Back to Journals » International Journal of Women's Health » Volume 15
Depression, Anxiety, Stress, Associated with Lichen Planus in Jordanian Women and the Impact on Their Quality of Life
Authors Alnazly E , Absy N , Sweileh I
Received 12 July 2023
Accepted for publication 22 November 2023
Published 27 November 2023 Volume 2023:15 Pages 1883—1892
DOI https://doi.org/10.2147/IJWH.S430162
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Elie Al-Chaer
Eman Alnazly,1 Nadine Absy,2 Ibrahim Sweileh3
1Faculty of Nursing, Al-Ahliyya Amman University, Amman, Jordan; 2Al Hussain New Salt Hospital, Amman, Jordan; 3Florida Gulf Coast University, Health Science Department, Fort Myers, FL, USA
Correspondence: Eman Alnazly, Faculty of Nursing, Al-Ahliyya Amman University, Amman, 19328, Jordan, Tel +966 5 3500211/217 Ext. 2593/4502, Fax +00962 -6- 5335169, Email [email protected]
Purpose: To identify mental health problems in patients with lichen planus (LP). We evaluated the impact of LP on patients’ mental health and quality of life and the associations with sociodemographic and clinical characteristics.
Materials and Methods: This cross-sectional study was conducted in Amman, Jordan, between August 2022 and May 2023. We conducted a survey of 126 women with LP mean age of 48.61 years and a standard deviation of 15.25 years. The survey included sociodemographic characteristics, the Arabic version of the Dermatology Life Quality Index (DLQI), and the 21-item Depression, Anxiety, and Stress scale.
Results: The DLQI scores indicated that LP had substantial effects on the quality of life of most of the participants (63.5%), and the condition was significantly correlated with depression (r = 0.381), anxiety (r = 0.469), and stress (r = 0.475). Longer disease duration and misdiagnosis prior to LP diagnosis were also significantly correlated with quality of life (r = 0.388 and r = 0.317, respectively), as were the LP symptoms. The most robust correlation coefficients were observed for itching symptoms and location in the genital area (r = 0.277 and r = 0.354), respectively.
Conclusion: Depression, anxiety, and stress can significantly reduce the quality of life among patients with LP. This study proves the need for healthcare providers to consider interventions that improve the psychological well-being and QOL of patients. Additionally, this study highlights the importance of the implementation of evidence-based practice to improve the timely diagnosis of LP. It is essential to follow a comprehensive approach when diagnosing and treating LP. This involves a multidisciplinary collaboration between different specialties as well focusing on patient education.
Keywords: dermatology life quality index, mental health, psychological distress, autoimmune disease, skin disease
Introduction
Lichen Planus (LP) is a chronic inflammatory disorder affecting the skin and mucous membranes.1,2 The prevalence of LP is approximately 1–2% globally.2 The prevalence of LP in Jordan was estimated to be 0.73% out of the total number of patients who visited the dermatology outpatient clinic. The clinic is located in the capital Amman and receives 63% of the Jordanian population.3 Oral LP is more common, and is reported in approximately 1% to 4% of the American population.4 Furthermore, Oral LP occurs mainly in middle-aged individuals.5
LP is characterized by the formation of itchy, flat-topped, shiny, reddish-purple polygonal bumps that may appear on the skin or mucous membranes.4 In the mouth and on genital mucosa, LP may present as bright red and painful open sores or lacy white patches,1,2, and, in healed areas, hyperpigmentation or hypopigmentation of the skin may occur.2
The exact cause of LP is unknown, but it is believed to be immune-mediated by T-T lymphocytes.5 Psychological stress, depression, anxiety, gender, and genetic disposition, are documented as triggering factors of LP.6 Women are more likely to be affected by LP than men.4
Individuals with LP often develop psychological problems, including stress, depression, and anxiety, owing to the profound effects associated with the condition.7 The condition can profoundly affect the quality of life, and likely to develop psychological problems.8 Vulval Lichen Sclerosus can affect patients’ ability to use the toilet, sit, and walk and cause other psychological issues such as low self-esteem and confidence.9 A survey found that five women with the condition had considered self-harm.10 A 2022 qualitative study of women with Vulval Lichen Sclerosus found that one of the major themes was the secret lives lived by women experiencing stigma and isolation due to the condition.7 Sadowink et al found that the main theme was suffering, with sub-themes of isolation, interference, and grief.11 These included being silent because women feel powerless to discuss their condition, lack of external validation and support, and feeling different. However, most of the women expressed negative images of the appearance of genitalia.11
