Back to Journals » Infection and Drug Resistance » Volume 16
Development and Validation of a Nomogram Prediction Model for Multidrug-Resistant Organisms Infection in a Neurosurgical Intensive Care Unit
Authors Wang Y , Zhang J, Chen X, Sun M, Li Y, Wang Y, Gu Y, Cai Y
Received 25 July 2023
Accepted for publication 21 September 2023
Published 9 October 2023 Volume 2023:16 Pages 6603—6615
DOI https://doi.org/10.2147/IDR.S411976
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Ya Wang,1,* Jiajia Zhang,2,* Xiaoyan Chen,1,* Min Sun,3 Yanqing Li,4 Yanan Wang,5 Yan Gu,6 Yinyin Cai1
1Neurosurgical Intensive Care Unit, Department of Neurosurgery, Affiliated Hospital of Nantong University, Nantong, Jiangsu, People’s Republic of China; 2Neurosurgery Section Two, Department of Neurosurgery, Affiliated Hospital of Nantong University, Nantong, Jiangsu, People’s Republic of China; 3Department of Geriatrics Section Three, Affiliated Hospital of Nantong University, Nantong, Jiangsu, People’s Republic of China; 4Department of Neurosurgery, Affiliated Hospital of Nantong University, Nantong, Jiangsu, People’s Republic of China; 5Respiratory and Critical Care Medicine Intensive Care Unit, Affiliated Hospital of Nantong University, Nantong, Jiangsu, People’s Republic of China; 6Infection Management Office, Affiliated Hospital of Nantong University, Nantong, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaoyan Chen, Email [email protected]
Objective: To develop a predictive model for assessing the risk of multidrug-resistant organisms (MDROs) infection and validate its effectiveness.We conducted a study on a total of 2516 patients admitted to the neurosurgery intensive care unit (NICU) of a Grade-III hospital in Nantong City, Jiangsu Province, China, between January 2014 and February 2022. Patients meeting the inclusion criteria were selected using convenience sampling. The patients were randomly divided into modeling and validation groups in a 7:3 ratio. To address the category imbalance, we employed the Synthetic Minority Over-sampling Technique (SMOTE) to adjust the MDROs infection ratio from 203:1558 to 812:609 in the training set. Univariate analysis and logistic regression analysis were performed to identify risk factors associated with MDROs infection in the NICU. A risk prediction model was developed, and a nomogram was created. Receiver operating characteristic (ROC) analysis was used to assess the predictive performance of the model.
Patients and Methods:
Results: Logistic regression analysis revealed that sex, hospitalization time, febrile time, invasive operations, postoperative prophylactic use of antibiotics, mechanical ventilator time, central venous catheter indwelling time, urethral catheter indwelling time, ALB, PLT, WBC, and L% were independent predictors of MDROs infection in the NICU. The area under the ROC curve for the training set and validation set were 0.880 (95% CI: 0.857– 0.904) and 0.831 (95% CI: 0.786– 0.876), respectively. The model’s prediction curve closely matched the ideal curve, indicating excellent predictive performance.
Conclusion: The prediction model developed in this study demonstrates good accuracy in assessing the risk of MDROs infection. It serves as a valuable tool for neurosurgical intensive care practitioners, providing an objective means to effectively evaluate and target the risk of MDROs infection.
Keywords: multidrug-resistant, infection, neurosurgical intensive care unit, nomogram
Introduction
Multiple drug-resistant microorganisms (MDROs) are bacteria that exhibit resistance to three or more antimicrobial agents,1 include methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococcus aureus (VRE), carbapenem-resistant Enterobacteriaceae (CRE), multidrug-resistant Pseudomonas aeruginosa (MDR-PA), and multidrug-resistant Acinetobacter baumannii (MDR-AB). The global mortality attributed to MDROs was reported to be 700,000 in 2015, and this number is projected to surpass 10 million by 2050.2 MDROs infections have emerged as a significant issue in nosocomial infections worldwide,3,4 particularly in intensive care units (ICUs).5–7 Numerous studies have highlighted that MDROs infections contribute substantially to morbidity and mortality among hospitalized patients, resulting in prolonged hospital stays and increased healthcare costs.8–11 Consequently, there is an urgent need to address the prevention and intervention of MDROs infections.
