterobacteriaceae in special populations: solid organ transplant recipients, stem cell transplant recipients, and patients with hematologic malignancies. Virulence. 2016;8(4):391–402. doi:10.1080/21505594.2016.1213472
4. Zhang Y, Guo LY, Song WQ, Wang Y, Dong F, Liu G. Risk factors for carbapenem-resistant K. pneumoniae bloodstream infection and predictors of mortality in Chinese paediatric patients. BMC Infect Dis. 2018;18(1):248. doi:10.1186/s12879-018-3160-3
5. Capone A, Giannella M, Fortini D, et al. High rate of colistin resistance among patients with carbapenem-resistant Klebsiella pneumoniae infection accounts for an excess of mortality. Clin Microbiol Infect. 2013;19(1):E23–E30. doi:10.1111/1469-0691.12070
6. Satlin MJ, Cohen N, Ma KC, et al. Bacteremia due to carbapenem-resistant Enterobacteriaceae in neutropenic patients with hematologic malignancies. J Infect. 2016;73(4):336–345. doi:10.1016/j.jinf.2016.07.002
7. Falcone M, Bassetti M, Tiseo G, et al. Time to appropriate antibiotic therapy is a predictor of outcome in patients with bloodstream infection caused by KPC-producing Klebsiella pneumoniae. Crit Care. 2020;24(1):29. doi:10.1186/s13054-020-2742-9
8. McConville TH, Sullivan SB, Gomez-Simmonds A, Whittier S, Uhlemann AC. Carbapenem-resistant Enterobacteriaceae colonization (CRE) and subsequent risk of infection and 90-day mortality in critically ill patients, an observational study. PLoS One. 2017;12(10):e0186195. doi:10.1371/journal.pone.0186195
9. Tischendorf J, de Avila RA, Safdar N. Risk of infection following colonization with carbapenem-resistant Enterobactericeae: a systematic review. Am J Infect Control. 2016;44(5):539–543. doi:10.1016/j.ajic.2015.12.005
10. Giannella M, Freire M, Rinaldi M, et al. Development of a risk prediction model for carbapenem-resistant Enterobacteriaceae infection after liver transplantation: a multinational cohort study. Clin Infect Dis. 2021;73(4):e955–e966. doi:10.1093/cid/ciab109
11. Giannella M, Trecarichi EM, De Rosa FG, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae bloodstream infection among rectal carriers: a prospective observational multicentre study. Clin Microbiol Infect. 2014;20(12):1357–1362. doi:10.1111/1469-0691.12747
12. Wang Y, Lin Q, Chen Z, et al. Construction of a risk prediction model for subsequent bloodstream infection in intestinal carriers of carbapenem-resistant Enterobacteriaceae: a retrospective study in hematology department and intensive care unit. Infect Drug Resist. 2021;14:815–824. doi:10.2147/idr.S286401
13. Zhang L, Zhai W, Lin Q, et al. Carbapenem-resistant Enterobacteriaceae in hematological patients: outcome of patients with carbapenem-resistant Enterobacteriaceae infection and risk factors for progression to infection after rectal colonization. Int J Antimicrob Agents. 2019;54(4):527–529. doi:10.1016/j.ijantimicag.2019.06.023
14. Clinical and Laboratory Standards Institute, USA. Performance standards for antimicrobial susceptibility testing, M100 30th edition; 2020. Available from: https://clsi.org/standards/products/microbiology/documents/m100/.
15. Centers for Disease Control and Prevention. Facility guidance for control of carbapenem- resistant Enterobacteriaceae (CRE); 2015. Available from: https://www.cdc.gov/hai/pdfs/cre/CRE-guidance-508.pdf.