In another study, the researchers indicated that the longer the duration of OLP, the poorer the quality of life and the higher the level of perceived stress.12 In addition, individuals with high levels of perceived stress were found to have elevated levels of depression and anxiety.12 Elevated levels of depressive symptoms were associated with a poor quality of life. Fiocco et al13 found that approximately 29% of patients with LP had mild to moderate depressive symptoms.14 However, six percent of patients with LP had severe depressive symptoms.13 In addition, five out of ten patients reported experiencing stress due to their condition.13
Symptoms associated with LP, such as pain, itching, and skin lesions, negatively impact patients’ health-related quality of life (HRQoL).15 The impact of LP on HRQoL includes adverse effects on emotional well-being (such as embarrassment and frustration), social functioning (including social activities and intimacy), activities of daily living (such as dressing and oral hygiene), and physical functioning (such as chewing and swallowing).15 Cutaneous LP also has a negative impact on patients’ emotional well-being and is mainly associated with depression, anxiety, frustration, sadness, worry, and embarrassment.15,16
Sawant et al17 found that approximately 25% of patients with LP had depression, with women being more affected than men. In addition, approximately 90% of patients with LP had poor QoL.17 Poor QoL in patients with LP was associated with work and time spent on treatment, the symptoms and feelings of illness, and interference with daily activities.17 Poor QoL was associated with depressive symptoms in both men and women with LP.17 Furthermore, patients with LP were more likely to experience mixed anxiety, depression, social phobia, panic attacks, obsessive thoughts, and dysthymia.18,19 Studies have furthermore shown that the impact of skin conditions on a patient’s quality of life is often considered to be a better indicator of psychiatric morbidity such as depression, anxiety, sleep disturbance, and adjustment disorders.14,20 Fiocco et al.13 A 2021 study13 reported that the disease burden of LP and its impact on depressive quality is influenced by the affected areas, after finding significantly higher Dermatology Life Quality Index (DLQI) scores in patients with genital LP; moreover, the scores were significantly elevated in ungual and cutaneous LP cases.13 One study reported that women avoid social activities because they are more conscious of their body appearance than men.21 However, few studies have examined mental health and quality of life (QoL) among patients with LP. Thus, this study was aimed at evaluating the impact of LP on mental health and QoL and its associations with the patients’ sociodemographic and clinical characteristics.
Materials and Methods
Study Design and Participants
This cross-sectional study was conducted in Jordan’s capital, Amman.
Recruitment Procedure
Participants were women recruited from 19 private primary care physician clinics, OBGYNs, dermatological clinics, and oral surgeons between May 2022 and May 2023. We placed flyers in waiting areas and on social media. A flyer announced the study, its purpose, and its significance. The researchers’ phone numbers were on the flyer for patients who were interested in contacting the researchers. The researchers screened 155 patients who contacted the researchers; 131 met the inclusion criteria, 126 participants completed the surveys, and five patients apologized for not participating.
All potential patients who provided verbal permission for their contact information to be shared with the research team were contacted by one of the research staff, phone interviews were conducted, and the study aims and procedures were explained. The participants were directed to provide consent and the e-survey form links.
Inclusion and Exclusion Criteria
As per the inclusion criteria, women older than 20 years were included. Each patient had been officially diagnosed with LP. All were either newly diagnosed or experiencing flare-ups of LP symptoms at the time of study participation. The exclusion criteria were diagnosis of another autoimmune disease, such as rheumatoid arthritis or scleroderma, and known cognitive impairments, such as dementia.
Data Collection
The e-Survey
Arabic versions of the DLQI and the DASS-21 were used.22,23 The e-survey questionnaires were created using Google Forms (GFs). Survey responses were automatically collected and exported to an Excel spreadsheet for data analysis.
A pilot study was conducted with 11 patients to determine the face validity of the instruments included in the survey—the DLQI22 and the Depression, Anxiety, and Stress Scale (DASS-21),23 which is a short version of the DASS-4224 and the practicality of administering questionnaires. None of the pilot study participants were included in the main study.
