Back to Journals » Clinical Interventions in Aging » Volume 17
Development and Validation of a Risk Nomogram Model for Predicting Recurrence in Patients with Atrial Fibrillation After Radiofrequency Catheter Ablation
Authors Zhao Z , Zhang F, Ma R, Bo L, Zhang Z, Zhang C, Wang Z, Li C, Yang Y
Received 2 June 2022
Accepted for publication 6 September 2022
Published 25 September 2022 Volume 2022:17 Pages 1405—1421
DOI https://doi.org/10.2147/CIA.S376091
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Zhihao Zhao, Fengyun Zhang, Ruicong Ma, Lin Bo, Zeqing Zhang, Chaoqun Zhang, Zhirong Wang, Chengzong Li, Yu Yang
Department of Cardiology, The Affiliated Hospital of Xuzhou Medical University, Xuzhou, People’s Republic of China
Correspondence: Yu Yang, Tel +86-15651359875, Email [email protected]
Purpose: This study aimed to develop and validate a risk nomogram model for predicting the risk of atrial fibrillation recurrence after radiofrequency catheter ablation.
Patients and Methods: A retrospective observational study was conducted using data from 485 patients with atrial fibrillation who underwent the first radiofrequency ablation in our hospital from January 2018 to June 2021. All patients were randomized into training cohort (70%; n=340) and validation cohort (30%; n=145). Univariate and multivariate logistic regression analyses were used to identify independent risk factors. The predictive nomogram model was established by using R software. The nomogram was developed and evaluated based on differentiation, calibration, and clinical efficacy by concordance statistic (C-statistic), calibration plots, and decision curve analysis (DCA), respectively.
Results: The nomogram was established by four variables including left atrial diameter (OR 1.057, 95% CI 1.010– 1.107, P=0.018), left ventricular ejection fraction (OR 0.943, 95% CI 0.905– 0.982, P=0.005), type of atrial fibrillation (OR 2.164, 95% CI: 1.262– 3.714), and systemic inflammation score (OR 1.905, 95% CI 1.408– 2.577). The C-statistic of the nomogram was 0.741 (95% CI: 0.689– 0.794) in the training cohort and 0.750 (95% CI: 0.670– 0.831) in the validation cohort. The calibration plots showed good agreement between the predictions and observations in the training and validation cohorts. Decision curve analysis and clinical impact curves indicated the clinical utility of the predictive nomogram.
Conclusion: The nomogram model has good discrimination and accuracy, which can screen high-risk groups intuitively and individually, and has a certain predictive value for atrial fibrillation recurrence in patients after radiofrequency ablation.
Keywords: nomogram, risk prediction model, atrial fibrillation, radiofrequency catheter ablation, recurrence
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia in clinical practice, affecting more than 35 million individuals worldwide annually.1 Atrial fibrillation is associated with a high incidence of stroke, peripheral embolism, and mortality, which aggravates the health and economic burden on both family and society.2,3
Radiofrequency catheter ablation (RFCA) has been widely used in treatment for atrial fibrillation,4 but the high rate of recurrence after RFCA remains a significant clinical problem during the postoperative follow-up period.5 Various risk scores for atrial fibrillation recurrence have now been identified, but the discriminatory ability of these scores is highly variable, and there are no widely used models to quantitatively predict AF recurrence in patients after RFCA.6 Mulder et al compared ten previously described risk scores for atrial fibrillation recurrence and found that CAAP-AF score,7 established by Winkle et al, demonstrated better predictive ability for AF recurrence than the other scores.8 However, it remains a challenge to make reliable discrimination whether patients with atrial fibrillation will recur after RFCA.
Inflammation plays an important role in AF, which can lead to atrial electrical remodeling and structural remodeling.9 Systemic inflammatory status was closely correlated with AF recurrence.10 However, few previous prediction models integrated with the inflammatory indicators to predict AF recurrence. The systemic inflammation score (SIS)11 was developed by Chang et al as an index to evaluate the intensity of systemic inflammatory status, and it may be useful for the prediction of AF recurrence.
