Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 14
Depression Among Patients with Type 2 Diabetes Mellitus: Prevalence and Associated Factors in Hue City, Vietnam
Authors Tran NMH , Nguyen QNL , Vo TH, Le TTA , Ngo NH
Received 9 November 2020
Accepted for publication 6 January 2021
Published 4 February 2021 Volume 2021:14 Pages 505—513
DOI https://doi.org/10.2147/DMSO.S289988
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Antonio Brunetti
Nhu Minh Hang Tran,1 Quang Ngoc Linh Nguyen,1 Thi Han Vo,1 Tran Tuan Anh Le,1 Ngoc Ha Ngo2
1Department of Psychiatry, Hue University of Medicine and Pharmacy, Hue University, Hue, Thua Thien Hue, Vietnam; 2Preventive Medicine, Hue University of Medicine and Pharmacy, Hue University, Hue, Thua Thien Hue, Vietnam
Correspondence: Nhu Minh Hang Tran
Department of Psychiatry, Hue University of Medicine and Pharmacy, Hue University, 346/1 Phan Chu Trinh, Hue, Thua Thien Hue, Vietnam
Tel +84905108019
Email [email protected]
Background and Aims: Depression is common in people with type 2 diabetes mellitus. The association of depression and diabetes has negative effects on patients. This study investigated the prevalence of depression in individuals with type 2 diabetes mellitus and examined the social, psychological and clinical factors associated with depression.
Patients and Methods: The study included 216 inpatients with type 2 diabetes mellitus at the Department of Endocrinology and Neurology, Hue Central Hospital and the Department of General Internal Medicine, Hue University Hospital. This descriptive cross-sectional study evaluated depression using the Patient Health Questionnaire-9 (PHQ-9). Data were collected on patients’ socio-demographic factors such as sex, age, marital and economic status, level of education and clinical factors including duration of type 2 diabetes mellitus, fasting blood glucose, HbA1C, comorbidities or complications as well as health behavior including alcohol consumption, smoking and physical activities. Logistic regression was used to analyze the factors associated with depression in patients with type 2 diabetes mellitus.
Results: 23.2% of the patients had depression. The rates of severe, moderate and mild depression were 0.5, 0.9 and 21.8%, respectively. Multivariate logistic regression analysis indicated several factors associated with depression in participants, including age under 60 years, poor economic status, unstable or part-time work, having stress during the past year, without/poor treatment adherence to type 2 diabetes mellitus, and engaging in heavy physical activity or physical activity less than three days per week.
Conclusion: The prevalence of depression among patients with type 2 diabetes mellitus is high. Endocrinologists should be made aware of the increased risk of depression in this patient population and screening individuals for relevant risk factors is highly recommended.
Keywords: depression, type 2 diabetes mellitus, prevalence, risk factors
Introduction
Depression is one of the most common mental health disorders with a lifetime prevalence estimated at approximately 20% of the worldwide population. According to the World Health Organization (WHO), the global prevalence of depression is about 5%, second only to cardiovascular diseases as the leading cause of functional impairment in patients by the year 2020. Any individual can suffer from depression; however, the risk is higher among those with type 2 diabetes mellitus than in the general population. Previous studies have shown that the prevalence of depression was two-fold higher in diabetic patients versus the general population.1 In 2018, Khaledi, Haghighatdoost, Feizi, Aminorroaya2 conducted a meta-analysis of 248 studies around the world (n= 83,020,812 study participants) and showed that the prevalence of depression in those affected by type 2 diabetes mellitus was 28%. This rate was much higher than the 5% reported for the general population by WHO. Alajmani, Alkaabi, Alhosaniet al3 studied 559 type 2 diabetes mellitus patients in Dubai, United Arab Emirates (UAE) using the Beck Depression Inventory (BDI) and found that the rate of depression in these patients was 17%. In Vietnam, the prevalence of depression was reported to be 25.6% in a study conducted by Dang,4 involving 606 diabetic patients at the center of Endocrinology (Quang Ngai province) using the PHQ-9 score of 9 as a cutoff. The combination of depression and diabetes is an important and complicated public health issue. The causal relationship between depression and diabetes is not well understood. Depression can be not only a cause but also a result of hyperglycemia. Diabetes is a chronic condition with a strict treatment regimen that typically includes adherence to medication, diet, and physical activity. Moreover, diabetes can also lead to many complications including macro- and micro-vascular diseases, neuropathy, and nephropathy. Diabetes is one of the most common causes of economic burden, comorbidities and an increase in mortality in the world. These factors become a psychological burden for patients, which can lead them down a path towards depression. Furthermore, depressed patients with type 2 diabetes mellitus have worse adherence to dietary, medication, physical inactivity, metabolic and glucose control problems which can exacerbate diabetic complications resulting in disease severity and increasing health-care expenditures, thereby lowering patients’ quality of life. There have been several studies on depression in type 2 diabetes mellitus in Vietnam and Hue but the associated factors with depression in type 2 diabetes mellitus were uncertain and different among studies. This study investigated the prevalence of depression in patients with type 2 diabetes mellitus by using PHQ-9 in Hue Central Hospital and Hue University Hospital and examined the risk factors associated with depression in these patients.
