Back to Journals » Advances in Medical Education and Practice » Volume 10
Development of a “Surgical Shadowing Scheme” to improve undergraduate experiences of surgery
Authors Bartlett RD , Momin SMB , Azam S , Rotimi O , Quick TJ
Received 12 February 2019
Accepted for publication 3 June 2019
Published 13 August 2019 Volume 2019:10 Pages 619—626
DOI https://doi.org/10.2147/AMEP.S205054
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Richard D Bartlett,1,* Sheikh MB Momin,1,* Saima Azam,1 Oloruntobi Rotimi,1 Tom J Quick1,2
1UCL Medical School, University College London, London WC1E 6BT, UK; 2Peripheral Nerve Injury Unit, Royal National Orthopedic Hospital NHS Trust, Stanmore, HA7 4LP, UK
*These authors contributed equally to this work
Purpose: To establish a sustainable model for a “Surgical Shadowing Scheme” (SSS) and assess how this affects undergraduate attitudes to surgical careers.
Patients and methods: Surgeons at university teaching hospitals associated with UCL Medical School and UCL Partners, United Kingdom, were approached for their willingness to participate in the scheme. Medical students were then invited to apply for the scheme, where students were individually matched to operating theater sessions with surgeons in their specialty of choice. Feedback was subsequently obtained, evaluating experiences of the placement and the effect this had on future career aspirations.
Results: After running for four consecutive years, approximately 220 students have participated in the scheme across a range of surgical units and specialties. A total of 91.5% of the students were pre-clinical (years 1–3), whilst the remainder were clinical (years 4–6). Fifty-four percent were female and 46% male. Eighty-three percent of the students did not have any previous experience of the specialty that they shadowed, and 67% agreed that participating in the scheme had either “increased” or “strongly increased” their desire to pursue a surgical career. Ninety-four percent said they would “recommend” or “strongly recommend” the SSS to a peer. Over a third of students reported scrubbing-up during their placements and 35% of these directly assisted the lead surgeon. Traditionally male-dominated surgical sub-specialties recruited a high proportion of female students.
Conclusion: This is the first published example of an established “Surgical Shadowing Scheme” for medical undergraduates. Our SSS has been highly valued by students and indicates that even a single high-quality surgical exposure is sufficient to increase the desire of undergraduates to pursue a surgical career. We hope that this SSS will act as a blueprint for other centers to develop their own shadowing schemes, in turn helping to ensure that surgery continues to inspire and attract the very best candidates for the future.
Keywords: Surgical Shadowing Scheme, surgical education, medical education, medical student, surgical careers, women in surgery
Introduction
The popularity of surgery as a career choice in the United Kingdom has decreased in recent years.1 Undergraduate experiences of surgery are known to closely correlate with future career choice, with positive experiences of surgery during medical school increasing the desire of students to enter surgical training.2 Undergraduates may be dissuaded from considering surgical careers by a number of negative pre-conceptions,3 but gender, exposure to appropriate surgical rotations and “fit” within the culture of surgery are likely to be important.4 Early exposure to positive role models has been shown to overcome inaccurate stereotypes and reduce negative pre-conceptions that students may have.3
Despite this, undergraduates may find it challenging to identify enthusiastic surgical mentors or gain early surgical exposure. Making contact with surgeons and assessing their willingness to allow students in the operating theater can be difficult. These logistical factors act as barriers to gaining high-quality early surgical exposure during medical school. This is particularly true for medical schools with “traditional” curricula, where there is often a divide between pre-clinical and clinical years. During pre-clinical years there is often no exposure to surgery, and even during clinical years, there may be very limited opportunities to explore specific surgical sub-specialties of interest. Even for proactive students, the administrative burden associated with facilitating one-off placements can disincentivize surgeons from offering attachments and limit the shadowing opportunities available to students.
We have developed and piloted a novel “Surgical Shadowing Scheme” (SSS) at University College London, United Kingdom, aiming to overcome many of the logistical challenges associated with students gaining access to high-quality surgical exposure. This scheme is now in its fourth consecutive year of running, yet, to the best of our knowledge, it remains the first and only scheme of its kind.
Methods
Consultant surgeons at local teaching hospitals were approached for their willingness to participate in the scheme and briefed about the expectations of encouraging positive student engagement in the operating theatre. In return, the medical school Surgical Society provided a centralized student-lead (a Shadowing Scheme Co-ordinator) to oversee the running of scheme and interface between students and surgeons. This minimized any administrative burden placed on surgeons and allowed any frequently asked questions from students to be dealt with in-house.
