Back to Journals » Clinical Ophthalmology » Volume 14
Defocus Curve and Patient Satisfaction with a New Extended Depth of Focus Toric Intraocular Lens Targeted for Binocular Emmetropia or Slight Myopia in the Non-Dominant Eye
Authors Sandoval HP, Lane S , Slade SG, Donnenfeld ED , Potvin R , Solomon KD
Received 26 January 2020
Accepted for publication 12 May 2020
Published 26 June 2020 Volume 2020:14 Pages 1791—1798
DOI https://doi.org/10.2147/OPTH.S247333
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Helga P Sandoval,1 Stephen Lane,2 Stephen G Slade,3 Eric D Donnenfeld,4 Richard Potvin,5 Kerry D Solomon1
1Carolina Eyecare Physicians, LLC, Mt. Pleasant, SC, USA; 2Associated Eye Care, Stillwater, MN, USA; 3Slade & Baker Vision, Houston, TX, USA; 4Ophthalmic Consultants of Long Island, Long Island, NY, USA; 5Science in Vision, Akron, NY, USA
Correspondence: Kerry D Solomon
Carolina Eyecare Physicians, LLC, 1101 Clarity Road, Suite 100, Mt Pleasant, SC 29464, USA
Email [email protected]
Purpose: To evaluate the defocus curve and patient satisfaction after implantation of an extended depth of focus (EDOF) toric IOL when both eyes were targeted for emmetropia and when the non-dominant eye was targeted for mini monovision (− 0.50D).
Methods: A prospective unmasked randomized clinical trial in three clinical practices in the USA. Subjects presenting for routine cataract surgery were assigned to one of two groups, both receiving bilateral toric EDOF lenses. One group had the non-dominant eye targeted for slight myopia (− 0.50D). Measures of interest were the postoperative defocus curve and reported patient satisfaction and visual disturbances.
Results: Questionnaire and defocus curve data were available from 37 subjects in the Emmetropia group, while the mini monovision group included questionnaire data from 39 subjects and valid defocus curve data from 14 subjects. Mini monovision subjects had significantly better VA (a half line to a line better, p < 0.05), from a defocus of − 1.50 D to − 3.00 D. Reported spectacle wear and satisfaction were not significantly different between groups at any distance, but more patients in the mini monovision group reported the ability to function comfortably without glasses at near and overall (near p = 0.02, overall p < 0.01). Halos and starbursts were the two phenomena reported most often for both groups, with reported starbursts slightly more common in the mini monovision group.
Conclusions: A slightly myopic correction in the non-dominant eye improved binocular near vision by 0.5 to 1.0 lines based on defocus curve data. Patients reported better functional vision, but with a slight increase in reported starbursts in the mini monovision group.
Keywords: symfony, extended depth of focus, intraocular lens, cataract surgery, monovision
Introduction
One of the biggest determinants of patient satisfaction after refractive cataract surgery is the ability to see clearly and comfortably at the desired viewing distances. A large segment of the population presenting for cataract surgery suffers from astigmatism1 so the ideal presbyopia-correcting intraocular lens (IOL) for these patients is a presbyopia-correcting toric IOL. Most diffractive multifocal toric intraocular lenses split incoming light into different foci, to enable good vision at different distances. However, this splitting can also increase glare and haloes,2 reducing patient satisfaction. de Vries et al3 reported that dissatisfaction after multifocal lens implantation was mostly related to blurred vision and photic phenomena. Mester et al4 noted that of the 183 patients examined, there was a strong correlation between satisfaction and residual refraction, contrast sensitivity and photic phenomena. Wang et al5 systematically evaluated refractive and diffractive multifocal lenses as well as monovision lens options and noted that multifocal lenses reduced contrast sensitivity and increased dysphotopsia while monovision and accommodative lenses did not provide sufficient independence from glasses. As such, a new approach to provide comfortable and clear vision remains desirable.
