Back to Journals » Journal of Hepatocellular Carcinoma » Volume 9
Development and Validation of Prognostic Nomograms for Hepatocellular Carcinoma After Hepatectomy Based on Inflammatory Markers
Authors Hu Z , Yuan Y, Hu Z, Liu Q, Fu Y , Hou J, Sun X, Li S, Duan W, Chen M
Received 28 September 2022
Accepted for publication 17 December 2022
Published 29 December 2022 Volume 2022:9 Pages 1403—1413
DOI https://doi.org/10.2147/JHC.S390858
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr David Gerber
Zili Hu,1,2,* Yu Yuan,3,* Zhiwen Hu,1,2,* Qingbo Liu,4 Yizhen Fu,1,2 Jingyu Hou,1,2 Xuqi Sun,5 Shaoqiang Li,6 Wenbin Duan,7 Minshan Chen1,2
1Department of Liver Surgery, Sun Yat-Sen University Cancer Center, Guangzhou, 510060, People’s Republic of China; 2Collaborative Innovation Center for Cancer Medicine, State Key Laboratory of Oncology in South China, Sun Yat-Sen University Cancer Center, Guangzhou, 510060, People’s Republic of China; 3Department of Respiratory Medicine, the Second Xiangya Hospital, Central South University, Changsha, 510235, People’s Republic of China; 4Department of Hepatobiliary Surgery, Shunde Hospital, Southern Medical University (The First People’s Hospital of Shunde), Foshan, 528308, People’s Republic of China; 5Department of Hepatobiliary and Pancreatic Surgery, the First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, 310003, People’s Republic of China; 6Hepatic Pancreatobiliary Surgery Center, the First Affiliated Hospital, Sun Yat-sen University, Guangzhou, 510080, People’s Republic of China; 7Department of Hepatobiliary Surgery, Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University), Changsha, 410005, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Minshan Chen; Wenbin Duan, Fax ++86-20-87343117 ; +86-20-877557668214, Email [email protected]; [email protected]
Background: The value of lactate dehydrogenase (LDH) compared with other inflammation-based scores in predicting the outcomes of hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC) patients after curative resection remains unknown. This study aims to evaluate the predictive value of LDH and develop novel nomograms to predict postoperative recurrence and survival in these patients.
Methods: This study retrospectively collected 1560 patients with HBV-related HCC who underwent curative resection from four institutions in China. In total, 924 patients were recruited from our center and randomly divided into the training cohort (n = 616) and internal validation (n = 308) cohorts. Additionally, 636 patients were selected from three other centers as the external validation cohort. The C index of inflammation-based scores was calculated and compared in the training cohort. Novel models were developed according to multivariable Cox regression analysis in the training cohort and validated in the internal and external validation cohorts.
Results: LDH showed a higher C-index than other inflammation-based scores for recurrence survival (RFS, 0.60, 95% CI, 0.58– 0.61) and overall survival (OS, 0.65, 95% CI, 0.63– 0.68). The nomograms of RFS and OS were developed based on tumor diameter, macrovascular invasion, AFP, operative hemorrhage, tumor differentiation, tumor number and LDH and achieved a high C-index (0.78, 95% CI, 0.76– 0.79 and 0.81, 95% CI, 0.79– 0.83), which were remarkably higher than the C-indexes of the five conventional HCC staging systems (0.52– 0.62 for RFS and 0.53– 0.67 for OS). The nomograms were validated in the internal validation cohort (0.77 for RFS, 0.78 for OS) and external validation cohort (0.80 for RFS, 0.81 for OS) and performed well-fitted calibration curves.
Conclusion: The two nomograms based on inflammatory markers achieved optimal prediction for RFS and OS of patients with HBV-related HCC after hepatectomy.
Keywords: hepatocellular carcinoma, hepatectomy, inflammation-based scores, lactate dehydrogenase, nomogram
Introduction
Hepatocellular carcinoma (HCC) is the fifth most frequent cancer and the third leading cause of cancer-related mortality globally.1–3 Many staging systems have been developed to predict the overall survival (OS) of HCC patients, including the American Joint Committee on Cancer (AJCC) seventh edition,4 Barcelona Clinic Liver Cancer (BCLC),5 Okuda staging system,6 Japan Integrated Staging Score (JIS),7 Cancer of the Liver Italian Program (CLIP)8 etc. However, none of the staging systems can predict the OS of HCC patients accurately and are popularized worldwide. A powerful and universal predicting system based on objective measures is urgently needed.
