Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 14
Descriptive Analysis of Rheumatic Heart Disease Related Complications in Pediatric Patients at Tertiary Hospital, Addis Ababa, Ethiopia
Authors Desta TT , Gezachew A, Eshetu K
Received 9 November 2022
Accepted for publication 31 January 2023
Published 11 February 2023 Volume 2023:14 Pages 45—57
DOI https://doi.org/10.2147/PHMT.S396854
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Temesgen Tsega Desta,1 Alem Gezachew,1 Konjit Eshetu2
1Department of Pediatrics and Child Health, Saint Paul Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2Department of Pediatrics and Child Health, Haramaya University College of Health and Medical Sciences, Harar, Ethiopia
Correspondence: Temesgen Tsega Desta, Email [email protected]
Introduction: Rheumatic heart disease continues to be a public health problem worldwide. In developing countries such as Ethiopia where rheumatic heart disease is endemic, most of the patients present with complaints related to complications including heart failure, arrhythmias, pulmonary hypertension, stroke, systemic embolic events and infective endocarditis.
Objective: To identify the types and magnitude of complications in pediatric patients with rheumatic heart disease.
Methodology: Hospital-based cross-sectional study was conducted at Saint Paul Hospital Millennium Medical College, pediatric and child health department. All pediatric cardiac patients with rheumatic heart disease seen from January 1, 2018 to December 30, 2021 were included in the study.
Conclusion: The majority of patients presented to our health facility with complications which implies the need for action at the community level to detect the disease at early stage.
Recommendations: We recommend a similar large-scale study to be conducted at the national level and introduce a national RHD registry to better understand the magnitude of the problem, based on which necessary action will be undertaken. There is also a need to assess the proper implementation of screening and preventive RHD programmes.
Keywords: rheumatic heart disease, heart failure, pulmonary hypertension and malnutrition
Introduction
Background
Rheumatic heart disease (RHD) continues to be a public health problem worldwide, with estimates of nearly 300,000 deaths globally and more than 10 million disability-adjusted life-years. Most of these cases occur in low- and middle-income countries (LMICs) while it has significantly declined in developed countries. In those areas with resource limitations various obstacles exist in implementation of RHD prevention strategies and also in the provision of standard medical and surgical management for affected patients.1–3
In countries where RHD is endemic, identification of subclinical RHD cases in school-aged children between the age of 5 and 15 years by performing echocardiographic screening will enable early detection of cases. Most of such asymptomatic cases are likely to be at a milder stage where secondary prophylaxis implementation will have a significant impact in aborting the disease progress. Echocardiography-based screening showed the pooled prevalence of subclinical RHD was about 7 times higher than that of clinically overt disease.4–6
Despite recommendations for echocardiography-based screening for RHD by the World Heart Federation, it is not practiced yet in many resource-limited countries and most of the patients with RHD arrive at the medical facilities once they are symptomatic and severe disease has occurred with complications related to RHD, which include heart failure, arrhythmias, pulmonary hypertension, stroke, systemic embolic events and infective endocarditis.7,8
Statement of the Problem
Because there is no national registry that WHO recommends as a vital adjunct for prevention and control of RHD, there is a paucity of data on community prevalence of RHD in much of sub-Saharan Africa. A multisite national echocardiography-based screening program across Ethiopia done by Yadeta D, Haileamlak A, Hailu A et al showed that among schoolchildren the prevalence of RHD is 19 per 1000. In a recent community-based prevalence study from south-western Ethiopia, it was reported that the prevalence of RHD was 37.5 per thousand people and this rate is almost 10-fold higher than the prevalence of RHD in schoolchildren from a rural town (Butajira) that was reported nearly 25 years ago.9–12
Pediatric data are scarce in Ethiopia regarding complications pertaining to rheumatic heart disease, mortality rate and main cause of death in such patients. Most of the studies are in the adult population and even among them we could not find a study with a special emphasis on RHD patients to point out related complications. A retrospective study from Ethiopia in adults regarding the contribution of RHD to all cardiovascular-related deaths reported that 26.5% of deaths were due to RHD, and in 70% of these patients, the deaths were attributable to heart failure.13
Significance of the Study
Despite the high prevalence of the disease in Ethiopia there are not sufficient data (specific to pediatric patients with RHD) to give a detailed description regarding complications (such as heart failure, pulmonary hypertension, infective endocarditis, etc.) and risk factors which contribute to these. This research should provide information about the extent of complications occurring in pediatric patients with RHD and will enable the health professionals and policymakers to formulate strategies towards avoiding the occurrence of these anticipated complications depending on the magnitude and severity of occurrence.