Subjects and Methodology
Subjects
A total of 216 patients over 18 years old with type 2 diabetes mellitus, using diagnostic criteria of WHO and Vietnamese Ministry of Health guidelines, were selected from their medical records at the Department of Endocrinology and Neurology, Hue Central Hospital and at the Department of General Internal Medicine, Hue University Hospital from September 2018 to April 2019. These are the two biggest hospitals in Hue city. Patients were invited to enroll in the study if they met the following inclusion criteria: signed the written informed consent form and had the ability to answer the questionnaire. The exclusion criteria were as follows: (1) diagnosis of gestational diabetes mellitus, (2) outpatients, (3) inability to understand Vietnamese, (4) having acute and severe complications such as ketoacidosis, high osmotic pressure coma, (5) having severe chronic diseases or/and severe mental disorders that did not allow the participants to answer the interview questions.
Size of Sample
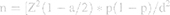
The sample size is calculated using the formula for evaluating disorder prevalence in the community.
n: number of participants, Z(1-a/2) = 1.96 (confidence interval: 95%), d: 0.05, p = 12% (prevalence of depression in patients with type 2 diabetes mellitus in America, in 2013 according to Katon, Young, Russoet al5). We estimated that the required sample size for statistical significance must include at least 162 study participants. Eligible participants were selected by convenient sampling technique, and during the time of the study, we selected a total of 216 patients with type 2 diabetes mellitus.
Methods
Research Design
This was a cross-sectional study, including descriptive and statistical analyses.
Data Measurement
The Vietnamese version of PHQ-9 was used to assess depression in the study participants. This instrument consisted of 9 items, a self-administered questionnaire based on the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) criteria for a major depressive disorder, assessing the patient’s mental health status for a 2-week duration, each rated on a 4-point scale ranging with 0 (not at all), 1 (several days), 2 (more than half the days) and 3 (nearly every day). Response options were used to calculate a continuous total score ranging from 0 to 27; scores of 9 or less indicating no depression, 10 to 14- mild depression, 15 to 19- moderate depression, and 20 to 27- severe depression.6 PHQ-9 have been used and adapted in the context of Vietnam with α Cronbach’ s alpha ranging from 0.823 to 0.867.7,8 To collect risk factors associated with depression, participants used a structured questionnaire on socio-demographic information such as age, gender, occupation, economic, marital status, and level of education, stress events during the past year; and clinical information including duration of diabetes, co-morbid diseases and complications, blood pressure, body mass index, and HbA1c; as well as health behavior consisting of smoking, alcohol consumption and physical activities. HbA1c, which reflects the average blood sugar level in the past three months, was recorded from each patient directly after their hospitalization to estimate how well the diabetes has been controlled over the last 3 months. The HbA1C test was done at the biochemistry departments of Hue Central Hospital and Hue University Hospital. Poor blood glucose control was determined by HbA1C over 7%.
To data quality control, research team members were psychiatrists with at least 6 years of experience and were carefully trained in group in the completion of all measures. For all research instruments, the first author trained the others, case studies, role plays and pilot testing were used in training. Besides, for 20% of interviews, two researchers attended, one as interviewer and the other as observer. And their independent rating was compared. Any difference was discussed with both interviewers.
Statistical Analysis
All statistical analyses were performed using SPSS version 20.0. Chi-squared tests were applied to measure the difference of characteristics between those with and without depression. The odds ratio (OR) and its 95% confidence intervals (CIs) were calculated. A p-value <0.05 was considered statistically significant. Multivariate logistic regression was employed to identify the potential factors associated with depression among patients with type 2 diabetes mellitus.
Ethics
Ethics approval was granted by Hue University. This study was conducted in accordance with the Declaration of Helsinki.