The neurosurgical intensive care unit (NICU) is a specialized facility that provides treatment and care for critically ill and comatose patients. These patients often experience disorders of consciousness, underlying chronic diseases, complex medical conditions, compromised immune function, and pathophysiological abnormalities. Additionally, tracheotomy, endotracheal intubation, and mechanical ventilation are commonly employed during their treatment. The invasive nature of these procedures increases the risk of bacterial infection and inflammation.11,12 Moreover, existing studies13–16 have demonstrated an alarming prevalence of MDROs infection in the NICU.
However, there are limitations in the advancement of MDRO therapy. Inappropriate and excessive use of antibiotics can lead to various adverse effects in patients. Choosing appropriate antibiotic treatment options for the high-risk population susceptible to MDROs infection and implementing predictive intervention management pose significant challenges for clinicians. Although numerous studies have investigated the risk factors associated with MDROs infection, most have focused solely on describing these factors and have provided limited information on predictors of MDRO colonization or infection.
Considering the aforementioned circumstances, the objective of this study was to develop a user-friendly nomogram that predicts the likelihood of MDROs infection among NICU patients. The aim is to identify patients at high risk of MDROs in NICU settings, facilitating the implementation of tailored antibiotic treatment plans and preventive management measures.
Methods
Patients and Study Design
Using convenience sampling, we retrospectively selected 2606 patients admitted to the neurosurgery intensive care unit of Nantong University Affiliated Hospital between January 2014 and February 2022. According to our inclusion and exclusion criteria, 31 consecutive NICU admissions during the same hospitalization, 18 patients younger than 18 years, and 41 patients with incomplete clinical and laboratory data were excluded. Ultimately, 2516 patients were enrolled in the study. Through literature review and expert panel discussions, this study identified factors associated with MDROs infection. Clinical data from all patients admitted to the neurosurgical intensive care unit were collected using the hospital’s intelligent integrated medical platform (Intelligent & Integrated Healthcare, IIH). The collected data included age, gender, disease diagnosis, length of stay, duration of fever, surgical history, number of hospitalizations, prophylactic antibiotic treatment, duration of first postoperative antibiotic treatment, antibiotic combinations, duration of mechanical ventilation, retention of central venous catheters, retention of urinary catheters, levels of albumin, total bilirubin, creatinine, white blood cell count, neutrophil ratio, lymphocyte ratio, and platelet count. Disease-related data and laboratory tests were collected on day 3 of hospital admission.
Pathogen Detection
The laboratory doctors at our hospital conducted biological sample testing. Bacterial identification was performed using the full-automatic microbial identification machine PhoenixTM-100. The drug sensitivity experiment method used for strain resistance identification was the K-B method, also known as the paper diffusion method. The testing process and drug susceptibility test results adhered to the standards set by the Clinical and Laboratory Standards Institute (CLSI) 2020 standard and the requirements outlined in the National Health and Family Planning Commission of China’s National Clinical Laboratory Test Operation Procedure.
Diagnostic Criteria for MDROs
MDROs are bacteria that demonstrate resistance to three or more antimicrobial drugs commonly used in clinical practice. The diagnosis of MDROs infection in this study was determined by clinicians and reviewed by the hospital’s infection department.
Inclusion Criteria
(1) adult patients aged 18 years or older; (2) MDROs infection occurring 48 hours after admission to the neurosurgical intensive care unit, meeting the diagnostic criteria for MDROs infection.
Exclusion Criteria
(1) MDROs infection diagnosed or occurring within 48 hours; (2) death or treatment abandonment within 48 hours; (3) multiple NICU admissions during the same hospitalization; (4) incomplete clinical and laboratory examination data.
Model Building
Patients were randomly assigned in a 7:3 ratio to either the model group or the validation group using R software. In the construction module, we used univariate and multivariate logistic regression analysis to determine the independent risk factors. In the multivariate analysis, we selected the independent variables with a significance level of P < 0.1 in the univariate analysis and utilized the least information criterion (Akaike information criterion, AIC) to choose the final prediction model, which was a logistic regression model. The nomogram model was obtained using R software.
Modelling Verification
To evaluate the discrimination and calibration of the constructed prediction model, we internally and externally verified it by using the receiver operating characteristic curve (ROC) and calibration curve on two patient groups. The area under the ROC curve (AUC) represents the predictive ability of the nomogram model, with a value closer to 1 indicating higher accuracy. Generally, an AUC > 0.717 suggests a well-differentiated model. The predictive ability of the model is considered better if the prediction calibration curve is closer to the calibration curve.