Objective
General Objective
To determine the magnitude of complications related to RHD in pediatric patients treated at Saint Paul Hospital Millennium Medical College, Addis Ababa, Ethiopia.
Specific Objective
To identify the type of complications seen in those children with RHD.
To sort out associated factors which contributed for occurrence of these complications.
Methodology
Study Area and Period
This study was conducted in Saint Paul Hospital Millennium Medical College (SPHMMC), pediatric department. It is the second largest hospital located in the capital, Addis Ababa, with a catchment population of more than 5 million. The study was conducted from May 2022 to September 2022 and it retrieved patients’ data who were admitted and/or followed at cardiac follow-up clinic from January 1, 2018 to December 30, 2021.
Study Design
Hospital-based cross-sectional study was conducted at SPHMMC, pediatric and child health department.
Source Population
All pediatric cardiac patients (<18 years of age) treated at SPHMMC, pediatric and child health department.
Study Population
All pediatric cardiac patients (<18 years of age) treated at SPHMMC with the diagnosis of rheumatic heart disease.
Inclusion and Exclusion Criteria
Inclusion Criteria
All pediatric cardiac patients (<18 years of age) treated with the diagnosis of RHD at SPHMMC, pediatric department and whose charts contain complete information were included.
Exclusion Criteria
Pediatric patients whose charts were incomplete or missing during the study period were excluded.
Sample Size Determination and Sampling Techniques
Using a purposive sampling technique, all pediatric patients with RHD and who fulfilled the inclusion criteria in the above-mentioned period are included in the study. We selected this time frame (from January 1, 2018 to December 30, 2021) because it was since 2018 that the department recruited pediatric cardiologists.
Data Collection Tools
Data collection was done using a structured and pre-tested questionnaire. It was prepared in English and later modifications made based on the pretest results before the study period. The main source of data was pediatric echocardiographic logbook, cardiac follow-up clinic registration and chart review by trained data collectors and general practitioners working in the pediatrics department. The primary investigator was responsible for reviewing the data collection forms to ensure their completeness and accuracy.
Study Variables
Dependent Variable
Complications related to RHD such as heart failure, malnutrition, pulmonary hypertension, infective endocarditis, arrhythmia, anemia, embolic stroke, thrombus and cardiogenic shock are the dependent variables.
Independent Variables
- Age.
- Sex.
- Nutritional status.
- Socioeconomic class of the family.
- Precipitating factors for heart failure.
- Types of valvular lesions.
- Severity of valvular involvement.
Operational Definitions
- Rheumatic heart disease: is the result of permanent heart valve damage secondary to acute rheumatic fever.
- Complications related to rheumatic heart disease: Complications which occurred mainly as a consequence of chronic rheumatic heart disease. For the purpose of this research, we described these as heart failure, pulmonary hypertension, malnutrition, infective endocarditis, arrhythmia, embolic stroke, cardiogenic shock and presence of clot in the left chambers of the heart.
- NYHA functional status is functional capacity classification of patients based on their symptoms.21
Class I - No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, dyspnea (shortness of breath).
Class II - Slight limitation of physical activity. Comfortable at rest. Ordinary physical activity results in fatigue, palpitation, dyspnea (shortness of breath).
