Back to Journals » Nature and Science of Sleep » Volume 15
Daytime Hypercapnia Impairs Working Memory in Young and Middle-Aged Patients with Obstructive Sleep Apnea Hypopnea Syndrome
Authors Wu HM, Wang ZJ , Cheng CH, Su T, Wang J, Li YZ , Wang QJ, Han F, Chen R
Received 20 November 2022
Accepted for publication 5 May 2023
Published 17 May 2023 Volume 2023:15 Pages 363—373
DOI https://doi.org/10.2147/NSS.S398440
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Hua-Man Wu,1,2,* Zhi-Jun Wang,1,* Chao-Hong Cheng,1 Tong Su,1 Jing Wang,1 Ye-Zhou Li,3 Qiao-Jun Wang,4 Fei Han,4 Rui Chen1,4
1Department of Respiratory, the Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu, People’s Republic of China; 2Department of Respiratory and Critical Care Medicine, Zigong First People’s Hospital, Zigong, Sichuan, People’s Republic of China; 3School of Medicine, the University of Manchester, Manchester, UK; 4Department of Sleeping Center, the Second Affiliated Hospital of Soochow University, Suzhou, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Rui Chen, Department of Respiratory/Department of Sleeping Center, the Second Affiliated Hospital of Soochow University, 1055 Sanxiang Road, Suzhou, 215004, People’s Republic of China, Tel +86(0512)67784857, Email [email protected]
Purpose: Obstructive sleep apnea hypopnea syndrome (OSAHS) can lead to cognitive impairment, though few studies have so far examined hypercapnia as its causal mechanism, due to the invasive nature of conventional arterial CO2 measurement. The study aims to investigate the effects of daytime hypercapnia on working memory in young and middle-aged patients with OSAHS.
Patients and Methods: This prospective study screened 218 patients and eventually recruited 131 patients (aged 25– 60 years) with polysomnography (PSG)-diagnosed OSAHS. Using a cut-off of 45mmHg daytime transcutaneous partial pressure of carbon dioxide (PtcCO2), 86 patients were assigned into the normocapnic group and 45 patients into the hypercapnic group. Working memory was evaluated using the Digit Span Backward Test (DSB) and the Cambridge Neuropsychological Test Automated Battery.
Results: Compared with the normocapnic group, the hypercapnic group performed worse in verbal, visual, and spatial working memory tasks. PtcCO2≥ 45mmHg was an independent predictor for lower DSB scores (OR=4.057), lower accuracy in the immediate Pattern Recognition Memory (OR=2.600), delayed Pattern Recognition Memory (OR=2.766) and Spatial Recognition Memory (OR=2.722) tasks, lower Spatial Span scores (OR=4.795), and more between errors in the Spatial Working Memory task (OR=2.734 and 2.558, respectively). Notably, PSG indicators of hypoxia and sleep fragmentation did not predict task performance.
Conclusion: Hypercapnia may be plays an important role in working memory impairment in patients with OSAHS, perhaps more so than hypoxia and sleep fragmentation. Routine CO2 monitoring in these patients could prove of utility in clinical practices.
Keywords: hypercapnia, obstructive, sleep apnea, working memory
Plain Language Summary
It has been suggested that cognitive impairment in obstructive sleep apnea hypopnea syndrome (OSAHS) patients is caused by nocturnal intermittent hypoxia and sleep fragmentation. Few studies have investigated the effect of hypercapnia on cognitive function in OSAHS patients. Thus, the contributary factors to cognitive impairment in OSAHS patients remain to be elucidated. This study shown that hypercapnia plays an important role in working memory impairment in OSAHS patients. Clinically, this provides insights that routine CO2 monitoring in these patients could prove of utility in clinical practices and future research should place an equal emphasis on the hypercapnia-mediated processes alongside those of hypoxia and sleep fragmentation when studying the cognitive function of OSAHS patients.
Introduction
Obstructive sleep apnea-hypopnea syndrome (OSAHS) induces nocturnal intermittent hypoxia and hypercapnia due to apnea and hypopnea caused by repeated airway collapse during sleep. The prevalence of OSAHS is increasing year by year, from 2% to 4% in the 1990s to the current 14% to 55%, and can be as high as 84% in the elderly.1,2 Many studies reported cognitive deficits in patients with OSAHS, mainly manifested by inattention, and impaired memory and executive function which reduces learning and working efficiency, affects interpersonal communication and quality of life, and increases the incidence of traffic accidents.3–5 As a result, cognitive impairment caused by OSAHS places a heavy effect on the patients’ families and the society.
The impact of OSAHS on cognitive impairment has been a subject of interest among researchers. In a model proposed by A. Baddeley working memory was hypothesized as a limited capacity temporary memory system for information storage and manipulation, which is the core of human advanced cognitive activities and facilitates the execution of complex cognitive tasks.6 Verbal working memory, visual memory, and spatial working memory are the important components of working memory. Various researches on working memory have been carried out,7–10 but there are few studies exploring the risk factors of working memory.
