Back to Journals » Clinical Epidemiology » Volume 10
Determinants of incident asthma–COPD overlap: a prospective study of 55,110 middle-aged adults
Authors Baarnes CB, Andersen ZJ , Tjønneland A , Ulrik CS
Received 5 March 2018
Accepted for publication 4 May 2018
Published 24 September 2018 Volume 2018:10 Pages 1275—1287
DOI https://doi.org/10.2147/CLEP.S167269
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Henrik Sørensen
Camilla Boslev Baarnes,1 Zorana Jovanovic Andersen,2 Anne Tjønneland,3 Charlotte Suppli Ulrik1,4
1Department of Pulmonary Medicine, Hvidovre Hospital, Hvidovre, Denmark; 2Center for Epidemiology and Screening, Department of Public Health, University of Copenhagen, Copenhagen, Denmark; 3Institute of Cancer Epidemiology, Danish Cancer Society, Copenhagen, Denmark; 4Institute of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Background and aim: Knowledge of the impact of social determinants driving asthma–chronic obstructive pulmonary disease overlap (ACO) is lacking. Our objective was to identify determinants of incident ACO.
Methods: A total of 55,053 adults (50–64 years) enrolled in the Danish Diet, Cancer, and Health cohort (1993–97) was followed in the National Patient Registry for admissions for asthma (DJ45–46) and chronic obstructive pulmonary disease (COPD; DJ40–44) and vital status. Incident ACO was defined as at least one hospital admission for both asthma and COPD (different time points, one after baseline). Detailed case history was obtained at baseline. Cox proportional hazards model was used to examine associations between possible determinants and incident ACO, in terms of hazard ratio (HR) and 95% confidence interval (CI).
Results: During follow-up, 561 incident cases of ACO were identified. Age (HR 4.4, 95% CI 3.3–5.9, age group 60–65 years), current smoking (HR 3.6, 95% CI 2.8–4.6), unemployment (HR 1.5, 95% CI 1.2–1.8), and being divorced (HR 1.5, 95% CI 1.2–1.9) determined a higher risk of incident ACO, whereas the opposite was found for leisure-time physical activity (HR 0.7, 95% CI 0.6–0.8) and high educational level (HR 0.7, 95% CI 0.5–0.9). In contrast to ACO, preexisting myocardial infarction (MI; HR 1.5, 95% CI 1.2–1.8) and stroke (HR 1.5, 95% CI 1.2–1.9) were associated with a higher risk of COPD.
Conclusion: Incident ACO is to a large extent determined by factors related to lifestyle and socioeconomic status.
Keywords: asthma–COPD overlap, socioeconomic status, lifestyle
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) have been regarded as distinct disease entities for decades. Asthma usually develops early in life and is characterized by episodes of reversible airflow limitation accompanied by typical respiratory symptoms, including wheeze,1 whereas COPD develops later in life and is characterized by persistent airflow limitation and excessive decline in lung function.2 Although classic asthma and COPD are easily distinguished, patients often present with overlapping features, especially among elderly patients as they may exhibit atypical symptoms and may also have altered perception of their symptoms, and in line with this, smoking history is not a clear-cut feature to distinguish asthma from COPD as a substantial proportion of patients with asthma are current or ex-smokers. Furthermore, the structural changes in the aging lung are associated with some degree of persistent airflow limitation, which may account for loss of bronchodilator reversibility in patients with underlying asthma and not COPD.3–5
To describe this coexistence of features of asthma and COPD, the term asthma–COPD overlap syndrome (ACOS) was introduced,6 which has been increasingly recognized in recent years’ literature.7–9 In line with this, the 2014 Global Initiative for Asthma–Global Initiative for Chronic Obstructive Lung Disease (GINA–GOLD) document suggests that patients with ACOS should be regarded as a subgroup of patients with obstructive lung diseases.10 However, more recently, the introduction of the widely accepted umbrella term asthma–COPD overlap (ACO) reflects that this coexistence of asthma and COPD features are unlikely to represent a single discrete disease entity.9
Previous studies have shown that individuals with ACO show more symptoms, worse quality of life, more frequent exacerbations, increased use of health care resources, more hospitalizations and a higher mortality compared to those who have asthma or COPD alone.8,9,11–13 However, further knowledge regarding the biology and pathophysiology of patients with ACO is clearly needed, also in relation to management strategy. In the very recently published American Thoracic Society/National Heart, Lung and Blood Institute Asthma–Chronic Obstructive Pulmonary Disease Overlap Workshop Report, it is stated that in future studies, it will be of outmost importance to address the effects of social determinants of health in driving asthma, COPD and ACO.9
The aim of this large population-based cohort study was to identify determinants of incident ACO compared to those of asthma and COPD alone.