Class III - Marked limitation of physical activity. Comfortable at rest. Less than ordinary activity causes fatigue, palpitation, dyspnea.
Class IV - Unable to carry on any physical activity without discomfort. Symptoms of heart failure at rest. If any physical activity is undertaken, discomfort increases.
- Infective endocarditis: For this research we included those with definite infective endocarditis and avoided those with a diagnosis of possible infective endocarditis.
- Nutritional status (Wasting and stunting): WHO Z-score classification for malnutrition was used to assess and categorize the nutritional status of the children included in our study. Acute malnutrition (wasting) assessed by weight/length score and chronic malnutrition (stunting) assessed by length/age score.
- Interpretation of anthropometric values was based on the WHO Z-scores, interpreted as moderate and severe wasting if weight for height is < - 2SD to > - 3SD and < -3SD respectively.
- Moderately and severely stunted if length/height for age was < - 2SD to > - 3SD and < -3SD respectively.
- According to the Ethiopian National Planning Commission analysis study interim Report in 2015/16, the total poverty line is less than 586 birrs (Ethiopian currency) per month.
Data Processing and Analysis
A properly designed data collection tool was prepared and utilized. This questionnaire is pretested, and the pretest results are not included in the final manuscript. The principal and co-investigators were involved to check the accuracy and completeness of the data.
After data collection, each data set was checked based on the code given during data collection. The data were entered into SPSS version 25 statistical package. Coding of individual questionnaires was checked before data entry into the software. Further data cleaning was performed to check for outliers, missed values and any inconsistencies before the data were analyzed using the software. Descriptive statistics were used to describe the independent variable. Bivariate analysis was done to see the association between dependent and independent variables using the binary logistic regression. Confidence limit of 95% and p-value less than 0.05 will be considered statistically significant.
Ethical Considerations
The study was approved by the Institutional Research Board (IRB) of SPHMMC according to Ethiopian national research guidelines. Informed consent was taken from each patient during their follow-up at the cardiac clinic, and the privacy and confidentiality of all participants were secured.
Results
Socio-Demographic Characteristics of Patients
From the total 140 patients who were diagnosed with RHD, 59.9% were females and the most common age group affected was in the range 11–15 years, accounting for 54.2% (76), and all the remaining subjects were between the age of 6–10 years. The mean age of study subjects was 10.8 years. Most of the patients are from rural parts of the country while 34.4% (48) of them are living in an urban area (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Patients with Rheumatic Heart Disease |
The crude odds ratio analysis has shown that patients’ age, address and parents’ income have associations with the likelihood of developing any of the three most common complications, but the adjusted odds ratio shows statistical significance is seen only in the higher ages where older children 11–15 years are at higher risk to develop any of those complications.
Pattern of Valvular Involvement with Severity
Echocardiographic report review has revealed 136 (97.1%) patients had mitral regurgitations (MR) out of which 62.5% had severe MR, 22.8% had moderate MR and 14.7% had mild MR. Females contribute to 60% of all patients with any degree of mitral regurgitation. The majority of patients (65.7%) had involvement of both mitral and aortic valve. Isolated mitral valve and aortic valve involvement were 33.6% and 1.45%, respectively. A variable degree of mitral stenosis is seen in 31.4% of patients, the majority (23; 52.3%) of whom are with moderate mitral stenosis. Severity and pattern of valve involvement are summarized in Table 2.
 |
Table 2 Severity and Pattern of Valvular Involvement |
Complications
At least one complication related to rheumatic heart disease was seen in 117 (83.6%) of the patients; of which the most common one was heart failure, 61.4%, followed by pulmonary hypertension (59.3%) and malnutrition (50.7%). Other complications identified were infective endocarditis (4.2%) and arrhythmia in 4 patients (n = 44, 9.1%), all of which were atrial fibrillation. Pericardial effusion was identified in 9 patients (6.4%) from the total of 140 patients, but its severity was not categorized. (See Figure 1, complications among pediatric patients with RHD.) The details of the results are described only for the three most common complications.