A relatively newer lens design uses extended depth of focus (EDOF) as opposed to light splitting to enhance viewing at different distances; one of these lenses is the Tecnis Symfony® lens (Johnson & Johnson Vision, Santa Ana, CA). This EDOF IOL was designed to provide good vision at all distances while providing high patient satisfaction by eliminating some of the visual symptoms associated with multifocal lenses. When compared to a monofocal lens, the Symfony EDOF IOL provided significantly better intermediate and near visual acuities with similar contrast sensitivity and optical quality at distance.6 Adequate near vision is a recognized concern, but to help improve near visual acuity (VA) with the lens the non-dominant eye may be targeted for slight residual myopia. A large study of 112 patients had the non-dominant eye with a mean target of −0.75D and the results showed a low rate of photic phenomena (4–13%) with 92% reporting to be satisfied with their EDOF lens selection.7 Similarly, those receiving EDOF lenses with a plano target in both eyes (285 patients) noted a low rate of photic phenomena (2–8%) and a high rate of satisfaction (95%).7 Subgroup analysis of the Concerto study by Cochener et al concluded that −0.75D was a good target for the non-dominant eye, providing one of the highest reports of patient satisfaction.8
Larger studies9,10 looking at defocus curves with bifocal toric lenses have shown a sharp drop in visual acuity at the intermediate range, which would not be expected with an EDOF lens. An EDOF lens is also likely to provide slightly better distance and intermediate vision when compared to trifocal lenses. The defocus curve with an EDOF IOL when the non-dominant eye was targeted for −0.75D demonstrated 20/20 or better visual acuity from distance to 67 cm, 20/25 visual acuity at 50 cm and 20/32 visual acuity at 40cm.11 Two large studies12,13 have examined the defocus curves of trifocal toric lenses and a study by Monaco et al14 compared the defocus curves of a trifocal lens with an EDOF lens and a monofocal lens. The results of Monaco et al’s study demonstrated improved vision at 67 cm and 40cm using the trifocal lens while distance and intermediate vision at 50cm remained similar between the EDOF and trifocal lens; both multifocal lenses provided similar distance vision to the monofocal lens group.14 Monaco et al14 set a target of emmetropia for both eyes in the EDOF group, which likely explains some of the drop in near acuity when compared to the trifocal lens.
The purpose of the current study was to evaluate the defocus curve and the patient satisfaction after bilateral implantation of an EDOF toric IOL when both eyes were targeted for emmetropia and when the non-dominant eye was targeted for mini monovision (−0.50D) in patients with astigmatism undergoing routine cataract surgery.
Methods
A multi-site, unmasked, randomized clinical trial was designed to evaluate the clinical outcomes associated with using a toric EDOF lens binocularly, but in two different modalities. The first involved targeting both eyes for emmetropia, while the second involved targeting the non-dominant eye for a residual refraction of −0.50D (termed “mini monovision” for the purposes of this manuscript). The study was approved by an institutional review board (Salus IRB, Austin, TX, USA) and registered with clinicaltrials.gov (record NCT03082599). Sample size calculations suggested 55 subjects in each group would be sufficient to detect a 1-line (0.1 logMAR) difference in visual acuity. The study was conducted adhering to good clinical practice and in a manner consistent with the tenets of the Declaration of Helsinki.
Subjects over 40 years of age who required a toric lens presenting for routine cataract surgery in both eyes, with no pathology that might affect postoperative visual outcomes and a potential visual acuity of at least 20/32 (0.2 logMAR), were considered for enrollment. Exclusion criteria included uncontrolled diabetes, severe dry eye, prior refractive or cataract surgery and any plans for an adjunct procedure (eg, insertion of a surgical glaucoma device at the time of cataract surgery). No vulnerable subject populations were enrolled. All eligible subjects reviewed and signed an approved informed consent and were randomized to one of two groups. The Emmetropia group was targeted for emmetropia in both eyes. The Mini monovision group was targeted for emmetropia in the dominant eye and −0.50D in the non-dominant eye.
Preoperative evaluation included uncorrected and best-corrected visual acuity (UCVA and BCVA, respectively), along with the clinic’s standard cataract evaluation procedures, including surgical planning methods and formulas. Surgery was performed using the physician’s standard procedures, including femtosecond lasers systems if applicable. Intraoperative aberrometry (IA) was used only to check lens alignment; no changes to lens sphere or cylinder power were allowed based on IA. Use of IA or a femtosecond laser system was recorded. Any subjects experiencing any intraoperative adverse event were documented and discontinued from the study; they were followed with the clinic’s usual standard of care.