The survey was administered online, and the checklist for reporting the results of e-surveys (usually abbreviated as “CHERRIES”) was used to report the results.25
Study Tools
The study tools included demographic data, DLQI, and the 21-item Depression, Anxiety, and Stress Scale (DASS-21).
Demographic Data
The first section included ten questions related to demographic characteristics. The authors composed a general list of questions relevant to the data, such as level of education and marital status (see Table 1).
 |
Table 1 Demographic Characteristics of the Participants |
The Dermatology Life Quality Index
The DLQI is a dermatology-specific questionnaire that assesses the health-related QoL in adult patients with skin diseases (Finlay & Khan, 1994).22 The DLQI is a 10 questions survey that asks patients about the impact of skin disorders on several aspects of their health-related QoL in the previous seven days. Each item is scored on a four-point Likert scale: very much = 3, a lot = 2, a little = 1, not a lot = 0, and not relevant = 0. Question 7, “prevents work or studying”, was scored as yes = 3 or no = 0. The total score was determined by adding each question’s score to a maximum of 30 and a minimum of 0. A score > 10 indicates that the patient’s skin ailments significantly impacted their lives.
Scores of 0–1 = no effect at all on patient’s life; 2–5 = small effect on patient’s life; 6–10 = moderate effect on patient’s life, 11–20 = very large effect on patient’s life; and 21–30 = extremely large effect on patient’s life. The DLQI can be divided into six subscales: symptoms and feelings, daily activities, leisure, work and school, personal relationships, and treatment.22
Depression, Anxiety, and Stress Scale (DASS-21)
The DASS-21 was used to evaluate patients’ symptoms of depression, anxiety, and stress scale in the last week.23 These three subscales assess the presence and intensity of depression, anxiety, and stress. Each subscale includes 7 items. The DASS-21 is a condensed version with 42 items. The items were rated on a Likert scale ranging from 0 to 3 (0 = does not apply to me at all; 1 = applies to me to some degree of the time; 2 = applies to me to a significant degree or a fair portion of the time; 3 = applies to me very much or most of the time). In this study, the scores of the relevant items were as follows: depression: normal 0–9, mild 10–13, moderate 14–20, severe 21–27, and extremely severe 28+; anxiety: normal 0–7, mild 8–9, moderate 10–14, severe 15–19, and extremely severe 20+; stress: normal 0–14, mild 15–18, moderate 19–25, severe 26–33, and extremely severe 34+. The scores of the relevant items are added to calculate depression, anxiety, and stress scores. The final score of each subscale is multiplied by two and evaluated according to its severity rating index because the DASS-21 is a short-form version of the 42-item DASS; severity ratings range from normal to extremely severe.23
Reliability and Sample Size
The questionnaires were piloted with 11 patients using test-retest reliability. The original DLQI’s reliability was tested in 53 patients using a one-week test-retest method, which was determined to be 0.99.22 The test-retest reliability of the DLQI for this study was 0.88.
For the DASS-21 (English version), Cronbach’s alpha was 0.81 for the depression scale, 0.89 for the anxiety subscale, and 0.78 for the stress scale.26 The DASS-21 Arabic version reliability alpha coefficients were 0.843 for depression, 0.818 for anxiety, 0.843 for stress, and the overall reliability was 0.939.27
In the present study, Cronbach’s alpha for DASS-21 test-retest reliability for the 11 pilot study participants was 0.890 for the depression scale, 0.910 for the anxiety subscale, and 0.920 for the stress scale; overall reliability = 0.940.
Regarding the sample size, the incidence in Jordan remains unclear. However, one similar study8 employed a sample size of 41. We were able to recruit 126 people over a year from the capital, Amman, Jordan, which has a population of four million people.
Ethical Approval and Consent to Participant
The Human Subjects Review Board at Al-Ahliyya Amman University approved this study in May 2022 by the Declaration of Helsinki ID number 3/7-2022.
Data Analysis
Data analyses were performed using the SPSS (version 20.0) software. No missing data were recorded. Descriptive statistics were used to analyze the variables of interest. This consisted of the mean, standard deviation, percentage, and frequency. Pearson’s correlation was used to test the relationship between the nominal demographic data and the LDQI and DASS-21 subscale scores. The significance level was set at p < 0.05.