Heart Failure
The most common complication recognized was heart failure, presented in 61.4% of subjects with higher percentage in female gender and older age groups (63.1% of females vs 58.9% of males and 56.3% in 6–10 vs 65.8% in 11–15 age groups). Association was found in patients with mitral regurgitation, aortic regurgitation and in those with combined mitral and aortic valve involvement but statistical significance occurred only in patients having moderate and severe degree of regurgitations (Table 3).
 |
Table 3 Association Between Heart Failure and Selected Independent Variables |
Pulmonary Hypertension
Next to heart failure, pulmonary hypertension was the second most common complication that existed in pediatric patients with RHD, seen in 59.3% of them. Among those who developed pulmonary hypertension almost half of them (51.8%) had severe pulmonary hypertension, 42.2% of them had moderate pulmonary hypertension and only 6% of them had mild pulmonary hypertension. Similar to heart failure it is observed in the older age group with 67.1% but having no statistical significance; but to the contrary, the gender percentage is dominated by males (71.4%), while nearly half (51.2%) of the females had developed pulmonary hypertension, showing statistical significance with p-value of 0.031. Similarly, association with pulmonary hypertension was identified in address, family income, moderate and severe MR, moderate and severe mitral stenosis (MS) and when both mitral and aortic valves are involved but statistical significance was seen only in severe MS. (Table 4).
 |
Table 4 Correlation Between Pulmonary Hypertension and Independent Variables |
Nutritional Status
Anthropometric measurements to assess the nutritional status revealed about 50.7% of the patients were malnourished (underweight and/or stunted and/or wasted). Nearly half of the patients (45.7%) had a variable degree of wasting. Severe wasting (severe acute malnutrition) is seen in 12.8% and moderate wasting (moderate acute malnutrition) among 32.9% of the patients. The overall occurrence of stunting was 3.7%, while severe stunting accounted for 0.8% and moderate stunting was 2.9% (Figure 2).
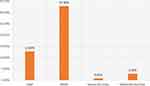 |
Figure 2 Nutritional status of patients with RHD. Abbreviations: MAM, moderate acute malnutrition; SAM, severe acute malnutrition. |
Both age categories contributed nearly half of the percentage among malnourished children but those in the older age group had a greater risk of developing malnutrition while the female gender lacks statistical significance even though association was seen calculating the crude odds ratio. Statistical significance with occurrence of malnutrition is noticed in those with moderate and severe MR and severe AR (Table 5).
 |
Table 5 Correlation between nutritional status and independent variables |
Classifications Based on Functional Status
According to the NYHA functional grading, the majority of patients were in NYHA class III (46.4%) followed with NYHA class I (26.4%), and NYHA classes II and IV each account for 13.6% of the patients. With regard to the age distribution among those with poor functional status (NYHA classes III and IV), most (61.9%) are in the age category 11–15 years. As was described earlier, severe MR is the commonest lesion identified while 62.4% of the patients had NYHA class III functional status. A statistically significant association is observed in those with NYHA class IV symptoms and with severe mitral and aortic regurgitant lesions.
Discussion
The majority of studies in the past have described either the female predominance14 or similarity15 in the incidence of rheumatic heart disease from a gender perspective. Likewise, in our study, the female: male ratio was found to be 1.5:1.
Each of the three most common complications (heart failure, pulmonary hypertension and malnutrition) or in combination are more likely to be seen in older age category (11–15 years), male gender, valve lesions involving both mitral and aortic valves and in those with moderate and severe MR and severe AR, but no statistical significance was observed in any of these.