Methods
Danish Diet, Cancer, and Health (DCH) cohort
We used the DCH cohort consisting of 57,053 individuals aged 50–64 years who were born in Denmark, lived in Copenhagen or Aarhus and were cancer free at baseline (1993–1997).14 All participants answered a detailed self-administered questionnaire on dietary habits, education, occupational history, lifestyle (smoking, physical activity, alcohol use), marital status, hormone replacement therapy (HRT) use, and preexisting conditions, including asthma, COPD, diabetes, myocardial infarction (MI), and stroke, and provided height and weight measurements. A detailed description of the DCH cohort has been published previously.14,15
Exposure definition
Tobacco exposure was calculated by equating a cigarette to 1 g, a cheroot or a pipe to 3 g, and a cigar to 5 g of tobacco and reported as daily tobacco consumption and years of smoking. Environmental tobacco smoke (ETS) was included as an indicator of exposure to second-hand smoke at home or work for minimum 4 hours/day. Occupational exposure relevant for chronic lung disease was defined as a minimum of 1 year’s employment in mining; in electroplating; in shoe or leather manufacturing; in welding; in painting; in steel mill or shipyard; in construction (roof, asphalt, or demolition); as a truck, bus, or taxi driver; in asbestos or cement manufacturing; in asbestos insulation; in glass, china, or pottery manufacturing; as a butcher; as a auto mechanic; as a waiter; or as a cook.
Definitions of health outcome
By using the unique identification number assigned to all Danish citizens (Danish Personal Identification Number),16 the DCH cohort was linked to the Danish National Patient Registry (DNPR)17,18 to prospectively extract hospital contacts from 1978 until July 1, 2013. DNPR includes all discharge diagnoses from all Danish hospitals since 1978 and from outpatient clinics since 1995.18 All registered hospital contacts were included in the present analyses: admissions, outpatient clinic visits, and emergency room visits. Unless otherwise specified, admission refers to all three types of contacts. COPD and asthma diagnoses were classified according to the International Classification of Diseases (ICD) as ICD-10 codes DJ40–44 (and 490.0–492.09 according to ICD-8 until 1994) and ICD-10 codes DJ45–46 (and ICD-8 codes 493.00–493.09), respectively, as ICD-9 was never implemented in Denmark. To allow for variations in classification procedures, patients with a primary diagnosis of DJ960 (acute respiratory failure) were also included, provided they had a secondary diagnosis of asthma or COPD. First hospital contacts after baseline (1993–1997) for asthma and/or COPD were classified as incident contacts.
Cohort participants were defined as having asthma if they, during the study period, exclusively had admissions for asthma, and the same was applicable for participants with COPD. Participants were defined as having ACO if they had at least one admission for asthma and at least one admission for COPD (at two different time points, regardless of which came first), as described previously.11 Participants were classified as having ACO at baseline if they had had at least one admission for asthma and also at least one admission for COPD before enrolment into the cohort. Incident ACO was thus defined as at least one first-time admission for either asthma or COPD occurring after baseline (1993–1997), with date of earliest admission as date of ACO onset. In line with this, participants classified as having asthma alone and COPD alone, respectively, were further divided into prevalent at baseline (first admission before 1993–1997) and incident (first admission after baseline). In the present analyses, only incident cases of ACO, asthma, and COPD were included (Figure 1).
