Back to Journals » Infection and Drug Resistance » Volume 16
Development and Validation of the Knowledge, Attitude, and Practice Questionnaire for Community Pharmacy Personnel in Tuberculosis Case Detection, Drug Monitoring, and Education: A Study from Indonesia
Authors Kausar MN, Fitriana E, Khairunnisa K , Faruque MO , Bahar MA , Alfian SD , Pradipta IS
Received 21 February 2023
Accepted for publication 2 June 2023
Published 13 June 2023 Volume 2023:16 Pages 3729—3741
DOI https://doi.org/10.2147/IDR.S409107
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Mersa Nurain Kausar,1– 4 Efi Fitriana,5 Khairunnisa Khairunnisa,6 Md Omar Faruque,7 Muh Akbar Bahar,8 Sofa D Alfian,1,3 Ivan Surya Pradipta1,3
1Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Bandung, Indonesia; 2Master of Clinical Pharmacy Program, Faculty of Pharmacy, Universitas Padjadjaran, Bandung, Indonesia; 3Drug Utilization and Pharmacoepidemiology Research Group, Center of Excellence in Higher Education for Pharmaceutical Care Innovation, Universitas Padjadjaran, Bandung, Indonesia; 4Occupational Health – Regional Public Hospital, West Java Provincial Government, Bandung, Indonesia; 5Department of General Psychology and Experiment, Faculty of Psychology, Universitas Padjadjaran, Bandung, Indonesia; 6Faculty of Pharmacy, Universitas Sumatera Utara, Medan, Indonesia; 7Department of Pathology and Laboratory Medicine, University of Kansas Medical Center, Kansas City, MO, USA; 8Department of Pharmacy, Faculty of Pharmacy, Universitas Hasanuddin, Makassar, Indonesia
Correspondence: Ivan Surya Pradipta, Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Jl. Raya Bandung-Sumedang, Km.21, Jatinangor, Sumedang, Jawa Barat, Bandung, 45363, Indonesia, Tel +62 842 88888, Fax +62 842 88898, Email [email protected]
Background: Validated and standardized structured questionnaires based on psychometric analysis are extremely limited, particularly for assessing community pharmacy personnel’s knowledge, attitude, and practice (KAP) in tuberculosis (TB) case detection, drug monitoring, and education. We, therefore, developed and validated a questionnaire to assess the KAP of community pharmacy personnel in TB case detection, drug monitoring, and community education.
Methods: This study was conducted in two phases. First, we developed the questionnaire, which included framework development, item generation, individual item content validity index (I-CVI), item screening, and pre-testing. Second, we validated the questionnaire with 400 participants using various analyses, including participant analysis, confirmatory factor analysis (CFA), adjusted goodness-of-fit index (AGFI), comparative fit index (CFI), non-normed fit index (NNFI), root mean square error of approximation (RMSEA), and standardized root mean square residual (SRMR). We determined the reliability test using Cronbach’s alpha and test−retest reliability using Pearson’s correlation.
Results: In the development phase, we defined 63 items that comprised 18 sociodemographic, 18 knowledge, 18 attitude, and 9 practice items. Across the 63 items, the I-CVI scores of sociodemographic and KAP items were one each. The CFA model parameter values were X2/df= 2.28; AGFI = 0.95; CFI = 0.99; NNFI = 0.98; RMSEA = 0.06; and SRMR = 0.03 (p < 0.05 for all). Cronbach’s alpha coefficients of KAP items were 0.75, 0.91, and 0.95, respectively. The test-retest reliability coefficients of KAP were 0.84, 0.55, and 0.91, respectively (p < 0.01).
Conclusion: This study indicates that the developed questionnaire is a valid and reliable instrument for assessing the KAP of community pharmacy personnel for TB case detection, drug monitoring, and community education in Indonesia. Community pharmacy personnel can support TB notification and treatment by assessing their prospective roles in surveys using this questionnaire, enabling TB eradication in 2030.
Keywords: development and validation, knowledge attitude and practice, community pharmacy, tuberculosis
Introduction
Tuberculosis (TB) is an infectious disease that was the leading cause of death from a single infectious agent, ranking above HIV/AIDS during coronavirus (COVID-19) pandemic.1 The WHO estimated a global TB incidence of approximately 10.6 million cases in 2021. The estimated TB burden in Indonesia is 969 thousand to 1.1 million cases in 2021.1
Reduces access to TB diagnosis and treatment is estimated to have increased TB deaths in 2020 and 2021.1 The three countries that accounted for most of the reduction in the reported number of people newly diagnosed with TB, in 2020 were India, Indonesia, and the Philippines (67% of the global total).1 The notification of TB fell from 7.1 million in 2019 to 5.8 million in 2020, a drop of 18%.1
Reductions in TB case notifications in 2020 and 2021 reflected a negative impact on TB case detection and led to an increase in the number of people with undiagnosed and untreated TB in the community.1 As one of the most TB-endemic countries, Indonesia faces challenges detecting TB cases and improving treatment outcomes. Involving the civil society and private sectors has been recommended as one of the global strategies to accelerate TB elimination.1
The community pharmacy has been identified as a potential facility for detecting TB cases and improving TB treatment outcomes. Studies in high-burden TB countries, including Indonesia, reported that most patients with TB initially presented at the pharmacy for first aid medication.2–7 However, improper management of people affected with TB in the community pharmacy was studied as a cause of delayed diagnosis and treatment.8,9 A study in Indonesia supported the total delay in TB diagnosis and treatment caused by visiting a pharmacy for first-aid medication.2 In another study, we found that when a patient with TB received inappropriate treatment recommendations from a pharmacy, it resulted in delayed diagnosis and treatment.10,11 Improper management of people affected by TB in pharmacies may result from the poor TB knowledge, attitude, and practices of pharmacy personnel. Therefore, improving TB care in community pharmacies is necessary to improve TB case detection and treatment outcomes.