Results
A total of 126 women patients with LP were recruited in the study with a mean age of 48.61 and a standard deviation of 15.25; most of the sample had a high school education level of 57 (45.2%) and married 81 (64.3) (Table 1).
Regarding LP characteristics, 86 (68.3%) of patients had been diagnosed by the biopsy; the multiple response analysis demonstrated that 89.7% and 78.6% of patients experienced itching and pain. LP locations were primarily the genitalia and mouth, at 50.0% and 28.6%, respectively. The sample mean and standard deviation ((M ± SD) of age when having the symptoms was (39.61 ±13.96) years, and the sample age when the LP was diagnosed was (M ± SD) (48.09 ±15.28) years, indicating there was a mean of (M ± SD) (8.48 ±5.51) years living with the symptoms before LP was diagnosed (Table 1). The mean DLQI score for the study sample with LP was (M ± SD) (16.43 ±4.68). The mean subscale treatment (2.34+0.77) followed by symptoms and feelings 2.06+0.66). However, the results have shown that all patients were affected, from moderate (12.7%), very large (63.3%), and extremely large (23.8%). Treatment and symptoms and feelings impacted patients the most (M ± SD) (2.34+0.77), (2.06+0.66), while the least impacts were observed on daily activities and personal relationships (M = 1.34 and M = 1.28). (M+SD) (1.34+0.84) (1.28+20) (Table 2 and Table 3). (Table 4) shows the depression, anxiety, and stress mean scores for the participants with LP.
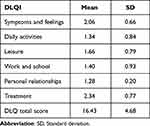 |
Table 2 Dermatology Life Quality Index Subscale Scores Among Patients with LP |
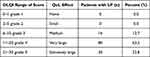 |
Table 3 Dermatology Life Quality Index Levels Among Patients with Lichen Planus |
 |
Table 4 Depression, Anxiety, and Stress Scores Among Patients with Lichen Planus |
After categorizing subscale scores based on the tool’s recommendation, (Table 5), reveals that 34.1% (one-third) were severely depressed and stressed, and the majority of participants, 86 (68.3%), had extremely severe anxiety.
 |
Table 5 Depression, Anxiety, and Stress Range of Score Among Patients with Lichen Planus |
(Table 6) revealed that poor DLQI scores significantly correlated with mental illness in terms of depression (r = 0.381), anxiety (r = 0.469), and stress (r = 0.475). Moreover, a longer duration of having the disease before diagnosis and giving the wrong diagnoses before LP was diagnosed was significantly correlated with poor QoL (r = 0.388 and r = 0.317). Similarly, having one of the LP symptoms and its location were significantly correlated with poor QoL. However, the most robust correlation coefficients were found between itching symptoms and their presence in the genital area (r = 0.277 and r = 0.354), respectively.
 |
Table 6 Correlation Among Patients’ Mental Illness, Lichen Planus Characteristics, and Dermatology Life Quality Index (DLQI) |
Discussion
This study evaluated the impact of LP on patients’ mental health and QoL and assessed their associations with sociodemographic and clinical characteristics. The mean age of patients with LP in this study was 48.16 years, which falls in the range of age group (30–70 years) commonly affected by LP.28
Our results indicate that all patients with LP experienced impaired QoL based on DLQI scores. Treatment, symptoms, and feelings were the highest mean subscales showing greater impairment. Patients were on new treatment regimens and lesions on their body parts which were exposed to the public caused them psychological discomfort. The majority of the patients had very large (63.5%) and extremely large (23.8%) effects of LP on their QoL. These results highlight that patients with LP experience a low QoL because of their illness. Other studies support these findings. Sawant17 and Sathianesan and Gopalan28 found that significant LP symptoms reported by the participants were itching, pain, burning, and ulcers. Another study found that pain was the main symptom reported by patients with OLP.29 Moreover, most patients (96%) reported oral symptoms that influence their QoL.29
Our study findings align with the responses to the components of the DLQI: reported symptoms and feelings, daily activities, leisure, work and school, and personal relationships were among the factors that constituted the DLQI scores in this study which aligns with Keswani.29 The identified factors can be used as target variables to implement interventions to improve the QoL of patients with LP. Such interventions targeting feelings of improvement can be implemented to enhance the psychological well-being of patients with LP.