Statistical analyses and ethics
We used Cox proportional hazards model with age as underlying time scale to examine the associations between a number of possible determinants of ACO: age, sex, active and passive smoking, occupational exposures, body mass index (BMI), leisure-time physical activity, fruit intake, education, employment status, civil status, and comorbidities (defined and listed in Tables 1–3) with ACO, asthma, and COPD, respectively, in three separate models. Follow-up started on the date of recruitment into the cohort (1993–1997) and ended at the date of first ACO, asthma, or COPD admission; date of death; date of emigration; or July 1, 2013, whichever came first. We evaluated the effect of each possible determinant in three steps: first, in a univariate model, adjusted for age (underlying time scale) (Model 1); second, in a fully adjusted model, with all variables included (Model 2); and in the final model, we included only variables that were statistically significantly associated with ACO, COPD, or asthma in the second model and performed a backward elimination (Model 3). We checked the proportional hazards assumption by testing for a nonzero slope in a generalized linear regression of the scaled Schoenfeld residuals on functions of time.19 Results are presented as hazard ratios (HRs) with 95% confidence intervals (CIs), estimated with stcox in Stata 11.2. The DCH cohort study was approved by the Central Danish Ethics Committee, and the present study was approved by the Danish Data Protection Agency (2014-41-3468). All participants in the DCH cohort provided written informed consent.
Results
Cohort
Of the 57,053 individuals enrolled in the cohort, we excluded 571 with cancer diagnoses before baseline, 70 with ACO before baseline, and 1,236 with missing information on covariates. The final cohort included in the present analysis, therefore, comprised 55,110 individuals.
Characteristics of participants with incident ACO
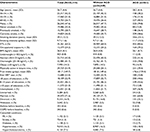
Among the 55,110 individuals without ACO at baseline, 561 (1.0%) of the cohort incident cases of ACO were observed during the mean follow-up period of 16 years, corresponding to 884,925 person-years, with an incidence rate of 63 cases per 100,000 person-years. At baseline, individuals classified as having ACO were less likely to be never smokers, physically active in leisure time, have ≥10 years of education, and to be married compared to the remaining cohort, whereas they were more likely to have cardiovascular comorbidity and to have been on postmenopausal HRT (Table 1).
Characteristics of participants with incident COPD
In analyses of incident COPD, we excluded 352 subjects with hospital admissions for COPD before baseline and 272 with missing information on covariates. Of the remaining 54,829 individuals without COPD at the baseline, 2,886 (5.3%) had a first-ever hospital admission for COPD during the mean follow-up period of 15.8 years or 868,424 person-years, corresponding to an incidence rate of 332 per 100,000 person-years. Among incident COPD cases, the majority (77.4%) were smokers at baseline (Table 2).
Characteristics of participants with incident asthma
In analyses of incident asthma, we excluded 363 persons with hospital admissions for asthma before baseline and 261 with missing information on covariates. Of the remaining 54,829 participants without asthma at the baseline, 785 (1.4%) were admitted to hospital for asthma for the first time during the mean follow-up period of 16 years or 875,333 person-years, corresponding to an incidence rate of 90 cases per 100,000 person-years. At baseline, more women with incident asthma reported use of HRT than participants without asthma (Table 3). A comparison of participants with incident ACO, COPD, and asthma is given in Table 4.
Determinants of incident ACO compared to asthma and COPD alone
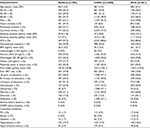
Details of the stepwise analysis of determinants of incident ACO during the observation period are given in Table 5. Age (HR 4.41, 95% CI 3.33–5.85, for age group 60–65 years compared to 50–55 years), current smoking (HR 3.59, 95% CI 2.81–4.59), ever use of HRT (women only; HR 1.37, 95% CI 1.11–1.70), unemployment (HR 1.48, 95% CI 1.23–1.79), and being divorced (HR 1.52, 95% CI 1.24–1.85) at baseline were associated with a statistically significant higher risk of ACO. On the other hand, physical activity in leisure time (HR 0.66, 95% CI 0.55–0.78) and high education (≥10 years; HR 0.67, 95% CI 0.51–0.87) were associated with a lower risk of ACO. No association was found between overweight or obesity, ETS, or comorbidity with MI, stroke, or diabetes at baseline and ACO. Notably, underweight was associated with an increased risk of ACO compared to overweight (HR 1.76, 95% CI 0.96–3.24), although statistically nonsignificant.