16. Wang L, Wang Y, Fan X, Tang W, Hu J. Prevalence of resistant gram-negative bacilli in bloodstream infection in febrile neutropenia patients undergoing hematopoietic stem cell transplantation: a single center retrospective cohort study. Medicine. 2015;94(45):e1931. doi:10.1097/MD.0000000000001931
17. Zhao Y, Lin Q, Liu L, et al. Risk factors and outcomes of antibiotic-resistant Pseudomonas aeruginosa bloodstream infection in adult patients with acute leukemia. Clin Infect Dis. 2020;71(Supplement_4):S386–S393. doi:10.1093/cid/ciaa1522
18. Komatsu T, Takahashi E, Mishima K, et al. A simple algorithm for predicting bacteremia using food consumption and shaking chills: a prospective observational study. J Hosp Med. 2017;12(7):510–515. doi:10.12788/jhm.2764
19. Concato J, Peduzzi P, Holford TR, Feinstein AR. Importance of events per independent variable in proportional hazards analysis. I. Background, goals, and general strategy. J Clin Epidemiol. 1995;48(12):1495–1501. PMID: 8543963. doi:10.1016/0895-4356(95)00510-2
20. Daikos GL, Markogiannakis A. Carbapenemase-producing Klebsiella pneumoniae: (when) might we still consider treating with carbapenems? Clin Microbiol Infect. 2011;17(8):1135–1141. doi:10.1111/j.1469-0691.2011.03553.x
21. Zhou C, Jin L, Wang Q, et al. Bloodstream infections caused by carbapenem-resistant Enterobacterales: risk factors for mortality, antimicrobial therapy and treatment outcomes from a prospective multicenter study. Infect Drug Resist. 2021;14:731–742. doi:10.2147/IDR.S294282
22. Kuiken NSS, Rings E, Blijlevens NMA, Tissing WJE. Biomarkers and non-invasive tests for gastrointestinal mucositis. Support Care Cancer. 2017;25(9):2933–2941. doi:10.1007/s00520-017-3752-2
23. Gudiol C, Bodro M, Simonetti A, et al. Changing aetiology, clinical features, antimicrobial resistance, and outcomes of bloodstream infection in neutropenic cancer patients. Clin Microbiol Infect. 2013;19(5):474–479. doi:10.1111/j.1469-0691.2012.03879.x
24. Yan CH, Xu T, Zheng XY, et al. 中国血液病患者中性粒细胞缺乏伴发热的多中心、前瞻性流行病学研究 [Epidemiology of febrile neutropenia in patients with hematological disease-A prospective multicentre survey in China]. Zhonghua Xue Ye Xue Za Zhi. 2016;37(3):177–182. Chinese. doi:10.3760/cma.j.issn.0253-2727.2016.03.001
25. Li C, Li Y, Zhao Z, Liu Q, Li B. Treatment options and clinical outcomes for carbapenem-resistant Enterobacteriaceae bloodstream infection in a Chinese university hospital. J Infect Public Health. 2019;12(1):26–31. doi:10.1016/j.jiph.2018.08.002
26. Cao W, Guan L, Li X, et al. Clinical analysis of bloodstream infections during agranulocytosis after allogeneic hematopoietic stem cell transplantation. Infect Drug Resist. 2021;14:185–192. doi:10.2147/IDR.S280869
27. Lin MY, Ray MJ, Rezny S, Runningdeer E, Weinstein RA, Trick WE. Predicting carbapenem-resistant Enterobacteriaceae carriage at the time of admission using a statewide hospital discharge database. Open Forum Infect Dis. 2019;6(12):ofz483. doi:10.1093/ofid/ofz483
28. Moghnieh R, Abdallah D, Jadayel M, et al. Epidemiology, risk factors, and prediction score of carbapenem resistance among inpatients colonized or infected with 3rd generation cephalosporin resistant Enterobacterales. Sci Rep. 2021;11(1):14757. doi:10.1038/s41598-021-94295-1
29. Taniguchi T, Tsuha S, Takayama Y, Shiiki S. Shaking chills and high body temperature predict bacteremia especially among elderly patients. Springerplus. 2013;2(1):624. doi:10.1186/2193-1801-2-624
30. Holmqvist M, Inghammar M, Pahlman LI, et al. Risk of bacteremia in patients presenting with shaking chills and vomiting - a prospective cohort study. Epidemiol Infect. 2020;148:e86. doi:10.1017/S0950268820000746
31. Gona F, Barbera F, Pasquariello AC, et al. In vivo multiclonal transfer of blaKPC-3 from Klebsiella pneumoniae to Escherichia coli in surgery patients. Clin Microbiol Infect. 2014;20(10):O633–O635. doi:10.1111/1469-0691.12577
32. Martin RM, Cao J, Brisse S, et al. Molecular epidemiology of colonizing and infecting isolates of Klebsiella pneumoniae. mSphere. 2016;1(5). doi:10.1128/mSphere.00261-16
33. Kocer K, Boutin S, Dalpke AH, Heeg K, Mutters NT, Nurjadi D. Comparative genomic analysis reveals a high prevalence of inter-species in vivo transfer of carbapenem-resistance plasmids in patients with haematological malignancies. Clin Microbiol Infect. 2020;26(6):780.e1–780.e8. doi:10.1016/j.cmi.2019.10.014
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.