While looking at a study conducted to assess the clinical profile of children (<18 years) with rheumatic heart disease in eastern India, mitral regurgitation is observed in 60.2% of 133 pediatric patients which is far less than the percent observed in our study, 97.1%, while mitral valve stenosis is more prevalent in their study, 87 (65.4%), than that of ours which is 31.4%. In a similar study aortic valve regurgitation is seen in only 3% but in our study 67.1% of patients had aortic regurgitation. We have classified and included all severity of involvement while that study mentioned only area of involvement and did not describe whether all severity categories are included or not.16
From the total 140 patients with RHD, at least one complication is observed in 117 (83.6%) patients. Heart failure was the most common identified complication, seen in 61.4% of all 140 patients, followed by pulmonary hypertension and malnutrition, 59.3% and 50.7%, respectively. Of those with pulmonary hypertension, 51.8% had severe pulmonary hypertension, moderate pulmonary hypertension was seen in 42.2%, and 6% had mild pulmonary hypertension. Other common complications observed among the 140 patients were malnutrition (45.7%) and infective endocarditis (3.6%). These results are comparable with a study conducted by Sayantani Ghosh and Saugat Dey at B S Medical College tertiary care institution in eastern India. They identified the three most common complications to be pulmonary hypertension (37.41%) followed by congestive cardiac failure (32.38%) and infective endocarditis (6.37%) of a total of 596 RHD patients aged <30 years. This particular study may not be a good comparison as the majority of study subjects were with age above 18 years, constituting 77.7% (463) of the study population and the nutritional status was not assessed.16 In our study all patients who are found to be severely malnourished have already developed heart failure as a complication which obviously affects the nutritional status of the patient. Arrhythmia is observed at higher rate (9.1%) in our study with a probable explanation of a relatively small number of patients, 44, who had an ECG. The most likely reason why these patients had an ECG might be because of the clinician suspicion for arrhythmia which could increase the yield of a positive result. These data have shown that only a small percentage of patients had a baseline ECG, which should have been done on every patient.
In our study infective endocarditis was seen only in 3.6% of patients which is lower in comparison with the above study from India (6.4%). The two possible reasons could be: first, we have included only definitive infective endocarditis while they have possibly included those cases with possible infective endocarditis diagnosis; and second, it is difficult to compare our study with theirs as they have included patients with older age who could have additional risk factors for infective endocarditis that are not frequently seen in a pediatric age group.
Various elements affect mortality in CHF patients, nutritional status being one of them. Those with malnutrition are at higher risk of death in comparison with those with normal nutritional status.17 Most of the studies in this spectrum to assess nutritional status in cardiac patients are from developed countries where rheumatic heart disease is no longer a problem and even in those conducted in developing nations including Ethiopia less emphasis is given than desirable. A prevalence of 50.7% malnutrition in our study is a significant figure which requires due attention as it will contribute to the prognosis of these patients.
There is scarcity of data describing the magnitude of malnutrition in pediatric patients with rheumatic heart disease. In Ethiopia, to our knowledge there are very few studies which have assessed the nutritional status in pediatric cardiac patients and all of them are in those with congenital heart disease except one, published in 2016 and which included all causes of heart failure.18 In this hospital-based review of 106 pediatric heart failure cases, 79.2% of patients had malnutrition, higher than the finding in our study (50.7%). The largest proportion, 53.8%, was mild malnutrition which is not in the current WHO Z-score classification of malnutrition severity. Again, they did not classify the malnutrition as acute (wasting) and chronic (stunting).
