Back to Journals » Journal of Multidisciplinary Healthcare » Volume 13
Determinants of Depressive Symptoms Among Rural Health Workers: An Application of Socio-Ecological Framework
Authors Bakhtari F, Sarbakhsh P , Daneshvar J, Bhalla D, Nadrian H
Received 25 March 2020
Accepted for publication 21 August 2020
Published 22 September 2020 Volume 2020:13 Pages 967—981
DOI https://doi.org/10.2147/JMDH.S255436
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Fatemeh Bakhtari,1 Parvin Sarbakhsh,2 Jalil Daneshvar,1 Devender Bhalla,3,4 Haidar Nadrian5
1Department of Health Education and Promotion, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran; 2Department of Statistics and Epidemiology, Faculty of Health, Tabriz University of Medical Sciences, Tabriz, Iran; 3Pôle Universitaire euclide Intergovernmental UN Treaty 49006/49007, Bangui, Central African Republic; 4Iranian Epilepsy Association, Tehran, Iran; 5Social Determinants of Health Research Center, Tabriz University of Medical Sciences, Tabriz, Iran
Correspondence: Haidar Nadrian Department of Health Education and Promotion, Faculty of Health
Tabriz University of Medical Sciences, Office No. 317, Attar-e-Neyshabouri St., Tabriz 6617777541, Iran
Email [email protected]
Objective: The objective of this study was to assess depressive symptoms among rural health workers (RHWs) through a multi-factorial socio-ecological framework (SEF) encompassing personal, interpersonal, organizational and community components.
Patients and Methods: A random sample of 394 RHWs in all rural areas of East Azerbaijan and fulfilling our other inclusion criteria were recruited. The participants underwent the Short-Form Beck’s Depression Inventory and a validated researcher-constructed SEF questionnaire, including subscales on personal, interpersonal, organizational and community factors associated with depressive symptoms. Internal consistency and factor structure parameters of the SEF were also calculated.
Results: A total of 394 RHWs were screened, of whom 170 (43.2%) had mild to major depressive symptoms. Only 6.8% were identified with major depressive symptoms. The SEF-based scale was found to have acceptable content validity (content validity index and ratio were 0.80 and 0.77, respectively) and reliability (Cronbach’s alpha=0.7). In the structural equation modeling, the fit indices showed our model to fit the data well (χ2=14.06, df=14, χ2/df=1.00, CFI=0.967, RMSEA=0.032). The highest direct contribution to depressive symptoms was found from the personal factors component (β=− 2.32). Also, “work load and roles interference” (from organizational level, β=− 0.76) and “family/colleague support” (from community level, β=− 1.28) made significant direct contributions towards depressive symptoms. Besides the SEF components, female gender (β=1.69), family history of mental illness (β=− 1.48), having chronic illnesses (β=− 1.64) and being religious (β=3.43) were the strongest direct contributors to depressive symptoms.
Conclusion: Depressive symptoms were common among RHWs, arising from all personal-, interpersonal-, organizational- and community-level factors. Our SEF had adequate internal consistency and factor structure parameters to be applied in the Middle East and North Africa (MENA) region countries, such as Iran, as a theoretical framework to plan for interventional efforts aiming at preventing depressive symptoms among RHWs. The burden of depressive symptoms should be reduced through multi-factorial interventions and rational perspectives.
Keywords: depression, rural healthcare, socio-ecological framework, rural health workers
Introduction
Depression is a public health concern and one of the most common psychiatric disorders.1,2 Depression is reported as the most important cause of disability and insufficiency, with decreased levels of willingness to work and take action as one of its major complications.3–5 Depressive symptoms are reported to be common among health and medical staff.3,6–9 Among depressed staff, absenteeism and job switching,10 as well as loss of productive time, are higher than in their non-depressed counterparts.11 The burden is far more severe among healthcare providers in settings in the Middle East and North Africa (MENA),4,6,7 where the overall frequency of depression is far higher3,12-14 than elsewhere.
About 45.0% of the population in the MENA region is rural. In such rural settings, rural healthcare workers (RHWs) are the primary healthcare workforce, who provide a broad multi-faceted service to the population they are closest to.15 In Iran, RHWs provide the rural populations with primary health care (PHC) and play a pivotal role in promoting the health of rural communities. Although they provide care to the other members of the public, they are not immune to poor mental health in general and mental health issues such as depressive symptoms in particular.3–5 For instance, about 70.0% of primary healthcare workers are likely to be affected by depressive symptoms.6 By being affected themselves, they may not provide adequate help to the patients,6,7 which also reflects negatively on the patients’ health.3,13
Depression cannot occur in isolation to one’s environmental factors.16,17 Thus, taking into account those factors that are innately related to home, immediate family, relatives, workplace, peers, co-workers, children’s school, neighbors, culture and the community in which RHWs live is essential. These factors cannot be posited together under personal variables17 as they, rather, represent a wide range of influences at multiple levels within what is known as a socio-ecological framework (SEF) (Figure 1). The World Health Organization (WHO) also agrees to a multi-directional complexity and dynamic interaction between a wide range of pathogenic and salutogenic factors under its bio-psycho-social model of health.3 Similarly, others have pointed out that individuals are “more than their mere illness”.18 In the present study, we assumed that a broad range of multilayered personal, cultural and environmental factors may be associated with depressive symptoms among RHWs. Therefore, in order to find a better understanding with a broader perspective on the various determinants of depressive symptoms, we decided to apply the SEF. This framework may advance the health promotion programs from focusing on changes on a behavioral or intrapersonal level to a broader range of changes in the social and environmental context related to behavior and health-related issues.19 In order to improve the health of populations, there is a need to investigate multiple levels of influence.20
 |
Figure 1 Socio-ecological framework. Note: Bronfenbrenner U,Toward an experimental ecology of human development, American Psychologist Association, 32, 7, 513, 1977, reprinted with permission from APA.77 |