Traditionally, it has been suggested that cognitive impairment is caused by nocturnal intermittent hypoxia and sleep fragmentation.5,11–14 However, some large clinical trials failed to find a strong correlation between cognitive impairment and nocturnal intermittent hypoxia and sleep fragmentation in patients with OSAHS.15–17 Alternatively, hypercapnia has been shown to impair the working memory in rats,18 as well as the mental processing speed and logical memory in obese patients with OSAHS.19 However, the sample size in such studies tends to be limited due to the invasive CO2 measuring procedure. Thus, the contributary factors to cognitive impairment in Patients with OSAHS remain to be elucidated.
In this study, we employed the transcutaneous carbon dioxide monitoring technique to measure the blood carbon dioxide level, and adopted the Digit Span Backward Test (DSB) and Cambridge Neuropsychological Test Automated Battery (CANTAB) to assess the working memory in patients. We aim to investigate the effects of daytime hypercapnia on working memory (verbal working memory, visual memory, and spatial memory) in young and middle-aged patients with OSAHS.
Materials and Methods
Participants
This prospective study screened 218 patients with a primary complaint of snoring received at the sleep center of the Second Affiliated Hospital of Soochow University from January 2020 to November 2020. The OSAHS diagnosis was confirmed by polysomnography (PSG) with an apnea-hypopnea index (AHI) score ≥ 5.20 Participants were between 25 to 60 years old. All participants were right-handed and received a minimum of 9 years of education. We excluded patients who have previously received treatment for OSAHS or undergone similar neuropsychological tests. Individuals with color blindness or color weakness were excluded. We also excluded patients who took medications that might affect sleep structure and working memory (i.e benzodiazepines, opioids). Individuals with other sleep-disordered breathing (such as central sleep apnea-hypopnea syndrome and obesity hypoventilation syndrome), unstable circulatory or respiratory conditions, or neuropsychological diseases (including Parkinson’s disease, Alzheimer’s disease, anxiety, and depression) were excluded.
Trial Procedures
We collected basic information from participants including gender, age, years of education, body mass index (BMI), smoking history, drinking history, sleep-related complaints. Medical background questionnaires were administered to gather the clinical and medical history of participants.
All participants underwent full-night, supervised, laboratory-based video-PSG. The participants slept in a standard sound-attenuated room. The PSG was recorded for a minimum of 7 hours. Compumedice E Series 57 PSG monitoring system (Compumedics Company, Australia) was used for all signal acquisition. Six electroencephalogram (EEG) channels (F3/A2, F4/A1, C3/A2, C4/A1, O1/A2, O2/A1), bilateral electrooculograms, submental and bilateral anterior tibialis electromyograms, nasal and oronasal airflow (by using nasal pressure monitor and thermistor), snoring, chest and abdominal movements, body position, arterial oxygen saturation (by finger pulse oximetry), and electrocardiograms were included in polysomnographic recordings. Sleep stage classification and sleep-related respiratory analysis were scored by a registered technician according to the American Academy of Sleep Medicine (AASM) criteria.20 Apnea was defined as any airflow reduction greater than 90% that lasted longer than 10s. Hypopnea was defined as any airflow reduction greater than 30% that lasted longer than 10s and resulted in either oxyhemoglobin desaturation more than 3% or microarousal. The AHI was defined as the sum of the number of apnea and hypopnea per hour of sleep. Other measures included total sleep time (TST), sleep efficiency, sleep latency, oxygen desaturation index (ODI), percentage of total sleep time at SaO2 <90% (TS90), lowest oxygen saturation (LSaO2), average oxygen saturation (avgSaO2), arousal index (ArI), and proportions of each sleep stage.
Daytime PtcCO2 of participants was measured using the V-check mode of the transcutaneous capnometer (SenTec Company, Switzerland) with patients in sitting position prior to cognitive test and participants were not informed of the values of PtcCO2 until the end of the cognitive test. The transcutaneous sensor was placed slightly below the cheekbones. The capnometer was automatically calibrated for 15 minutes to obtain a stable signal, after which the average PtcCO2 was captured in a 5-minute window.
The working memory of participants was evaluated using the DSB and neuropsychological tasks including Pattern Recognition Memory (PRM), Spatial Recognition Memory (SRM), Spatial Span (SSP) and Spatial Working Memory (SWM) selected from the CANTAB in a quiet room before PSG. All participants completed neuropsychological tasks in the same order instructed by an experienced doctor.
DSB was used to evaluate the verbal working memory. The numbers were read to the participants at an even rate of 1 digit per second. The participants were then asked to list the digits in reverse order. The test starts from three-digit sequences and can increase to a maximum of 12 digits. The test stops when the participant produces two consecutive incorrect responses. Each repeat of the correct string of digits awards one point.