In a retrospective cross-sectional study from 2016 to 2019, conducted in Hawassa University Comprehensive Specialized Hospital (HUCSH), Ethiopia, higher prevalence (51.8%) of severe acute malnutrition was found among unoperated children with congenital heart disease (CHD);19 and another study also identified the overall prevalence of wasting, underweight and stunting were 41.3%, 49.1% and 43%, respectively in children with age ranging from 3 months to 17 years diagnosed to have CHD.20
In a cross-sectional study of 315 subjects that was conducted at Mulago National Referral Hospital, Uganda with a median age of 30 years in both genders, unlike that of ours which is 10 years, they assessed complications in newly diagnosed rheumatic heart disease patients. Complications were identified in 49% (152/309) of them which is lower than our study at 83.6% (117/140). Some complications such as malnutrition and cardiogenic shock were not included in their study which will lower the prevalence. In line with our study, heart failure was the most common complication (46.9%).8
The finding in NYHA functional grading is inconsistent with the study done in eastern India in which 68.2% were in the early stage, NYHA class I, while most of our patients were in NYHA class III (46.4%).16 Such variation might be due to the large number of patients with complications in our study with severe valvular lesions and most are from rural part of the country with limited access to a health facility. In the previously mentioned study, they have included patients with age up to 30 years which could also have an impact on the values. The other explanation is most of our patients are admitted as inpatients with exacerbation of the symptoms because of other factors and if we evaluate these patients in the cardiac follow-up clinic after discharge there might be improvement on the functional status, so it would be better to have the comparison when patients are at the same level, either at admission or discharge or at cardiac follow-up clinics.
Recommendation
We recommend a similar large-scale study to be conducted at the national level and the introduction of a national RHD registry to better understand the magnitude of the problem, based on which necessary action will be undertaken. There is also a need to assess the proper implementation of screening and preventive RHD programs.
Strength and Limitations
Strength
- This study has addressed its objectives and the team constitutes senior pediatricians with public health background and pediatric cardiologist.
Limitations
- Lack of national registry which could provide all desired information.
- It is a retrospective study, and data were obtained from medical cards which lack proper documentation.
- Some of the investigations were not properly handled or documented, especially ECG, that was difficult to obtain and interpret.
- Some patients’ diagnoses was documented simply as cardiac patient which required additional effort.
- It is a study from a single institution which may limit to draw conclusions as a nation.
Conclusions
The majority of patients presented to our health facility with complications which implies the need for actions at the community level to detect the disease at an early stage. Malnutrition is seen in a highpercentage of patients with RHD which necessitates the need to establish nutritional guideline for such patients. More than half of the patients are with poor functional status which signifies the need for intervention. The three most common complications are more likely to be seen at older age, in male gender, in those with mixed lesions involving both mitral and aortic valves.
Abbreviations
AR, Aortic Regurgitation; AS, Aortic Stenosis; LMICs, low- and middle-income countries; MAM, moderate acute malnutrition; MR, Mitral Regurgitation; MS, Mitral Stenosis; NYHA, New York Heart Association; RHD, Rheumatic Heart Disease; SAM, severe acute malnutrition; SPHMMC, Saint Paul Hospital Millennium Medical College; SPSS, Statistical Package for Social Sciences; WHO, World Health Organization.
Ethics
Our study complies with the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Watkins DA, Johnson CO, Colquhoun SM, et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N Engl J Med. 2017;377:713–722. doi:10.1056/NEJMoa1603693