Based on the SEF, health and behavior are the outcomes of interest,21 which are determined by the factors from personal and interpersonal levels to organizational, social and political levels.22 Personal-level factors are the characteristics of an individual, including knowledge, attitudes, self-concept and skills. Interpersonal factorsare social support systems and formal/informal social networks, including family, friendship and work group networks. Organizational-level factors are institutional characteristics associated with organizations and their formal/informal operation, rules and regulations, including financial policies and workplace climate (tolerance/intolerance). Community-level factors include the characteristics related to the location in the community, housing, culture, neighborhood associations, built environment, community leaders and transportation. Policy-level factors are local, national and/or international laws and policies that serve as a mediating structure to connect people and the larger social environment to make healthy choices, e.g. increased taxes on cigarettes and alcohol, and policies related to social injustice and global warming.23–25
The SEF has widely been used to approach different health problems.19,26-29 Worldwide, there are only partial uses of this framework in depression.30,31 Smokowski et al, applying a socio-ecological approach, investigated individual-, social- and school-level characteristics associated with depressive symptoms and self-esteem among a sample of US rural youth, and found that having a low income, being female, and having negative relationships with parents and peers were risk factors for higher levels of depressive symptoms.31 In another study, Olson and Goddard applied the SEF to determine the factors associated with depressive symptoms among US adolescents, and reported several protective factors that directly contributed to lower levels of depressive symptoms.32 As far as we are aware, no study has previously evaluated depression and depressive symptoms among RHWs in a non-Western context using a multi-dimensional SEF.20,22,27 Thus, with such a vision, we conducted a population-based assessment of depressive symptoms among those working as RHWs in East Azerbaijan, Iran, using the SEF. The following questions guided our study:
- What is the pattern of depressive symptoms among RHWs in Iran, as a developing country?
- What are the personal-, interpersonal-, organizational- and community-level factors contributing to depressive symptoms among RHWs?
- What are the direct and indirect contributions of the SEF-based factors towards depressive symptoms among RHWs?
- Could the SEF be used in a MENA region country, such as Iran, as a theoretical framework to plan for interventional efforts aiming at preventing depressive symptoms among RHWs?
Methods
Study Design and Participants
In this cross-sectional study, we aimed to determine the predictors of depressive symptoms among RHWs in East Azarbaijan province, Iran. In this developing country, healthcare services in rural areas are delivered by rural health care centers (RHCCs), which cover some health houses (HHs) in proportion to the population under their coverage. In this healthcare system, HHs are the first level of contact with rural and remote populations, and provide rural communities with a wide range of PHC services, e.g. maternal and child health, health education, family planning, disease surveillance and prevention, environmental health and healthy nutrition education. Depending on the geographical situations, population of the villages and communication facilities, one to three RHWs are employed in every HH.
In 2017, multi-stage random sampling was employed to recruit 394 RHWs. As the first step, the province was divided into four separate regions: north, south, east and west. Then, one county was randomly selected from each region (in total four counties were selected). In the third step, 300 HHs were again randomly selected from all four counties. In total, 421 RHWs were employed in the 300 HHs, within which 200 HHs had two RHWs and 21 HHs had only one RHW, as personnel. In the Iranian health system, only one or two RHWs are employed in each rural HH. Finally, all RHWs in the selected HHs were invited to participate in the study. The estimation of 10 samples per item was considered to determine sample size for applying structural equation modeling (SEM).33
As the number of items was 37 and considering an attrition rate of 10%, the sample size was estimated to be 407. Fourteen respondents declined to participate in the study (response rate = 96.6%). Also, the information for 13 respondents was not included in the analytical process, owing to missing data. Finally, the data on 394 RHWs were included in the data analysis. All respondents were invited to participate in the study; before providing them with the questionnaire, they were informed about the aim of study and assured on the confidentiality of data, and, finally, they all signed a consent form. The RHWs with more than 1 year of work experience in the current job, with no close relatives having died in the previous year and with no history of severe mental disorder in the family were included in the study. The RHWs who were being treated with anti-depression medications (as we presumed that the answers for such cases, because of medication, might bias the answers of all those who do not use any anti-depression drugs) and those who refused to complete the questionnaire were excluded from the study.
Measures
A researcher-constructed demographic and underlying data form with seven items was used to obtain data related to age, level of education, saying prayers (Yes/No), reading religious texts/words (the Quran, prayers and so on) (Yes/No), current smoking (smoking at least one cigarette per day) (Yes/No), history of childbirth during the previous 3 years (Yes/No) and being menopausal in the previous 3 years (for female RHWs only) (Yes/No). These last two questions were asked to identify those who may be at risk for postnatal depression and depression at menopause, respectively.
The Beck’s Depression Inventory – Short Form (BDI-13-SF)34 was used to measure the level of depressive symptoms among the respondents. The Persian version of this inventory is validated in Iran.35 BDI-13-SF is a 13-item standard self-report questionnaire used to classify the severity of depression symptoms in the following four categories: normal (0–4); mild depression (5–7); mild to moderate depression (8–15); and severe depression (16–39). The items are scored on a four-point basis from 0 to 3. The total score for the scale ranges from 0 to 39.
After a review of literature,36–40 a pool of factors associated with depressive symptoms at various workplaces was prepared. The research team selected the most relevant factors and then, by applying the socio-ecological approach, classified them into three levels: personal-, organizational- and community- level factors. The factors in the three levels were considered as the basis on which to develop the questionnaire.
Personal-Level Factors
To investigate the factors at the personal level, a researcher-constructed questionnaire including four items was developed. This questionnaire included “level of interest in job”, “level of satisfaction with job”, “ability to do things with current literacy” and “perception on the level of success in the field of work”. For all four items, a five-point Likert-type scale was used as the response format (none=1, low=2, moderate=3, high=4 and very high=5). The scores of respondents on the four items were summed to find a final score for the personal-level factors.