In contrast to ACO, preexisting MI (HR 1.48, 95% CI 1.23–1.80), stroke (HR 1.54, 95% CI 1.23–1.92), ETS (HR 1.21, 95% CI 1.15–1.23), and occupational exposure (HR 1.29, 95% CI 1.18–1.41) were associated with a higher risk of COPD (Table 6). Furthermore, in contrast to ACO and COPD, asthma risk was increased by obesity (HR 1.52, 95% CI 1.24–1.86) and high education level (≥10 years; HR 1.24, 95% CI 1.02–1.52; Table 7). Comparing incident ACO only to participants with at least two admissions for asthma or COPD, respectively, did not substantially change the observations. A more detailed description of determinants for incident ACO, COPD, and asthma is given in Table 8.
Discussion
This prospective study of a large population-based cohort of middle-aged adults revealed that incident asthma–COPD is to a large extent determined by factors related to lifestyle, including currently smoking, being unemployed, marital status, and leisure-time physical activity, and socioeconomic status, including level of education.
Characteristics of participants with ACO compared to asthma and COPD only
As might have been expected, the proportion of ever-smokers in the ACO group was found to be in between that of participants with asthma and COPD only, as has been shown in previous studies.20–22 The proportion of participants with ≥10 years of education was similar for participants with ACO and COPD (12.8% and 13.0%, respectively), whereas it was substantially higher for participants with asthma alone (21.3%). This confirms previous findings by Kumbhare et al21 of 17.7%, 18.8%, and 34.9%, respectively, graduating from college in the ACO, COPD-only, and asthma-only groups. On the other hand, Kim et al20 found a more distinct separation between the three groups, as 9.7%, 17.7% and 25.9% of participants had >12 years of education in the ACO, COPD, and asthma groups, respectively, whereas Sorino et al22 found no difference between the three groups with regard to years of education. Although the varying definitions of education make it difficult to compare studies, these differences may also be influenced by different sampling of cohorts and diagnostic criteria. In the study by Kim et al,20 a similar cut point was used for level of education, but the cohort investigated was much younger than in the present study comparable to the study by Kumbhare et al,21 whereas the cohort studied by Sorino et al22 was similar to ours. Kumbhare et al21 conducted a telephone survey and defined ACO as self-reported ever-diagnosed COPD and self-reported current asthma, whereas Kim et al20 performed a national survey of a representative selection of the population, measured lung function, and defined ACO as a FEV1/FVC ratio below lower limit of normal plus wheezing within the previous 12 months. On the other hand, Sorino et al22 performed a multicenter study of an elderly population, with several criteria for being classified as having ACO, based on lung function, bronchodilator reversibility, wheezing, and atopy. So, although not all reported findings are consistent, it seems highly likely that the characteristics of patients with ACO differ from those of patients with asthma and COPD alone.
Determinants of ACO
HRT has previously been shown to be a risk factor for incident asthma in postmenopausal women,15,23–25 and in keeping with that, the present study showed that HRT was associated with a higher risk of both incident asthma and ACO (HR 1.5 and 1.37, respectively). HRT was also associated with a higher risk of incident COPD (HR 1.24), possibly related to earlier menopause in female smokers, as also suggested by the large proportion of women with incident COPD on HRT at baseline (28.5%).
In keeping with other studies,21,26,27 participants with incident ACO had a higher prevalence of comorbidity at baseline than participants with asthma and COPD alone, although this difference did not reach statistical significance in the fully adjusted model. However, this association persisted in the fully adjusted model for participants with incident COPD (HR 1.17, 1.49, and 1.54 for hypertension, MI, and stroke, respectively) and taken together, suggesting that the prevalence and impact of comorbidity in ACO are primarily driven by the COPD component of the disease.
In line with our findings, de Marco et al12 have previously reported a lower relative risk ratio (RRR) for ACO for people with higher education completed. The same was found for COPD, while the association was inversed for asthma (RRR 0.30, 0.38, and 1.61 for ACO, COPD, and asthma, respectively), similar to the findings in the present study. In contrast, Ekerljung et al28 found no associating between length of education and either of the three groups of patients with obstructive lung disease in their adjusted analyses.
Our study revealed, to our knowledge not previously reported, that being divorced was a strong determinant of incident ACO (HR 1.52) and also a determinant of incident COPD (HR 1.28). Furthermore, being widowed was also associated with a higher risk of incident ACO (HR 1.53). The explanation for these findings related to marital status may be that it reflects social network and status, including not having someone at close hand to look out for you, eg, in relation to smoking cessation. In line with this, unemployment was also associated with a significant higher HR for ACO (HR 1.48) and also for COPD (HR 1.22), probably also reflecting socioeconomic status.