Regular operating slots were obtained from surgeons, and these were uploaded by the Shadowing Scheme Co-ordinator to a centralized online calendar booking system. Students who wished to participate in the scheme could then book a shadowing slot for a surgical sub-specialty of interest. Shadowing sessions were allocated on a first-come first-served basis, with each student being limited to one shadowing session per term unless there were unfilled sessions or students wished to participate in other specialties that had capacity. Students who had not previously participated in the scheme were given priority. Closer to the time of the placement, the Shadowing Scheme Co-ordinator sent detailed joining instructions to students. At this stage, they also performed a final check to reduce the risk of non-attendance by participating students, and provided an emergency contact telephone number in case of any last-minute problems. Where possible, summaries of the procedures on the operating list for the day of shadowing sessions were sent in advance as part of the joining instructions. For example, students would be told there was one Roux-en-Y bypass case and one esophagojejunostomy case etc., although no personally identifiable patient information was circulated. This allowed students to pre-read around the likely pathologies and specific surgical techniques that they may encounter, and aimed to increase student confidence, participation, and engagement during shadowing sessions.5,6
The scheme was closely evaluated and audited from the outset. Following each individual student placement, the quality of the shadowing session was audited. During the first year of running, the Shadowing Scheme Co-ordinator individually contacted each student after their session by email to gain qualitative feedback and highlight any logistical problems. After one continuous year of running, evaluation of the scheme switched to use a quantitative online questionnaire. This explored various metrics, including previous exposure to surgery, value of the surgical session provided by the SSS, and whether participating in the SSS had influenced future career choice. The questionnaire clearly stated that participant responses may later be anonymously pooled for analysis.
Anonymized data were exported to Microsoft Excel and analyzed using IBM SPSS Statistics 22.0 (IBM Inc. Armonk, NY). Where appropriate, data were assessed for normality and equality of variance was tested using Levene’s statistic. Statistical tests were deemed to be significant at the 5% level.
Results
Over four years, approximately 220 students have participated in the SSS. Of the 180 students who were sent the evaluative questionnaire, approximately 140 completed it, indicating a response rate of 77.7%.
All major surgical sub-specialties were secured to provide shadowing slots for students, including general surgery, vascular surgery, neurosurgery, pediatrics, ENT, trauma and orthopedics, cardiothoracics, oral and maxillofacial, urology, and obstetrics and gynecology. However, the greatest number of shadowing sessions were undertaken in neurosurgery (26%) and cardiothoracic surgery (26%), followed by plastic surgery (13%) and trauma and orthopedics (13%), respectively (Figure 1A).
Of the students who participated in our scheme, there was a reasonably even split between male and females, with slightly more female students participating in the scheme than males (53.9% vs 46.1%, respectively) (Figure 2A). There was also a higher proportion of female students than male students opting for placements in neurosurgery (15.0% vs 11.4%), trauma and orthopedics (10.0% vs 2.86%), and maxillofacial surgery (3.6% vs 0%) (Figure 1B). The overwhelming majority of students participating in the scheme were from pre-clinical years of medical school, with only 8.5% of the respondents having already completed clinical placements (Years 4–6) (Table 1). Consequently, 83% of the students did not have any previous exposure to the specialty that they shadowed prior to the shadowing session, although 17% did report some previous experience (Figure 2B).
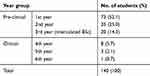 |
Table 1 Breakdown of students participating in the shadowing scheme by medical school year group |
When on shadowing sessions, the majority of students reported staying in the operating theater for at least 6 hrs (31%), with only 11% of the students staying less than 3 hrs (Figure 2C). The majority of students did not scrub-up (61%) during their shadowing sessions, although 39% reported that they were able to scrub-up. Of those who did scrub-up, 92.7% were pre-clinical students, broadly in line with the proportion of pre-clinical students overall, and 35% reported being able to directly assist the lead surgeon during procedures (Figure 2D).
Feedback from students participating in the shadowing scheme was overall extremely positive. Ninety-four percent of the students stated that they would either “recommend” or “strongly recommend” the shadowing scheme to a peer. Similarly, when assessed using a 5-point Likert scale, students indicated that participating in the scheme significantly improved their understanding of the sub-specialty that they shadowed (median difference =1, p<0.001) (Figure 3A). The majority of students (69%) also indicated that participating in a one-off session as part of the shadowing scheme had “increased” or “strongly increased” their desire to pursue a surgical career in the future (Figure 3B).