Cancer-related inflammation is recognized as the seventh hallmark of cancer.9,10 In addition, hepatitis B virus (HBV) is a major cause of HCC, especially in the Asia-Pacific region, including China.11,12 Consequently, inflammation plays a vital role in HBV-related HCC. Lactate dehydrogenase (LDH) is a well-known serum inflammatory marker. It has been reported that the release of LDH from hepatocytes increases after HBV infection13,14 and LDH is a well-identified prognostic factor in HCC.15–17 However, there is no research to evaluate the predictive competence of LDH compared with other inflammation-based scores in HBV-related HCC patients after hepatectomy.
Herein, we aimed to evaluate the prognostic role of LDH in HBV-related HCC patients after hepatectomy compared with other inflammation-based scores and establish novel prediction systems with nomograms based on LDH, which give rise to a satisfying prognostic indication for HBV-related HCC patients after hepatectomy.
Methods
Study Populations and Design
We retrospectively collected consecutive patients diagnosed with HBV-related HCC who underwent liver resection as initial treatment at Sun Yat-sen University Cancer Center (SYSUCC) from June 2011 to September 2019.
Patients were included if they met the following eligibility criteria: (1) age 18 to 75 years; (2) primary resectable HBV-related HCC; (3) histological confirmation of HCC; (4) liver function at Child-Pugh class A; (5) an Eastern Cooperative Oncology Group (ECOP) performance status of 0. Patients were excluded if they met any of the following criteria: (1) coinfection with hepatitis virus C; (2) received preoperative treatment, including interventional therapy, radiofrequency ablation, etc.; (3) metastasis to extrahepatic sites, including lymph nodes, lung, etc.; (4) patients with incomplete clinical data; (5) patients who were lost to follow-up within 3 months after hepatectomy; (6) history of other malignancies; (7) non-R0 liver resection. In our center, a total of 924 consecutive patients were included and randomly distributed to a training cohort (n = 616) and an internal validation cohort (n = 308).
In addition, a total of 636 patients from three other institutions served as an external validation cohort: The First Affiliated Hospital of Sun Yat-sen University (Jan 2009 to Jun 2015, n = 312), Hunan Provincial People’s Hospital (Mar 2008 to Dec 2016, n = 222) and Shunde Hospital of Southern Medical University (Jan 2009 to Dec 2016, n = 102). The flowchart of patient selection is shown in Figure 1S. This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee Board of the four institutions.
Inflammation-Based Prognostic Scores
Blood samples were obtained within 1 week anterior to the liver resection. The inflammatory-based scores were calculated and are described in detail in Table 1S.
Following Up
In this study, all patients were observed in the first month after surgery, every 3 months within 2 years and then every 6 months thereafter. Laboratory tests (including serum AFP level, liver function tests, and blood tests) and magnetic resonance imaging (MRI) were conducted in follow-up examinations.
Definitions
Overall survival (OS) was defined as the interval between curative resection and death from any cause or the date of last follow-up. Recurrence-free survival (RFS) was defined as the time from the date of curative resection to the date at which HCC recurred. HBV-related HCC was defined as the persistence of serum hepatitis B surface antigen (HBsAg) positivity for more than 6 months before the diagnosis of HCC. We divided the histologic grade of tumor differentiation into three levels based on the Edmondson–Steiner (ES) classification:18 ES stage I was defined as high differentiation, ES stage II was defined as medium differentiation, and ES stages III and IV were defined as low differentiation. Cirrhosis was defined histologically according to the pathology of resected liver specimens.