Several studies have focused on knowledge, attitude, and practice (KAP) regarding TB in many countries and found a positive correlation between KAP and improving TB care and prevention.12–14 A cross-sectional study in Peru and Pakistan reported that pharmacists with adequate TB knowledge and a willingness to learn TB more contributed to TB prevention and care.12,13 In the general population, a cross-sectional study in Indonesia predicted that adequate knowledge of TB could aid in the treatment and prevention of TB.14 All these studies have highlighted that the assessment of KAP is essential for improving TB prevention and care, especially in community pharmacies.
However, current TB-KAP instruments used to evaluate pharmacy personnel continue to focus on a limited domain, ie, TB case detection only.12,13,15,16 Because the potential role of pharmacy in TB management extends beyond TB case detection, a comprehensive instrument is required to cover the assessment of TB drug monitoring and education activities. The instrument can assess the current KAP situation and develop strategies for engaging community pharmacy personnel in TB prevention and care.
The potential role of pharmacy personnel in TB notification and treatment must first be assessed before an intervention study. This questionnaire is required to determine the actual potency of pharmacy personnel in TB for further interventions. For example, if the findings of the KAP study indicate that pharmacy personnel are still lack knowledge about TB management, a comprehensive training can be delivered to increase their knowledge. According to a study conducted in India, developing intervention studies required a constantly updated training program.15 This questionnaire will therefore be very helpful in interventional studies.
Therefore, we developed and validated a questionnaire to assess the KAP of community pharmacy personnel for improving their role in TB case detection, drug monitoring, and community education in the Indonesia population. Besides using the WHO survey guidelines and psychological theories, we constructed the questionnaire based on the National Guidelines for Medical Services and the most recent national guideline for managing Tuberculosis case, to balance the development of TB treatment programs and guidelines in line with the most recent research advancements.
Materials and Methods
Study Design and Setting
This study was conducted in Indonesia from July 2021 to March 2022 that consisted of development phase in July to November 2021 and validation phase in December to March 2022. Ethics approval was granted by the ethics committee of Universitas Sumatera Utara (No. 599/KEP/USU/2021) and all methods were performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants.
The study was divided into a development phase and a validation phase. In the development phase, relevant items in the questionnaire were developed based on the study objective. This phase consisted of framework development, item generation, item screening, content validity, and pre-testing activities. In the validation phase, the items were validated using various analyses, including participant analysis, confirmatory factor analysis (CFA), Cronbach’s alpha analysis, and test-retest reliability.
Participants and Sample Size
Considering that pharmacists and pharmacy technicians generally operate a pharmacy, we included all those who had worked in a pharmacy for > 6 months for the validation process. To represent the characteristics of pharmacy personnel in Indonesia, we selected participants with various characteristics and locations, including sex, age, profession (pharmacist and pharmacy technician), pharmacy type (single and chain), working experience, working hours, education level, TB training experience, and pharmacy location (western, central, and eastern parts of Indonesia as well as urban and peripheral areas). The purposive sampling was used in the development and validation phases. Samples were recruited based on the above criteria.
In the development phase, we recruited 32 participants in four areas to develop the questionnaire. In the validation phase, the minimum number of participants for developing a questionnaire was five for each item.17,18 To observe the acceptable comparison patterns, the minimum sample size was estimated to range from 300–450 participants.19,20 Then, we determined that five participants were required for each item. Therefore, a total of 400 participants were included in the validation phase. A total of 400 participants recruited from 284 pharmacies in four locations (Bandung City, Bandung District, Medan City, and Makassar City). The proportion of participants was 234 pharmacists and 166 pharmacy technicians.
Item Development
The items were developed in Bahasa Indonesia in four steps: framework development, item generation, item screening, content validity, and pre-testing.
Framework Development
We considered the activity, domain, indicator, and construction of the questionnaire to specify the scopes of the domain and facilitate item generation.20 The activities included TB case detection, drug monitoring, and education, whereas the domains included sociodemographic characteristics and KAP. Among the activities and domains, we developed and set indicators for each construction.20 To clarify the terminology, the three main activities were operationally defined as follows: TB case detection was defined as screening pharmacy visitors for TB signs and symptoms and referring presumptive TB patients to healthcare facilities or community healthcare centers for further examination. TB drug monitoring was defined as acting as a supervisor for TB drug use, creating medication schedules, monitoring medication adherence, monitoring and reporting adverse drug reactions. TB education was defined as improving pharmacy visitors’ understanding of TB, including signs and symptoms of the disease, prevention of transmission, side effects of TB drugs, and adherence to TB drugs.
We considered three primary sources of information related to KAP for the item development: (1) a practical book for developing a KAP study published by the WHO,21 (2) a national regulation that described pharmacists’ roles and systems in managing TB cases in Indonesia,22 and (3) a consensus on psychological theory for implementing evidence-based practices.23 We also considered several KAP-related questionnaires for TB healthcare providers to develop a comprehensive questionnaire.24–26
Item Generation
The purpose of item generation was to identify appropriate questions that were suitable for previously defined domains.20 We conducted a literature review to generate items based on previously defined activities, domains, indicators, and constructions. The questionnaire consisted of closed-ended questions and was self-administered. It was divided into four sections: sociodemographic (S), knowledge (K), attitude (A), and practice (P). Item generation entailed framing the questions, creating options for responses, and planning for scoring.27
Item Screening
Experts reviewed the developed items to evaluate whether each item was relevant, accurately represented the content, and had good technical quality.20 We consulted four experts: a TB programmer (general practitioner), a community pharmacist, a pharmacy technician, and an epidemiologist. The experts reviewed all the items, examined the necessary/unnecessary items, modified them as needed,27 and provided constructive suggestions and feedback to improve the questionnaire.