Discussion
Over a consecutive four-year period, approximately 220 students have participated in the SSS, gaining exposure to a range of surgical specialties. Owing to the unique infrastructure and teaching hospitals surrounding UCL Medical School, placements were offered in all major surgical sub-specialties at a range of world-leading specialist units, including the National Hospital for Neurology and Neurosurgery, Great Ormond Street Hospital for Children, the Royal National Orthopaedic Hospital, The Heart Hospital, and the Royal National Throat, Nose and Ear Hospital.
Interestingly, the majority of students participating in our scheme have been in their pre-clinical years, meaning that they did not have any major previous clinical attachments or internships. This may reflect a desire amongst pre-clinical students for increased early surgical exposure. Indeed, in recent years there has been a shift away from traditional medical curricula with a distinct pre-clinical/clinical divide, instead focusing on developing courses that incorporate increased early clinical exposure.7 The high proportion of students participating in our scheme from the first year of the medical school course may also reflect that students found the scheme an easy and accessible way of securing surgical exposure in sub-specialties of interest, overcoming some of the challenges typically associated with pre-clinical students making first contact with surgeons and entering the clinical environment. Additionally, the two most popular specialties shadowed – neurosurgery and cardiothoracic surgery – tend to receive minimal exposure in the medical school curricula,8,9 suggesting that the scheme may provide unique opportunities that are not otherwise available to undergraduates. Indeed, some proactive clinical students may have used opportunities afforded by the scheme to gain exposure to a particular specialty of interest, perhaps in order to show commitment to specialty for competitive surgical applications or to develop a network of mentors for future career advice. In the future, it may be interesting to explore the reasons clinical students cite for participating in the scheme.
Our data also suggest that there was a reasonably equal split between male and female students participating in the scheme. This is interesting as there has traditionally been a strong male bias in a number of surgical specialties, despite UCL Medical School cohorts being 51% female for the years 2013–17 and national UK medical school intake now being approximately 55% female.10 Indeed, it is estimated that around only 12% of the consultant surgeons are female, with sub-specialties such as trauma and orthopedics and cardiothoracic surgery displaying a particular male gender bias.11 In contrast, our results suggest that, at least early on during medical school, female students are equally as motivated as male students to seek out and undertake surgical shadowing opportunities. This challenges the assumption that male students are more likely to be interested in surgery.12 Even in very male-dominated sub-specialties such as neurosurgery and trauma and orthopedics, we actually observed a higher proportion of female students undertake shadowing sessions than male students. Shadowing schemes such as this one may, therefore, offer a mechanism to empower all students to gain early surgical exposure and help overcome traditional gender biases.
Indirect metrics indicate that the shadowing scheme piloted was well received by students. The majority of students stayed for at least 6 hrs on their placements, suggesting that surgical consultants participating in the scheme facilitated an engaging and enjoyable clinical environment. A significant proportion of students also reported that consultants encouraged them to scrub-in, and for many this may have been their first opportunity to do this in a clinical setting. A smaller proportion of students also reported that they were allowed to directly assist in operations, suggesting that shadowing schemes may provide the ideal platform for students to gain real-life practical experiences of surgery even at a relatively early career stage.13 Indeed, more direct hands-on surgical exposure during medical school has been proposed as one method to mitigate the decreasing popularity of surgical careers in the United Kingdom.14
Direct feedback was also very positive, with the majority of students reporting that the shadowing scheme directly increased their understanding of the surgical sub-specialty they shadowed. This may enable students to make better informed choices about whether surgery is the right career for them,15 or to explore alternative surgical sub-specialties in the future. However, the majority of students stated that even participating in one-off surgical sessions offered as part of the shadowing scheme significantly increased their likelihood of wishing to pursue a surgical career in the future. This suggests that high-quality surgical sessions facilitated by the shadowing scheme could improve undergraduate experiences of surgery,16 potentially mitigating many of the challenges associated with gaining positive early surgical exposure during medical school.
Indeed, the importance of shadowing and surgical exposure on student choice to go into surgical careers must not be underestimated. For example, even in student cohorts where the proportion of students expressing an interest in surgery is low, it has been shown that operative exposure may increase the number of students applying for surgical residency by more than twofold.17 The quality of mentors encountered during surgical placements is also important, and where students encounter surgeons who are effective educators they rate their desire to pursue a surgical career more highly.18 Yet, when surveyed, surgeons often do not believe they play an important role in shaping students’ future career paths.19 However, even involving students with seemingly trivial tasks may dramatically increase their desire to pursue surgery. For example, allowing students to suture increases student interest in surgery by fivefold, and operating the camera increases this to sevenfold.20 The potential impact surgeons have on shaping medical student careers during every surgical encounter cannot therefore be overstated. Initiatives such as this SSS, which recruit engaged surgical mentors and promote active student involvement through scrubbing in and assisting, are thus likely to have a significant long-term impact on encouraging more students to consider surgical careers. This may be particularly important for supporting women in surgery initiatives, especially given the high proportion of students participating in this scheme who were female.