This retrospective study analyzed clinical data from AF patients after RFCA in our cardiology department. Independent risk factors for AF recurrence were identified by univariate and multivariate logistic regression analysis. The aim of our study was to develop and validate a nomogram model for evaluating the risk of AF recurrence in patients after operation so that physicians can intervene in high-risk patients early and reduce the rate of AF recurrence after RFCA.
Materials and Methods
Study Population
The flow chart of our study was shown in Figure 1. This retrospective study was based on the Electronic Medical Record system of patients admitted to the inpatient Department of Cardiology of the Affiliated Hospital of Xuzhou Medical University. Patients who underwent first-time radiofrequency ablation from January 2018 to June 2021 were included in the study. Based on the inclusion and exclusion criteria, 485 patients were eligible for analysis. The inclusion criteria were as follows: non-valvular AF; radiofrequency catheter ablation for the first time. Exclusion criteria were as follows: severe hepatic or renal dysfunction; organic heart disease; recent blood transfusions or other surgery; preoperative infections; combined with hematologic or rheumatic immune system diseases; a history of tumor.
 |
Figure 1 Flow chart of our study. Abbreviation: RFCA, radiofrequency catheter ablation. |
Radiofrequency Ablation Operation Method
A three-dimensional reconstruction of the left atrium and pulmonary veins were completed with the aid of the electroanatomic mapping system (CARTO 3). Circumferential pulmonary vein isolation was performed in all patients using a radiofrequency ablation catheter. Additional ablation was added if necessary, such as the left atrial apex, posterior line, anterior line, and even mitral isthmus. Some patients also underwent direct current cardioversion if atrial fibrillation still existed after initial ablation. All patients took amiodarone and rivaroxaban regularly for at least 3 months after the operation.
Definition and Follow Up
Patients were followed up regularly in our clinic at 1 month, 3 months, and 6 months after the operation and a 12-lead electrocardiogram (ECG) and 24-hour Holter were recorded. If patients had AF symptoms such as palpitations, chest pain, and fatigue, they were recommended to perform a 12-lead ECG and 24-hour Holter. After 6 months, they were followed up regularly in the clinic or by remote telephone.
Atrial fibrillation recurrence: any atrial tachyarrhythmias (AF, atrial flutter, and atrial tachycardia) that lasted over 30 seconds more than 3 months after the ablation was considered as AF recurrence. Atrial tachyarrhythmias that occurred within 3 months did not represent the failure of the operation.
Systemic inflammation score (SIS) was composed by lymphocyte-to-monocyte ratio and albumin. The total points of systemic inflammation score (SIS) were 0–2, lymphocyte-to-monocyte ratio (LMR) < 4.44 was scored as 1, lymphocyte-to-monocyte ratio (LMR) ≥4.44 was scored as 0, and albumin < 40 g/L was scored as 1, and albumin ≥ 40 g/L was scored as 0.
CAAP-AF score was composed by coronary artery heart disease, left atrial diameter, age, type of AF, number of failed antiarrhythmic drugs and gender. The total points of CAAP-AF score were 0–13, coronary heart disease was scored as 1; Left atrial diameter < 4.0 cm was scored as 0, 4.0–4.4 cm was scored as 1, 4.5–4.9 cm was scored as 2, 5.0–5.4 cm was scored as 3, and ≥5.5 cm was scored as 4, Age < 50 years old was scored as 0, 50–59 years old was scored as 1, 60–69 years old was scored as 2 and age ≥70 years old was scored as 3; persistent atrial fibrillation was scored as 2; none failed anti-arrhythmic drugs (AAD) was scored as 0, one or two failed AAD was scored as 1, and >2 failed AAD was scored as 2; women was scored as 1.
Severe hepatic disease was defined as significant liver injury as an AST and ALT elevations increased by 5 or more times the upper limit of normal.
Severe renal disease was defined as eGFR< 30mL/min·1.73 m−2.