Item Content Validity Index (I-CVI)
The content validity index (CVI) was defined as the degree to which elements of an instrument are relevant and representative of the defined construct.28 Expert opinions were used to determine the CVI.17 The individual-CVI (I-CVI) was calculated based on Lynn’s theory.29 Lynn recommended an I-CVI of 1.0 for 3–5 experts and a minimum I-CVI of 0.78 for 6–10 experts.29,30 In this study, four experts were asked to score each item on a five-point Likert scale as follows: 1 = highly not relevant, 2 = not relevant, 3 = neutral, 4 = relevant, and 5 = highly relevant. The experts were asked to write a comment on the provided form. They could add, delete, substitute, or correct the items. We conducted two rounds of calculations for I-CVI, with an expected I-CVI value of 1.0 for the final questionnaire.
Pre-Testing
Pre-testing was performed to assess the items’ clarity, known as face validity.17 The recommended number of participants for this step was 30.31 Therefore, we recruited 32 participants (pharmacists and pharmacy technicians) to assess item clarity and difficulty filling out the questionnaire.27 In addition, the participants were asked to provide feedback to improve their clarity.32
Validation Processes
The questionnaire was validated with 400 participants. For a broader nationwide representation, we collected participant information from four areas: Bandung City, Bandung District, Medan City, and Makassar City, representing the western, central, and eastern parts of Indonesia. We included 100 participants from each area, and data were collected using electronic-based and paper-based questionnaires.
Data used in the validation phase were analyzed using several methods, including participant analysis, CFA for construct validity, Cronbach’s alpha, and test-retest reliability. We used the IBM SPSS® statistics software for Windows, version 25 (IBM Corp., Armonk, NY, USA), and LISREL® for data analyses.
Participant Analysis
Participant analysis summarizes of the characteristics of study participants.33 We used the mean, standard deviation, and minimum–maximum values to determine the participants’ sociodemographic characteristics, which are important because these characteristics might affect KAP.14,18,34–37
Confirmatory Factor Analysis (CFA)
CFA was used to psychometrically assess the possibility of a systematic comparison of a factor based on a systematic suitability assessment as well as to estimate the relationship between latent constructs that had been corrected for measurement errors, or as a construct validity test.20,38 The CFA was performed using LISREL®. Theoretically, the minimum sample size for the CFA is 200 participants.39 However, we included 400 participants in this study.40,41 We expected a ratio of Chi-squared to degree of freedom of <3 (p > 0.05), a comparative fit index (CFI) of >0.90, adjusted goodness-of-fit index (AGFI) of >0.90, non-normed fit index (NNFI) of >0.90, root mean square error of approximation (RMSEA) of ≤0.08, and standardized root mean square residual (SRMR) of ≤0.08.17
Cronbach’s Alpha
The reliability test is used to determine the extent to which the scores generated by a questionnaire are consistent and reproducible.32 A reliability test was performed using Cronbach’s alpha. Cronbach’s alpha was used to explain the internal consistency of the questionnaire.42 A Cronbach’s alpha coefficient in the range of 0.6–0.7 is generally considered acceptable, whereas a Cronbach’s alpha coefficient of 0.8 indicates good reliability.42,43
Test–Retest Reliability
The test-retest reliability can be evaluated using Pearson’s correlation.44 Test-retest reliability refers to the ability of the scores of an instrument to be reproducible if used on the same participant and condition.44 This test presumes that the actual measured score will yield the same result over a short time interval.45
Pearson’s correlation coefficients of 0.00–0.10, 0.10–0.39, 0.40–0.69, 0.70–0.89, and 0.90–1.00 indicate negligible, weak, moderate, strong, and very strong correlation, respectively.40 We chose ≥0.5 to represent a good correlation because higher correlation values indicate higher test-retest reliability.20 This test was conducted with the same 32 participants within a 1-week interval.46
Results
A total of 56 items were defined in the development phase. In the item screening, 56 items were modified after two rounds of expert evaluation. We then developed 56–63 items in the pre-testing step. Finally, we defined 63 items for the validation phase. All the steps and results are summarized in Figure 1.
 |
Figure 1 A flow diagram of questionnaire development and validation. |
Item Development
Framework Development
The sociodemographic domain included several indicators, including sex, age, marital status, education level, work experience, income, and information about the pharmacies that they visit. The knowledge domain included indicators related to the knowledge of TB pathogen, infection site, spreading mechanism, signs, symptoms, risk factors, diagnosis, drug regimen, drug use, and potential adverse drug reactions.21,22 The attitude domain included indicators related to beliefs about capabilities/self-efficacy (perceived competence, self-confidence, and optimism/pessimism) and beliefs about consequences (anticipated regret and characteristics of outcome expectancies: valued or not valued).21,23 The practice domain included indicators related to activities associated with TB case detection, drug monitoring, and education. TB case detection-related constructs included TB screening and referral of presumptive TB patients to appropriate healthcare facilities, while the drug monitoring-related constructs included treatment-supporting activities (supervising TB drug use, creating medication schedules, monitoring medication adherence, monitoring adverse drug reactions, and reporting). We defined TB educational activity-related constructs as providing TB information to society.21,22
Item Generation
The initial 56 items were developed, comprising 18 sociodemographic, 11 knowledge, 18 attitude, and 9 practice items. The knowledge section items were scored 1 for a correct answer and 0 for a wrong answer or a do not know the response. A five-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree), was used to assess attitudes toward the importance of case detection, drug monitoring, and education activities for reducing TB incidence. In the practice domain, five options were provided to identify the frequency of specific practices, with a score of 1 (never) indicating that the practice was not performed in the past six months, a score of 2 (rarely) indicating that the practice was performed once every 5–6 months, a score of 3 (sometimes) indicating that the practice was performed once every 24 months, a score of 4 (often) indicating that the practice was performed every month, and a score of 5 (very often) indicating that the practice was performed every month. A higher score indicated a better KAP assessment.