Establishing the first major SSS has required considerable effort, yet we have demonstrated that such schemes are extremely well received by students, have numerous benefits, and are sustainable in the long term. Having demonstrated large-scale sustainability at a single center, we now hope that other centers will build-on this model to develop their own variants of the shadowing scheme pioneered at UCL. This particular SSS was primarily student-led, but received input and guidance from surgical faculty within the medical school. Our experiences would, therefore, suggest that student surgical societies and trainee-run organizations are ideally placed to initiate, oversee, and administrate such schemes elsewhere.
Nevertheless, establishing this SSS has also emphasized that student-run surgical societies may run into challenges. For example, making initial contact with consultant surgeons in a particular sub-specialty specialty was sometimes problematic, and where this occurred local surgeon “champions” at both the consultant and trainee level were essential for opening up lines of communication, recruiting colleagues, and promoting the long-term sustainability of the scheme. For other medical schools wishing to establish a shadowing scheme similar to this one, there must be an initial time commitment to recruit local surgeons and establish appropriate infrastructure such as an online calendar booking system. Once this is has been established though, our experiences suggest that the SSS is largely self-sustaining with minimal regular long-term time demands. Where these have occurred, they have been managed by the student surgical society creating a dedicated “Shadowing Scheme Co-Ordinator” committee position, whose responsibility it is to oversee the day-to-day running of the scheme and act as a lead point of contact for both students and surgeons for a period of one academic year. We have found this works well as a model and would recommend this. However, other medical schools may wish to pilot only one or two specialties in the first instance (neurosurgery and cardiothoracic surgery were the most popular based on our data) to establish the appropriate infrastructure and gauge demand from the student body before offering all surgical sub-specialties. We have also been fortunate to be affiliated with a number of specialist hospitals, providing access to all major surgical sub-specialties, yet other medical schools may need to make reasonable adjustments as to what specialties they offer for shadowing based on local hospital service provision and expertise.
In the future, we hope to further capitalize on the mentorship opportunities that arise through schemes such as this one. Shadowing schemes present the ideal opportunity to foster long-term links between students and surgeons, providing excellent foundations for career advice, exposure to positive role models, and potential opportunities for personal development such as research and audit in a given surgical sub-specialty. Increased engagement from organizations such as the Royal Colleges of Surgeons in the UK and the American College of Surgeons in the US may also help facilitate wider uptake of SSSs such as this one. Professional colleges could help ensure a minimum acceptable running standard and incentivize engagement from both students and surgeons through formal recognition or accreditation. Undergraduate shadowing schemes that manage to incorporate significant mentoring or teaching components could also present significant continuing professional development opportunities for consultant and trainee surgeons.
One limitation of this shadowing scheme was that no data were formally collected from the surgeons who participated. However, quantifying the surgeon experience may be important for the future, particularly in the context of approaching the Colleges to explore the possibility of formally endorsing or accrediting such schemes. Nevertheless, informal feedback suggested that surgeons enjoyed the philanthropic aspect of promoting surgical careers amongst the next generation, and some commented on how it was refreshing to have keen students who were prepared and had read up on the procedures and pathologies on the case list. This allowed them to facilitate an engaging and interactive learning experience for students. In addition, given the strong evidence indicating that interactivity in the operating theatre greatly increases the desire of student to pursue a surgical career, more could be done to increase the percentage of students who were able to scrub-in or assist with cases during shadowing sessions. For example, a dedicated “Preparation for Shadowing” workshop, which teaches all students how to scrub-in and general theatre etiquette may help increase the proportion of students who are confident to scrub-in during shadowing sessions in the future. This may be particularly beneficial for pre-clinical students (the majority of those who participated in this scheme), who have not yet been formally taught how to scrub-in as the part of the medical school curriculum. Additional efforts to capitalize on the one-to-one mentoring opportunities available with participating surgeons could also be expanded moving forward.
Conclusion
SSSs offer an innovative method to provide medical students, and particularly those early on in medical school, with increased access and exposure to high-quality surgical sessions. Students greatly value such schemes and they help increase both student understanding of surgical specialties and the desire of students to pursue surgical careers. Locally administrated SSSs have great potential to increase undergraduate engagement in surgery, and in doing so they will ensure that surgery continues to inspire and attract the very best students from a diverse candidate pool in the future.
Abbreviations
SSS, Surgical Shadowing Scheme; UCL, University College London.