Statistical Analysis
For data management, we established a database using Excel for double entry and verification. Statistical analysis was performed using SPSS 26.0 and R 4.1.3 software. Count data was expressed as frequency and percentage (%), and analyzed using the chi-square test or Fisher exact test. Mean ± standard deviation (Mean ± SD) was used for normally distributed measurement data, and group comparisons were made using the t-test. Non-normally distributed measurement data were described using M (P25, P75), and group comparisons were made using the non-parametric Mann–Whitney U-test. A stepwise variable screening method based on the AIC criteria was used for the multivariate logistic regression analysis, including variables with a significance level of P < 0.1 in the univariate analysis. All tests were two-sided, and a significance level of P < 0.05 was considered statistically significant. The nomogram was established using R 4.1.3 software, and ROC curve and calibration curve were plotted to evaluate the differentiation and consistency of the nomogram prediction model for predicting the risk of MDROs infection in neurosurgical intensive care units.
Results
General Data of the Study Subjects
Among the 2516 patients included in this study, 290 had MDROs infection, resulting in an incidence of 11.5%. In the training set (1761 patients), there were 203 cases of MDROs infection (11.5%), while in the validation set (755 patients), there were 87 cases (11.5%). There was no statistical difference between the training set and the validation set (P > 0.05). Refer to Table 1 for detailed information.
 |
Table 1 Descriptive Analysis of the Validation Set and Training Set Data |
Univariate Analysis of the Risk of Developing MDROs Infection in the Modeled Group
Regarding the occurrence of MDROs infection as the dependent variable, we conducted univariate analysis using patient demographic data, disease data, and laboratory-related examination indicators as independent variables. The results showed that sex, hospitalization time, febrile time, invasive operation, number of inpatient operations, number of days of antibiotic use after the first surgery, combination of antibiotics, mechanical ventilator time, central venous catheter indwelling time, urethral catheter indwelling time, FBG, ALB, PLT, Cr, WBC, N%, and L% were significant influencing factors for the occurrence of MDROs in the NICU (P < 0.05). Refer to Table 2 for detailed information.
 |
Table 2 Univariate Analysis of the Multidrug-Resistant Organisms Infection Group and Non-Multidrug-Resistant Organisms Infection Group in the Training Set |
Multivariate Analysis of the Risk of MDROs Infection in the Modeling Group
Based on the univariate analysis with a significance level of P < 0.1, we included the 15 variables (sex, hospitalization time, febrile time, invasive operation, postoperative prophylactic use of antibiotics, number of days of antibiotic use after the first surgery, combination of antibiotics, mechanical ventilator time, central venous catheter indwelling time, urethral catheter indwelling time, ALB, TBil, PLT, WBC, and L%). The analysis results demonstrate that sex, hospitalization time, febrile time, invasive operation, combination of antibiotics, mechanical ventilator time, central venous catheter indwelling time, urethral catheter indwelling time, ALB, PLT, WBC, and L% are independent influencing factors for the occurrence risk of MDROs in the NICU, as shown in Table 3.
 |
Table 3 Logistic Regression Analysis Results of Multidrug-Resistant Organisms Infection in a Neurosurgical Intensive Care Unit |
Predictive Model and Nomogram of the Risk of MDROs Infection in Neurosurgical Intensive Care Units
A risk prediction model was developed using independent variables representing risk factors for MDROs infection. A stepwise logistic regression equation based on AIC was constructed, and a visual nomogram was created (see Figure 1). The nomogram includes sex, hospitalization time, febrile time, invasive operation, combination of antibiotics, mechanical ventilator time, central venous catheter indwelling time, and urethral catheter indwelling time, as well as ALB, PLT, WBC, and L%. Each risk factor is assigned a corresponding score, and the total score indicates the probability of MDROs infection.
 |
Figure 1 Prediction nomogram model for multidrug-resistant organisms infection in a neurosurgical intensive care unit. |
Evaluation and Validation of the Nomogram Prediction Model
The training set of this model showed an area under the ROC curve of 0.880, with a sensitivity of 89.2% and a specificity of 73.4%. The validation set demonstrated an area under the ROC curve of 0.831, with a sensitivity of 74.7% and a specificity of 73.2% (see Figures 2–4).
