Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Development of a Pulmonary Rehabilitation Patient Decision Aid for Patients with Chronic Obstructive Pulmonary Disease: Mixed Methods Study
Authors Jiang Y, Guo J, Chen M , Zou X, Sun P, Gao J , Nuerdawulieti B, Wang S
Received 5 October 2022
Accepted for publication 14 June 2023
Published 12 July 2023 Volume 2023:18 Pages 1377—1389
DOI https://doi.org/10.2147/COPD.S392191
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Yuyu Jiang,1 Jianlan Guo,2 Mengjie Chen,1 Xueqiong Zou,1 Pingping Sun,1 Jing Gao,1 Baiyila Nuerdawulieti,1 Shanshan Wang1
1Research Office of Chronic Disease Management and Rehabilitation, Wuxi School of Medicine, Jiangnan University, Wuxi, People’s Republic of China; 2Department of Nursing, Wuxi Higher Health Vocational Technology School, Wuxi, People’s Republic of China
Correspondence: Yuyu Jiang, Research office of chronic disease management and rehabilitation, Wuxi School of Medicine, Jiangnan University, No. 1800 Lihu Avenue, Wuxi, Jiangsu Province, People’s Republic of China, Tel +86-0510-85328363, Email [email protected]
Background: Pulmonary rehabilitation is an important part of the management of chronic obstructive pulmonary disease (COPD), but the participation rate of pulmonary rehabilitation in COPD patients is low. Patient decision aids can facilitate patient participation in pulmonary rehabilitation decisions by providing information and incorporating patient values. The aim of this study was to develop a pulmonary rehabilitation decision aid for patients with COPD.
Objective: The aim of this study was to develop a WeChat-based pulmonary rehabilitation patient decision aid to help older patients with COPD participate in pulmonary rehabilitation decision-making.
Methods: We developed the decision aid in 3 stages: (1) a literature review was performed to determine the evidence for pulmonary rehabilitation options and outcomes for patients with COPD. (2) a semi-structured interview study was conducted to develop and iterate patient decision aids. (3) usability, acceptability and language expression testing in patients and healthcare professionals.
Results: A total of 16 randomized controlled studies were included in the literature review. Thirty-six participants received semi-structured interviews. The results of interview include four themes: key points of age-friendly design, content of the tool, presentation requirements of contents and study evidence of the tool and other views and suggestions. The resultant goals-of-care decision aid achieved good usability and acceptability. The frequency of language expression increased in both patients and healthcare professionals.
Conclusion: This study uses a systematic development process to develop the first pulmonary rehabilitation decision aid for patients with COPD. It has good usability, acceptability and increased communication between patients and healthcare professionals in the pulmonary rehabilitation decision-making process.
Trial Registration: Chinese Clinical Trial Registry (ChiCTR): ChiCTR1900028563; http://apps.who.int/trialsearch/default.aspx.
Keywords: chronic obstructive pulmonary disease, shared decision making, pulmonary rehabilitation, patient decision aid
Introduction
The healthcare system needs to rapidly reform the delivery of healthcare services, following the outbreak of novel coronavirus disease 2019 (COVID-19).1 Telemedicine has become an important means of ensuring patients’ access to contactless healthcare services during the COVID-19 pandemic.2 The older population with chronic obstructive pulmonary disease (COPD) is at high risk of susceptibility during the pandemic.3 Therefore, older patients with COPD should be provided with healthcare services based on contactless remote service mode to ensure their safety.
Shared decision-making (SDM) is a desirable component of clinical decision-making, a decision-making process in which both physicians and patients reach consensus through communication based on evidence.4,5 Sharing decision is a key strategy to promote patients’ participation in medical decision-making, which can improve the quality of clinical decision-making.6,7 Recently, SDM has become an important means to promote patient participation in rehabilitation services and improve patient adherence to rehabilitation in rehabilitation management.8,9 In addition, patient decision aids (PtDAs) is an important part of SDM and can help patients make informed choices about healthcare.10
Pulmonary rehabilitation is a core component of the management of COPD patients, yet low participation rates and difficulties in adherence are pressing challenges in the implementation of pulmonary rehabilitation.11,12 Studies pointed to the need to integrate SDM into pulmonary rehabilitation services.13,14 However, little research has been found on the application of SDM in pulmonary rehabilitation and no decision aids for pulmonary rehabilitation have been developed.