Postoperative evaluation was performed at 1 day, 1 week, 1 month and 3 months. Clinical outcomes data included slit lamp examination, manifest refraction and visual acuity at distance, intermediate (60cm) and near (40cm). At the 3-month visit a binocular defocus curve was generated and two questionnaires were administered. The patient reported spectacle independence questionnaire (PRSIQ)15 was used to determine subjects’ need for spectacles or contact lenses and their satisfaction with vision at various distances. Visual symptoms were reported using a proprietary patient-reported visual symptom questionnaire. Adverse events and/or device deficiencies were also recorded.
Results reported here are limited to the defocus curve and questionnaire data collected at the 3-month visit. The defocus curve for the Emmetropia group was collected with both eyes corrected for the appropriate chart distance (4m). In the Mini monovision group, the dominant eye was corrected for the chart distance and the non-dominant eye was left −0.50D more myopic.
Data were collected on appropriate case report forms and collated in MS Excel, then imported into an Access database for data checking and preliminary analysis (both Microsoft Corp., Redmond, WA, USA). Statistical analyses were performed using the Statistica data analysis software system, version 12 (TIBCO Software Inc., Palo Alto, CA, USA). Parametric comparisons between groups were made using analysis of variance (ANOVA) and non-parametric data were compared using the Chi-squared test.
Deidentified data and all other study documentation will not be made available for sharing.
Results
Table 1 summarizes the demographics of the Emmetropia and Mini monovision groups analyzed here. The groups were similar with regard to subject age and sex. Preoperative refractions were slightly more myopic in the Mini monovision group, but average corneal astigmatism and average keratometry were similar. Questionnaire data were available from 37 subjects in the Emmetropia group and 39 subjects in the Mini monovision group at 3 months postoperative. There were 37 subjects in the Emmetropia group and 14 subjects in the Mini monovision group with binocular defocus curves collected.
 |
Table 1 Subject Demographics |
Table 2 contains the summary refractive and distance visual acuity data for the two groups at 3 months postoperative. There was (as expected) a significant difference in the residual spherical equivalent refraction between the dominant and non-dominant Mini monovision eyes (+0.05 D vs −0.24 D, p < 0.001). The magnitude of residual cylinder was not statistically significantly different between groups; mean residual refractive astigmatism was about 0.25D in both groups. Mean residual refractive astigmatism was 0.50D or lower in 92% of eyes (72/78) in the Mini monovision group and 95% of eyes (70/74) in the Emmetropia group at 3 months postoperative. No eye had more than 1.0D of refractive cylinder at that time. The binocular uncorrected distance visual acuity was better than 0.0 logMAR (20/20) for both groups, with no statistically significant difference between groups (p = 0.34).
 |
Table 2 Refractive Status and Distance Visual Acuity |
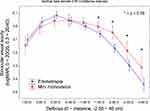
Figure 1 shows the binocular defocus curves for the two groups three months postoperative. These were based on the best-corrected distance vision in both eyes for the Emmetropia group. For the Mini monovision group, the dominant eye was best-corrected for distance vision and the non-dominant eye was best-corrected for distance vision plus 0.5D. There was no statistically significant difference in the binocular VA from a defocus of +1.00 D to −1.00 D. However, from a defocus of −1.50 D to −3.00 D, the Mini monovision group had significantly better binocular VA; the better VA ranged from a half line at −1.50D (corresponding to a reading distance of about 66 cm) to a full line from −2.00D to −3.00 (corresponding to a reading distance range of 50 to 33 cm). The pattern evident from 0.00 to −2.50 is a “rightward shift” of the Mini monovision curve by 0.50D.
Figure 2 summarizes the findings of the PRSIQ measures of spectacle independence, showing A) reported independence from spectacles or contact lenses for working at different distances, B) the percentage of subjects wearing spectacles or contact lenses to see at different distances “all of the time” or “most of the time”, C) the percentage of subjects able to function comfortably “all of the time” or “most of the time” at different distances without spectacles or contact lenses and D) the percentage of subjects satisfied with their vision at different distances “all of the time” or “most of the time”. While somewhat more subjects in the Emmetropia group reported needing spectacles or contact lenses for intermediate and near vision, there was no statistically significant difference between the groups (Chi-squared test, intermediate p = 0.07, near p = 0.06). Similarly, there was a trend for subjects in the Emmetropia group to wear spectacles or contact lenses more often for near and intermediate work, but the differences were not statistically significant (Chi-squared test, intermediate p = 0.14, near p = 0.16). However, a statistically significantly higher percentage of patients in the Mini monovision group reported the ability to function comfortably without glasses or contact lenses at near and overall (Chi-squared test, near p = 0.02, overall p < 0.01). There were no statistically significant differences in satisfaction between groups at any distance or overall.