Organic heart disease includes congenital heart disease (ventricular septal defect, atrial septal defect, patent ductus arteriosus, tetralogy of Fallot, etc.), heart valve disease (mitral, tricuspid, aortic, pulmonary, etc.) and cardiomyopathy (hypertrophic cardiomyopathy, dilated cardiomyopathy, etc.)
Data Collection
Baseline and clinical characteristics were collected from the medical record system by trained physicians who were blinded to the aim of the study. The following blood markers were recorded including counts of white blood cell, lymphocyte, monocyte, platelet, hemoglobin, hs-CRP, glycosylated hemoglobin, fasting plasma glucose, serum creatinine (SCr), serum uric acid (SUA), estimated glomerular filtration rate (eGFR), albumin, urea, cystatin C, triglyceride, total cholesterol (TC), low-density lipoprotein-C (LDL-C), and high-density lipoprotein-C (HDL-C). Cardiac ultrasound, 12-lead electrocardiogram, and 24-hour Holter were obtained for analysis. Demographics and clinical characteristics were collected from patients including age, sex, body mass index (BMI), duration of AF, type of AF, CHA2DS2-VASc score, CAAP-AF score, systemic inflammation score, smoking history, hypertension, diabetes, coronary artery disease, history of myocardial infarction and stroke.
Statistical Analysis
Categorical variables were expressed as counts and percentages (%), while continuous variables were expressed as mean standard deviation or median and interquartile range. The independent samples t-tests were used to compare parameter values between the two groups, Mann–Whitney U-tests were used to compare non-parameter values between the two groups, and chi-square tests were used to compare categorical variables. Univariate analysis was performed using univariate logistic regression analysis. The significance of each variable in the training cohort was assessed by univariate logistic regression analysis in order to investigate independent risk factors for recurrence in patients with atrial fibrillation after the operation. Variables with P < 0.05 in the univariate analysis were considered as potential candidates and included in the multivariate analysis. Variables used in the nomogram model had P<0.05 in the multivariable logistic regression analysis. Finally, we calculated regression coefficients and OR for each variable in the model using two-sided 95% confidence intervals. We assessed the predictive model based on three quantities, namely discriminative capacity, calibration ability, and clinical effectiveness. Since the consistency index (C-index) is equal to the area under the receiver operating characteristic curve (AUC) in logistic regression, we used the AUC to evaluate the discriminative ability of the nomogram. At the same time, area under curve comparison between the nomogram and the CAAP-AF score was performed by DeLong’s test. Calibration accuracy was assessed by calibration plots and Hosmer-Lemeshow tests. Clinical effectiveness was assessed by decision curve analysis (DCA). All tests were two-tailed, and P < 0.05 were considered statistically significant. All statistical analyses were performed using SPSS version 26.0 (SPSS Inc., Chicago, IL, USA), Stata version 13.0 (Stata Inc., College Station, TX, USA), and the statistical package R, Version 4.0.3 (https://cran.r-project.org) were prepared.
Results
Baseline Patient Characteristics
According to the follow-up results, 207 patients developed atrial fibrillation recurrence after RFCA. General information and laboratory data for both groups are shown in Table 1. The proportion of patients with atrial fibrillation recurrence after RFCA was 43.8% (149/340) in the training cohort and 40% (58/145) in the validation cohort. Baseline characteristics of patients in the training and validation cohorts are listed in Table 2. There were significant differences between the recurrent and non-recurrent groups in terms of AF type, CHA2DS2-VASc score, BMI, hypertension, SIS, left atrial diameter (LAD), left ventricular ejection fraction (LVEF), serum uric acid, lymphocyte count, lymphocyte-to-monocyte ratio (LMR), and albumin (P<0.05).