Organizational-Level Factors
Eight items were also developed to investigate the factors at the organizational level: having work load (two items), level of monitoring and evaluation (two items), reinforcing factors (two items) and satisfaction with the organization (two items). The scores of the respondents on the eight items were also summed to find a final score for the social-level factors. For all three levels, the items were rated on a five-point Likert-type scale ranging from 1 to 5 (1=none to 5=very high).
Community-Level Factors
Twelve items were developed to investigate the factors at the community level. This researcher-constructed scale included five subscales: relationships with colleagues, family and others (three items), perceived social support from colleagues, family and others (three items), perceived cultural and environmental barriers in the village (two items), facilities in the village (two items), and enjoyment from living and working in the village (two items). The scores of respondents on the 12 items were summed to find a final score for the community-level factors.
Content Validity
The content validity of the instrument was qualitatively assessed by an expert panel including 11 specialists in the fields of psychology, psychiatry, health education and promotion, and experts from a health worker training school. The responses from the expert panel were used to alter and/or modify the items. The content validity index (CVI) was measured. A CVI score higher than 0.75 was considered as acceptable.41 The content validity ratio (CVR) was also calculated. The scales with CVRs equal to or higher than 0.59 were considered to have good levels of content validity. The CVI and CVR for the scale were 0.85 and 0.77, respectively. In order to conduct a preliminary test on internal consistency, and to assess ambiguity and clarity, the scales were then pilot tested among 35 RHWs, who were not included in our final sample.
Reliability
The internal consistency reliability of the scale was approved after calculating Cronbach’s alpha in our pilot (α=0.66) and final (α=0.70) samples. Also, the Spearman–Brown coefficient was used to assess the stability of the scale over time in the final sample (r=0.72).
Ethical Approval
Ethical approval for this study was provided by the research committee in an Iranian Medical Sciences University (Ethic Code: IR.TBZMED.REC.1396.284).
Statistical Analysis
Data are presented as mean (standard deviation; SD) and frequency (percent) for quantitative and qualitative variables, respectively. In order to compare the demographic and underlying variables between the groups with and without depressive symptoms, the independent sample t-test and χ2-test were used.
Construct Validity
To assess the factor structure of the scale, exploratory factor analysis (EFA) was conducted, applying principal component factor analysis with varimax rotation, using the randomization function on SPSS version 22. The factor loadings greater than or equal to 0.3 were considered as appropriate, and eigenvalues above 1 were the bases for assigning the number of factors. The Kaiser–Meyer–Olkin (KMO) test and Bartlett’s test of sphericity were applied to determine the appropriateness of the sample.
Structural Equation Modeling
Considering the SEF approach and on the basis of the EFA results, the levels of factors influencing depressive symptoms were categorized into four levels: personal, interpersonal, organizational and community. SEM with identity link function and maximum likelihood estimation was applied to investigate the relationships between the variables, and the direct effects (dealing with the direct impact of an SEF factor on the dependent variable, depressive symptoms, when not mediated through a third factor) and indirect effects (the impact of an SEF factor on the dependent variable, depressive symptoms, mediated by a third factor) of the factors at different levels on the depression score. Stata software, version 14, was applied to test the fit of the determinant model of depressive symptoms to the data. As our aim was to determine the relationships between the socio-ecological factors at four levels and depressive symptoms based on SEF, all levels and depression were considered as observed variables and thus the SEM analysis was conducted as a path analysis. The path coefficients and correlations were reported as standardized estimates. Two primary tests were conducted to survey the data fit. The practical indicators of fit, according to confirmatory factor analysis, included chi-square, χ2/df, root mean square error of approximation (RMSEA) and comparative fit index (CFI).
The values for the CFI range from 0 to 1 and are derived from comparisons between a hypothesized model and the independent model; a value greater than 0.90 indicates an acceptable fit to the data. Conventionally, there is a good model fit if the RMSEA is less than or equal to 0.08 and the root mean square of the residuals (RMSR) is less than 0.05. There is also adequate fit if the RMSEA is less than or equal to 0.08 and the RMSR is less than 0.05.42 The level of significance was considered to be less than 0.05, a priori.
Results
Participants
A total of 394 RHWs were screened, of whom 170 subjects (43.5%) were found to have mild to major depressive symptoms. The socio-demographic details in association with depressive symptoms are provided in Table 1. The mean±SD age of participants was 40.86±6.53 years. Of those affected, 22.9% were men, although there was no statistically significant gender difference in the frequency of depressive symptoms (p=0.26) (Table 1).
 |
Table 1 Associations Between Demographic Characteristics and Depressive Symptoms Among Rural Health Workers |
Factor Structure
In the EFA, the KMO measure of sampling adequacy for the scale was 0.838 (approximate χ2=2647.13, df=276, p≤0.001). In the last iteration of EFA, seven distinctive factors were extracted as the best solution, which together explained about 59.7% of the total variance between the items. The list of factors loaded (subscales), their range and number of items, mean and standard deviation, floor and ceiling effects, as well as kurtosis and skewness of the factors, are shown in Table 2. Table 3 shows the rotated factor pattern coefficient for the seven-factor solution. The research team then compared this solution with the SEF model and found that it to matched the theoretical framework. Then, after a consultation with the initial panel of experts, the seven factors were categorized into the four levels of the SEF, namely personal, interpersonal, organizational and community levels (Table 4). In summary, the average alpha coefficient of our entire SEF was about 0.70, with different mean scores for each of its three components for different degrees of depressive symptoms (Table 4). Furthermore, the overall CVI and CVR for SEF items were 0.85 and 0.77, respectively. The Spearman–Brown coefficient, used to assess the stability of SEF over time, was estimated to be 0.72.