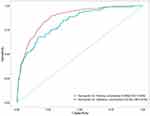 |
Figure 2 Receiver operating characteristic curves for the nomogram model. |
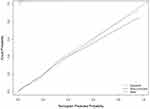 |
Figure 3 Calibration curves for the nomogram model in the training set. |
 |
Figure 4 Calibration curves for the nomogram model in the validation set. |
Discussion
The results of this study revealed that out of 2516 NICU inpatients, 290 cases had MDROs infection, resulting in an incidence rate of 11.5%. This rate is comparable to studies conducted in Australia18 and Ukraine,19 and slightly lower than the domestic data in China20 (20.6%). Possible reasons for this difference could be attributed to the healthcare technology in southeast China and the increasing attention given by hospital staff to the prevention of MDROs infection. It has been demonstrated that MDROs infection significantly impacts the treatment outcomes of NICU patients, prolongs hospital stays,9 and increases the case fatality rate.21,22 Therefore, it is of great clinical significance to identify the risk factors for MDROs infection in NICU wards and utilize quantitative indicators for personalized prediction of NICU inpatients.
This study utilized easily obtainable indicators including sex, hospitalization time, febrile time, invasive operation, combination of antibiotics, mechanical ventilator time, central venous catheter indwelling time, urethral catheter indwelling time, ALB, PLT, WBC, and L% to establish the nomogram for MDROs infection in the NICU ward. This visual presentation of the prediction model enables medical staff to calculate the risk of MDROs infection for individual patients based on their respective risk factors. The area under the ROC curve for the model was 0.880, and for the validation set it was 0.831, indicating a high ability of the model to identify the occurrence of MDROs infection in NICU patients. The calibration curve demonstrated that the model accurately predicted the probability of MDROs infection in NICU inpatients.
Interestingly, this study identified female gender as an independent risk factor for MDROs infection in NICU inpatients, which is consistent with the findings of Alnajjar MS23 et al and Gong L24 et al. However, studies by Li Wang6 et al and Carvalho-Brugger25 et al reported male sex as an independent risk factor for MDROs infection. This discrepancy may be attributed to differences in race and the range of diseases included in the studies, and it should be further investigated through prospective studies with larger sample sizes. In a descriptive observational study, Memon H26 et al found a significant association between the duration of fever and extensively drug-resistant infections in hospitalized children. Similarly, this study found that longer durations of fever in NICU patients were associated with a higher risk of MDROs infection. However, evidence regarding the association between fever duration and MDROs infection in adults is currently limited. The results of this study also demonstrated that longer hospital stays, combined antibiotic use, longer mechanical ventilator use, longer central venous catheterization, longer urinary catheterization, and lower ALB were associated with an increased risk of MDROs infection, which is consistent with numerous previous studies.27–31 Medical staff should pay close attention to patients with longer hospital stays, more invasive operations, and poor nutritional status in their clinical practice. Surprisingly, this study found that not undergoing surgery was a risk factor for MDROs infection in hospitalized NICU patients, which contradicts previous studies. This finding may be explained by the fact that unoperated patients in the NICU are often critically ill patients without surgical indications, such as those with brain hernia, who may be more susceptible to MDROs infection. Additionally, this study discovered for the first time that higher PLT, higher WBC, and lower L% may have some predictive value for MDROs infection, although these associations have been rarely reported thus far. We expect more research to focus on these points in the future.
Limitation of the Study
There are certain limitations to this study. The study subjects were recruited from a single center, and the nomogram prediction model was not validated in an external validation cohort.
Conclusion
This study identified female gender, longer hospitalization, longer fever, invasive operation, postoperative prophylactic use of antibiotics, longer mechanical ventilator use, longer central venous catheterization, longer catheter indwelling time, lower ALB, higher PLT, higher WBC, and lower L% as factors increasing the risk of MDROs infection in the NICU. The risk nomogram prediction model developed in this study aids clinical medical staff in efficiently identifying high-risk patients, providing personalized preventive measures, and demonstrating good differentiation and calibration. It holds promise for clinical application and implementation.
Abbreviations
MDROs, Multidrug-resistant microorganisms; NICU, Neurosurgery intensive care unit; SMOTE, Synthetic Minority Over-sampling Technique; ROC, Receiver operating characteristic curve; IIH, Intelligent & Integrated Healthcare; CLSI, Clinical and Laboratory Standards Institute; AIC, Akaike information criterion; FBG, Fasting blood glucose; ALB, Albumin; TBil, Total bilirubin; PLT, Platelet; Cr, Creatinine; WBC, White blood cell count; L%, Lymphocyte percentage; N%, Neutrophil percentage.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Statement
This study received approval from the Ethics Committee of the Affiliated Hospital of Nantong University (Code 2022-K011) and was conducted in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The clinical data of the patients were collected from their medical records and did not include any personal information such as names, addresses, or other identifying details. In this way, the data for this study has been anonymized and the privacy of all participants has been protected. Informed consent was waived by our hospital ethics committee because of the retrospective nature of our study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Social Livelihood Guiding Project of Nantong Science and Technology Bureau (MSZ2022075) and the Affiliated Hospital of Nantong University (Tfh 2109).