 |  |  |
Table 1 Comparison of Clinical Baseline Information Between the Recurrent and Non-Recurrent Groups of Patients with Atrial Fibrillation |
 |  |  |
Table 2 Comparison of the Information in the Training and Validation Cohorts |
Univariate and Multivariate Logistic Regression Analysis
Univariate logistic regression results are shown in Table 3, type of AF, CHA2DS2-VASc score, BMI, hypertension, SIS, LAD, LVEF, serum uric acid, lymphocyte count, lymphocyte-to-monocyte ratio (LMR), and albumin were statistically significant (P<0.05). Significant indicators were screened and included in multivariate logistic regression analysis. Systemic inflammation scores included albumin and lymphocyte-to-monocyte ratio (LMR) and their lymphocyte counts, so these variables were not included in the logistic regression analysis model. The results showed that left atrial diameter, left ventricular ejection fraction, type of AF, and SIS were independent influences in patients with AF after radiofrequency ablation (P<0.05), as shown in Table 4.
 |
Table 3 Univariate Logistic Regression Analysis of Recurrence Based on Data in the Training Cohort |
 |
Table 4 Multivariate Logistic Regression Analysis of Recurrence Based on Data in the Training Cohort |
Predictive Nomogram Development
Based on these analyses, we developed a nomogram model for predicting AF recurrence in patients after RFCA using four variables: left atrial diameter (LAD), left ventricular ejection fraction (LVEF), type of AF, and systemic inflammation score (SIS). As is shown in Figure 2, each of these independent predictors was projected upward to the “point” of that value at the top of the nomogram to obtain a score from 0 to 100, and the total score of these points was then recorded to predict the probability of postoperative AF recurrence. The result of the Hosmer-Lemeshow test was χ 2 = 3.697 (P=0.883), indicating a good degree of calibration of the model. The calibration curve showed good agreement between the predicted and actual risk of postoperative recurrence in patients with AF from Figure 3A. The C-statistic was 0.741 (95% CI: 0.689–0.794). The prediction model showed good discrimination, as shown in Figure 4A. In addition, the nomogram showed a better predictive value for AF recurrence compared with the CAAP-AF score (Z=2.091, P=0.036) from Figure 5.
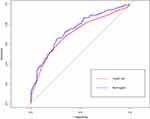 |
Figure 5 The receiver operator characteristic curves of the nomogram and the CAAP-AF score. |
Validation of the Nomogram
In the validation cohort, there were 58 (40%) patients with AF recurrences after RFCA. Hosmer-Lemeshow test was χ2 = 7.042 (P=0.531). The calibration curve showed good agreement and good fit of the nomogram model, as shown in Figure 3B. The C-statistic was 0.750 (95% CI: 0.670 −0.831), indicating good discriminatory performance of the prediction model, as shown in Figure 4B.
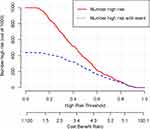
Decision Curve Analysis of the Prediction Model
Decision curve analysis (DCA) showed the ability of the nomogram to predict AF recurrence (Figure 6A and B). A horizontal line represents the intervention-none and the net benefit with zero, the oblique line shows intervention-all-patients. From the decision curves, the range of high-risk threshold probabilities was wide and applicable to both the training and validation sets, which suggests that the nomogram was clinically useful. From Figure 7, we can see that the red curve shows the number of subjects classified as positive by the nomogram model at each threshold probability (Number high risk); the blue curve (Number high risk with event) is the number of true positives at each threshold probability. It implies a good consistency between the actual distribution and the distribution predicted by the nomogram.
Discussion
Radiofrequency catheter ablation has been widely used in the clinical treatment of AF.12 However, not all patients have sinus rhythm restored after RFCA and the high rate of AF recurrence remains a challenge for clinicians. Accurate prediction of AF recurrence may guide the clinical decision and influence patient selection for ablation.13 Consequently, it is essential to estimate each patient’s individual risk of recurrent AF before ablation.
This study found a 42.7% (207/485) incidence of recurrence after RFCA in patients with AF. We screened for independent predictive factors for AF recurrence by comparing the baseline data of 485 patients with atrial fibrillation. Also, a nomogram model for predicting atrial fibrillation recurrence was developed according to standard procedures. It is worth highlighting that our study is the first to add the systemic inflammation score (SIS) to the prediction model for predicting AF recurrence. In addition, this study made it easier to predict the probability of recurrence after radiofrequency ablation in patients with atrial fibrillation by nomogram.