 |
Table 2 Characteristics of the Factors Derived from Exploratory Factor Analysis |
 |
Table 3 Rotated Factor Pattern Coefficients for Variable Solutions (24 Items) of the SEF Factors |
 |
Table 4 Socio-Ecological Framework (SEF) by Different Degrees of Depressive Symptoms Among Rural Health Workers |
Differences in the SEF Factors by Depressive Symptoms
Levels of difference in the SEF factors according to different degrees of depressive symptoms among RHWs are displayed in Table 4. Of all those affected (n=170), 15.8% were found to have major depressive symptoms (Table 4). Minor, moderate and major depressive symptoms were found in 16.4%, 19.7% and 6.8% of participants, respectively. Applying one-way ANOVA, significant differences were found in all seven domains of the factors (categorized in all four levels of SEF) with respect to depressive symptoms among RHWs. The only exception was for the “reinforcing factors”. The highest and the lowest scores were found to be for “interaction with villagers” at the interpersonal level (7.78 out of 10) among non-depressed RHWs and “reinforcing factors” at the organizational level (3.26 out of 10) among RHWs with major depressive symptoms, respectively. Also, Tukey’s HSD test showed that non-depressed RHWs had significantly greater mean (SD) scores in “personal factors”, “interaction with colleagues/monitoring and evaluation”, “culture and environment of village” and “family/colleague support” compared to the RHWs with moderate and severe levels of depressive symptoms. Non-depressed RHWs were also found to have higher mean scores on “work load and roles interference”, compared to those with low and moderate levels of depressive symptoms.
Structural Equation Modeling
The fit indices showed that our model fitted the data well (χ2=14.06, df=14, χ2/df=1.00, CFI=0.967, RMSEA=0.032). The highest direct contribution to depressive symptoms was found with the “personal factors” component (β=−2.32), which also made the highest total contribution towards depressive symptoms (β=−2.26). Among other factors of SEF, “work load and roles interference” (from the organizational level) and “family/colleague support” (from the community level) made both significant direct (“work load and roles interference”, β=−0.76; “family/colleague support”, β=−1.28) and total (“work load and roles interference”, β=−0.86; “family/colleague support”, β=−1.38) contributions towards depressive symptoms (Table 5 and Figure 2). In addition, we found that “belief in oneself as a religious man/woman” (β=3.43), family history of mental illness (β=−1.48), gender (β=1.69), educational level (β=−0.56), income status (β=−0.84) and having chronic illness (β=−1.64) directly contributed to depressive symptoms (Table 5 and Figure 2). The effects of personal, interpersonal, organizational and community components on depressive symptoms are displayed in Figure 2.
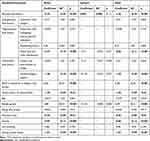 |
Table 5 Contributions (Direct, Indirect and Total) of Socio-Ecological Framework (SEF) to Depressive Symptoms Among Rural Health Workers |
 |
Figure 2 Standardized coefficients and relations of socio-ecological framework (SEF)-based factors with depressive symptoms among rural health workers in Iran. |
Discussion
The aim of this study was to investigate the factors associated with depressive symptoms among Iranian RHWs by applying the SEF of health in East Azerbaijan province, Iran. RHWs are at the bottom of the healthcare delivery system, and are more prone to poor mental health than other medical workers because of poorer remuneration, and fewer occupational, reward, relocation, professional support and training opportunities.43 RHWs also need to make frequent field visits without adequate transport facilities and are likely to be overburdened,4 which may affect their recreational and socializing opportunities as well as their family environment. As one example, the monthly wage of RHWs is merely one-sixth of that of other healthcare providers in Iran.44 Elsewhere in MENA, the compensation of similar health workers is likely to be far higher.45
Depressive symptoms were present in 43.2% of our subjects, and although this is an unacceptable number, major depressive symptoms were present in only 6.8% of our overall sample population and 15.8% of the affected subjects. A direct comparison with other studies is unsuitable given the possibility of methodological differences, but our overall frequency of depressive symptoms was lower than,46,47 similar to4 and higher than12 those reported by others. In two studies applying the BDI questionnaire, 10.9% of Brazilian intensive care nurses48 (n=91) and 10.5% of Swedish men in a primary care unit49 (n=223) had symptoms of depression. In another study among 2798 students using the same scale in India,50 depressive symptoms were reported among 40.2%, 38.5% and 47.2% of engineering, dentistry and medical students, respectively. The reason for such study-to-study disagreement may be related to the type of questionnaire, study setting, nature of participants and study design applied.4,12 For instance, the study that reported higher levels of depressive symptoms than ours recruited its participants from healthcare homes belonging to a single university and used a different questionnaire, i.e. the Patient Health Questionnaire (PHQ-9) for depression than ours. In a randomized trial,51 the BDI, which we used, was reported to have better psychometric properties and factor structure parameters than PHQ-9. Moreover, the BDI questionnaire provided a greater proportion of subjects with major depression than PHQ-9, which was true for us as well. Nevertheless, another study that was conducted among RHWs and used the same questionnaire as ours found nearly an identical frequency of depressive symptoms (43.4%),4 even though the sample size was considerably smaller than ours.