Results
A total of 216 patients with type 2 diabetes mellitus, with the mean age of 64.73 (SD 13.68), 114 women (52.80%) and 102 men (47.20%), participated in the study and completed the questionnaire. Among them, 50 participants (23.20%) had depression according to the PHQ-9 score in which severe depression was 0.5%, moderate was 0.9% and mild was 21.8% (Table 1).
 |
Table 1 Prevalence of Depression According to PHQ-9 Score |
Table 2 shows that the prevalence of depression was significantly higher in patients of age under 60 years (p<0.01), poor economic status (p<0.01), unstable job vs unemployment (30.0% vs 17.7%, p<0.05) and stable job vs unemployment (34,5% vs 17.7%, p<0.05) and having stress events during the past year (p<0.01). There were no significant differences between the depression group and without depression group in gender, marital status, religion, ethnicity, place of living and level of education (p>0.05).
 |
Table 2 Socio-Demographic Characteristics of the Participants and Differences Between Depression and Without Depression Groups |
Among clinical characteristics, there was only poor/no adherence to diabetic treatment associated with depression in patients with type 2 diabetes mellitus (p<0.05), others including BMI, duration of diabetes, glycemic control, co-morbid diseases/complication have no association with depression in the participants (p>0.05) (Table 3).
 |
Table 3 Clinical Characteristics Associated with Depression in Participants |
Patients doing heavy physical activities had the highest prevalence of depression among groups (46,2%, p<0.01) and patients doing physical activities less than 3 days have the rate of depression higher than other groups (50%, p<0.01) (Table 4).
 |
Table 4 Association Between Health Behavior to Depression in the Participants |
Multivariate logistic regression analysis indicated several factors associated with depression in participants including age under 60 years (OR=2.64, 95% CI: 1.38–5.03, p<0.01), poor economic status (OR=2.8, 95% CI: 1.32–5.95, p<0.01), unstable or part-time job (OR=2.45, 95% CI: 1.21–4.95, p<0.05), having stress during the past year (OR=11.18, 95% CI: 2.18–57.33, p<0.01), without/poor treatment adherence with type 2 diabetes mellitus (OR=2.44, 95% CI: 1.07–5.53, p<0.05), doing heavily physical activity (OR=3.88, 95% CI: 1.63–9.24, p<0.01), doing physical activity less than 3 days/week (OR=4.48, 95% CI: 1.80–11.13, p<0.01) (Table 5).
 |
Table 5 Multivariate Logistic Regression Model Predicting Co-Morbid Depression (PHQ-9 Score ≥10) by Socio-Demographic, Clinical, and Health Behavior Factors |
Discussion
The previous studies showed that the prevalence of co-morbid depression is high in patients with type 2 diabetes mellitus.1,2,4 In this study, we found that 23.2% of the study population suffered from depression according to PHQ-9 with a cutoff of 10. The prevalence of depression in type 2 diabetes mellitus varied widely in different countries and studies. Zhang, Xu, Zhaoet al9 studied 2500 patients with type 2 diabetes mellitus in China and showed that the rate of depression in this study was 5.7% (142/2500) according to BDI scores (BDI score ≥14). The prevalence in an Australian study by Nanayakkara, Pease, Ranasinhaet al10 was 29% according to the Brief Case find for Depression (BCD). Khaledi, Haghighatdoost, Feizi, Aminorroaya2 in their meta-analysis study including 248 studies with 83,020,812 diabetic patients around the world presented that the global prevalence of depression in patients with type 2 diabetes is 28%. In this meta-analysis, Europe (24%) and Africa (27%) have a lower depression prevalence than Australia (29%) and Asia (32%). The criteria used to determine depression in the studies varied according to the usage of different instruments such as BDI, PHQ-9, Center for Epidemiologic Studies Depression Scale (CESD), Hospital Anxiety and Depression Scale (HADS), DASS-21.2 Thus, the difference in the prevalence rate of co-morbid depression in type 2 diabetes mellitus patients among the studies could be explained by using different assessments of depression and even with the same instrument but different cutoff scores for depression.