Statistical Analysis
All statistical analyses were performed with SAS (version 26.0, SAS Institute, Cary, NC) and R 3.63 (R Foundation for Statistical Computing, Vienna, Austria, https://www.R-project.org/). Categorical variables are presented as frequencies and percentages and were compared by the chi-square test between two groups. Continuous variables are presented as the median with interquartile range and were compared by Student’s t test. The scores and cut points of the GPS, mGPS, PI, PNI, NLR, and PLR were defined and calculated as described in previous studies,19,20 which were generally recognized. In view of the lack of widely accepted cut points for the LDH and SII scores, we defined their optimal cut points (LDH = 219.2; SII = 293.6 for RFS and 366.6 for OS) using the “maxstat” R package. We calculated the C-index and area under the ROC curve (AUC) by the “Hmisc” and “time ROC” R packages to estimate the predictive value of the inflammation-based scoring system.21
Survival curves were generated by the Kaplan–Meier method and compared by log-rank. Univariable and multivariable Cox proportional hazards models were used to assess the risk factors for tumor recurrence and patient overall survival. The nomogram was formulated based on the risk factors in multivariate analysis and performed by the “rms” R package. The calibration curve was generated based on regression analysis. We used the “Hmisc” R package to compare the C-index of the nomogram and other staging systems. We used X-tile to determine the optimal cut off values to stratify the risk of patients based on nomogram scores. We applied the nomogram in the validation groups to confirm the predictive value by using the same statistical methods.
Results
Patient Characteristics
This study collected a total of 1560 HBV-related HCC patients receiving hepatectomy from four different institutions. The median follow-up time was 43.0 (95% CI 40.7–45.3) months. The total population consisted of 1315 (84%) males and 245 (16%) females. 1223 (78%) patients were under 60 years old. All patients were infected with HBV. The median tumor size was 5.6 (interquartile range: 3.98–8.1) cm. The median LDH level was 182.8 (interquartile range: 160.4–215.7) U/L. The other clinical and pathological characteristics of the patients are presented in Table 1.
 |
Table 1 Baseline Clinicopathological Characteristics of the Patients |
There were no significant differences in baseline characteristics among the 3 cohorts except that there were more female patients and fewer cirrhosis patients in the external validation cohort than in the training and internal validation cohorts from SYSUCC. The judgment of cirrhosis NY pathologists from different institutions is diverse, which may lead to the different cirrhosis rates among the four institutions.
Independent Prognostic Factors for RFS and OS
Our univariable analysis revealed that male, larger tumor size, lower tumor differentiation, more tumor number, microvascular invasion, cirrhosis, more operative hemorrhage, shorter resection margin, higher serum levels of AFP, AST, ALB and longer PT were significantly associated with tumor recurrence. Five of eight inflammation-based scores (LDH, GPS, mGPS, PI, SII) were dependent prognostic factors for RFS. Multivariate analysis identified that tumor size (p < 0.001), tumor number (p < 0.001), tumor differentiation (p = 0.005), microvascular invasion (p = 0.003) and LDH (p < 0.001) were independent prognostic factors for RFS (Table 2).
 |
Table 2 Univariate and Multivariate Analysis of Risk Factors for Overall Survival and Recurrence-Free Survival |
Our univariable analysis revealed that larger tumor size, lower tumor differentiation, microvascular invasion, more operative hemorrhage, higher serum levels of AFP, AST, ALB and longer PT were significantly associated with unfavorable overall survival. All eight inflammation-based scores were dependent prognostic factors for OS, which indicated that inflammation plays a vital role in HCC. Multivariate analysis identified that tumor size (p = 0.001), microvascular invasion (p < 0.001), operative hemorrhage (p = 0.033), AFP (p = 0.020), LDH (p = 0.030), mGPS (p < 0.001) and SII (p = 0.001) were independent prognostic factors for OS (Table 2).
Comparison of LDH and the Current Commonly Used Inflammation-Based Prognostic Systems
Plots of the time-dependent AUC for RFS and OS are shown in Figure 1, LDH performed better in predicting RFS and OS. The details of the AUC and C-indexes of the eight inflammation-based scores for RFS and OS are provided in Tables 3 and 4. LDH had a higher C-index value than all of the other scoring systems for both RFS (0.60, 95% CI, 0.58–0.61) and OS (0.65, 95% CI, 0.63–0.68).