The identification and processing of patient preferences by physicians and encouraging patients’ to express preferences are the difficulties of implementing SDM.15,16 Using effective communication skills to solve the above problems is a worthwhile way to try.15 Existing studies on the expression of preferences in SDM mostly focused on patients’ role preferences and preference selection in medical decision-making, and there are few studies on the use of communication skills to encourage patients’ expression of preference and to help physicians’ identification and processing of patient preferences.17–19
Non-Violent Communication (NVC) is a communication skill that emphasizes stimulating friendship and creating harmonious relationships. In NVC, the communication process is combined with two parts: “expression” and “listening”, and “expression” are subdivided into four components: “observation”, “feeling”, “needs” and “request”. It helps to express oneself honestly and clearly while respecting and listening to others through a detailed reading of these parts and components.20 This communication skill may help facilitate patient expression, improve the chances of healthcare professionals (HCPs) identifying patient preferences, and increase communication and information sharing between patients and HCPs to achieve true SDM.
This study proposed to develop a WeChat-based pulmonary rehabilitation PtDAs for older patients with COPD. Wechat is a free mobile application that is widely used in China and functions like social media (like Facebook). The study also tested the acceptability and usability of the PtDAs. Aiming to provide decision support for COPD patients facing pulmonary rehabilitation decision-making. NVC skills were incorporated in the communication skills training of the PtDAs to motivate patients to participate in the pulmonary rehabilitation decision-making process, to actively express their personal preferences in the decision-making process, to improve the quality of medical decision-making and to promote patient participation in pulmonary rehabilitation.
Materials and Methods
From December 2020 to March 2022, we used a mixed methods approach to develop a PtDAs for pulmonary rehabilitation. First, a meta-analysis of outcome indicators from the pulmonary rehabilitation in older patients with COPD studies was conducted and the results of the data analysis were rated by GRADE. Secondly, the paper-based patient decision aid was developed according to Ottawa Personal Decision Guide(OPDG),21 and was iterated through semi-structured interviews. Thirdly, the content modules of the paper-based patient decision aid were presented on a WeChat Official Account. Fourth, WeChat-based patient decision aid tested, including expression testing of patients and HCPs. Finally, the usability and acceptability of the PtDAs were tested.
This study was approved by the Medical Ethics Committee of Jiangnan University (JNU20200109IRB01) and was registered in the Chinese registry of clinical trials (ChiCTR1900028563). All subjects signed informed consent before participating in the study. The participants informed consent included publication of anonymized responses.
Meta-Analysis and GRADE Rating
Data Sources and Searches
A meta-analysis of outcome indicators of pulmonary rehabilitation interventions in older patients with COPD was conducted and the results of the data analysis were rated with GRADE. We searched for clinical randomised controlled trials (RCTs) in Embase, Cochrane Library, PubMed, CNKI, Wanfang and VIP for the last decade. The retrieval form of the Medical Subject Headings (Mesh): [Pulmonary Disease, Chronic Obstructive] and [Aged] and [Pulmonary rehabilitation or lung rehabilitation or lung therapy or pulmonary treatment or rehabilitation program].
Selection Criteria
The inclusion criteria for RCTs were as follows: (1) Randomized-controlled trials; (2) COPD was definitely diagnosed by medical units; (3) age ≥60 years; (4) The intervention group was given pulmonary rehabilitation training, consisting mainly of exercise training or (and) respiratory training, in addition to disease promotion, nutritional support, and psychosocial rehabilitation; (5) Outcomes: CAT (COPD Assessment Test), 6MWD (6-minute walking distance), SGRQ (St George’s Respiratory Questionnaire), FEV1% (pre) (Forced Expiratory Volume in the first second).
Date Extraction and Data Analysis
Meta-analysis of the studies included was performed using Review manager 5.3 statistical software, and GRADE was used to rate the level of evidence. The screening of research literature and the data extraction was conducted by two researchers (M.C. and X.Z.). A third researcher (Y.J.) was consulted when differences in opinions occurred.