Our study results showed that the prevalence of depression was significantly higher in patients under 60 years of age (34.1%) compared to those ≥60 years old (16.4%). This difference was also still present in multivariate logistic regression (OR=2.64, 95% CI: 1.38–5.03, p<0.01). Our study findings were consistent with those reported in the literature. Katon, Pedersen, Ribeet al11 studied on 2,454,532 patients with type 2 diabetes mellitus and follow up in many years, the results showed that the rate of depression was higher in people under 65 years compared with people from and above 65 years. In another study, Tran12 also found that younger age (under 60 years) is predictor of depression in type 2 diabetes mellitus patients. However, in a meta-analysis study, Roy, Lloyd1 reported that the association between age and depression with type 2 diabetes mellitus was uncertain. Several studies revealed that depression occurred more often in patients under 60 years but others showed an inverse relationship.1 Younger age, which was one of the predictors of depression in type 2 diabetes mellitus, could be explained by the fact that younger people are less experienced when coping with difficult situations, have more negative influences in many dimensions of their daily life including marital status, working and social functions. These factors could all lead to depression. Besides, it is known that type 2 diabetes mellitus is chronic condition and last for a lifetime so if the younger people get disease the longer duration of illness and the more complications they have in their life. This thought would lead younger people to depression.
Evidence from other study points to poor economic status as significant predictors of depression in both the general population and diabetic patients.13,14 In univariate analysis in our study, depression was significantly associated with poor economic status (p=0.006) (Table 2). In multivariate logistic regression analysis, this risk factor remained significant (OR 2.8, 95% CI 1.32–5.95, p<0.01) (Table 5).
Unemployment is also a risk factor of depression in several studies. Unemployment was attributed to depression by causing poor economic status, lowering self-esteem. However, we found that patients with an unstable job had a higher rate of depression than those with unemployment (34.5% vs 17.7%, p<0.05) in single-variate analysis. This difference was also found in multivariate logistic regression (OR=2.45, 95% CI: 1.21–4.95, p<0.05). We conducted the study in diabetic inpatients so the patients with unstable jobs, they were likely to lose their jobs during hospitalization, making it difficult for them to find work again after discharge. Besides, those were often combined with poor economic status in our study. These would result in them more likely to succumb to depression. Correlation of having stressful events during the past year with depression in patients with type 2 diabetes mellitus was also found in our study (OR=11.18, 95% CI: 2.18–57.33, p<0.01). Stressful events could provoke and cause relapses of depression in both the general and diabetic population. Lee, Brazeal, Choiet al15 studied 421 patients with type 2 diabetes mellitus and revealed that the patients with stressful events had higher prevalence of depression than those who had no stressful events. Bădescu, Tătaru, Kobylinskaet al16 also demonstrated similar results. Our study also showed that there were no significant differences between the depressive versus non-depressive groups in gender, marital status, religion, ethnicity, place of living and level of education (p>0.05). Adherence to treatment of diabetes in both dietary and medication was a protective factor in several studies.10,17 Treatment adherence treatment improved blood glucose control, reduced diabetic complications, leading to increase quality of life and lower expenditure for health care. We presented that the prevalence of depression in patients with poor adherence to diabetic treatment was significantly higher than that prevalence in patients with good adherence to diabetic treatment (OR=2.44, 95% CI: 1.07–5.53, p<0.05). Practicing and doing exercise and other physical activities were good to the health of normal people and people with type 2 diabetes mellitus. Our study findings showed that duration of physical activities less than 3 days had the highest of prevalence of depression in the participants (50% vs 22.9% and 18.2% for rest two groups) (Table 4) (OR=4.48, 95% CI: 1.80–11.13, p<0.01). Doing physical activities heavily was associated with more than a 3-fold increase in the risk of depression in our study (OR=3.88, 95% CI: 1.63–9.24, p<0.01). Doing physical activities heavily could make patients with chronic disease including diabetes more fatigue, worsen complications or comorbidities especially cardiovascular diseases. So these negative influences could lead patients to depression. The combination of people doing physical activities heavily, poor economic status, and having an unstable job all provoked the onset of depression. BMI, duration of diabetes, glycemic control, co-morbid diseases/complications, smoking cigarettes and drinking alcohol had no association with depression in the patient population.
There were limitations to our study. First, we did not use random sample selection but instead used a convenient sample selection technique. Second, some potential variables that could be associated with depression may involve the type and route of medication administration. Finally, we only used the PHQ-9 questionnaire to determine the prevalence of depression as a screening tool and did not use other clinical criteria to definitively diagnose depression.
Conclusion
The prevalence of depression is high in patients with type 2 diabetes mellitus. Multivariate logistic regression analysis indicated several factors associated with depression in participants including age under 60 years, poor economic status, unstable or part-time job, having stress during the past year, without/poor treatment adherence with type 2 diabetes mellitus, doing heavy physical activity, or doing physical activity less than three days per week.