With regard to tobacco exposure, both current and former smokers had a higher HR for ACO (HR 3.59 and 2.23, respectively), and likewise, we found that current smokers had a higher HR for incident COPD, probably also primarily a marker of lower socioeconomic status.29 In a study published in 2013, de Marco et al12 found the RRR for smoking status to be higher for COPD (3.1 and 1.56, respectively, for current and former smokers) than for ACO (1.79 and 1.56, respectively), but, in contrast to our results, also a higher RRR for asthma (1.27). Ekerljung et al28 found the association between smoking and ACO to be statistically significant only for individuals with lifetime tobacco exposure of >20 pack-years (odds ratio [OR] 3.01) and found no difference in OR between ACO and COPD. Taken together, these findings therefore further support the notion that ACO is linked to markers of socioeconomic status.
Limitations
This being a register-based study means that we unfortunately had no access to information on change of risk behavior, including smoking habits, clinical findings, and information about prescribed medication and filled prescriptions, all factors that may have improved the characterization of the participants in our cohort. However, the attending physicians have had access to the individual disease manifestations, ie, symptoms, and clinical and para-clinical findings. The validity of discharge diagnoses in the DNPR has been assessed for both COPD30 and asthma,31 giving us confidence that the registered diagnoses are reliable.32 Another limitation of our study is that since we have only included patients with hospital contacts for asthma and/or COPD, we are likely to have excluded patients with milder diseases, as these are often diagnosed and followed solely by their general practitioner.
Conclusion and future perspectives
Our study has revealed that incident ACO is to a large extent determined by factors related to lifestyle and socioeconomic status, and by that, we have pinpointed areas that are likely to be important for assessing risk of ACO in individuals evaluated for possible obstructive airways disease. Furthermore, as lower socioeconomic status and less healthy lifestyle are likely to have negative impact on long-term outcome of obstructive airways diseases; our observations may also provide guidance to identify a vulnerable group of high-risk patients. Another important aspect of identifying patients with ACO is the ongoing debate of positioning of treatment with inhaled corticosteroid for COPD, as patients with an asthma component of their obstructive airways disease are likely to benefit substantially from anti-inflammatory therapy.
Acknowledgments
The abstract of this paper was presented at the annual meeting of the European Respiratory Society as a conference talk with interim findings. The abstract was published in the European Respiratory Journal 2017 (suppl. 61) OA 318.
Author contributions
CBB and CSU take overall responsibility for the content of the manuscript. ZJA had full access to all data in the study, analyzed the data, and takes responsibility for the accuracy of the data analysis. CBB wrote the first draft of the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Sideleva O, Suratt BT, Black KE, et al. Obesity and asthma: an inflammatory disease of adipose tissue not the airway. Am J Respir Crit Care Med. 2012;186(7):598–605. | ||
Telenga ED, Tideman SW, Kerstjens HA, et al. Obesity in asthma: more neutrophilic inflammation as a possible explanation for a reduced treatment response. Allergy. 2012;67(8):1060–1068. | ||
Battaglia S, Benfante A, Spatafora M, Scichilone N. Asthma in the elderly: a different disease? Breathe. 2016;12(1):18–28. | ||
Scichilone N, Pedone C, Battaglia S, Sorino C, Bellia V. Diagnosis and management of asthma in the elderly. Eur J Intern Med. 2014;25(4):336–342. | ||
Ulrik CS. Late-onset asthma: a diagnostic and management challenge. Drugs Aging. 2017;34(3):157–162. | ||
Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009;64(8):728–735. | ||
Baarnes CB, Kjeldgaard P, Nielsen M, Miravitlles M, Ulrik CS. Identifying possible asthma-COPD overlap syndrome in patients with a new diagnosis of COPD in primary care. NPJ Prim Care Respir Med. 2017;27:16084. | ||