The results of this study showed that AF patients had a significant higher recurrence rate in the left atrial diameter (LAD) >43.5 mm group than the LAD ≤43.5 mm (60.1% vs 25.9%, P < 0.001). Previous reports have demonstrated that LAD is a predictor of recurrences after RFCA.14,15 The enlargement of left atrium can result in the structural and electrical remodeling of the left atrium, which promote the persistence of atrial arrhythmias.16,17 Our study shows that patients with low LVEF are more likely to develop AF recurrence. The reason for this may be that low LVEF leads to the elevation of left atrial pressure18 and the prolonged elevation of left atrial pressure can lead to myocardial damage and atrial fibrosis.19,20 Atrial fibrosis can cause conduction disturbances and make contribution to the progression of atrial remodeling, which result in AF.21,22 Previous research showed that the SIS was associated with higher risk of AF occurrence.23 In our study, Systemic Inflammation Score (SIS) is related to an increased risk of AF recurrence after RFCA. SIS is an index to evaluate the intensity of systemic inflammatory status.11 Inflammation has been implicated in the pathophysiology of atrial fibrillation (AF) and participates in the process of myocardial fibrosis, which is the potential mechanism of AF recurrence.10,24 The SIS is a novel prognostic score formulated by albumin and lymphocyte-to-monocyte ratio (LMR). Inflammation promotes lymphocyte apoptosis25 and the increase in monocytes reflects the level of chronic systemic inflammation.26 In addition, LMR has been proved to be a potential prognostic predictor of all-cause mortality in AF patients.27 It is well established that lower levels of albumin were prospectively associated with a higher risk of AF.28 The chemical structure of albumin can transport inflammatory mediators, modulate inflammatory reactions, and prevent damage of myocardium caused by oxidative stress.29 Besides, albumin reflects the nutritional status of the body, which has been shown to be associated with recurrence of atrial fibrillation.30 Patients with persistent AF had a higher risk of recurrence than patients with paroxysmal AF. Persistent atrial fibrillation leads to atrial fibrosis that leads to electrical remodeling and structural remodeling.31 Therefore, the application of these parameters in the model is more than adequate. Nomogram was a visual chart established by different lines of high and low level to predict the incidence of clinical events.32 In this study, we finally included four predictors: “LAD”, “LVEF”, “Type of AF”, and “SIS” to create a nomogram model. The nomogram had good discriminatory ability in the training and validation cohorts. A certain degree of validity and applicability of the model has been demonstrated, making our risk prediction more clinically attractive. Doctors can predict the probability of recurrence in patients with AF after RFCA based on the summation of scores for each risk factor.
In summary, nomogram contains four risk factors to predict AF recurrence after RFCA. The strength of our study is that the predictors in the model were routinely tested before ablation. which enables physicians to assess the risk of atrial fibrillation recurrence and take further preoperative precautions. The nomogram has high clinical application and deserves further use.
Limitations
There are several limitations to this study. First, this was a single-center retrospective study, which would affect patient selection and produce selection bias. Second, patients with asymptomatic atrial fibrillation may be overlooked during follow-up. Finally, the cases in this study were a small sample size in the same hospital, and the clinical predictive value still requires a model for further evaluation by multicenter and expanded sample size.
Conclusion
We developed and internally validated a novel nomogram to predict the risk of recurrence after RFCA in patients with AF. The nomogram has good discrimination and accuracy, which can screen high-risk groups intuitively and individually, and has a certain predictive value for atrial fibrillation recurrence in patients after radiofrequency ablation. In addition, it is necessary to confirm these findings through prospective, randomized, multicenter studies.