Item Screening
In the first round of expert evaluation, 56 items generated from framework development and item generation were screened. The experts provided corrections and suggestions by arranging sentences and clarifying the meaning of the items. No changes were made in the number of items, but items and answers were modified. The experts advised using standard terms for the items and improving sentence structure to make them more understandable, particularly in the sociodemographic domain. For example, an expert suggested using the standard term for the type of pharmacy and fee for service in the sociodemographic section. After all the items were corrected, the revisions were subjected to another round of approval by the experts.
I-CVI
The results for I-CVI for sociodemographic, knowledge, attitude, and practice items were 0.89, 1.0, 0.86, and 0.89, respectively. We improved the questionnaire to achieve an I-CVI score (<1.0) that met Lynn’s criteria.29,47 A total of 4 of 18 items in the sociodemographic section were modified and refined according to the experts’ suggestions. In the attitude section, we modified 8 of 18 items, whereas, in the practice section, we modified 4 of 9 items. The rate of change was minor. The experts suggested to re-arrange the sentences for ease of understanding and to be in line with the concept. After improving the items, the I-CVI value for all sections was 1.0. This value indicated that the contents of the questionnaire represented all items. The result of I-CVI in the first and second rounds are represented in Table 1.
 |
Table 1 I-CVI in First and Second Round |
Pre-Testing
Before the questionnaire was distributed to the target population, we performed a face validity test on 32 participants representing the target population. These participants act as target population whom judges as experts at evaluating face validity, which is a component of content validity.20 In the face validity test, 32 participants could give corrections and suggestions in the questionnaire, and we accepted the corrections and suggestions for improvement.
We received feedback and suggestions from the participants when they completed the questionnaire for face validity. The participants completed the questionnaire in about 15 minutes on average. Using responses from 32 participants, the correlation coefficient was <0.3 for knowledge items and ≥0.3 for attitude and practice items. Thereafter, improvements were made to obtain better results in the knowledge domain, which are presented in Supplementary Table 1.
Most corrections were in the knowledge domain. All minor corrections to the sociodemographic, attitude and practice domains were made correctly. Some questions in the knowledge domain, such as those related to the infection site, spreading mechanism, and drug use, were rephrased for better sentence construction to improve participants’ understanding of the questions.
We removed one item about the drug regimen because it was not relatable as constructed. In addition, the constructions of signs, symptoms, risk factors, drug regimens, and side effects were modified and broken down into multiple items to make them more meaningful. Therefore, the number of knowledge items increased from 11 (original questionnaire) to 18 (final questionnaire). After correction, the correlation coefficient for all domain were ≥0.3. No change was made to the number of items in the attitude and practice domains. Finally, 63 items were identified for the validation process listed in Supplementary Table 2.
Validation Processes
Participant Analysis
Considering that the minimum number of participants required for the validity test was 315, we distributed the final questionnaire to 400 participants. Most participants in the validity test were women (79%). The proportion of pharmacists and pharmacy technicians was balanced (58.5% vs 41.5%). The education level of the participants varied, ranging from senior high school to doctorate. The participant characteristics are presented in Table 2.
 |
Table 2 Participant Characteristics That Were Included in the Validation Processes |
CFA
The CFA model of the questionnaire was composed of three factors loaded with eight items. The first factor, knowledge, included K1 (total score of knowledge on TB case detection) and K2 (total score of knowledge on TB drug monitoring). We included only two items in the knowledge domain because the total score for knowledge of education activity was the same as that for TB case detection and drug monitoring. The second factor, attitude, included A1 (total score for attitude on TB case detection), A2 (total score for attitude on TB drug monitoring), and A3 (total score for education). The final factor, practice, included P1 (total score for practice on TB case detection), P2 (total score for practice on drug monitoring), and P3 (total score for practice on education).
The results of the CFA were as follows: ratio of Chi-squared to the degree of freedom. X2/df= 2.28, AGFI = 0.95, CFI = 0.99, NNFI = 0.98, RMSEA = 0.06, and SRMR = 0.03 (p < 0.05 for all). The model fit test is presented in Table 3. The results of the CFA model are presented in Supplementary Figure 1.
 |
Table 3 Model Fit Test for Confirmatory Factor Analysis |
Cronbach’s Alpha
Cronbach’s alpha coefficients of knowledge, attitude, and practice were > 0.70, indicating that the questionnaire had good internal consistency. The results of Cronbach’s alpha are presented in Table 4
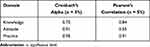 |
Table 4 Cronbach’s Alpha and Test–Retest Reliability |
Test–Retest Reliability
Pearson’s correlation coefficients of knowledge, attitude, and practice for the test-retest reliability were ≥ 0.30 (p < 0.01 for all), indicating good correlations. The results of test-retest reliability (Pearson’s correlation) are presented in Table 4.