Although not fatal, in this study the high level of LP on QoL might be due to the prevalence of LP symptoms; itching (89.7%), pain (78.6%), 56.3%). Ranum and Pearson reported LP has a significant negative impact on the QoL of patients because of itching and lesions.30 Systematic reviews and meta-analyses by De Porras-Carrique et al31 indicated that depression, anxiety, and stress are more prevalent in patients with OLP than in the general population.31 Correspondingly, the patients with LP in this study experienced various psychological distresses associated with the disease, including depression, anxiety, and stress. Women with LS had a 2.16-to-2.5-fold increase or receiving a diagnosis of comorbid depression or anxiety compared with the control group.32 However, Fiocco et al reported that no significant differences in stress levels were observed between both sexes.13 Based on the Depression, Anxiety, and Stress Score (DASS-21), most patients experienced moderate to extremely severe depression, anxiety, and stress. This indicates that mental health patients with LP in Jordan have similar mental health distress, and lower quality of life.
In a study of patients with Lichen Planopilaris, Nasimi et al17 found a statistically significant correlation between age, disease activity, and DLQI scores. Specifically, age > 45 years and increasing disease symptoms were associated with higher DLQI scores and lower QoL.17 Also, Nasimi et al found that QoL and general health negatively correlated with disease activity.17 Location of LP also affects psychological distress and quality of life. A study found that QoL in patients with OLP was significantly associated with anxiety, pain, and stress.30 Specifically, Wiriyakijja et al.33 Our findings in line with previous studies indicate a significant impact of LP symptoms, location, and psychological well-being on QoL among patients with LP.
Our results highlight a significant correlation between the DLQI scores and depression, anxiety, stress, and illness duration before diagnosis. We also found a significant correlation between the DLQI scores and LP symptoms, such as itching, pain, burning, and bleeding. Moreover, the DLQI scores were significantly correlated with the LP location, including the mouth, genitalia, and face. Therefore, the findings of this study and those reported in the literature support the implications of the effects of psychological distress, LP symptoms, and LP location on QoL among patients with LP.8,33
Considering the significant negative impacts of LP on patients’ QoL, dermatologists should address the QoL aspects alongside treating physical symptoms.8 In this study, we found statistically significant correlations between QoL measured using the DLQI and psychological distress, such as stress, anxiety, and depression, among patients with LP. Therefore, clinicians can improve the QoL of patients with LP by addressing their psychological needs.
In this study, we also demonstrated a statistically significant correlation between QoL based on the DLQI and incorrect diagnoses before LP was diagnosed, since the onset of symptoms and the duration of illness before diagnosis. Therefore, there is a need to implement evidence-based interventions to improve the timely diagnosis of LP. Timely diagnosis facilitates early treatment, reduces the associated negative impacts, and improves the QoL of patients with LP.
In this study, there were cases of late diagnosis and misdiagnosed LP, and both had significant correlations with QoL based on the DLQI. Therefore, the QoL and adverse health outcomes can be improved by implementing interventions that facilitate the accurate and timely diagnosis of LP.
Strengths, Limitations, and Implications
The strengths of this study include the use of a large sample and a valid and reliable tool for measuring QoL in patients with LP compared to previous research. The use of a large sample size improved the power of the study to detect causal effects in correlational tests. In addition, using valid and appropriate tools ensured the accurate measurement of the construct of interest in this study. Another strength is that the participants were newly diagnosed or the symptoms were flared up, implying that they were reflecting on their mental status. These findings may not be valid in other populations, including males with LP or already diagnosed and do not have a flare up the time of the study.
LP negatively impacts the mental health of patients and can cause depression, stress, anxiety, and poor quality of life. Skin disorders affect mental health negatively. A comprehensive approach by physicians should be followed to treat patients’ mental health issues. Referral psychiatrists may be prompted at the time of diagnosis or when symptoms flare. As a result, healthcare providers should address the physical and emotional aspects of LP to provide comprehensive care for patients and achieve optimal clinical outcomes.