Ethics Statement
The study was conducted in accordance with the Declaration of Helsinki and has been approved by the Medical Ethics Committee of the Affiliated Hospital of Xuzhou Medical University. Due to the study being a retrospective analysis, the review committee waived the requirement for written informed consent. Confidential patient information was removed from the entire data set prior to analysis.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chung MK, Refaat M, Shen WK, et al. Atrial fibrillation: JACC council perspectives. J Am Coll Cardiol. 2020;75(14):1689–1713. doi:10.1016/j.jacc.2020.02.025
2. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS): the Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
3. Rillig A, Magnussen C, Ozga AK, et al. Early rhythm control therapy in patients with atrial fibrillation and heart failure. Circulation. 2021;144(11):845–858. doi:10.1161/CIRCULATIONAHA.121.056323
4. Poole JE, Bahnson TD, Monahan KH, et al. Recurrence of atrial fibrillation after catheter ablation or antiarrhythmic drug therapy in the CABANA trial. J Am Coll Cardiol. 2020;75(25):3105–3118. doi:10.1016/j.jacc.2020.04.065
5. Erhard N, Metzner A, Fink T. Late arrhythmia recurrence after atrial fibrillation ablation: incidence, mechanisms and clinical implications. Herzschrittmacherther Elektrophysiol. 2022;33(1):71–76. doi:10.1007/s00399-021-00836-6
6. Li Z, Wang S, Hidru TH, et al. Long atrial fibrillation duration and early recurrence are reliable predictors of late recurrence after radiofrequency catheter ablation. Front Cardiovasc Med. 2022;9:864417. doi:10.3389/fcvm.2022.864417
7. Winkle RA, Jarman JW, Mead RH, et al. Predicting atrial fibrillation ablation outcome: the CAAP-AF score. Heart Rhythm. 2016;13(11):2119–2125. doi:10.1016/j.hrthm.2016.07.018
8. Mulder MJ, Kemme M, Hopman L, et al. Comparison of the predictive value of ten risk scores for outcomes of atrial fibrillation patients undergoing radiofrequency pulmonary vein isolation. Int J Cardiol. 2021;344:103–110. doi:10.1016/j.ijcard.2021.09.029
9. Harada M, Nattel S. Implications of inflammation and fibrosis in atrial fibrillation pathophysiology. Card Electrophysiol Clin. 2021;13(1):25–35. doi:10.1016/j.ccep.2020.11.002
10. Wu N, Xu B, Xiang Y, et al. Association of inflammatory factors with occurrence and recurrence of atrial fibrillation: a meta-analysis. Int J Cardiol. 2013;169(1):62–72. doi:10.1016/j.ijcard.2013.08.078
11. Chang Y, An H, Xu L, et al. Systemic inflammation score predicts postoperative prognosis of patients with clear-cell renal cell carcinoma. Br J Cancer. 2015;113(4):626–633. doi:10.1038/bjc.2015.241
12. Rottner L, Bellmann B, Lin T, et al. Catheter ablation of atrial fibrillation: state of the art and future perspectives. Cardiol Ther. 2020;9(1):45–58. doi:10.1007/s40119-019-00158-2
13. Sato T, Sotomi Y, Hikoso S, et al. Sex differences in the efficacy of pulmonary vein isolation alone vs. extensive catheter ablation in patients with persistent atrial fibrillation. Circ J. 2022;86(8):1207–1216. doi:10.1253/circj.CJ-21-0671
14. Guo F, Li C, Yang L, et al. Impact of left atrial geometric remodeling on late atrial fibrillation recurrence after catheter ablation. J Cardiovasc Med. 2021;22(11):909–916.