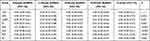 |
Table 3 Comparison of the Performance and Discriminative Ability for Recurrence-Free Between the Inflammation-Based Scores |
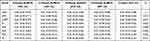 |
Table 4 Comparison of the Performance and Discriminative Ability for Overall Survival Between the Inflammation-Based Scores |
 |
Figure 1 Time-dependent AUC (area under ROC curve) plot for recurrence-free survival (A) and overall survival (B) prediction of inflammation-based scores. |
Development of Inflammation-Based Nomograms for RFS and OS in the Training Cohort
According to the multivariate analysis, tumor size, tumor number, microvascular invasion and tumor differentiation were integrated to build the nomogram of RFS; tumor size, microvascular invasion, operative hemorrhage and AFP were integrated to build the nomogram of OS. Regarding inflammation-based prognostic scores, LDH was an independent prognostic factor for both RFS and OS, and mGPS and SII were independent prognostic factors for OS as well. In view of better predictive ability compared with other inflammation-based prognostic scores, LDH was selected to build the nomograms of both RFS and OS. The details of the nomograms are shown in Figure 2.
 |
Figure 2 Nomograms for predicting the 1-, 3- and 5-year recurrence (A) and mortality (B) rates in patients with hepatitis B virus-related hepatocellular carcinoma. |
Calibration and Validation of Novel Nomograms
The C-indexes of the nomograms for RFS and OS prediction were 0.78 (95% CI, 0.76–0.79) and 0.81 (95% CI, 0.79–0.83), respectively, in the training cohort. In the internal validation cohort, the C-indexes for RFS and OS prediction were 0.77 (95% CI, 0.75–0.79) and 0.78 (95% CI, 0.75–0.81), respectively. In the external validation cohort, the C-indexes for RFS and OS prediction were 0.80 (95% CI, 0.78–0.81) and 0.81 (95% CI, 0.79–0.83), respectively. The calibration plots for the probability of recurrence and survival at 1, 3 or 5 years showed fair agreement between the prediction by the nomogram and actual observation in the training cohort (Figure 3A and B), internal validation cohort (Figure 3C and D), and external validation cohort (Figure 3E and F).
Stratifying the Risk of Patients Based on Nomogram Scores
We grouped patients in the training cohort into three subgroups according to the optimal cut-off values determined by total nomogram scores. We stratified patients into low risk (score ≤76), medium risk (score 76–117) and high risk (score >117) of recurrence based on nomogram scores of RFS, and each group represented a distinct prognosis (Figure 4A). Similar results were obtained from the internal validation cohort (Figure 4B) and the external validation cohort (Figure 4C).
Similarly, the nomogram of OS could also stratify patients into low risk (score ≤126), medium risk (score 126 to 193) and high risk (score >193) of survival and each group represented a distinct group prognosis (Figure 4D). Similar results were observed in the internal validation cohort (Figure 4E) and in the external validation cohort (Figure 4F).
Comparative Performance of Conventional Staging Systems
The C-index of the nomogram for RFS was 0.78 (95% CI, 0.76–0.79) in the training cohort, which was markedly higher than the C-indexes of five conventional staging systems, including AJCC (0.62, 95% CI, 0.60–0.63, P<0.001), Okuda (0.60, 95% CI, 0.59–0.51, P<0.001), JIS (0.60, 95% CI, 0.58–0.61, P<0.001), CLIP (0.61, 95% CI, 0.59–0.62, P<0.001) and BCLC (0.56, 95% CI, 0.55–0.57, P<0.001). We obtained similar results in the internal validation cohort and external validation cohort (Table 5).
 |
Table 5 C‐index and 95% CI of the Nomogram and Staging Systems (RFS) |
The C-index of the nomogram for OS was 0.81 (95% CI, 0.79–0.83) in the training cohort, which was markedly higher than the C-indexes of five conventional staging systems, including AJCC (0.63, 95% CI, 0.61–0.65, P<0.001), Okuda (0.61, 95% CI, 0.60–0.62, P<0.001), JIS (0.65, 95% CI, 0.63–0.67, P<0.001), CLIP (0.66, 95% CI, 0.64–0.69, P<0.001) and BCLC (0.54, 95% CI, 0.52–0.56, P<0.001). We obtained similar results in the internal validation cohort and external validation cohort (Table 6).
 |
Table 6 C‐index and 95% CI of the Nomogram and Staging Systems (OS) |
Discussion
In this study, we established two novel inflammation‐based predictive systems with nomograms in a retrospective cohort of HBV-related HCC patients after hepatectomy. Among a series of inflammation‐based scoring systems (LDH, GPS, mGPS, PI, PNI, NLR, PLR and SII), LDH was selected to construct the novel predictive system because of its better predictive ability. The other variables, including tumor diameter, macrovascular invasion, serum AFP level, operative hemorrhage, tumor differentiation and tumor number were also selected according to multivariate analysis. The two nomograms showed a more accurate value in the prediction of postsurgical outcomes compared with the conventional HCC staging systems.