We finally included 63 items for the final item: sociodemographic, knowledge, attitude, and practice items. The process of developing the questionnaire items is summarized in Supplementary Table 3.
Discussion
We developed and validated a KAP instrument for community pharmacy personnel to use when providing TB services. The instrument included 63 items covering fundamental KAPs for TB case detection, drug monitoring, and education. The items were divided into four sections: sociodemographic (18 items), knowledge (18 items), attitude (18 items), and practice (9 items).
In the development phase, originally 56 items were produced in item generation processes. The item questionnaire in the knowledge domain increased from 11 to 18 because there were 2 items unmodified, 8 items modified, 1 item deleted, and 8 items added in pre-testing processes (see Supplementary Table 3).
Because this is a newly developed instrument that comprehensively assesses the KAP of community pharmacy personnel for specific activities, such as TB case detection, drug monitoring, and education, a content validity assessment is needed to ensure that all items are relevant to the domain being measured. We consulted four experts: a TB programmer (general practitioner), a community pharmacist, a pharmacy technician, and an epidemiologist, and we determined the I-CVI for content validation. The general practitioner is a medical staff of the hospital’s Directly Observed Therapy (DOT) team and has more than 7 years of clinical expertise treating TB patients. A pharmacist expert from the community pharmacy has had pharmaceutical experience with TB patients for more than 20 years. The pharmacy technician who was selected as an expert has worked in pharmacy for more than 8 years to serve TB patients. The epidemiologist expert has been a lecturer and researcher for more than 10 years at the university and is concerned about the epidemiology of TB disease. All experts suggested improvements that complement each other in the questionnaire development process.
According to the current studies,17,18,44 in the development phase, we should establish a framework that contains the activity, domain, indicator, and construction of the questionnaire to identify the scopes of the domain and facilitate item generation. This framework was then evaluated by the expert to verify the validity of the content. Boateng et al suggested that expert judges should be independent of those who developed the item pool. No blinded selected expert to examine the questionnaire, as indicated by Boateng et al. We need to know precisely the background of the experts to make sure that the questionnaire is examined by an expert at its finest. Expert judgment can be done systematically to avoid bias in the assessment of items.20 Their assessments have been measured using defined scaling and statistical processes such as the content validity ratio for quantifying consensus48 or content validity index for measuring proportional agreement.29 We chose Lynn criteria29 for measuring proportional agreement to clarify the content validity index.
There were several techniques to determine content validity index by expert. Based on Polit and Back (2006), content validity index consist of: I-CVI (item-level content validity index), S-CVI (scale-level content validity index), S-CVI/ UA (scale-level content validity index, universal agreement calculation method), and S-CVI/Ave (scale-level content validity index, averaging calculation method).47 The I-CVI is computed as the number of experts giving a rating of either 3 or 4 (thus dichotomizing the ordinal scale into relevant and not relevant), divided by the total number of experts.47 We used I-CVI information to guide us in revising, deleting, or substituting items. The value of I-CVI for four expert is one.29,47 In the first round of expert judgment, we found some items less than one, so we made modification to each item and after second round expert judgment, the I-CVI was one each. We found that the final I-CVI met the criteria of Lynn,29 ie, a valid item should have an I-CVI of 1.0 for 3–5 experts.29
After we determined content validity index, a total of 32 participants were selected as representatives of the target population selected in the pre-testing process to determine face validity. They acted as experts, evaluating the questionnaire that had been approved by four experts so that discrepancies could be eliminated. In the pre-testing process, several items in the knowledge domain produced a correlation coefficient < 0.3, so we made some improvements and did the second round of the test with the same 32 participants. The improvement was based on feedback and suggestions from the participants. No change was made to the number of items in the attitude and practice domains because correlation coefficient of these domain ≥ 0.3.
A validation process was performed with 400 participants with various characteristics, and the results revealed that the instrument was valid and reliable for assessing the KAP of community pharmacy personnel in TB case detection, drug monitoring, and education. A study involving 1125 pharmacy personnel in Indonesia showed that sex, age, pharmacist profession, chain pharmacy, working experience, TB training experience, and pharmacy location were associated with KAPs in TB case detection.49 Similarly, level of education, patient volume, and workload were found to be associated with TB care in community pharmacies in Peru, India, and Indonesia.12,14,50,51 Therefore, we considered those sociodemographic characteristics in recruiting participants for the validation process to develop a comprehensive instrument for the KAP assessment.
The questionnaire was developed in accordance with the sequence of questionnaire development suggested by Boateng et al.20 Based on psychometric analysis of the face, content, and construct validities, this study showed acceptable values, and the test-retest reliability was also acceptable.
Regarding the CFA, our factor model fits with the latent construct. The ratio of Chi-squared to the degree of freedom was < 3 (p >0.05), indicating that the number of differences between the expected and observed covariance matrices met the standard requirement.17 The CFI was > 0.90, indicating that the value was equal to the discrepancy function adjusted for the sample size and exhibited a better model fit.52 Our RMSEA, a residual model, met the criteria reported by Hu and Bentler (1999), who stated that a value of ≤0.06 is acceptable as a model fit.52
We found that Cronbach’s alpha coefficient was >0.70 for all parameters in the first test of reliability, indicating that the questionnaire had good internal consistency.42,43 Several factors affected the value of the test reliability, such as the duration between the first and second tests44 and the small number of participants.53 The first and second test periods should not be too short. Otherwise, participants may overestimate their answers.44 Marx et al found no significant difference in the test-retest reliability within two days and two weeks.46 Therefore, we conducted the test with a 1-week interval, which is an acceptable duration. Consistent with the results of the validation phase, the overall psychometric test indicated good values for the parameters. Therefore, the results of our study can be used as an assessment instrument for evidence regarding the role of community pharmacy personnel and TB prevention and care.