2. Zühlke L, Engel ME, Karthikeyan G, et al. Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart dis- ease: the Global Rheumatic Heart Disease Registry (the REMEDY study). Eur Heart J. 2015;36:1115–1122a. doi:10.1093/eurheartj/ehu449
3. Remenyi B, Carapetis J, Wyber R, Taubert K, Mayosi BM; World Heart Federation. Position statement of the World Heart Federation on the prevention and control of rheumatic heart disease. Nat Rev Cardiol. 2013;10:284–292. doi:10.1038/nrcardio.2013.34
4. Rothenbühler M, O’Sullivan CJ, Stortecky S, et al. Active surveillance for rheumatic heart disease in endemic regions: a systematic review and metanalysis of prevalence among children and adolescents. Lancet Glob Health. 2014;2:e717–e726. doi:10.1016/S2214-109X(14)70310-9
5. Mirabel M, Tafflet M, Noël B, et al. Prevalence of rheumatic heart disease in the Pacific: from subclinical to symptomatic heart valve disease. J Am Coll Cardiol. 2016;67:1500–1502. doi:10.1016/j.jacc.2016.01.019
6. Tompkins DG, Boxerbaum B, Liebman J. Long-term prognosis of rheumatic fever patients receiving regular intramuscular benzathine penicillin. Circulation. 1972;45:543–551. doi:10.1161/01.cir.45.3.543
7. Zühlke L, Karthikeyan G, Engel ME, et al. Clinical outcomes in 3343 children and adults with rheumatic heart disease from 14 low- and middle-income countries: two-year follow-up of the Global Rheumatic Heart Disease Registry (the REMEDY study). Circulation. 2016;134:1456–1466. doi:10.1161/CIRCULATIONAHA.116.024769
8. Okello E, Wanzhu Z, Musoke C, et al. Cardiovascular complications in newly diagnosed rheumatic heart disease patients at Mulago Hospital, Uganda. Cardiovasc J Afr. 2013;24:80–85. doi:10.5830/CVJA-2013-004
9. Yadeta D, Hailu A, Haileamlak A, et al. Prevalence of rheumatic heart disease among school children in Ethiopia: a multisite echocardiography-based screening. Int J Cardiol. 2016;221:260–263. doi:10.1016/j.ijcard.2016.06.232
10. World Health Organization. Rheumatic Fever and Rheumatic Heart Disease: Report of a WHO Expert Consultation, Geneva, 29 October- 1November 2001. World Health Organization; 2004.
11. Gemechu T, Parry EHO, Yacoub MH, Phillips DIW, Kotit S. Community-based prevalence of rheumatic heart disease in rural Ethiopia: five-year follow-up. PLoS Negl Trop Dis. 2021;15(10):e0009830. doi:10.1371/journal.pntd.0009830
12. Mengistu AD. The hidden epidemic of rheumatic heart disease in Ethiopia: a wake-up call. Ethiop Med Jl. 2019;57:1.
13. Oli K, Asmera J. Rheumatic heart disease in Ethiopia: could it be more malignant? Ethiop Med J. 2004;42(1):1–8. PMID: 15884271.
14. Berry JN. Prevalence survey for chronic rheumatic heart disease and rheumatic fever in northern India. Br Heart J. 1972;34:143–149. doi:10.1136/hrt.34.2.143
15. Grover A, Dhawan A, Iyengar SD, Anand IS, Wahi PL, Ganguly NK. Epidemiology of rheumatic fever and rheumatic heart disease in a rural community in northern India. Bull World Health Organ. 1993;71:59–66.
16. Ghosh S; Saugat Dey: B S Medical College, India. Clinical profile of Rheumatic Heart Disease in children and young people in Eastern India. Int J Collab Res Inter Med Public Health. 2011;2011:1.
17. Abdoul Carime N, Cottenet J, Clerfond G, et al. Impact of nutritional status on heart failure mortality: a retrospective cohort study. Nutrit J. 2022;21. doi:10.1186/s12937-021-00753-x
18. Gebremariam S, Moges T. ”pediatric heart failure, lagging, and sagging of care in low income settings: a hospital based review of cases in Ethiopia”. Cardiol Res Pract. 2016;2016:7. doi:10.1155/2016/7147234
19. Assefa B, Tadele H, Abedi S. Severe acute malnutrition among unoperated Ethiopian children with congenital heart disease: a wake-up call to reverse the situation, a retrospective cross-sectional study. Ethiop J Health Sci. 2020;30:5. doi:10.4314/ejhs.v30i1.2
20. Tsega T, Tesfaye T, Dessie A, Teshome T. Nutritional assessment and associated factors in children with congenital heart disease, Ethiopia. PLoS One. 2022;17(9):e0269518. doi:10.1371/journal.pone.0269518
21. Little, Brown & Co. Boston. The Criteria Committee of the New York Heart Association. Nomenclature and Criteria for Diagnosis of Diseases of the Heart and Great Vessels.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