Develop and Iterate Patient Decision Aid
We designed the first draft of the paper-based PtDAs (The paper-based PtDAs has been uploaded in Patient Decision Aids-Ottawa Hospital Research Institute. It is available on http://wxms.jiangnan.edu.cn/info/1028/1610.html), with eight sections contained: (1) Know about COPD; (2) Treatments of COPD; (3) Understanding Pulmonary Rehabilitation; (4) Choices you face; (5) Comparison of different choices; (6) Attention points of Pulmonary Rehabilitation; (7) Your thoughts; (8) Your final decisions. The evidence base was informed by evidence-based guidelines for pulmonary rehabilitation, GOLD (Global Initiative for Chronic Obstructive Lung disease) 2020, results of meta-analysis and GRADE rating. The first draft of the paper version of PtDAs is formed.
Paper-based PtDAs iteration was carried out by interview. The interviewees included respiratory physicians, clinical nurses, older patients with COPD who undergone and not undergone pulmonary rehabilitation, and family members. The interviewees were recruited by oral recruitment and HCP recommendations from third class A general hospital. The inclusion criteria for patients: (1) age ≥60 years; (2) confirmed diagnosis of chronic obstructive pulmonary disease according to the diagnosis and treatment guidelines for chronic obstructive pulmonary disease;22 (3) clear consciousness; and (4) ability to communicate in Chinese. The inclusion criteria for HCPs: (1) pulmonary rehabilitation professionals; (2) involvement in the treatment or care of pulmonary rehabilitation. The inclusion criteria for family members: (1) experience in caring for older patients with COPD; (2) ability to communicate in Chinese. Participants were interviewed face-to-face through semi-structured interviews. Interviewees were asked about the content of information patients needed to know to decide whether to participate in pulmonary rehabilitation, the important factors that they considered in the decision-making process for pulmonary rehabilitation, and their perspective and feelings about the paper-based PtDAs. The interviews focused on the following: (1) the main points of age-friendly design of PtDAs, (2) what PtDAs should contain, (3) the presentation of the tool, the content of the tool and risk evidence, (4) views and suggestions on PtDAs. After every 3–4 interviews, team members initiated group discussions on interviewee feedback and suggestions, revised and iterated on the paper-based PtDAs, and used the iterated PtDAs to conduct the next round of qualitative interviews. Each interview was recorded (with permission), and the transcribed text was analysed with themes were extracted. The interview and analysis process continued until data saturation occurred with no new themes formed.
Then, the WeChat PeR23 Official Account was used as a carrier to display the content module of the paper-based PtDAs, which consisted of three parts: (1) Moments: providing decision aid for patients through others’ decision-making experiences and rehabilitation experiences; (2) Pulmonary Rehabilitation Options: containing two sections on whether to participate in pulmonary rehabilitation and knowledge expansion; and (3) Training of communication: coaching patients and HCPs on methods of communication and expression based on NVC theory.20
(1) Moments
The decision-making or rehabilitation experience of others can help patients to make better judgements about what is right for them. By comparing other people’s health conditions and rehabilitation outcomes, the patient’s understanding of the pulmonary rehabilitation programme can be improved and the “best” decision can be made to suit the patient better.
1) Process and content of recruitment: Data from patients was collected using a rehabilitation experience collection form designed by the research team. Data included gender, age, disease diagnosis, duration of illness, lung function, CAT score, treatment experienced and perception of the treatment, changes in physiological condition (eg symptoms, mobility), daily living, emotion and social support status before and after the rehabilitation intervention.
2) Production and publication: The researcher created an account at the moment and named it “Rehabilitation Kiosk”. The researcher wrote a structured rehabilitation story (my situation, my past, my changes and my feelings) based on the collection form. The research team reviewed the objective expression of the language of the rehabilitation story. Finally, the researcher published the story through the account “Rehabilitation Kiosk” with the story confirmed by the patient.
(2) Training of communication skills
Communication skills training module was constructed using the three elements (expressing, observing and listening) of NVC.20 The module was divided into two parts: I am a patient and I am a professional. Through learning and completing exercises, patients and HCPs learn how to use the appropriate language to express their feelings and thoughts, how to express things or events in objective terms (eg frequency, time, place, person) and to avoid using judgmental language. Professionals need to understand the patient’s feelings and needs correctly, be able to give correct feedback using interrogative statements and ultimately recognize the patient’s feelings and needs.
The structured content of the training includes concept interpretation, example demonstration, judgment of statements that express personal feelings, judgment of statements that distinguish observation from comment, and practice training. Example demonstration is to analyze the expression statements in narrative cases without critical analysis. Patients and HCPs are required to accurately complete the practice training and pass the test.