Visual memory was evaluated by PRM and SRM. PRM focuses on graphic visual memory. The patients were asked to remember twelve patterns shown individually in the presentation phase. In the immediate recognition phase, the patients were shown each of the learned patterns with a distractor and were asked to select the previously seen pattern. This recognition task was carried out again after a delay of 20 minutes. The outcome measures included response accuracy, delay, and total test duration. SRM focuses on spatial visual memory. In the presentation phase, patients were asked to remember the locations of a white square shown on the screen at five different locations consecutively. In the recognition phase, two squares appear simultaneously each time and the patients were tasked to select the one at one of the five previously seen locations, avoiding the other distractor square. The response accuracy and delay were recorded.
Spatial working memory was evaluated by SSP and SWM. SSP assesses memory capacity. A set of nine white squares were shown on the screen. In the presentation phase, the squares were colorized, one at a time, in a sequence from two to nine squares. The patients were tasked to reproduce the sequence in the recognition phase. The outcome measure is the longest sequence successfully recalled by the patients. SWM evaluates the patient’s ability to retain spatial information and to manipulate remembered items in working memory. A set of three to eight white squares were shown on the screen. The patients were told that a blue token was “hidden” in one of the white squares and they could look for it by clicking on the white squares. Once found, they need to click on the collection box to deposit the blue token. This then repeated with a new token spawned in any of the white boxes, except in the one where the previous token was found. The outcome measure included strategy score, i.e, the average number of clicks required to find each token, and between error, i.e, the number of times the patients revisited the square where the previous token was found, that is, where the current token could not be.
Statistical Analysis
The statistical analysis was performed using SPSS version 22 (SPSS Inc., Chicago, USA). Normality tests were conducted using the Kolmogorov–Smirnov test. Normally distributed variables were expressed as mean ± standard deviation (SD), and non-normally distributed variables were expressed as median and interquartile range (IQR). Numerical variables between two groups were compared using the unpaired t-test or the Mann–Whitney rank-sum test as appropriate. Categorical variables were expressed as numbers and percentages (%). Categorical variables were compared using the chi-square test, the chi-square test for continuous calibration, or Fisher’s exact test as appropriate. Binary logistic regression analysis was used to identify potential predictors of cognitive impairment in basic information, sleep-related complaints such as daytime sleepiness, morning fatigue and poor memory, PSG parameters and hypercapnia. All independent variables with P < 0.2 in the univariate analysis as well as basic demographic parameters (age, gender, BMI, years of education) were included in multivariate analysis. The threshold for statistical significance was set at P<0.05.
Results
A flow chart illustrating the participants recruitment and design is shown in Figure 1. A total of 131 participants that met the inclusion and exclusion criteria were divided into two groups according to daytime PtcCO2:21 86 were normocapnic with PtcCO2<45mmHg and 45 were hypercapnic with PtcCO2 ≥ 45mmHg.
Demographic and Clinical Parameters
Table 1 shows a cross-group comparison of demographic and clinical parameters. The hypercapnic group exhibits significantly higher daytime PtcCO2 (51.40 vs 39.20 mmHg, P<0.01) than that in the normocapnic group. Compared with the normocapnic group, complaints of morning fatigue and daytime sleepiness were more frequent in the hypercapnic group(P<0.05). There were no significant cross-group differences in other demographic and clinical parameters.
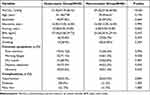 |
Table 1 Baseline and Clinical Data in the Hypercapnic and Normocapnic Groups |
Polysomnographic Parameters
Table 2 shows the polysomnographic parameters of the two groups. The proportion of stage N3 sleep in the hypercapnic group was lower than that in the normocapnic group (8.20% vs 12.70%, P<0.05). The AHI (46.80/h vs 31.00/h, P<0.05), ODI (42.00/h vs 21.20/h, P<0.05), and TS90 (10.30% vs 1.90%, P<0.05) in the hypercapnic group were in turn higher than those in the normocapnic group. There were no significant cross-group differences in other polysomnographic parameters between the two groups.
 |
Table 2 Polysomnographic Parameters in the Hypercapnic and Normocapnic Groups |
Neuropsychological Tasks
The results of neuropsychological tasks were shown in Table 3. For verbal working memory, the DSB test scores in the hypercapnic group were significantly lower than that in the normocapnic group (5.00 vs 6.00, P<0.01). In the visual memory task, compared with the normocapnic group, the total PRM test duration in the hypercapnic group was significantly longer (170497.00ms vs 166829.50ms, P<0.05), and the accuracy in the delayed PRM task in the hypercapnic group was significantly lower (83.33 vs 91.67, P<0.05). The accuracy in the SRM task for the hypercapnic group was lower than that in the normocapnic group (80.00% vs 90.00%, P<0.01). There was no significant difference in the response delay for the SRM task between the hypercapnic group and normocapnic group. Lastly, in the spatial memory task, the SSP task scores in the hypercapnic group were lower than that in the normocapnic group (6.00 vs 7.00, P<0.01). For the SWM between errors and SWM strategy scores, both were significantly higher in the hypercapnic group (32.00 vs 29.50 and 107.00 vs 104.00, respectively. All P<0.01).