Considering the potential role of community pharmacy in TB prevention and care, this questionnaire can be used to assess the current situation of the pharmacy personnel KAP in three domains, ie, TB case detection, drug monitoring, and education in Indonesia. Since developing a strong coalition with all resources in TB management is strongly recommended as the global pillar for the END TB strategy, this questionnaire can be beneficial in identifying and developing strategies to engage pharmacies in TB patient detection, drug monitoring, and education.
KAP assessment in Tuberculosis Case Detection, Drug Monitoring, and Education is essentially needed to develop appropriate and effective intervention to improve practice of community pharmacy personnel in Tuberculosis Case Detection, Drug Monitoring, and Education. The practice itself will support global TB elimination that face with two major challenges, ie, high number of people with underdiagnosed TB and failed TB treatment.
Private sector and community contributions to TB notification and treatment support are needed for TB elimination as part of the WHO strategy to END TB by 2030.1 A study conducted in western India indicated that private practitioners are still slow in raising TB notifications.54 Collaboration within private practitioners and community pharmacy is expected to raise TB case notification. Community pharmacy personnel can screen pharmacy visitors for TB signs and symptoms and refer presumptive TB patients to healthcare facilities or community healthcare centers for further examination as has been done in India and Pakistan13,15 to enhance the notification of TB cases.
In terms of treatment support, community pharmacy personnel can provide education to TB patients through education, as described by Karuniawati et al in 2019.37 This advice can improve TB patients’ compliance with their medication. In the monitoring aspect, community pharmacy personnel, especially pharmacists, can identify drug therapy problems (medication adherence and reporting adverse drug reactions). Furthermore, they can help identify possible issues with medication therapy after the initiation of a complex medication regimen.55 We believe that the three big roles of community pharmacy personnel can contribute to TB notification and treatment to reach the goal of TB elimination by 2023.
The study limitations should be considered. First, the questionnaire may not be used for the global pharmacy population as it was developed and validated in the Indonesian pharmacy population in Bahasa Indonesia. Second, the knowledge items related to TB medication were focused on non-drug-resistant (DR) TB regimens. Thus, this questionnaire did not cover the knowledge of DR-TB regimen. Because the multi-DR-TB center coordinates DR-TB treatment owing to the complexity of the regimen, we limited the role of pharmacy to people with presumed TB and patients with drug-sensitive TB for this instrument. Third, since the guidelines for treating TB can be modified based on the updated evidence, this questionnaire needs to be further adapted with the update guideline particularly in the knowledge domain. Nevertheless, we believe that using different participant characteristics in the validation process and conducting a systematic and comprehensive analysis will contribute to the questionnaire’s validity and reliability.
Conclusion
This study indicates that the developed questionnaire is a valid and reliable instrument for assessing the KAP of community pharmacy personnel for TB case detection, drug monitoring, and community education in Indonesia. Community pharmacy personnel can support TB notification and treatment by assessing their prospective roles in surveys using this questionnaire, enabling TB eradication in 2030. Further studies should be conducted to translate and validate the questionnaire for its utility as an instrument for the global pharmacy population.
Acknowledgments
We thank the Indonesian Pharmacist Association (IAI = Ikatan Apoteker Indonesia) and Pharmacy Technician Association (PAFI = Perhimpunan Ahli Farmasi Indonesia) for supporting this study.
The abstract of this paper was presented at the “The 4th INA-TIME (Indonesia Tuberculosis International Meeting 2022” as an oral presentation with interim findings. The abstract was published in the 4th INA-TIME (Indonesia Tuberculosis International Meeting 2022 Abstract Book: http://repository.umj.ac.id/id/eprint/11147
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Ministry of Education, Culture, Research, and Technology, Republic of Indonesia (Grant no. 2393/UN6.3.1/PT.00/2022).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization. Global Tuberculosis Report 2022. World Health Organization; 2022.