(3) Pulmonary Rehabilitation Options
The module “Pulmonary Rehabilitation Options” includes two sections: whether to participate in pulmonary rehabilitation and knowledge expansion.
1) Whether to participate in pulmonary rehabilitation: the content of this section includes disease information, pulmonary rehabilitation information, choices faced, comparison of the costs and rewards of the two choices, comparison of the research evidence of the two choices, important considerations of pulmonary rehabilitation and final decision confirmation. The expression of the incidence of benign outcomes in the research evidence of the two choices was expressed as a bar chart.
2) Knowledge expansion: The “knowledge expansion” section introduces the knowledge related to disease and pulmonary rehabilitation in detail, which was written and uploaded by the research members. The “knowledge expansion” section was presented both in graphics and video, allowing patients to choose their own preferred format.
Update of materials: The content of “knowledge expansion” was updated every month, and research evidence was reviewed and updated by researchers every month.
Usability, Acceptability and Language Expression Test
The self-designed acceptability questionnaire of PtDAs and the validated System Usability Scale (SUS)24 were used to investigate the acceptability and usability of PtDAs by stakeholders. The acceptability questionnaire of PtDAs consisted of 11 items, including readability, operability, comprehensiveness (including its length and content) and ability to solve goal decisions. The SUS scale measured the availability of the tool. The SUS scale is a 10-item Likert scale with scores ranging from 0 to 100 (higher scores indicate higher availability). Among the items, 1,3,5,7,9 are positive questions, while 2,4,6,8,10 are reverse questions. There is a high correlation between the 10 questions. The higher SUS score represents the better product availability. SUS≥71 is the accepted standard for good usability.
The methods of language expression test are mainly derived from NVC and discussion coding systems. The core of NVC skills training is the facilitation of expression, in order to recognize changes in expression during the communication process between physicians and patients. Based on the definition of the four elements (observation, comment, need and feeling) in NVC theory, we calculated the number of expressions of the four elements in the communication between patients and HCPs before and after training.20 We then calculated the frequency of expressions of observation, comment, imperative, needs and feeling statements by patients and HCPs based on a discussion coding system.25 It is calculated by dividing the sum of each statement of the individual by the sum of all statements of the individual.
In addition, other suggestions from the participants were used for further iterations and revisions of the tool.
Results
Results of Meta-Analysis and GRADE Rating
The final study on pulmonary rehabilitation in older COPD patients included 23 RCTs, mostly conducted in China and published between 2011 and 2021, in which the experimental group underwent appropriate pulmonary rehabilitation and the control group used conventional treatment and care. The literature screening process can be seen in Supplementary Figure 1. The characteristics of the studies can be seen in Supplementary Table 1. The results of Meta-analysis can be seen in Supplementary Figure 2-8. The results of GRADE Rating can be seen in Supplementary Table 2 and Supplementary Figure 9. The results of the 6MWD had high certainty. The certainty for CAT, FEV1 (Pre) and SGRQ was moderate.
Results of Interviews
A total of 36 participants received semi-structured interviews, including 12 HCPs, 13 older patients with COPD and 11 family caregivers of patients (see Supplementary Table 3 for the table of general information about participants). Four themes were identified: (1) age-friendly design points to consider for decision aids; (2) tool content needs; (3) requirements for tool content presentation and evidence presentation; and (4) other views and suggestions. Table 1 provides the results of interviews.
 |
Table 1 Results of Qualitative Interview |
Results of the Test
A total of 45 participants completed the alpha test of the WeChat version of PtDAs. General information on 22 older patients with COPD, 6 family caregivers and 17 HCPs is presented in the Supplementary Table 4.
The SUS scale scores are shown in Figure 1. The results of the acceptability survey are shown in Table 2.
 |
Table 2 Acceptability of PtDAs Among Study Participants |
 |
Figure 1 The SUS scale scores. |
Results of Language Expression Test
The means and standard deviations of the number of observation statements, comment statements, imperative statements, statements expressing needs and statements expressing feeling spoken by patients and HCPs are shown in Table 3 and Table 4. The frequency of expressions of observation statements, commentary statements, statements expressing feeling and statements expressing needs increased for patients. The frequency of expressions of observation statements, statements expressing feeling and statements expressing needs increased for health professionals, while the frequency of expressions of commentary and imperative statements decreased.
 |
Table 3 Results of Language Expression Test for Patients |
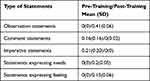 |
Table 4 Results of Language Expression Test for HCPs |
Discussion
To our knowledge, this is the first decision aid developed to facilitate decision-making in pulmonary rehabilitation for older patients with COPD. The study emphasized that the methods to developing a web-based educational resource should include an extensive review of existing resources, literature exploration on patient education and website development, interviews with patients and clinical experts, and the development and pilot testing of tools.26 These methods can facilitate informed and supported decision-making. We applied these methods to create high-quality decision aid that met international quality standards for decision aids and demonstrated a high level of acceptability and usability. These methods can be used as a reference for the development of other PtDAs.