Our high level of depressive symptoms, and of major depression,14 reinforces that RHWs are possibly more prone to depressive symptoms than other medical workers, both in Iran7 and elsewhere.3,8 Their susceptibility to depressive symptoms should not be unexpected, given their inferior situation, regarding to their family, social and occupational life,52 for themselves and their spouse and children.13,53 For instance, the majority of RHWs (69%) reported that they are not interested in their job as an RHW. Moreover, the proportion of major depressive symptoms among RHWs was similar to that observed among truck drivers.54 This should also be not surprising, for many reasons. For instance, RHWs can change their place of residence but cannot change their place of work, placing them against the theory of locus of control, which is closely linked to the risk of depressive symptoms.55 Moreover, the relocated RHWs have to commute a certain distance daily, in addition to the field travel that they have to do as part of their usual work, often without adequate transportation facilities, which may lead to burnout.56 According to previous studies, 30–40% of healthcare workers may suffer from burnout.57–59
The topic of depression is fairly broad. Nevertheless, our SEF sought to be comprehensive by capturing the necessary risk-related information peculiar to the ecology of RHWs at various levels of influence (Figure 2). For instance, our SEF examined individual-level factors (e.g. gender and educational level) and personal-level factors (e.g. having the necessary skills to perform the tasks) that increase the likelihood of becoming a victim; interpersonal factors (e.g. interaction with villagers) that may increase the risk of experiencing depressive symptoms as a victim; organizational factors (e.g. work load and roles and interaction with colleagues) to identify the characteristics of these settings that are associated with becoming victims of depression; and broad community factors (e.g. culture and environment of village and family/colleague support) that provide a broad climate in which one may become a victim of depressive symptoms or remain protected. In addition, the SEF-based scale showed acceptable levels of content and construct validity, and our SEF had high fit indices and adequate alpha coefficients, which all imply that the seven components and their items fitted well for the assessment of depressive symptoms.
The highest direct contribution to depressive symptoms occurred from the personal-level factors, which should not be surprising because job satisfaction, job skills and capability are consistently associated with depressive symptoms.60–62 Furthermore, the lowest mean score among the components was found among the reinforcing factors, which shows that the RHWs’ organization has not worked well in providing them with encouraging mechanisms and recreational and welfare programs. This is unfortunate since such programs are associated with improved efficiency,61 reduced medical costs63 and depressive symptoms13 among the workers. One of the major organizational deficiencies with the job of an RHW is the wide range of responsibilities and also the high level of accountability to a wide range of health personnel from various levels of the healthcare system,12 which make them more vulnerable to depressive symptoms. Others have also pointed out that the lack of definition in RHWs’ roles and duties is an important factor for depressive symptoms.64
Similarly, the support of family/colleagues, from the community component, provided both direct and total contributions to depressive symptoms. These results are in line with the well-known effect of social factors on depression.65 Different studies have indicated the role of family and peer social support,28 emotional support66 and provision of social networks31 in preventing depressive symptoms. RHWs essentially have a rural living, which may expose them to circumstances, conditions and behaviors that challenge their health and may increase the prevalence of depressive symptoms among them. For instance, rural living is associated with severe depressive symptoms and poor mental health,64 possibly due to resource disparities that are common in rural areas.67 As one example, the place of residence and having public facilities, such as parks and transportation, have been reported to affect the outbreak of depressive symptoms.53
Similarly, work load and roles interference, as organizational factors, were equally contributory to depressive symptoms as some other components, but with no indirect contribution. The subjects had been working as RHWs for an average of 16 years, and depressive symptoms are known to be associated with length of employment.68 Thus, burnout may mediate depressive symptoms among vulnerable subjects. For instance, many RHWs may have additional duties such as child rearing.62 Furthermore, only a few percent (17%) of RHWs reported being interested in their job as an RHW. The job dissatisfaction may arise from a number of direct factors, such as poor compensation, the overburden of duties, the effect on other areas of life (e.g. family, social) and poor utilization of skills69–71 For instance, long daily commutes or overburden or shift duties may directly disturb people’s eating and cooking times; provide inadequate time for amusement, sexual fulfillment, affection and communication with their partner; reduce their participation in family affairs; increase the pressure to meet financial expenses from nagging spousal or children’s demands; or affect their resilience in general.
We found that the belief in oneself as a religious person was the strongest inverse contributor to the risk of depressive symptoms. Iman (i.e. faith/belief) is one of the ten fundamental qualities that is expected among Muslims in order for them to receive God’s mercy and help (Quran, verse 33:35) during predestined definite testing, “And We will surely test you with something of fear and hunger and a loss of wealth and lives and fruits, but give good tidings to the patient” (verse 2:155). In addition, the protective effect of religious beliefs can be easily understood through conventional theoretical models; for instance, the theory of hope:72 “So, verily, with every difficulty, there is relief: Verily, with every difficulty there is relief.” (Quran, 94:5–6). The association of such theoretical models with depression is well recognized, even among non-believers.73
In our study, the standardized direct contribution to depressive symptoms due to female gender was about 1.7 (Table 5). There was no indirect contribution of gender on depressive symptoms (Table 5), which may mean that any possible gender difference in the frequency (and the nature) of depressive symptoms is possibly biological, and not due to social or cultural factors.74 One simple example from our sample was that entering the menopause was significantly associated with depressive symptoms (Table 1). So, this supports our premise that time-bound biological changes (e.g. in ovarian hormones and hippocampal volume64,67) may be artificially reflected as a higher risk or frequency of depressive symptoms among females.74 Another supporting argument could be related to the presumed change in social attitude to promote supposed equality in the West and the semi-West; yet, there has been no clear change in terms of a reduction in the female:male depression ratio.14 The WHO reports also support that there is no difference in the prevalence of depressive symptoms between males and females.22 Moreover, besides the above reasons, there are many other counter-explanations that must be overcome before a female risk differential could be reliably accepted. For instance, since females have two identical copies of the X chromosome, they are likely to be better protected.75
Lastly, we recruited our subjects from all rural areas of the selected counties. Moreover, as far as we are aware, this was the first study to examine the simultaneous contribution of multi-level factors for depressive symptoms among RHWs. However, our study has similar limitations to other published studies of comparable study design. The SEF can be fairly extensive and so is the risk of depressive symptoms, and, therefore, it was not feasible for us to cover many factorial contexts (e.g. genetic, political, biological, psychoneurotic) without overburdening our participants. As an example, the target population in our study was RHWs, who unequivocally were in direct contact with the recipients of their service. A previous study has shown that emotional labor may also lead to emotional burnout, which further increases the risk for depressive symptoms.76
Conclusion
Depressive symptoms were common among RHWs, arising from all personal-, interpersonal-, organizational- and community-level factors, which reinforces that RHWs are possibly more prone to depressive symptoms than other medical workers, both in Iran and elsewhere. In addition, our SEF had adequate internal consistency and factor structure parameters to be applied in countries in the MENA region, like Iran, as a theoretical framework to plan for interventional efforts aiming at preventing depressive symptoms among RHWs. Given these results, we are confident in suggesting that the burden of depressive symptoms can only be reduced through multi-factorial interventions and rational perspectives. We believe that our work could facilitate a better understanding of the determinants that underlie depressive symptoms, and, therefore, better interventional efforts to reduce the ever-growing burden of depressive symptoms among the at-risk subjects. RHWs are critical stakeholders in rural healthcare, so their health and welfare should be as high a priority as the health and welfare of the general public.