Serum LDH is a standardized and simple inflammatory marker, which is easy to use in the clinic, and is a well-identified prognostic marker in multiple malignancies, including HCC, colorectal cancer, breast cancer, lymphoma, melanoma, renal cell carcinoma, and germ cell tumors.15,22–29 In addition, our study found that LDH displayed a better ability in predicting both RFS and OS of HBV-related HCC patients after hepatectomy compared with other inflammatory markers. Therefore, LDH was selected to establish the nomogram among a series of inflammatory markers.
Tumor diameter, AFP, MVI and tumor differentiation are well-known potential risk factors related to the postsurgical outcome of HCC.30–32 Our study showed that these factors were also significantly associated with the prognosis of HBV-related HCC patients after hepatectomy. Several studies have reported that the incidence of MVI ranges from 15% to 57.1% in surgical specimens and is positively correlated with tumor diameter.33,34 Interestingly, these two distinctive tumor pathological factors cooperatively affected the postsurgical prognosis of HBV-related HCC.
Operative hemorrhage was another surgical factor included in the OS nomogram model, whereas it was not a risk factor for RFS. It has been reported that operative hemorrhage is associated with poor postsurgical survival.35 The reason may be that most HVB-related HCC patients have underlying cirrhosis, which causes an increased risk of haemorrhage due to abnormal liver function or decreased platelet counts.36
In 2016, Shen’s research showed that HBeAg, AFP, resection margin, tumor number, tumor diameter, tumor capsule, MVI, and HBV-DNA level were independent risk factors for disease-free survival (DFS) or OS of HBV-related HCC patients. These independent risk factors were incorporated into the DFS and OS nomograms, respectively. Similar to Shen’s research, our study showed that AFP, tumor number, tumor diameter and MVI were independent risk factors for RFS and OS. However, HBeAg and HBV-DNA levels were not independent risk factors in our study. Recent research reports that antiviral treatments can eliminate the adverse impacts of high baseline HBV-DNA levels on the survival of HBV-related HCC patients.37 In recent years, effective antiviral drugs such as entecavir and tenofovir have been applied universally. Most patients in our study received NAs therapy and HBV-DNA levels were under good control, which could illustrate why HBeAg and baseline HBV-DNA levels were not independent risk factors in our study. In addition, inflammatory markers, which play a pivotal role in HBV-related HCC, were not considered in Shen’s research.
Notably, patients were accurately stratified into three subgroups with significantly different risks of recurrence or mortality according to the proposed nomograms of RFS and OS. Therefore, it is helpful to guide clinicians to design follow-up regimens for patients with different risks of tumor recurrence after surgery and select proper candidates to receive effective adjuvant therapy. In addition, it is helpful to guide research to stratify patients when designing randomized controlled clinical trials of postsurgical adjuvant therapy.
Our study has several limitations. First, our nomograms are based on HBV-related HCC patients. Whether the nomograms can be used in HCC patients with aetiologies other than HBV infection needs further validation. Second, although our nomograms display a satisfactory C-index based on multicenter and large sample data, selection bias is inevitable as a retrospective study. Third, the enrolled patients in this study who underwent hepatectomy for HCCs within Milan criteria might be suitable for liver transplantation. Fourth, we only include inflammatory biomarkers in blood, inflammatory biomarkers in tumor tissue are not included, such as DNASE1L3.38
In conclusion, we developed and validated two nomograms based on inflammatory markers that could accurately and objectively predict RFS and OS in patients with HBV-related HCC after curative resection. For patients with high risk of recurrence after surgery, close surveillance regimens and adjuvant therapy should be considered.
Data Sharing Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethics Approval Statement
This study was conducted according to the ethical guidelines of the 1975 Declaration of Helsinki. This research was approved by the institutional review board of four institutions.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Akinyemiju T, Abera S, Ahmed M., et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level results from the Global Burden of Disease Study 2015. JAMA Oncology. 2017;3(12):1683–1691. doi:10.1001/jamaoncol.2017.3055
2. Fitzmaurice C, Abate D, Abbasi N, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017 a systematic analysis for the Global Burden of Disease Study. JAMA Oncology. 2019;5(12):1749–1768. doi:10.1001/jamaoncol.2019.2996
3. Vos T, Abajobir AA, Abate KH. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi:10.1016/S0140-6736(17)32154-2
4. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17(6):1471–1474. doi:10.1245/s10434-010-0985-4
5. Forner A, Reig ME, de Lope CR, Bruix J. Current strategy for staging and treatment: the BCLC update and future prospects. Semin Liver Dis. 2010;30(1):61–74. doi:10.1055/s-0030-1247133
6. Okuda K, Ohtsuki T, Obata H, et al. Natural history of hepatocellular carcinoma and prognosis in relation to treatment. Cancer. 1985;56(4):918–928.