Studies have pointed out that decision aids that present narrative information enhance patients’ processing and use of health information more than that present textual information.26 Therefore, several studies have used story information in decision aids to promote facts and key considerations more understandable.26–28 However, Bekker et al29 noted in the review that current evidence of the impact of narrative personal stories on the effectiveness of decision aids is insufficient. Moreover, it is unclear how to maximise the role of personal stories and factual information in patient information processing to ensure that patients’ healthcare decisions are supported rather than biased. In order to ensure that the information is processed objectively in this study, the story messages are presented using the observational and objective language in NVC. Further, a structured story framework is used to describe personal stories to avoid the potential criticism of bias that can influence the decision-making process.20 However, the effectiveness of structured story messages needs to be further explored.
The results of the qualitative study suggested that the language used in the tool, with the patient as the first person, is more likely to allow the patient to perceive the content of the message, eg replacing “improve your breathing” with “make you breathe better”, which is in line with the content of prospect theory.30 Prospect theory states that decision makers study risk primarily in terms of perceived decision gains and losses, and that the decision makers’ perceptions and attitudes towards the message provided will influence decision-making behavior.31 As a result, different ways of presenting the same message may lead decision makers to adopt different decision-making behavior, especially when decision makers encounter difficult decisions where their irrational factors may dominate. The messages in the tool developed in this study are presented as verbally as possible from the patient’s perspective to increase the patient’s perception of the content of the messages in order to facilitate the patient’s health behavioural decisions.
The study highlighted the need for better PtDAs to be developed in clinical practice to diagnose and respond to patient preferences.16 To date, most PtDAs are designed to help clarify patient preferences by articulating treatment options, the value balance of benefits and risks (balancing benefits and risks), and clarifying important considerations in decision-making.31–33 These approaches have helped patients clarify their preferences through informational means, neglecting patient’s own initiative. Some studies have pointed out that an important challenge in SDM is the need to use communication skills to stimulate the patient’s internal preferences.15 In addition, older people are less likely to be involved in the decision-making process than younger people.34 Therefore, this study uses NVC techniques to facilitate patients’ expression of preferences and to help HCPs identify preferences. Previous research has demonstrated that by applying training and practice in NVC theory, participants can learn to feel emotions and express their attitudes towards values, and can better identify the feelings and needs of others.35,36 The study designed a communication training course for patients and HCPs based on NVC theory. The aim was to facilitate patient expression and to help HCPs to recognise and give feedback to patients’ expressions in a timely manner. Our observational measurement of verbal and expressive behaviour of trained healthcare professionals and patients using a discussion coding system, we demonstrated that training based on NVC significantly increased the expression of needs by HCPs and patients.37 At present, we are not aware of any studies using verbal and behavioural measures to validate the effects of decision aids, which may provide ideas for future research related to decision aids.
The way in which messages are presented can influence patients’ decision-making behavior. The study published in JAMA noted that participants’ perception of disease risk and willingness to receive treatment was significantly lower when the same disease risk estimates were displayed with a facial graphic compared to a bar chart or no graphic.38 Therefore, we used bar charts to show the probability of risk for different outcomes. In addition, older patients expressed a preference for larger values to represent better results and smaller values to represent worse results in the presentation of the data. They felt that this type of presentation was better for understanding, which deserves the attention of researchers developing decision aids for older people in the future. Some of the older patients also wanted us to change the option “refuse pulmonary rehabilitation” to “do not participate in pulmonary rehabilitation”, saying that they preferred the simple and clear language of “yes” or “no” in the decision-making process.