Disclosure
The authors declare no competing interests.
References
1. Cheng G, Wang D, Zhu P, et al. Clinical characteristics of acute pancreatitis patients with multidrug-resistant bacterial infection. Infect Drug Resist. 2022;15:1439–1447. doi:10.2147/IDR.S354347
2. Wang Y, Xiao Y, Yang Q, Wang F, Wang Y, Yuan C. Clinical prediction models for multidrug-resistant organism colonisation or infection in critically ill patients: a systematic review protocol. BMJ Open. 2022;12(9):e064566. doi:10.1136/bmjopen-2022-064566
3. Safdar N, Sengupta S, Musuuza JS, et al. Status of the Prevention of Multidrug-Resistant Organisms in International Settings: a Survey of the Society for Healthcare Epidemiology of America Research Network. Infect Control Hosp Epidemiol. 2017;38(1):53–60. doi:10.1017/ice.2016.242
4. Muller J, Voss A, Kock R, et al. Cross-border comparison of the Dutch and German guidelines on multidrug-resistant Gram-negative microorganisms. Antimicrob Resist Infect Control. 2015;4:7. doi:10.1186/s13756-015-0047-6
5. Al-Sunaidar KA, Aziz NA, Hassan Y, Jamshed S, Sekar M. Association of Multidrug Resistance Bacteria and Clinical Outcomes of Adult Patients with Sepsis in the Intensive Care Unit. Trop Med Infect Dis. 2022;7(11). doi:10.3390/tropicalmed7110365
6. Wang L, Huang X, Zhou J, et al. Predicting the occurrence of multidrug-resistant organism colonization or infection in ICU patients: development and validation of a novel multivariate prediction model. Antimicrob Resist Infect Control. 2020;9(1):66. doi:10.1186/s13756-020-00726-5
7. Ma X, Wu Y, Li L, et al. First multicenter study on multidrug resistant bacteria carriage in Chinese ICUs. BMC Infect Dis. 2015;15(1):358. doi:10.1186/s12879-015-1105-7
8. Chen YP, Tasi XW, Chang K, Cao XD, Chen JR, Liao CS. Multi-Drug Resistant Organisms Infection Impact on Patients Length of Stay in Respiratory Care Ward. Antibiotics. 2021;10(5). doi:10.3390/antibiotics10050608
9. Jia H, Li L, Li W, et al. Impact of Healthcare-Associated Infections on Length of Stay: a Study in 68 Hospitals in China. Biomed Res Int. 2019;2019:2590563. doi:10.1155/2019/2590563
10. Johnston KJ, Thorpe KE, Jacob JT, Murphy DJ. The incremental cost of infections associated with multidrug-resistant organisms in the inpatient hospital setting-A national estimate. Health Serv Res. 2019;54(4):782–792. doi:10.1111/1475-6773.13135
11. Kim CJ, Song KH, Choi NK, et al. Socioeconomic burden of pneumonia due to multidrug-resistant Acinetobacter baumannii and Pseudomonas aeruginosa in Korea. Sci Rep. 2022;12(1):13934. doi:10.1038/s41598-022-18189-6
12. Munier AL, Biard L, Legrand M, et al. Incidence, risk factors and outcome of multi-drug resistant Acinetobacter baumannii nosocomial infections during an outbreak in a burn unit. Int J Infect Dis. 2019;79:179–184. doi:10.1016/j.ijid.2018.11.371
13. Gocmez C, Celik F, Tekin R, et al. Evaluation of risk factors affecting hospital-acquired infections in the neurosurgery intensive care unit. Int J Neurosci. 2014;124(7):503–508. doi:10.3109/00207454.2013.863773
14. Lopez Pereira P, Diaz-Agero Perez C, Lopez Fresnena N, et al. ‘Epidemiology of surgical site infection in a neurosurgery department’. Br J Neurosurg. 2017;31(1):10–15. doi:10.1080/02688697.2016.1260687
15. Kolpa M, Walaszek M, Rozanska A, Wolak Z, Wojkowska-Mach J. Epidemiology of Surgical Site Infections and Non-Surgical Infections in Neurosurgical Polish Patients-Substantial Changes in 2003(-)2017. Int J Environ Res Public Health. 2019;16(6). doi:10.3390/ijerph16060911
16. Karhade AV, Cote DJ, Larsen AM, Smith TR. Neurosurgical Infection Rates and Risk Factors: a National Surgical Quality Improvement Program Analysis of 132,000 Patients, 2006-2014. World Neurosurg. 2017;97:205–212. doi:10.1016/j.wneu.2016.09.056
17. Yunjiao M, Haoye G, Xuan Q, et al. Establishment of a nomogram for predicting prolonged mechanical ventilation in cardiovascular surgery patients. Eur J Cardiovasc Nurs. 2022.