15. Peng Z, Wen-Heng L, Qing Z, et al. Risk factors for late recurrence in patients with nonvalvular atrial fibrillation after radiofrequency catheter ablation. Ann Noninvasive Electrocardiol. 2021;27:e12924. doi:10.1111/anec.12924
16. den Uijl DW, Delgado V, Bertini M, et al. Impact of left atrial fibrosis and left atrial size on the outcome of catheter ablation for atrial fibrillation. Heart. 2011;97(22):1847–1851. doi:10.1136/hrt.2010.215335
17. Kriatselis C, Unruh T, Kaufmann J, et al. Long-term left atrial remodeling after ablation of persistent atrial fibrillation: 7-year follow-up by cardiovascular magnetic resonance imaging. J Interv Card Electrophysiol. 2020;58(1):21–27. doi:10.1007/s10840-019-00584-1
18. Hussein AA, Saliba WI, Barakat A, et al. Radiofrequency ablation of persistent atrial fibrillation: diagnosis-to-ablation time, markers of pathways of atrial remodeling, and outcomes. Circ Arrhythm Electrophysiol. 2016;9(1):e003669. doi:10.1161/CIRCEP.115.003669
19. Zhao J, Chen M, Zhuo C, Huang Y, Zheng L, Wang Q. The effect of renin-angiotensin system inhibitors on the recurrence of atrial fibrillation after catheter ablation. Int Heart J. 2020;61(6):1174–1182. doi:10.1536/ihj.20-346
20. Zhao Y, Di Biase L, Trivedi C, et al. Importance of non-pulmonary vein triggers ablation to achieve long-term freedom from paroxysmal atrial fibrillation in patients with low ejection fraction. Heart Rhythm. 2016;13(1):141–149. doi:10.1016/j.hrthm.2015.08.029
21. Sagnard A, Hammache N, Sellal JM, Guenancia C. New Perspective in Atrial Fibrillation. J Clin Med. 2020;9(11):3713. doi:10.3390/jcm9113713
22. Chen G, Chelu MG, Dobrev D, Li N. Cardiomyocyte inflammasome signaling in cardiomyopathies and atrial fibrillation: mechanisms and potential therapeutic implications. Front Physiol. 2018;9:1115. doi:10.3389/fphys.2018.01115
23. Zhang H, Li J, Chen X, et al. Association of systemic inflammation score with atrial fibrillation: a case-control study with propensity score matching. Heart Lung Circ. 2018;27(4):489–496. doi:10.1016/j.hlc.2017.04.007
24. Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015;12(4):230–243. doi:10.1038/nrcardio.2015.2
25. Oksuz F, Elcik D, Yarlioglues M, et al. The relationship between lymphocyte-to-monocyte ratio and saphenous vein graft patency in patients with coronary artery bypass graft. Biomark Med. 2017;11(10):867–876. doi:10.2217/bmm-2017-0079
26. Quan XQ, Wang RC, Zhang Q, Zhang CT, Sun L. The predictive value of lymphocyte-to-monocyte ratio in the prognosis of acute coronary syndrome patients: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2020;20(1):338. doi:10.1186/s12872-020-01614-x
27. Yu Y, Wang S, Wang P, et al. Predictive value of lymphocyte-to-monocyte ratio in critically Ill patients with atrial fibrillation: a propensity score matching analysis. J Clin Lab Anal. 2022;36(2):e24217. doi:10.1002/jcla.24217
28. Mukamal KJ, Tolstrup JS, Friberg J, Grønbaek M, Jensen G. Fibrinogen and albumin levels and risk of atrial fibrillation in men and women (the Copenhagen City Heart Study). Am J Cardiol. 2006;98(1):75–81. doi:10.1016/j.amjcard.2006.01.067
29. Arroyo V, García-Martinez R, Salvatella X. Human serum albumin, systemic inflammation, and cirrhosis. J Hepatol. 2014;61(2):396–407. doi:10.1016/j.jhep.2014.04.012
30. Zhu S, Zhao H, Zheng M, Peng J. The impact of malnutrition on atrial fibrillation recurrence post ablation. Nutr Metab Cardiovasc Dis. 2021;31(3):834–840. doi:10.1016/j.numecd.2020.12.003
31. Yan Q, Dong J, Ma C. Recurrent pseudo focal atrial tachycardia after ablation of persistent atrial fibrillation. Acta Cardiol. 2013;68(2):213–215. doi:10.1080/AC.68.2.2967283
32. Xiao S, Zhang L, Wu Q, et al. Development and validation of a risk nomogram model for predicting revascularization after percutaneous coronary intervention in patients with acute coronary syndrome. Clin Interv Aging. 2021;16:1541–1553. doi:10.2147/CIA.S325385
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.