Limitations
This study had some limitations. Validation of the effectiveness of the decision aid is lacking in this study. This decision aid is not yet suitable for participants whose native language is not Chinese, as PtDAs have not been translated or validated in this population. Future studies could consider translating PtDAs into English and validating the translated PtDAs. Moreover, respondents of alpha test may have some bias, as some of them have already known the researchers. Finally, we plan to collaborate with other experts in the field to determine which outcome measures are appropriate and clinically meaningful for validation testing.
Conclusions
In this mixed method study, we developed a pulmonary rehabilitation patient decision aid for older patients with chronic obstructive pulmonary disease. This study innovatively applied NVC theory in the decision aid. The results showed the decision aid has good usability, acceptability and increased communication between patients and healthcare professionals in the pulmonary rehabilitation decision-making process.
Abbreviations
COPD, chronic obstructive pulmonary disease; SDM, shared decision-making; PtDAs, patient decision aids; NVC, non-violent communication; HCPs, healthcare professionals; OPDG, Ottawa Personal Decision Guide; RCTs, randomised controlled trials; SUS, System Usability Scale.
Data Sharing Statement
The data that support the findings of this study are available from http://apps.who.int/trialsearch/default.aspx.
Ethics Approval
This study was approved by the Medical Ethics Committee of Jiangnan University (JNU20200109IRB01) and conducted in line with Helsinki Declaration principles.
Informed Consent
Informed consent has been provided by all participants.
Acknowledgments
This study was supported by the Wuxi Municipal Bureau on Science and Technology (CN) (Grant N20192046) and National Natural Science Foundation of China (72274080). The authors are grateful for the assistance of the hospitals and wish to extend special thanks to all interviewees.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020;323(23):2375–2376.
2. Omboni S, Ballatore T, Rizzi F, et al. Telehealth at scale can improve chronic disease management in the community during a pandemic: an experience at the time of COVID-19. PLoS One. 2021;16(9):e0258015.
3. Olloquequi J. COVID-19 Susceptibility in chronic obstructive pulmonary disease. Eur J Clin Invest. 2020;50(10):e13382.
4. Hart J, Yadav K, Szymanski S, et al. Choice architecture in physician-patient communication: a mixed-methods assessments of physicians’ competency. BMJ Qual Saf. 2021;30(5):362–371.
5. While A. Shared decision-making. Br J Community Nurs. 2019;24(5):250.
6. Jayakumar P, Moore MG, Furlough KA, et al. Comparison of an Artificial Intelligence-Enabled Patient Decision Aid vs Educational Material on Decision Quality, Shared Decision-Making, Patient Experience, and Functional Outcomes in Adults With Knee Osteoarthritis: a Randomized Clinical Trial. JAMA Netw Open. 2021;4(2):e2037107.
7. Mccarus SD, Wiercinski K, Heidrich N. Shared decision-making to improve patient engagement in minimally invasive hysterectomy. Surg Technol Int. 2019;34:265.
8. Faller H. Shared decision making: an approach to strengthening patient participation in rehabilitation. Rehabilitation (Stuttg). 2003;42(3):129–135.
9. Rose A, Rosewilliam S, Soundy A. Shared decision making within goal setting in rehabilitation settings: a systematic review. Patient Educ Couns. 2017;100(1):65–75.
10. Joseph-Williams N, Abhyankar P, Boland L, et al. What Works in Implementing Patient Decision Aids in Routine Clinical Settings? A Rapid Realist Review and Update from the International Patient Decision Aid Standards Collaboration. Med Decis Making. 2021;41(7):907–937.
11. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13–64.
12. Alison JA, Mckeough ZJ, Johnston K, et al. Australian and New Zealand Pulmonary Rehabilitation Guidelines. Respirology. 2017;22(4):800–819.
13. Jiang Y, Guo J, Sun P, et al. Perceptions and experiences of older patients and healthcare professionals regarding shared decision-making in pulmonary rehabilitation: a qualitative study. Clin Rehabil. 2021;35(11):1627–1639.
14. Madsen C, Tomkinson J. P120 Shared Decision Making In A Pulmonary Rehabilitation Setting For COPD Patients. Thorax. 2014;69(Suppl 2):A130–A1.
15. Kopecky KE, Urbach D, Schwarze ML. Risk calculators and decision aids are not enough for shared decision making. JAMA Surg. 2019;154(1):3–4.
16. Elwyn G, Cochran N, Pignone M. Shared decision making-the importance of diagnosing preferences. JAMA Intern Med. 2017;177(9):1239–1240.