Acknowledgment
We would like to extend our thanks to all the surgeons, trainees and local hospitals that have kindly participated in the SSS and helped contribute to its longevity and success. We would also like to thank Professor Deborah Gill and UCL Medical School for kindly providing unpublished data on gender split within UCL Medical School.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Eardley I, Scott H, Wilkinson D. Why a career in surgery is no longer the golden ticket. BMJ. 2015;351:h3685.
2. Marshall DC, Salciccioli JD, Walton SJ, Pitkin J, Shalhoub J, Malietzis G. Medical student experience in surgery influences their career choices: a systematic review of the literature. J Surg Educ. 2015;72(3):438–445. doi:10.1016/j.jsurg.2014.10.018
3. Twigg V. What can surgeons do to increase the appeal of a surgical career? Bull R Coll Surg Engl. 2017;99(9):320–323.
4. Peel JK, Schlachta CM, Alkhamesi NA. A systematic review of the factors affecting choice of surgery as a career. Can J Surg. 2018;61(1):58–67. doi:10.1503/cjs.008217
5. Moravec M, Williams A, Aguilar-Roca N, O’Dowd DK. Learn before lecture: a strategy that improves learning outcomes in a large introductory biology class. CBE Life Sci Educ. 2010;9(4):473–481. doi:10.1187/cbe.10-04-0063
6. Porter J, Morphet J, Missen K, Raymond A. Preparation for high-acuity clinical placement: confidence levels of final-year nursing students. Adv Med Educ Pract. 2013;4:83–89. doi:10.2147/AMEP.S42157
7. Basak O, Yaphe J, Spiegel W, Wilm S, Carelli F, Metsemakers JF. Early clinical exposure in medical curricula across Europe: an overview. Eur J Gen Pract. 2009;15(1):4–10. doi:10.1080/13814780902745930
8. Whitehouse KJ, Moore AJ. Undergraduate teaching of neurosurgery – what is the current practice in the UK and is there a need for improvement? Br J Neurosurg. 2015;29(6):753–757. doi:10.3109/02688697.2015.1054361
9. Devnani A, Lim D, Loganathan K, et al. Inspiring the next generation of cardiothoracic surgeons: an easily reproducible, sustainable event increases UK undergraduate interest in the specialty. Interact Cardiovasc Thorac Surg. 2015;22(1):106–108.
10. General Medical Council. The State of Medical Education and Practice in the UK; 2016. Available from: https://www.gmc-uk.org/-/media/documents/SOMEP_2016_Full_Report_Lo_Res.pdf_68139324.pdf. Accessed July 30, 2019.
11. Moberly T. A fifth of surgeons in England are female. BMJ. 2018;363:k4530. doi:10.1136/bmj.k4530
12. Ek EW, Ek ET, Mackay SD. Undergraduate experience of surgical teaching and its influence and its influence on career choice. ANZ J Surg. 2005;75(8):713–718. doi:10.1111/j.1445-2197.2005.03500.x
13. Toll E. More trainees and less operative exposure: a quantitative analysis of training opportuntiies for junior surgical trainees. Bull R Coll Surg Engl. 2010;92(5):170–173.
14. Bartlett J. Addressing the recruitment shortfall in surgery – how do we inspire the next generation? Ann Med Surg. 2017;25:30–32. doi:10.1016/j.amsu.2017.11.024
15. Gill R, Massey V, Kimbrough MK, Mizell JS, Bentley FR, Thrush CR. Surgical career choices in medical students: timing, stability and important factors. J Am Coll Surg. 2017;225(4):e161. doi:10.1016/j.jamcollsurg.2017.07.962
16. Allen JG, Weiss ES, Patel ND, et al. Inspiring medical students to pursue surgical careers: outcomes from our cardiothoracic surgery research program. Ann Thorac Surg. 2009;87(6):1816–1819. doi:10.1016/j.athoracsur.2009.03.007
17. O’Herrin JK, Lewis BJ, Rikkers LF, Chen H. Why do students choose careers in surgery? J Surg Res. 2004;119(2):124–129. doi:10.1016/j.jss.2004.03.009
18. Musunuru S, Lewis B, Rikkers LF, Chen H. Effective surgical residents strongly influence medical students to pursue surgical careers. J Am Coll Surg. 2007;204(1):164–167. doi:10.1016/j.jamcollsurg.2006.08.029
19. Quillin RC
20. Berman L, Rosenthal MS, Curry LA, Evans LV, Gusberg RJ. Attracting surgical clerks to surgical careers: role models, mentoring, and engagement in the operating room. J Am Coll Surg. 2008;207(6):
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