2. Lestari BW, McAllister S, Hadisoemarto PF, et al. Patient pathways and delays to diagnosis and treatment of tuberculosis in an urban setting in Indonesia. Lancet Reg Heal. 2020;5:100059. doi:10.1016/j.lanwpc.2020.100059
3. Surya A, Setyaningsih B, Suryani Nasution H, et al. Quality tuberculosis care in Indonesia: using patient pathway analysis to optimize public-private collaboration. J Infect Dis. 2017;216(Suppl_7):S724–S732. doi:10.1093/infdis/jix379
4. Lönnroth K, Uplekar M, Blanc L. Hard gains through soft contracts: productive engagement of private providers in tuberculosis control. Bull World Health Organ. 2006;84(11):876–883. doi:10.2471/BLT.06.029983
5. Daftary A, Jha N, Pai M. Enhancing the role of pharmacists in the cascade of tuberculosis care. J Epidemiol Glob Health. 2016;7(1):1–4. doi:10.1016/J.JEGH.2016.05.001
6. Kiwuwa MS, Charles K, Harriet MK, Karaarslan K. Patient and health service delay in pulmonary tuberculosis patients attending a referral hospital: a cross-sectional study. BMC Public Health. 2005;5:5. doi:10.1186/1471-2458-5-122
7. Sreeramareddy CT, Qin ZZ, Satyanarayana S, Subbaraman R, Pai M. Delays in diagnosis and treatment of pulmonary tuberculosis in India: a systematic review. Int J Tuberc Lung Dis. 2014;18(3):255–266. doi:10.5588/IJTLD.13.0585
8. Satyanarayana S, Kwan A, Daniels B, et al. Use of standardised patients to assess antibiotic dispensing for tuberculosis by pharmacies in urban India: a cross-sectional study. Lancet Infect Dis. 2016;16(11):1261–1268. doi:10.1016/S1473-3099(16)30215-8
9. Zawahir S, Le H, Nguyen TA, et al. Standardised patient study to assess tuberculosis case detection within the private pharmacy sector in Vietnam. BMJ Glob Heal. 2021;6(10):e006475. doi:10.1136/BMJGH-2021-006475
10. Pradipta IS, Idrus LR, Probandari A, et al. Barriers and strategies to successful tuberculosis treatment in a high-burden tuberculosis setting: a qualitative study from the patient’s perspective. BMC Public Health. 2021;21(1):1–12. doi:10.1186/s12889-021-12005-y
11. Pradipta IS, Idrus LR, Probandari A, et al. Barriers to optimal tuberculosis treatment services at community health centers: a qualitative study from a high prevalent tuberculosis country. Front Pharmacol. 2022;1:936. doi:10.3389/FPHAR.2022.857783
12. García PJ, Hernández-Córdova G, Pourjavaheri P, Gómez-Paredes HJ, Sudar S, Bayer AM. Knowledge, attitudes and practices related to tuberculosis in pharmacy workers in a cross-sectional survey in El Agustino, Peru. PLoS One. 2018;13(7):1–11. doi:10.1371/journal.pone.0196648
13. Mustafa T, Shahzad Y, Kiani A. A survey of knowledge, attitude, and practices of private retail pharmacies staff in tuberculosis care: study from Dera Ismail Khan City, Pakistan. J Pharm Policy Pract. 2018;11(1):1–7. doi:10.1186/s40545-018-0134-1
14. Ramadhany S, Achmad H, Singgih MF, Ramadhany YF, Inayah NH, Mutmainnah N. A review: knowledge and attitude of society toward tuberculosis disease in soppeng district. Syst Rev Pharm. 2020;11(5):57–62. doi:10.31838/srp.2020.5.10
15. Daftary A, Satyanarayana S, Jha N, et al. Can community pharmacists improve tuberculosis case finding? A mixed methods intervention study in India. BMJ Glob Heal. 2019;4(3):e001417. doi:10.1136/bmjgh-2019-001417
16. Priyandani Y, Rahem A, Djunaedi M, Athiyah U, Qomaruddin MB. Pharmacist’s knowledge of pulmonary tuberculosis in a cross sectional survey at primary health care centers in Surabaya, Indonesia. Indian J Forensic Med Toxicol. 2019;13(4):1547–1550. doi:10.5958/0973-9130.2019.00522.X
17. Jiang H, Zhang S, Ding Y, et al. Development and validation of college students’ tuberculosis knowledge, attitudes and practices questionnaire (CS-TBKAPQ). BMC Public Health. 2017;17(1):1–11. doi:10.1186/s12889-017-4960-x
18. Fan Y, Zhang S, Li Y, et al. Development and psychometric testing of the Knowledge, Attitudes and Practices (KAP) questionnaire among student Tuberculosis (TB) Patients (STBP-KAPQ) in China. BMC Infect Dis. 2018;18(1):1–10. doi:10.1186/s12879-018-3122-9
19. Guadagnoli E, Velicer WF. Relation of sample size to the stability of component patterns. Psychol Bull. 1988;103(2):265–275. doi:10.1037/0033-2909.103.2.265
20. Boateng GO, Neilands TB, Frongillo EA, Melgar-Quiñonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Heal. 2018;6(June):1–18. doi:10.3389/fpubh.2018.00149
21. World Health Organization. A Guide to Developing Knowledge, Attitude and Practice Surveys. World Health Organization Press; 2008.
22. Ministry of Health The Repuclic of Indonesia. National Guidelines for Medical Service. Management of Tuberculosis; 2020.
23. Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Heal Care. 2005;14(1):26–33. doi:10.1136/qshc.2004.011155
24. Vigenschow A, Edoa JR, Adegbite BR, et al. Knowledge, attitudes and practices regarding tuberculosis amongst healthcare workers in Moyen-Ogooué Province, Gabon. BMC Infect Dis. 2021;21(1):1–7. doi:10.1186/s12879-021-06225-1
25. Noé A, Ribeiro RM, Anselmo R, et al. Knowledge, attitudes and practices regarding tuberculosis care among health workers in Southern Mozambique. BMC Pulm Med. 2017;17(1):1–7. doi:10.1186/s12890-016-0344-8
26. Kumar G SP A, P S. A cross sectional study on knowledge, attitude and practice towards tuberculosis among health care workers. Int J Pharm Sci. 2019;10(4):2632–2646. doi:10.26452/ijrps.v10i4.1521
27. Andrade C, Menon V, Ameen S, Kumar Praharaj S. Designing and conducting knowledge, attitude, and practice surveys in psychiatry: practical guidance. Indian J Psychol Med. 2020;42(5):478–481. doi:10.1177/0253717620946111
28. Rossiter JR. Content validity of measures of abstract constructs in management and organizational research. Br J Manag. 2008;19(4):380–388. doi:10.1111/j.1467-8551.2008.00587.x
29. Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(6):382–386. doi:10.1097/00006199-198611000-00017
30. Johari J, Sahari J, Abd Wahab D, et al. Difficulty index of examinations and their relation to the achievement of programme outcomes. Procedia Soc Behav Sci. 2011;18:71–80. doi:10.1016/j.sbspro.2011.05.011
31. Perneger TV, Courvoisier DS, Hudelson PM, Gayet-Ageron A. Sample size for pre-tests of questionnaires. Qual Life Res. 2015;24(1):147–151. doi:10.1007/s11136-014-0752-2
32. Artino AR, La Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research: AMEE Guide No. 87. Med Teach. 2014;36(6):463–474. doi:10.3109/0142159X.2014.889814
33. Mathur B, Kaushik M. Data analysis of students marks with descriptive statistics object oriented system view project. Int J Recent Innov Trends Comput Commun. 2014;2:1188–1191.