Given the high prevalence of depression among patients with type 2 diabetes mellitus, awareness of depression in type 2 diabetes mellitus should be raised among endocrinologists. Screening patients with type 2 diabetes mellitus for co-morbid depression and its risk factors is also recommended.
Acknowledgments
The authors wish to thank the patients and the hospital staff who participated and facilitated us in the study.
Funding
This research was supported by Hue University (grant number: DHH-04-80).
Disclosure
The authors have no conflict of interest to declare.
References
1. Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142:S8–S21. doi:10.1016/S0165-0327(12)70004-6
2. Khaledi M, Haghighatdoost F, Feizi A, Aminorroaya A. The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. 2019;56(6):631–650.
3. Alajmani DSA, Alkaabi AM, Alhosani MW, et al. Prevalence of undiagnosed depression in patients with type 2 diabetes. Front Endocrinol (Lausanne). 2019;10:259. doi:10.3389/fendo.2019.00259
4. Dang T. Nghiên cứu tỷ lệ trầm cảm và một số yếu tố liên quan ở bệnh nhân đái tháo đường típ 2 điều trị ngoại trú tại trung tâm nội tiết tỉnh Quảng Ngãi năm 2019 [Thesis for the specialist level two program]. Hue, Vietnam: Hue University Of Medicine and Pharmacy; 2019.
5. Katon WJ, Young BA, Russo J, et al. Association of depression with increased risk of severe hypoglycemic episodes in patients with diabetes. Ann Fam Med. 2013;11(3):245–250. doi:10.1370/afm.1501
6. Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
7. Dang DT. Đánh giá sơ bộ giá trị của bảng hỏi sức khỏe bệnh nhân (PHQ –9) trong sàng lọc Bệnh nhân Trầm cảm. J Pract Med. 2011;774(7):173–176.
8. Tam NT. Assessing validity of patient health questionnaire- 9 in detecting depression in community setting in Khanh Hoa and Danang provinces. PHQ-9 Valid Rep. 2009;1–25.
9. Zhang W, Xu H, Zhao S, et al. Prevalence and influencing factors of co-morbid depression in patients with type 2 diabetes mellitus: a general hospital based study. Diabetol Metab Syndr. 2015;7(1):60. doi:10.1186/s13098-015-0053-0
10. Nanayakkara N, Pease A, Ranasinha S, et al. Depression and diabetes distress in adults with type 2 diabetes: results from the Australian national diabetes audit (ANDA) 2016. Sci Rep. 2018;8(1):7846. doi:10.1038/s41598-018-26138-5
11. Katon W, Pedersen HS, Ribe AR, et al. Effect of depression and diabetes mellitus on the risk for dementia: a national population-based cohort study. JAMA Psychiatry. 2015;72(6):612–619. doi:10.1001/jamapsychiatry.2015.0082
12. Tran THA. Nghiên cứu đặc điểm lâm sàng trầm cảm và một số yếu tố liên quan ở bệnh nhân đái tháo đường type 2 [PhD thesis]. Hanoi, Vietnam: Hanoi Medical University; 2018.
13. Park CY, Kim SY, Gil JW, Park MH, Park J-H, Kim Y. Depression among korean adults with type 2 diabetes mellitus: ansan-community-based epidemiological study. Osong Public Health Res Perspect. 2015;6(4):224–232. doi:10.1016/j.phrp.2015.05.004
14. Camara A, Baldé NM, Enoru S, Bangoura JS, Sobngwi E, Bonnet F. Prevalence of anxiety and depression among diabetic African patients in Guinea: association with HbA1c levels. Diabetes Metab. 2015;41(1):62–68. doi:10.1016/j.diabet.2014.04.007
15. Lee J, Brazeal M, Choi H, Rehner TA, McLeod ST, Jacobs CM. Physical and psychosocial factors associated with depression among adults with type 2 diabetes mellitus at a federally qualified healthcare center. Soc Work Health Care. 2018;57(10):834–850. doi:10.1080/00981389.2018.1508113
16. Bădescu SV, Tătaru C, Kobylinska L, et al. The association between diabetes mellitus and depression. J Med Life. 2016;9(2):120–125.
17. Mendes R, Martins S, Fernandes L. Adherence to medication, physical activity and diet in older adults with diabetes: its association with cognition, anxiety and depression. J Clin Med Res. 2019;11(8):583–592. doi:10.14740/jocmr3894
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.