Ethical Approval and Consent to Participate
Ethical approval for the study was received from the Ethics Committee in Research Affairs, Tabriz University of Medical Sciences. All respondents were informed about the aim of study and assured about the confidentiality of the data, and all signed a consent form.
Acknowledgments
We thank all the rural health workers who participated in our study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no potential competing interests for this work.
References
1. Lakhan R, Ekúndayò OT. Application of the ecological framework in depression: an approach whose time has come. AP J Psychol Med. 2013;14:103–109.
2. WHO. Depression and Other Common Mental Disorders: Global Health Estimates; 2017.
3. Letvak S, Ruhm CJ, McCoy T. Depression in hospital-employed nurses. Clin Nurse Specialist. 2012;26:177–182.
4. Dehghan A, Ghavami L, Ghahramani F, Bazrafshan MR, Namavar S. Prevalence of depression and its relation with their performance in larestan rural health workers in 2010. J Rafsanjan Univ Med Sci. 2012;11:79–84.
5. Fushimi M. Prevalence of depressive symptoms and related factors in Japanese employees: a comparative study between surveys from 2007 and 2010. Psychiatry J. 2015;2015:1–7. doi:10.1155/2015/537073
6. Alkhazrajy L, Sabah S, Abed SMH. Prevalence of depressive symptoms among primary health care providers in Baghdad. Int J Health Psychol Res. 2014;2:1–20.
7. Ardekani Z, Kakooei H, Ayattollahi SM, Choobineh A, Seraji GN. Prevalence of mental disorders among shift work hospital nurses in Shiraz, Iran. Pak J Biol Sci. 2008;11(12):1605–1609. doi:10.3923/pjbs.2008.1605.1609
8. Martin F, Poyen D, Bouderlique E, et al. Depression and burnout in hospital health care professionals. Int J Occup Environ Health. 1997;3:204–209. doi:10.1179/oeh.1997.3.3.204
9. Obi IE, Aniebue PN, Okonkwo KO, Okeke TA, Ugwunna NC. Prevalence of depression among health workers in Enugu, South East Nigeria. Niger J Clin Pract. 2015;18:342–347. doi:10.4103/1119-3077.151726
10. Kessler R, Barber C, Birnbaum HG, et al. Depression in the workplace: effects on short-term disability. Health Aff. 1999;18:163–171. doi:10.1377/hlthaff.18.5.163
11. Adler D, McLaughlin TJ, Rogers WH, Chang H, Lapitsky L, Lerner D. Job performance deficits due to depression. Am J Psychiatry. 2006;163(9):1569–1576. doi:10.1176/ajp.2006.163.9.1569
12. Ansaripour S, Hasanzadeh A, Gramian N, Akhavan S, Moghadas T. The prevalence of depression and its impact on health workers’ performance in Isfahan University of Medical Sciences, Iran, 2013. J Isfahan Med School. 2016;33:1884–1890.
13. Costello CG. Depression: loss of reinforcers or loss of reinforcer effectiveness? – republished article. Behav Ther. 2016;47(5):595–599. doi:10.1016/j.beth.2016.08.007
14. Dehghani M, Zoladl M, Boland-Parvaz S, Keshtkaran Z, Mahmoudi R, Jabbarnejad A. A survey on depression and its related factors in nurses who work in Namazi Hospital of Shiraz University of medical sciences-2008. Iran Occup Health. 2009;6:29–34.
15. Maharaj SLT, Lees S, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int J Environ Res Public Health. 2018;16(1):61. doi:10.3390/ijerph16010061
16. Shibata AOK, Harada K, Nakamura Y, Muraoka I. Psychological, social, and environmental factors to meeting physical activity recommendations among Japanese adults. Int J Behav Nutr Phys Act. 2009;6:1–12.
17. Ishii KSA, Shibata K, Oka K. Environmental, psychological, and social influences on physical activity among Japanese adults: structural equation modeling analysis. Int J Behav Nutr Phys Act. 2010;7(1):61. doi:10.1186/1479-5868-7-61
18. Reupert A, Maybery D, Cox M, Scott Stokes E. Place of family in recovery models for those with a mental illness. Int J Ment Health Nurs. 2015;24:495–506. doi:10.1111/inm.12146
19. Robinson T. Applying the socio-ecological model to improving fruit and vegetable intake among low-income African Americans. J Community Health. 2008;33(6):395–406. doi:10.1007/s10900-008-9109-5
20. Sallis JF, Owen N, Fisher E. Ecological models of health behavior. Health Behav. 2015;5:43–64.
21. Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. John Wiley & Sons; 2008.