 |
Figure 2 Need for spectacles (A), wearing patterns (B), functional vision (C) and satisfaction (D) by group. |
The frequencies of various visual disturbances reported as “Always” or “Often” seen on the PRVSQ questionnaire are shown in Figure 3. Halos and starbursts were the two phenomena reported most often for both groups. While the percentage of subjects reporting halos and starbursts was slightly higher in the Mini monovision group, the differences were not statistically significant. Fewer than 10% of subjects in both groups reported glare seen “Always” or “Often”.
 |
Figure 3 Reported frequency of visual disturbances “Always” or “Often” seen, by group. |
Figure 4 shows the level of severity that subjects assigned to the 4 most commonly reported visual disturbances in Figure 3: A) Halos, B) Starbursts, C) Poor mesopic vision and D) Sensitivity to light. The distributions are generally similar, except in the case of Starbursts. More Mini monovision subjects reported moderately to extremely bothersome Starbursts relative to the Emmetropia group, though the difference was not statistically significant (Chi-squared test, p = 0.10).
 |
Figure 4 Severity of reported visual disturbances by group (A) halos, (B ) starbursts, (C ) poor mesopic vision and (D) sensitivity to light. |
Discussion
The current study looked at objective and subjective outcomes three months postoperative, after implantation with a toric EDOF lens in two groups of subjects based on target refractions. The refractive and distance visual acuity results in Table 2 indicate that differences in the defocus curve, satisfaction and visual disturbances are unlikely to be related to differences in residual refractive error (except where intended, with the Mini monovision group) or postoperative uncorrected visual acuity. A detailed review of the acuity and refractive results in this group has been published in an earlier manuscript.16
The defocus curve (Figure 1) demonstrated that the Mini monovision group provided better intermediate and near VA than the emmetropia group. The result for the emmetropia group is relatively consistent with the defocus curve result reported by Monaco et al except at distance, 67 cm and 33 cm.14 When compared to the current study, Monaco et al14 report 1-line better VA at 33cm, 0.5-line worse VA at distance and 67 cm; the reason for the difference is unclear as Monaco used the same lens with a target of emmetropia. Ganesh et al11 provided a defocus curve of the same EDOF lens when the target was −0.75D in the non-dominant eye. When compared to the Mini monovision group from the current study, the Ganesh results show worse VA at 50 cm by 0.5 line but results are otherwise reasonably consistent with those from the current study.
Compared to other multifocal toric lenses, the current lens provided similar distance VA.9,12 In a large study of 142 patients, mean intermediate vision of 0.2 logMAR at best was reported for a diffractive bifocal toric lens.9 Mean intermediate VA in the current study was better than 0.2 logMAR in the Emmetropia group and never fell below 0.1 logMAR in the Mini monovision group.9 At near, the bifocal lens in the previous study provided comparable vision to the Mini monovision group at 40 cm, but better near VA at 33 cm relative to both the mini monovision and emmetropia groups in the current study. When compared to one diffractive-refractive trifocal toric lens, the Mini monovision and Emmetropia groups provided at least 1-line better VA at 67 cm. At 50 cm the Emmetropia group provided similar VA, while the Mini monovision group provided a VA 1.5 lines better.12 At 40 cm, the Mini monovision group provided similar VA to the diffractive-refractive trifocal toric lens.12 Monaco et al14 also compared the results of this EDOF lens targeted for emmetropia with another trifocal lens and noted that the trifocal lens had better VA at 67 cm, 40 cm and 33 cm. The mini monovision results here were better than the EDOF results reported by Monaco et al for emmetropia.14 Near vision in the Mini monovision group was similar to that reported for the trifocal lens, but better at 67 cm by about 0.5 lines and better at 50 cm by 1.0 to 1.5 lines. It should be noted that while comparisons with previous studies provide context, results between studies will vary because of differences in the population and possible differences in testing methods/conditions.