Conclusion
This study reports the results of a survey of Jordanian mental health patients with flared symptoms or newly diagnosed with LP and their quality of life. The findings of this study will add to the existing evidence. The study reveals that one-third of the participants were severely depressed and stressed, and most of them had severe anxiety and poor quality of life. The symptoms are correlated with the localization of LP, especially itching and in the genital area. These findings provide valuable insights into and have clinical implications for reducing the psychological effect of LP and improving patients’ quality of life. The clinical impact is developing strategies for reducing patients’ psychological distress during diagnosis and referring them to a mental health support group. Doctors, nurses, counselors, social services, and other health care providers should be aware of LP and the psychological distress caused in patients and provide appropriate support for patients with autoimmune diseases. In conclusion, there is a need to incorporate mental health support into the treatment plan for individuals with LP to address the negative impact on their emotional well-being and thereby achieve improved clinical outcomes.
Data Sharing Statement
Data will be available from the corresponding author upon request.
Acknowledgments
We thank the participants for their contributions and time.
Author Contributions
All authors made a significant contribution to the work reported either in the conception, study design, execution, acquisition of data, analysis, and interpretation or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No financial or material support was provided for this research.
Disclosure
All authors report no conflicts of interest in this work.
References
1. National Health Service Inform. Lichen planus; 2023. Available from: https://www.nhsinform.scot/illnesses-and-conditions/skin-hair-and-nails/lichen-planus#:~:text=Lichen%20planus%20is%20thought%20to,is%20more%20common%20in%20women.
2. National Organization for Rare Disorders. Lichen planus; 2018. Available from: https://rarediseases.org/rare-diseases/lichen-planus/.
3. Leasure AC, Cohen JM. Prevalence of lichen planus in the United States: a cross-sectional study of the all of US research program. JAAD. 2022;87(3):686–687. doi:10.1016/j.jaad.2021.12.013
4. Arnold DL, Krishnamurthy K. Lichen planus. StatPearls Publishing; 2018. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526126/.
5. Foroughi F, Davari P, Fazel N. Cutaneous and mucosal lichen planus: a comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis. Sci World J. 2014. doi:10.1155/2014/742826
6. Vičić M, Hlača N, Kaštelan M, Brajac I, Sotošek V, Prpić Massari L. Comprehensive insight into lichen planus immunopathogenesis. Int J Mol Sci. 2023;24(3):3038. doi:10.3390/ijms24033038
7. Arnold S, Fernando S, Rees S. Living with vulval lichen sclerosus: a qualitative interview study. Br J Dermatol. 2022;187(6):909–918. doi:10.1111/bjd.21777
8. Nasimi M, Ahangari N, Lajevardi V, et al. The quality of life and mental health status in patients with lichen planopilaris based on dermatology life quality index and general health questionnaire-28 questionnaires. Int J Womens Dermatol. 2020;6(5):399–403. doi:10.1016/j.ijwd.2020.09.005
9. Van de Nieuwenhof HP, Meeuwis KA, Nieboer TE, Vergeer MC, Massuger LF, De Hullu JA. The effect of vulvar lichen sclerosus on quality of life and sexual functioning. J Psychosom Obstet Gynaecol. 2010;31(4):279–284. doi:10.3109/0167482X.2010.507890
10. British Association of Dermatologists. One in five women with a vulval health condition contemplate self-harm or suicide. [press release]; 2015.