7. Kudo M, Chung H, Osaki Y. Prognostic staging system for hepatocellular carcinoma (CLIP score): its value and limitations, and a proposal for a new staging system, the Japan Integrated Staging Score (JIS score). J Gastroenterol. 2003;38(3):207–215. doi:10.1007/s005350300038
8. Cancer of the Liver Italian Program (CLIP). A new prognostic system for hepatocellular carcinoma: a retrospective study of 435 patients: the Cancer of the Liver Italian Program (CLIP) investigators. Hepatology. 1998;28(3):751–755. doi:10.1002/hep.510280322
9. Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539–545. doi:10.1016/S0140-6736(00)04046-0
10. Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–1081. doi:10.1093/carcin/bgp127
11. Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015;386(10003):1546–1555. doi:10.1016/S0140-6736(15)61412-X
12. Liang LLY, Wong GLH. Unmet need in chronic hepatitis B management. Clin Mol Hepatol. 2019;25(2):172–180. doi:10.3350/cmh.2018.0106
13. Lin M, Chen Q, Yang LY, et al. Hepatitis B virus infection and replication in primarily cultured human fetal hepatocytes. World j Gastroenterol. 2007;13(7):1027–1031. doi:10.3748/wjg.v13.i7.1027
14. Wang L, He T, Wan B, Wang X, Zhang L. Orexin A ameliorates HBV X protein-induced cytotoxicity and inflammatory response in human hepatocytes. Artif Cells, Nanomed Biotechnol. 2019;47(1):2003–2009. doi:10.1080/21691401.2019.1614014
15. Zhang JP, Wang HB, Lin YH, et al. Lactate Dehydrogenase Is an Important Prognostic Indicator for Hepatocellular Carcinoma after Partial Hepatectomy. Transl Oncol. 2015;8(6):497–503. doi:10.1016/j.tranon.2015.11.006
16. Scartozzi M, Faloppi L, Bianconi M, et al. The role of LDH serum levels in predicting global outcome in HCC patients undergoing TACE: implications for clinical management. PLoS One. 2012;7(3):e32653. doi:10.1371/journal.pone.0032653
17. Wu SJ, Lin YX, Ye H, Xiong XZ, Li FY, Cheng NS. Prognostic value of alkaline phosphatase, gamma-glutamyl transpeptidase and lactate dehydrogenase in hepatocellular carcinoma patients treated with liver resection. Int j Surgery. 2016;36(Pt A):143–151. doi:10.1016/j.ijsu.2016.10.033
18. Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer. 1954;7(3):462–503. doi:10.1002/1097-0142(195405)7:3<462::AID-CNCR2820070308>3.0.CO;2-E
19. Kinoshita A, Onoda H, Imai N, et al. Comparison of the prognostic value of inflammation-based prognostic scores in patients with hepatocellular carcinoma. Br J Cancer. 2012;107(6):988–993. doi:10.1038/bjc.2012.354
20. Proctor MJ, Morrison DS, Talwar D, et al. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer. 2011;47(17):2633–2641. doi:10.1016/j.ejca.2011.03.028
21. Rodríguez-álvarez MX, Meira-Machado L, Abu-Assi E, Raposeiras-Roubín S. Nonparametric estimation of time-dependent ROC curves conditional on a continuous covariate. Stat Med. 2016;35(7):1090–1102. doi:10.1002/sim.6769
22. Egberts F, Kotthoff EM, Gerdes S, Egberts JH, Weichenthal M, Hauschild A. Comparative study of YKL-40, S-100B and LDH as monitoring tools for Stage IV melanoma. Eur J Cancer. 2012;48(5):695–702. doi:10.1016/j.ejca.2011.08.007
23. Weide B, Elsässer M, Büttner P, et al. Serum markers lactate dehydrogenase and S100B predict independently disease outcome in melanoma patients with distant metastasis. Br J Cancer. 2012;107(3):422–428. doi:10.1038/bjc.2012.306