18. Cleland H, Tracy LM, Padiglione A, Stewardson AJ. Patterns of multidrug resistant organism acquisition in an adult specialist burns service: a retrospective review. Antimicrob Resist Infect Control. 2022;11(1):82. doi:10.1186/s13756-022-01123-w
19. Salmanov A, Shchehlov D, Svyrydiuk O, et al. Epidemiology of healthcare-associated infections and mechanisms of antimicrobial resistance of responsible pathogens in Ukraine: a multicentre study. J Hosp Infect. 2023;131:129–138. doi:10.1016/j.jhin.2022.10.007
20. Wang M, Wei H, Zhao Y, et al. Analysis of multidrug-resistant bacteria in 3223 patients with hospital-acquired infections (HAI) from a tertiary general hospital in China. Bosn J Basic Med Sci. 2019;19(1):86–93. doi:10.17305/bjbms.2018.3826
21. Johnston KJ, Thorpe KE, Jacob JT, Murphy DJ. The incremental cost of infections associated with multidrug-resistant organisms in the inpatient hospital setting-A national estimate. Health Serv Res. 2019;54(4):782–792.
22. Ellithy M, Mitwally H, Saad M, et al. Mortality incidence among critically ill burn patients infected with multidrug-resistant organisms: a retrospective cohort study. Scars Burn Heal. 2021;7:20595131211015133. doi:10.1177/20595131211015133
23. Alnajjar MS, Aldeyab MA, Scott MG, et al. Influence of primary care antibiotic prescribing on incidence rates of multidrug-resistant Gram-negative bacteria in hospitalised patients. Infection. 2019;47(5):781–791. doi:10.1007/s15010-019-01305-6
24. Gong L, Zhang L, Liu X, et al. Distribution and Antibiotic Susceptibility Pattern of Multidrug-Resistant Bacteria and Risk Factors Among Kidney Transplantation Recipients with Infections Over 13 Years: a Retrospective Study. Infect Drug Resist. 2021;14:5661–5669. doi:10.2147/IDR.S318941
25. Carvalho-Brugger S, Miralbes Torner M, Jimenez Jimenez G, et al. Preventive isolation criteria for the detection of multidrug-resistant bacteria in patients admitted to the Intensive Care Unit: a multicenter study within the Zero Resistance program. Med Intensiva. 2023. doi:10.1016/j.medine.2023.04.005
26. Memon H, Saeed F, Iqbal M, Saboohi E, Hanif S, Mallick AHH. Association of extensively drug resistant salmonella infection in children with typhoid fever. Pak J Med Sci. 2022;38(7):1864–1869. doi:10.12669/pjms.38.7.5868
27. Ang H, Sun X. Risk factors for multidrug-resistant Gram-negative bacteria infection in intensive care units: a meta-analysis. Int J Nurs Pract. 2018;24(4):e12644. doi:10.1111/ijn.12644
28. Li F, Zhang F, Wan X, et al. Infections in Acute Pancreatitis: organisms, Resistance-Patterns and Effect on Mortality. Dig Dis Sci. 2023;68(2):630–643. doi:10.1007/s10620-022-07793-1
29. Mader MM, Grensemann J, Kluge S, Westphal M, Czorlich P. Rate and impact of multidrug-resistant organisms in patients with aneurysmal subarachnoid hemorrhage. Acta Neurochir. 2018;160(10):2049–2054. doi:10.1007/s00701-018-3637-2
30. Zhou T, Yang W, Yang Q, et al. Distribution, diagnosis, and analysis of related risk factors of multidrug-resistant organism in patients with malignant neoplasms. Int J Clin Exp Pathol. 2020;13(10):2648–2655.
31. Han Y, Zhang J, Zhang HZ, Zhang XY, Wang YM. Multidrug-resistant organisms in intensive care units and logistic analysis of risk factors. World J Clin Cases. 2022;10(6):1795–1805. doi:10.12998/wjcc.v10.i6.1795
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