None of the patients in the current study reported needing glasses for distance and only about 3% and 14% reported needing correction for intermediate in the Mini monovision and Emmetropia groups, respectively. At near, about 60% of subjects in the Mini monovision group and 80% in the Emmetropia group reported needing glasses at some time for near vision, though reported wear was generally “some of the time” or less. Only 8% of mini monovision subjects and 21% of Emmetropia subjects reported wearing spectacles for near all of the time. In a large study using the same EDOF lens, 16% and 24% reported wearing a correction at intermediate and near, respectively, in a group targeted for emmetropia, while 8% and 14% reported wearing spectacles for near and intermediate, respectively, in the Mini monovision group targeted around −0.50D.8 These results are reasonably consistent with those in the current study.8
Satisfaction results here were slightly better for the Mini monovision group at intermediate and near. Cochener et al,7 who studied the same lens with emmetropia and mini monovision targets, noted similar satisfaction results to the current study at distance and near. However, they noted slightly higher satisfaction at intermediate in the emmetropia group compared to the monovision group. The difference may be due to the fact that the mini monovision target in the previous study was −0.75D, slightly higher than the −0.50D in the current study.
Visual disturbances were relatively similar in both groups with halos and starbursts being the most often reported. Cochener et al7 reported more halos and glare using the same lens and groupings as the current study, with glare more often reported in the emmetropia group than the Mini monovision group. Similar to results in the current study, Cochener et al7 noted slightly greater reports of halos and starbursts in the Mini monovision group when compared to the emmetropia group.
In conclusion, the current study indicates that when utilizing an extended range of vision toric IOL, targeting slight myopia in the non-dominant eye maintains binocular distance VA while improving intermediate and near VA based on defocus curve findings. This resulted in greater spectacle independence at intermediate and near as well as more comfortable and functional vision at those distances. The overall reported need for glasses, and overall satisfaction, did not appear to be different. There were slightly greater reports of visual disturbances, but this did not seem to impede visual performance or satisfaction.
Acknowledgments
Sarah Y. Makari, OD is a consultant to Science in Vision who received compensation for writing assistance in preparation of the manuscript. The results reported here were collected at 3 clinical practices (Solomon, Lane, Slade) in the USA. Subsets of the data were presented at the annual ASCRS meeting in Washington, DC, April 14-17, 2018.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Helga Sandoval, Stephen Lane, Stephen Slade, Richard Potvin, and Kerry D. Solomon. The first draft of the manuscript was written by Richard Potvin and Helga Sandoval and all authors revised and commented on previous versions of the manuscript, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Helga P Sandoval reports grants from Johnson and Johnson Vision, during the conduct of the study; grants from Alcon, Lenstec, and Johnson and Johnson Vision, outside the submitted work. Stephen S. Lane was a consultant to Alcon, B&L, ClarVista, Ivantis, I-Veena, Kala, Mati, Ocular Therapeutix, Omeros, PowerVision, PRN, RPS, Shire, TearScieince, TearLab, VisionCare during the study. He is now Alcon’s CMO and has no other financial interests at the present time. Stephen Slade, MD is a consultant to Alcon, Allotex, Avedro, B&L, CorneaGen, EyeBrain, Eyegate, Glaukos, Johnson and Johnson Vision, LensTec, Occumetrics, Omega Ophthalmics, Presbyopia Therapies RxSight, Surgilum, Zeiss. Eric D. Donnenfeld is a consultant for Acufocus, Allergan, Alcon, AMO, Aquesys, Bausch & Lomb, CRST, Beaver-visitec Elenza, Glaukos, Icon Biosciences, Kala, Katena Lacripen, Mati Pharmaceuticals, Merck, Mimetogen, Novabay, Novaliq, Odyssey, Omega Ophthalmics, Pfizer, Ocuhub, Omeros, PRN, RPS, Shire, Strathspey Crown, Tearlab, TLC Laser Centers, TrueVision, Versant Ventures, and Zeiss. Richard Potvin is a consultant to Alcon Laboratories, Inc. Kerry D. Solomon is a consultant for Alcon Laboratories, Allergan, Aquesys, Bausch and Lomb, Clarvista Medical, Glaukos, Icon Bioscience, Imprimis, Integrity Digital Solutions, Johnson & Johnson Vision, Kala Pharmaceuticals, Lenstec, Mati Therapeutics, Octane Visionary VC Fund, Ocuhub, Omeros Corporation, Pogotec, PRN, Tearlab, Versuant. The authors have no proprietary or financial interest in any product mentioned herein. The authors report no other conflicts of interest in this work.