Nielsen M, Bårnes CB, Ulrik CS. Clinical characteristics of the asthma-COPD overlap syndrome – a systematic review. Int J Chron Obstruct Pulmon Dis. 2015;10:1443–1454. | ||
Woodruff PG, van den Berge M, Boucher RC, et al. American Thoracic Society/National Heart, Lung, and Blood Institute Asthma-Chronic Obstructive Pulmonary Disease Overlap Workshop Report. Am J Respir Crit Care Med. 2017;196(3):375–381. | ||
Global Initiative for Chronic Obstructive Lung Diseases GIfA. Diagnosis of Diseases of Chronic Airflow Limitation: Asthma, COPD and Asthma-COPD Overlap Syndrome (ACOS). Available from: www.ginasthma.org. Accessed July 21, 2018. | ||
Baarnes CB, Andersen ZJ, Tjønneland A, Ulrik CS. Incidence and long-term outcome of severe asthma-COPD overlap compared to asthma and COPD alone: a 35-year prospective study of 57,053 middle-aged adults. Int J Chron Obstruct Pulmon Dis. 2017;12:571–579. | ||
de Marco R, Pesce G, Marcon A, et al. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One. 2013;8(5):e62985. | ||
Kauppi P, Kupiainen H, Lindqvist A, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011;48(3):279–285. | ||
Tjønneland A, Olsen A, Boll K, et al. Study design, exposure variables, and socioeconomic determinants of participation in diet, cancer and health: a population-based prospective cohort study of 57,053 men and women in Denmark. Scand J Public Health. 2007;35(4):432–441. | ||
Bønnelykke K, Raaschou-Nielsen O, Tjønneland A, Ulrik CS, Bisgaard H, Andersen ZJ. Postmenopausal hormone therapy and asthma-related hospital admission. J Allergy Clin Immunol. 2015;135(3):813–816. | ||
Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(7 suppl):22–25. | ||
Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 suppl):30–33. | ||
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. | ||
Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81(3):515–526. | ||
Kim J, Kim YS, Kim K, et al. Socioeconomic impact of asthma, chronic obstructive pulmonary disease and asthma-COPD overlap syndrome. J Thorac Dis. 2017;9(6):1547–1556. | ||
Kumbhare S, Pleasants R, Ohar JA, Strange C. Characteristics and prevalence of asthma/chronic obstructive pulmonary disease overlap in the United States. Ann Am Thorac Soc. 2016;13(6):803–810. | ||
Sorino C, Pedone C, Scichilone N. Fifteen-year mortality of patients with asthma-COPD overlap syndrome. Eur J Intern Med. 2016;34:72–77. | ||
Barr RG, Wentowski CC, Grodstein F, et al. Prospective study of postmenopausal hormone use and newly diagnosed asthma and chronic obstructive pulmonary disease. Arch Intern Med. 2004;164(4):379–386. | ||
Troisi RJ, Speizer FE, Willett WC, Trichopoulos D, Rosner B. Menopause, postmenopausal estrogen preparations, and the risk of adult-onset asthma. A prospective cohort study. Am J Respir Crit Care Med. 1995;152(4 pt 1):1183–1188. | ||
Lange P, Parner J, Prescott E, Ulrik CS, Vestbo J. Exogenous female sex steroid hormones and risk of asthma and asthma-like symptoms: a cross sectional study of the general population. Thorax. 2001;56(8):613–616. | ||
Hardin M, Cho M, Mcdonald ML, et al. The clinical and genetic features of COPD-asthma overlap syndrome. Eur Respir J. 2014;44(2):341–350. | ||
Rhee CK, Yoon HK, Yoo KH, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD. 2014;11(2):163–170. | ||
Ekerljung L, Mincheva R, Hagstad S, et al. Prevalence, clinical characteristics and morbidity of the Asthma-COPD overlap in a general population sample. J Asthma. 2018;55(5):461–469. | ||
Lange P, Marott JL, Vestbo J, Ingebrigtsen TS, Nordestgaard BG. Socioeconomic status and prognosis of COPD in Denmark. COPD. 2014;11(4):431–437. | ||
Thomsen RW, Lange P, Hellquist B, et al. Validity and underrecording of diagnosis of COPD in the Danish National Patient Registry. Respir Med. 2011;105(7):1063–1068. | ||
Jensen AØ, Nielsen GL, Ehrenstein V. Validity of asthma diagnoses in the Danish National Registry of Patients, including an assessment of impact of misclassification on risk estimates in an actual dataset. Clin Epidemiol. 2010;2:67–72. | ||
Dirksen A, Christensen H, Evald T, et al. Bronchodilator and corticosteroid reversibility in ambulatory patients with airways obstruction. Dan Med Bull. 1991;38(6):486–489. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.