11. Sadownik LA, Koert E, Maher C, Smith KB. A qualitative exploration of women’s experiences of living with chronic vulvar dermatoses. J Sex Med. 2020;17(9):1740–1750. doi:10.1016/j.jsxm.2020.06.016
12. Radwan-Oczko M, Zwyrtek E, Owczarek JE, Szcześniak D. Psychopathological profile and quality of life of patients with oral lichen planus. J Appl Oral Sci. 2018;26(2018):1–9. doi:10.1590/1678-7757-2017-0146
13. Fiocco Z, Kupf S, Patzak L, et al. Quality of life and psychopathology in lichen planus: a neglected disease burden. Acta Derm Venereol. 2021;101(12):adv00619–adv00625. doi:10.2340/actadv.v101.442
14. Picardi A, Abeni D, Melchi CF, Puddu P, Pasquini P. Psychiatric morbidity in dermatological outpatients: an issue to be recognized. Br J Dermatol. 2000;143(5):983–991. doi:10.1046/j.1365-2133.2000.03831.x
15. Mahon-Smith A, Clifford M, Batish A, et al. Patient experience of lichen planus: a qualitative exploration of signs, symptoms, and health-related quality of life impacts. Dermatol Ther. 2023;13(9):2001–2017. doi:10.1007/s13555-023-00968-2
16. Kalkur C, Sattur AP, Guttal KS. Role of depression, anxiety, and stress in patients with oral lichen planus: a pilot study. Indian J Dermatol. 2015;60(5):445–449. doi:10.4103/0019-5154.159625
17. Sawant NS, Vanjari NA, Khopkar U, Adulkar S. A study of depression and quality of life in patients of lichen planus. Sci World J. 2015;2015(2015):817481–817487. doi:10.1155/2015/817481
18. Magin PJ, Pond CD, Smith WT, Watson AB, Goode SM. A cross-sectional study of psychological morbidity in patients with acne, psoriasis and atopic dermatitis in specialist dermatology and general practices. J Eur Acad Dermatol Venereol. 2008;22(12):1435–1444. doi:10.1111/j.1468-3083.2008.02890.x
19. Kanwar AJ, De D. Lichen planus in children. Indian J Dermatol Venereol Leprol. 2010;76(4):366–372. doi:10.4103/0378-6323.66581
20. Gupta MA, Gupta AK. Psychiatric and psychological co-morbidity in patients with dermatologic disorders: epidemiology and management. Am J Clin Dermatol. 2003;4(12):833–842. doi:10.2165/00128071-200304120-00003
21. Nolen-Hoeksema S. Gender Differences in Depression. Curr Dir Psychol Sci. 2000;10(5):173–176. doi:10.1111/1467-8721.00142
22. Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19(3):210–216. doi:10.1111/j.1365-2230.1994.tb01167.x
23. Moussa MT, Lovibond P, Laube R, Megahead HA. Psychometric properties of an Arabic version of the Depression Anxiety Stress Scales (DASS). Res Soc Work Pract. 2017;27(3):375–386. doi:10.1177/1049731516662916
24. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety & Stress Scales.
25. Eysenbach G. Improving the quality of web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34. doi:10.2196/jmir.6.3.e34
26. Coker AO, Coker OO, Sanni D. Psychometric properties of the 21-item Depression Anxiety Stress Scale (DASS-21). Afr Res Rev. 2018;12(2):135–142. doi:10.4314/afrrev.v12i2.13
27. Al-Kalbani M, Al-Adawi S, Alshekaili W. Psychometric properties of the depression, anxiety, stress scales-21 (DASS-21) in a sample of health care workers in Oman. J Affect Disord Rep. 2022;10(2022):100451. doi:10.1016/j.jadr.2022.100451
28. Sathianesan CP, Gopalan K. A clinico-epidemiological study and assessment of Life Quality Index among patients with lichen planus at a tertiary care centre in South India. J Pak Med Assoc. 2023;33(1):204–214.
29. Keswani N, Dubey S, Kulkarni S, Keswani N. Association between clinical signs of oral lichen planus and oral health-related quality of life. J Life Sci Biotechnol Pharma Res. 2013;12(1):303–308.
30. Ranum A, Pearson DR. The impact of genital lichen sclerosus and lichen planus on quality of life: a review. Int J Womens Dermatol. 2022;8(3):e042. doi:10.1097/JW9.0000000000000042
31. De Porras-Carrique T, González-Moles MÁ, Warnakulasuriya S, Ramos-García P. Depression, anxiety, and stress in oral lichen planus: a systematic review and meta-analysis. Clin Oral Invest. 2022;26(2):1391–1408. doi:10.1007/s00784-021-04114-0
32. Fan R, Leasure AC, Maisha FI, Little AJ, Cohen JM. Depression and Anxiety in Patients With Lichen Sclerosus. JAMA Dermatol. 2022;158(8):953–954. doi:10.1001/jamadermatol.2022.1964
33. Wiriyakijja P, Porter S, Fedele S, et al. Health-related quality of life and its associated predictors in patients with oral lichen planus: a cross-sectional study. Int Dent J. 2020;71(2):140–152. doi:10.1111/idj.12607
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