22. Krug E, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. 2002;360(9339):1083–1088. doi:10.1016/S0140-6736(02)11133-0
23. McLaren L, Hawe P. Ecological perspectives in health research. J Epidemiol Community Health. 2005;59:6–14. doi:10.1136/jech.2003.018044
24. Stokols D. Establishing and maintaining healthy environments: toward a social ecology of health promotion. Am Psychol. 1992;47:6. doi:10.1037/0003-066X.47.1.6
25. McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi:10.1177/109019818801500401
26. Aghdam FBMM, Jafarabadi MA, Allahverdipour H, Nikookheslat SD, Nourizadeh R. Explaining the role of personal, social and physical environment factors on employed women’s physical activity: a structural equation analysis. Glob J Health Sci. 2013;5:189.
27. Bakhtari F, Nadrian H, Matlabi H, Sarbakhsh P, Bidar M. Personal, interpersonal, and organizational predictors of the mode of delivery among urban women: a prospective study with socio-ecological approach. Clin Nurs Res. 2017;1054773817740530.
28. Sameroff AJPS, editors. Contrasting ecological models for adolescent mental health, problem behavior, and academic achievement.
29. Schueller SM, Aguilera A, Mohr DC. Ecological momentary interventions for depression and anxiety. Depress Anxiety. 2017;34:540–545. doi:10.1002/da.22649
30. Poleshuck E, Perez-Diaz W, Wittink M, et al. Resilience in the midst of chaos: socioecological model applied to women with depressive symptoms and socioeconomic disadvantage. J Community Psychol. 2019;47:1000–1013. doi:10.2/jcop.22188
31. Smokowski PR, Evans CB, Cotter KL, Guo S. Ecological correlates of depression and self-esteem in rural youth. Child Psychiatry Hum Dev. 2014;45:500–518. doi:10.1007/s10578-013-0420-8
32. Olson J, Goddard HW. An ecological risk/protective factor approach to understanding depressive symptoms in adolescents. J Ext. 2010;48:1–10.
33. MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. 1996;1:130. doi:10.1037/1082-989X.1.2.130
34. Beck AT, Beck RW. Screening depressed patients in family practice: a rapid technic. Postgrad Med. 1972;52:81–85. doi:10.1080/00325481.1972.11713319
35. Dadfar M, Kalibatseva Z. Psychometric properties of the persian version of the short beck depression inventory with Iranian psychiatric outpatients. Scientifica (Cairo). 2016;2016:8196463.
36. Costello C. Social factors associated with depression: a retrospective community study. Psychol Med. 1982;12(2):329–339. doi:10.1017/S0033291700046663
37. Ngin CPK, Tuot S, Chhoun P, Yi R, Yi S. Social and behavioural factors associated with depressive symptoms among university students in Cambodia: a cross-sectional study. BMJ Open. 2018;8:e019918. doi:10.1136/bmjopen-2017-
38. Madsen IEH, Nyberg ST, Magnusson Hanson LL, et al.; IPD-Work Consortium. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med. 2017;47(8):1342–1356. doi:10.1017/S003329171600355X.
39. Bernburg MVK, Vitzthum K, Groneberg DA, Mache S. Physicians‘ occupational stress, depressive symptoms and work ability in relation to their working environment: a cross-sectional study of differences among medical residents with various specialties working in German hospitals. BMJ Open. 2016;6(6):e011369. doi:10.1136/bmjopen-2016-011369
40. Theorell THA, Hammarström A, Aronsson G, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health. 2015;15(1):738. doi:10.1186/s12889-015-1954-4
41. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–575. doi:10.1111/j.1744-6570.1975.tb01393.x
42. Kline R. Principles and Practice of Structural Equation Modeling. Vol. 2. New York: Guilford Press; 2004.
43. Liu J, Zhu B, Wu J, Mao Y. Job satisfaction, work stress, and turnover intentions among rural health workers: a cross-sectional study in 11 western provinces of China. BMC Fam Pract. 2019;20(1):9. doi:10.1186/s12875-019-0904-0
44. Chowdhury Z, Javadi D. Iran’s community health worker program; 2014 [cited March 17, 2020]. Available from: http://www.chwcentral.org/blog/iran’s-community-health-worker-program.
45. Indeed. Healthcare assistant salaries in the United Arab emirates; 2020 [cited March 17, 2020]. Available from: https://www.indeed.ae/salaries/healthcare-assistant-Salaries.
46. Nabipour A, Gholami H, Amini A, Riahi SM, Ghanbarifar S, Zirak MH. Prevalence of depression and its related factors in Pishva District health network employees in 2013. 2015.
47. Fallah RFS, Amini K, Mohajeri M. Prevalence of depression in personnel of Zanjan University of medical sciences. ZUMS J. 2011;19:107–113.
48. Vasconcelos EMD, Martino MMFD, França SPDS. Burnout and depressive symptoms in intensive care nurses: relationship analysis. Rev Bras Enferm. 2018;71(1):135–141. doi:10.1590/0034-7167-2016-0019
49. Strömberg R, Backlund LG, Löfvander M. A comparison between the Beck’s Depression Inventory and the Gotland Male Depression Scale in detecting depression among men visiting a drop-in clinic in primary care. Nord J Psychiatry. 2010;64(4):258–264. doi:10.3109/08039480903511407
50. Nezam S, Golwara AK, Jha PC, Khan SA, Singh S, Tanwar AS. Comparison of prevalence of depression among medical, dental, and engineering students in Patna using beck’s depression inventory II: a cross-sectional study. J Family Med Prim Care. 2020;9(6):3005. doi:10.4103/jfmpc.jfmpc_294_20
51. Titov N, Dear BF, McMillan D, Anderson T, Zou J, Sunderland M. Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cogn Behav Ther. 2011;40(2):126–136. doi:10.1080/16506073.2010.550059
52. World Bank. Exploring Factors Driving the Performance of Rural Health Care in Papua New Guinea (English). Washington, DC: World Bank; 2018. Available from: http://documents.worldbank.org/curated/en/611831528823049450/Exploring-factors-driving-the-performance-of-rural-health-care-in-Papua-New-Guinea.