References
1. Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal stigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36(9):1479–1485. doi:10.1016/j.jcrs.2010.02.025
2. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12:CD003169. doi:10.1002/14651858.CD003091.pub4
3. de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011;37(5):859–865. doi:10.1016/j.jcrs.2010.11.032
4. Mester U, Vaterrodt T, Goes F, et al. Impact of personality characteristics on patient satisfaction after multifocal intraocular lens implantation: results from the “happy patient study”. J Refract Surg. 2014;30(10):674–678. doi:10.3928/1081597X-20140903-05
5. Wang SY, Stem MS, Oren G, Shtein R, Lichter PR. Patient-centered and visual quality outcomes of premium cataract surgery: a systematic review. Eur J Ophthalmol. 2017;27(4):387–401. doi:10.5301/ejo.5000978
6. Pedrotti E, Bruni E, Bonacci E, Badalamenti R, Mastropasqua R, Marchini G. Comparative analysis of the clinical outcomes with a monofocal and an extended range of vision intraocular lens. J Refract Surg. 2016;32(7):436–442. doi:10.3928/1081597X-20160428-06
7. Cochener B; Concerto Study Group. Clinical outcomes of a new extended range of vision intraocular lens: international multicenter concerto study. J Cataract Refract Surg. 2016;42(9):1268–1275. doi:10.1016/j.jcrs.2016.06.033
8. Cochener B. Influence of the level of monovision on visual outcome with an extended range of vision intraocular lens. Clin Ophthalmol. 2018;12:2305–2312. doi:10.2147/OPTH.S184712
9. Bellucci R, Bauer NJ, Daya SM, et al.; Lisa Toric Study Group. Visual acuity and refraction with a diffractive multifocal toric intraocular lens. J Cataract Refract Surg. 2013;39(10):1507–1518. doi:10.1016/j.jcrs.2013.04.036
10. Chaves MA, Hida WT, Tzeliks PF, et al. Comparative study on optical performance and visual outcomes between two diffractive multifocal lenses: AMO Tecnis ® ZMB00 and AcrySof ® IQ ReSTOR ® Multifocal IOL SN6AD1. Arq Bras Oftalmol. 2016;79(3):171–176. doi:10.5935/0004-2749.20160050
11. Ganesh S, Brar S, Pawar A, Relekar KJ. Visual and refractive outcomes following bilateral implantation of extended range of vision intraocular lens with micromonovision. J Ophthalmol. 2018;2018:7321794. doi:10.1155/2018/7321794
12. Piovella M, Colonval S, Kapp A, Reiter J, Van Cauwenberge F, Alfonso J. Patient outcomes following implantation with a trifocal toric IOL: twelve-month prospective multicentre study. Eye (Lond). 2019;33(1):144–153. doi:10.1038/s41433-018-0076-5
13. García-Pérez JL, Gros-Otero J, Sánchez-Ramos C, Blázquez V, Contreras I. Short term visual outcomes of a new trifocal intraocular lens. BMC Ophthalmol. 2017;17(1):72. doi:10.1186/s12886-017-0462-y
14. Monaco G, Gari M, Di Censo F, Poscia A, Ruggi G, Scialdone A. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43(6):737–747. doi:10.1016/j.jcrs.2017.03.037
15. Morlock R, Wirth RJ, Tally SR, Garufis C, Heichel CWD. Patient-reported spectacle independence questionnaire (PRSIQ): development and validation. Am J Ophthalmol. 2017;178:101–114. doi:10.1016/j.ajo.2017.03.018
16. Sandoval HP, Lane S, Slade S, Potvin R, Donnenfeld ED, Solomon KD. Extended depth-of-focus toric intraocular lens targeted for binocular emmetropia or slight myopia in the nondominant eye: visual and refractive clinical outcomes. J Cataract Refract Surg. 2019;45(10):1398–1403. doi:10.1016/j.jcrs.2019.05.019
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.