34. Maharajan MK, Rajiah K, Belotindos JAS, Basa MS. Social determinants predicting the knowledge, attitudes, and practices of women toward zika virus infection. Front Public Heal. 2020;8(June):1–9. doi:10.3389/fpubh.2020.00170
35. Luba TR, Tang S, Liu Q, Gebremedhin SA, Kisasi MD, Feng Z. Knowledge, attitude and associated factors towards tuberculosis in Lesotho: a population based study. BMC Infect Dis. 2019;19(1):1–10. doi:10.1186/s12879-019-3688-x
36. Khairunnisa NA, Nasution A. Pharmacists’ perception about their roles in tuberculosis control program in Medan, Indonesia. Asian J Pharm Clin Res. 2017;10(4):256–258. doi:10.22159/ajpcr.2017.v10i4.16688
37. Karuniawati H, Putra ON, Wikantyasning ER. Impact of pharmacist counselling and leaflet on adherence of pulmonary tuberculosis patient in lung hospital in Indonesia. Indian J Tuberc. 2019;66:364–369. doi:10.1016/j.ijtb.2019.02.015
38. Morin AJS, Katrin Arens A, Marsh HW. A bifactor exploratory structural equation modeling framework for the identification of distinct sources of construct-relevant psychometric multidimensionality. Struct Equ Model. 2015;23(1):116–139. doi:10.1080/10705511.2014.961800
39. Zijlmans EAO, Tijmstra J, van der Ark LA, Sijtsma K. Item-score reliability as a selection tool in test construction. Front Psychol. 2019;9(JAN). doi:10.3389/fpsyg.2018.02298
40. Nishimura A, Tabuchi Y, Kikuchi M, Masuda R, Goto K, Iijima T. The amount of fluid given during surgery that leaks into the interstitium correlates with infused fluid volume and varies widely between patients. Anesth Analg. 2016;123(4):925–932. doi:10.1213/ANE.0000000000001505
41. Robert L, Ebel DDF. Essentials of Educational Measurement. Prentice-hall of India; 1991.
42. Douglas G, Bonett TAW. Cronbach’s alpha reliability: interval estimation, hypothesis testing, and sample size planning. J Organ Behav. 2014;36(1):3–15. doi:10.1002/job.1960
43. Hulin C, Cudeck R, Netemeyer R, Dillon WR, McDonald R, Bearden W. Cronbach’s alpha on two-item scales. J Consum Psychol. 2001;10(1–2):55–69.
44. Tsang S, Royse CF, Terkawi AS. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi J Anaesth. 2017;11(5):S80–S89. doi:10.4103/sja.SJA_203_17
45. Shou Y, Martin Sellbom HF. Fundamentals of Measurement in Clinical Psychology. Asmundson GJ ed. Elsevier; 2022.
46. Marx RG, Menezes A, Horovitz L, Jones EC, Warren RF. A comparison of two time intervals for test-retest reliability of health status instruments. J Clin Epidemiol. 2003;56(8):730–735. doi:10.1016/S0895-4356(03)00084-2
47. Denise F, Polit CTB. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Research Nurs Heal. 2006;29:489–497. doi:10.1002/nur
48. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28:563–575. doi:10.3412/jsb.16.926
49. Pradipta IS, Khairunnisa K, Bahar MA, et al. Knowledge, attitude and practice of community pharmacy personnel in tuberculosis patient detection: a sectional study in a burden tuberculosis setting. BMJ Open. 2022:1–9. doi:10.1136/bmjopen-2021-060078
50. Abdulah R, Barliana MI, Pradipta IS, Halimah E, Diantini A, Lestari K. Assessment of patient care indicators at community pharmacies in Bandung City, Indonesia. Southeast Asian J Trop Med Public Health. 2014;45(5):1196–1201.
51. Gayathri P, Shah PB, Rajanandh MG. Barriers of community pharmacists in identification and referral of presumptive tuberculosis cases in Tiruvallur district of Tamil Nadu. Indian J Tuberc. 2020;67(4):560–563. doi:10.1016/j.ijtb.2020.07.018
52. Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model. 1999;6(1):1–55. doi:10.1080/10705519909540118
53. Jampol LEEM, Tanna AP, Portney G, Watkins MP, Saddle U, Hall P. Multimedia reviews foundations of clinical research: application. Surv Opthalmology. 2002;47(6):6257. doi:10.1016/s0039-6257(02)00362-4
54. Rupani MP, Shah CJ, Dave JD, Atul V, Trivedi KGM. We are not aware of notification of tuberculosis’: a mixed-methods study among private practitioners from western India. Int J Health Plann Manage. 2021;36(4):1011–1382. doi:10.1002/hpm.3151
55. Woods AM, Mara KC, Rivera CG. Clinical pharmacists’ interventions and therapeutic drug monitoring in patients with mycobacterial infections. J Clin Tuberc Other Mycobact Dis. 2023;30(January):100346. doi:10.1016/j.jctube.2023.100346
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