53. Weich SBM, Prince M, Burton E, Erens B, Sproston K. Mental health and the built environment: cross-sectional survey of individual and contextual risk factors for depression. Br J Psychiatry. 2002;180:428–433. doi:10.1192/bjp.180.5.428
54. Vakili MEFS, Hossein SMH, Dehghani Tafti MH. Prevalence of depression and its related factors among truck drivers in Yazd Province −2008. Iran Occup Health J. 2010;6:69–76.
55. Khumalo T, Plattner I. The relationship between locus of control and depression: a cross-sectional survey with university students in Botswana. S Afr J Psychiatr. 2019;25:1221. doi:10.4102/sajpsychiatry.v25i0.1221
56. Xu W, Pan Z, Li Z, Lu S, Zhang L. Job burnout among primary healthcare workers in rural China: a multilevel analysis. Int J Environ Res Public Health. 2020;17(3):727. doi:10.3390/ijerph17030727
57. Gómez-Urquiza JLD-SE, Albendín-García L, Vargas-Pecino C, Ortega-Campos EM, Cañadas-de la Fuente GA. Prevalence of burnout syndrome in emergency nurses: a meta-analysis. Crit Care Nurse. 2017;37:e1–e9. doi:10.4037/ccn2017508
58. Soler JKYH, Esteva M, Dobbs F, et al. Burnout in European family doctors: the EGPRN study. Fam Pract. 2008;25:245–265. doi:10.1093/fampra/cmn038
59. Blanchard PTD, Albiges-Sauvin L, Dewas S, et al. Prevalence and causes of burnout amongst oncology residents: a comprehensive nationwide cross-sectional study. Eur J Cancer. 2010;46:2708. doi:10.1016/j.ejca.2010.05.014
60. Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med. 2005;62:105–112. doi:10.1136/oem.2002.006734
61. Howarth A, Quesada J, Mills PR. A global, cross cultural study examining the relationship between employee health risk status and work performance metrics. Ann Occup Environ Med. 2017;29:17. doi:10.1186/s40557-017-0172-1
62. O’Donnell LA, Deldin PJ, Grogan-Kaylor A, et al. Depression and executive functioning deficits predict poor occupational functioning in a large longitudinal sample with bipolar disorder. J Affect Disord. 2017;215:135–142. doi:10.1016/j.jad.2017.03.015
63. Aldana SG, Merrill RM, Price K, Hardy A, Hager R. Financial impact of a comprehensive multisite workplace health promotion program. Prev Med. 2005;40:131–137. doi:10.1016/j.ypmed.2004.05.008
64. Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–138. doi:10.1146/annurev-publhealth-031912-114409
65. Grav S, Hellzèn O, Romild U, Stordal E. Association between social support and depression in the general population: the HUNT study, a cross‐sectional survey. J Clin Nurs. 2012;21:111–120. doi:10.1111/j.1365-2702.2011.03868.x
66. Santini ZI, Koyanagi A, Tyrovolas S, Mason C, Haro JM. The association between social relationships and depression: a systematic review. J Affect Disord. 2015;175:53–65. doi:10.1016/j.jad.2014.12.049
67. Sakuraya A, Imamura K, Inoue A, et al. Workplace social capital and the onset of major depressive episode among workers in Japan: a 3-year prospective cohort study. J Epidemiol Community Health. 2017;71:606–612. doi:10.1136/jech-2016-208561
68. DeSanto IJ, Cullen M, Cantley L, Slade M, Fiellin M, Kasl S. Effects of externally rated job demand and control on depression diagnosis claims in an industrial cohort. Am J Epidemiol. 2010;171:303–311. doi:10.1093/aje/kwp359
69. Jayasuriya R, Whittaker M, Halim G, Matineau T. Rural health workers and their work environment: the role of inter-personal factors on job satisfaction of nurses in rural Papua New Guinea. BMC Health Serv Res. 2012;12(1):156. doi:10.1186/1472-6963-12-156
70. Jin Y, Wang H, Wang D, Yuan B. Job satisfaction of the primary healthcare providers with expanded roles in the context of health service integration in rural China: a cross-sectional mixed methods study. Hum Resour Health. 2019;17(1):70. doi:10.1186/s12960-019-0403-3
71. Kebriaei A, Moteghedi M. Job satisfaction among community health workers in Zahedan District, Islamic Republic of Iran. East Mediterr Health J. 2009;15(5):1156–1163. doi:10.26719/2009.15.5.1156
72. Leite A, de Medeiros A, Rolim C, et al. Hope theory and its relation to depression: a systematic review. Ann Psychiatr Clin Neurosci. 2019;2:1014.
73. The Guardian. Non-believers turn to prayer in a crisis, poll finds; 2020 [cited March 18, 2020]. Available from: https://www.theguardian.com/world/2018/jan/14/half-of-non-believers-pray-says-poll.
74. Albert P. Why is depression more prevalent in women? J Psychiatry Neurosci. 2015;40(4):219–221. doi:10.1503/jpn.150205
75. Dunford A, Weinstock D, Savova V, et al. Tumor-suppressor genes that escape from X-inactivation contribute to cancer sex bias. Nat Genet. 2017;49:10–16. doi:10.38/ng.3726
76. Jeung D, Kim C, Chang S. Emotional labor and burnout: a review of the literature. Yonsei Med J. 2018;59(2):187–193. doi:10.3349/ymj.2018.59.2.187
77. Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513. doi:10.1037/0003-066X.32.7.513
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