17. Shinkunas LA, Klipowicz CJ, Carlisle EM. Shared decision making in surgery: a scoping review of patient and surgeon preferences. BMC Med Inform Decis Mak. 2020;20(1):190.
18. Cho HE, Baxter NB, Billig JI, et al. Task-specific patient preferences for shared decision-making in hand surgery. Plast Reconstr Surg. 2022;149(2):229e–39e.
19. Alokozai A, Eppler SL, et al. Patient preferences for shared decision making: not all decisions should be shared. J Am Acad Orthop Surg. 2020;28(10):419–426.
20. Rosenberg MB, Chopra D. Nonviolent Communication: A Language of Life: Life-Changing Tools for Healthy Relationships [M]. PuddleDancer Press; 2015.
21. Hoefel L, Lewis KB, O’connor A, et al. 20th anniversary update of the Ottawa decision support framework: part 2 subanalysis of a systematic review of patient decision aids. Med Decis Making. 2020;40(4):522–539.
22. Chronic obstructive pulmonary disease group, respiratory branch, Chinese Medical Association. Guidelines for diagnosis and treatment of chronic obstructive pulmonary disease (2013 Revision). Chine J Med Front. 2014;2(02):67–80.
23. Jiang Y, Liu F, Guo J, et al. Evaluating an intervention program using wechat for patients with chronic obstructive pulmonary disease: randomized controlled trial. J Med Internet Res. 2020;22(4):e17089.
24. Brooke J. Sus: a quick and dirty’usability. Usability Evaluation Industry. 1996;189(3):564.
25. Schermuly CC, Scholl W. The Discussion Coding System (DCS)—A new instrument for analyzing communication processes. Commun Methods Meas. 2012;6(1):12–40.
26. Hawkins Virani AK, Creighton SM, Hayden MR. Developing a comprehensive, effective patient-friendly website to enhance decision making in predictive testing for Huntington disease. Genet Med. 2013;15(6):466–472.
27. Shaffer VA, Focella ES, Scherer LD, et al. Debiasing affective forecasting errors with targeted, but not representative, experience narratives. Patient Educ Couns. 2016;99(10):1611–1619.
28. Mcqueen A, Kreuter MW, Kalesan B, et al. Understanding narrative effects: the impact of breast cancer survivor stories on message processing, attitudes, and beliefs among African American women. Health Psychol. 2011;30(6):674–682.
29. Bekker HL, Winterbottom AE, Butow P, et al. Do personal stories make patient decision aids more effective? A critical review of theory and evidence. BMC Med Inform Decis Mak. 2013;2(Suppl 2):S9.
30. Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk [M]. Handbook of the fundamentals of financial decision making: part I. World Scientific. 2013;2:99–127.
31. Greenhawt M, Shaker M, Winders T, et al. Development and acceptability of a shared decision-making tool for commercial peanut allergy therapies. Ann Allergy Asthma Immunol. 2020;125(1):90–96.
32. Chabrera C, Font A, Caro M, et al. Developing a decision aid to support informed choices for newly diagnosed patients with localized prostate cancer. Cancer Nurs. 2015;38(1):E55–60.
33. Ankolekar A, Vanneste BGL, Bloemen-Van Gurp E, et al. Development and validation of a patient decision aid for prostate Cancer therapy: from paternalistic towards participative shared decision making. BMC Med Inform Decis Mak. 2019;19(1):130.
34. Van Weert JC, Van Munster BC, Sanders R, et al. Decision aids to help older people make health decisions: a systematic review and meta-analysis. BMC Med Inform Decis Mak. 2016;16(45):e6.
35. Nosek M, Durán M. Increasing Empathy and Conflict Resolution Skills through Nonviolent Communication (NVC) Training in Latino Adults and Youth. Prog Community Health Partnersh. 2017;11(3):275–283.
36. Museux AC, Dumont S, Careau E, et al. Improving interprofessional collaboration: the effect of training in nonviolent communication. Soc Work Health Care. 2016;55(6):427–439.
37. Yilmaz NG, Van Weert JCM, Peters E, et al. Testing the effects of modality and narration style on patients’ information use in a lung cancer treatment decision aid. Med Decis Making. 2020;40(8):990–1002.
38. Navar AM, Wang TY, Mi X, et al. Influence of cardiovascular risk communication tools and presentation formats on patient perceptions and preferences. JAMA Cardiol. 2018;3(12):1192–1199.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