24. Koukourakis MI, Giatromanolaki A, Sivridis E, et al. Prognostic and predictive role of lactate dehydrogenase 5 expression in colorectal cancer patients treated with PTK787/ZK 222584 (vatalanib) antiangiogenic therapy. Clin Cancer Res. 2011;17(14):4892–4900. doi:10.1158/1078-0432.CCR-10-2918
25. Scartozzi M, Giampieri R, Maccaroni E, et al. Pre-treatment lactate dehydrogenase levels as predictor of efficacy of first-line bevacizumab-based therapy in metastatic colorectal cancer patients. Br J Cancer. 2012;106(5):799–804. doi:10.1038/bjc.2012.17
26. Brown JE, Cook RJ, Lipton A, Coleman RE. Serum lactate dehydrogenase is prognostic for survival in patients with bone metastases from breast cancer: a retrospective analysis in bisphosphonate-treated patients. Clin Cancer Res. 2012;18(22):6348–6355. doi:10.1158/1078-0432.CCR-12-1397
27. Cairo MS, Sposto R, Gerrard M, et al. Advanced stage, increased lactate dehydrogenase, and primary site, but not adolescent age (≥ 15 years), are associated with an increased risk of treatment failure in children and adolescents with mature B-cell non-Hodgkin’s lymphoma: results of the FAB LMB 96 study. J Clin Oncol. 2012;30(4):387–393. doi:10.1200/JCO.2010.33.3369
28. Armstrong AJ, George DJ, Halabi S. Serum lactate dehydrogenase predicts for overall survival benefit in patients with metastatic renal cell carcinoma treated with inhibition of mammalian target of rapamycin. J Clin Oncol. 2012;30(27):3402–3407. doi:10.1200/JCO.2011.40.9631
29. Gerlinger M, Wilson P, Powles T, Shamash J. Elevated LDH predicts poor outcome of recurrent germ cell tumours treated with dose dense chemotherapy. Eur j Cancer. 2010;46(16):2913–2918. doi:10.1016/j.ejca.2010.07.004
30. Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314. doi:10.1016/S0140-6736(18)30010-2
31. Zhang B, Zhang B, Zhang Z, et al. 42,573 cases of hepatectomy in China: a multicenter retrospective investigation. Sci China Life Sci. 2018;61(6):660–670. doi:10.1007/s11427-017-9259-9
32. Kudo M, Izumi N, Sakamoto M, et al. Survival Analysis over 28 Years of 173,378 Patients with Hepatocellular Carcinoma in Japan. Liver Cancer. 2016;5(3):190–197. doi:10.1159/000367775
33. Rodríguez-Perálvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol. 2013;20(1):325–339. doi:10.1245/s10434-012-2513-1
34. Lei Z, Li J, Wu D, et al. Nomogram for Preoperative Estimation of Microvascular Invasion Risk in Hepatitis B Virus-Related Hepatocellular Carcinoma Within the Milan Criteria. JAMA Surg. 2016;151(4):356–363. doi:10.1001/jamasurg.2015.4257
35. Wada H, Eguchi H, Nagano H, et al. Perioperative allogenic blood transfusion is a poor prognostic factor after hepatocellular carcinoma surgery: a multi-center analysis. Surg Today. 2018;48(1):73–79. doi:10.1007/s00595-017-1553-3
36. Li J, Zhou J, Yang PH, et al. Nomograms for survival prediction in patients undergoing liver resection for hepatitis B virus related early stage hepatocellular carcinoma. Eur j Cancer. 2016;62:86–95. doi:10.1016/j.ejca.2016.04.011
37. Hu Z, Sun X, Mei J, et al. Antiviral Treatments Eliminate the Adverse Impacts of High Baseline HBV Loads on the Survival of HBV-Related HCC Patients. J Hepatocellular Carcinoma. 2022;9:315–325. doi:10.2147/JHC.S363123
38. Wang S, Ma H, Li X, et al. DNASE1L3 as an indicator of favorable survival in hepatocellular carcinoma patients following resection. Aging. 2020;12(2):1171–1185. doi:10.18632/aging.102675
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