 |
Table 3 Results of the Neuropsychological Tasks in the Hypercapnic and Normocapnic Groups |
Variables Associated with Working Memory Among Patients with OSAHS
Each parameter of neuropsychological tasks was dichotomized using the median, and patients with scores lower than the median were classified into the poor performance group. Based on the results of the initial univariate analysis (for details see Tables A1-A3), we included all independent variables with P < 0.2 as well as basic demographic parameters (age, gender, BMI, years of education) in multivariate logistic regression. Due to the strong collinearity of ODI and AHI, ODI was excluded in the multivariate regression analysis.
The results showed that years of education (OR 0.734; 95% CI 0.612–0.881, P=0.001) and hypercapnia (OR 4.057; 95% CI 1.711–9.619, P=0.001) were independent predictors of low DSB score, which indicates poor verbal working memory (See Figure 2).
In terms of visual memory, the results of multivariate logistic regression showed that hypercapnia (OR 2.600; 95% CI 1.121–6.029, P=0.026) and years of education(OR 0.836; 95% CI 0.714–0.978, P=0.025) were independent predictors of accuracy in the immediate PRM task, hypercapnia (OR 2.766; 95% CI 1.150–6.654, P=0.023) and REM% (OR 1.099; 95% CI 1.014–1.192, P=0.022) were independent predictors of accuracy in the delayed PRM task, and hypercapnia(OR 2.722; 95% CI 1.083–6.843, P=0.033) was an independent predictor of accuracy in the SRM task(See Figure 3).
For spatial memory, hypercapnia (OR 4.795; 95% CI 1.844–12.472, P=0.001), years of education (OR 0.776; 95% CI 0.643–0.937, P=0.008) and years of snoring(OR 0.890; 95% CI 0.816–0.971, P=0.0009) were independent predictors of poor SSP task performance, and hypercapnia was an independent predictor of poor SWM task performance, in terms of both the between errors and strategy scores (OR 2.734; 95% CI 1.167–6.404, P=0.021; OR 2.558; 95% CI 1.169–5.595, P=0.019; respectively) (See Figure 4).
Discussion
Daytime hypercapnia can develop in patients with OSAHS due to various factors including obesity, impaired lung function, sleep respiratory disorder, and a decrease in the regulatory ability of the respiratory center.22–24 The prevalence of daytime hypercapnia is estimated to be 11–43%in patients with OSAHS.24–26 Many previous studies have shown that PtcCO2 is well correlated with PaCO2.27–30 Compared with other methods of measuring blood carbon dioxide levels, transcutaneous carbon dioxide monitoring can be a suitable alternative to blood gas analysis with minimal loss to precision. Therefore, this study employed transcutaneous carbon dioxide monitoring to measure the CO2 level in all patients. In the present study, OSAHS was accompanied by daytime hypercapnia in 35.8% of cases, consistent with previous studies. Previous studies suggested that high BMI is associated with daytime hypercapnia in patients with OSAHS, but no cross-group difference in BMI was observed in the present study.31 This could suggest that the hypercapnia experienced by patients in our study cohort may be attributable to other factors such as the distribution of fat (such as upper airway stenosis caused by fat accumulation in the neck, or upward movement of the diaphragm caused by fat accumulation in the abdomen) and maxillofacial anatomy (such as the presence of a small mandible or mandibular retraction), rather than BMI itself.
Previous studies tended to use questionnaires to assess cognitive function,32 which are less objective than the precise reaction time measurements offered by modern computerized cognitive tests. We selected non-verbal tests containing only patterns and tones in the CANTAB suite to minimize the effects of language and level of education, to which traditional questionnaires can easily be liable. The CANTAB has the exceptionally small practice effects and has also been widely used in neuropsychiatric research.28,33 The present study employed the DSB to evaluate the verbal working memory and the CANTAB tests to assess the visual and spatial memory. The PRM, SRM, SSP, and SWM in CANTAB are highly sensitive in detecting impairments in visual and spatial working memory.34 In the present study, DSB scores in the hypercapnic group were lower than those in the normocapnia group, demonstrating poorer verbal working memory. Compared with patients in the normocapnic group, patients in the hypercapnic group performed worse in the PRM and SRM tasks, suggesting worse spatial-visual memory. Hypercapnic patients showed poorer performance in the SWM and SSP tasks, suggesting impaired spatial working memory. In summary, the memory and execution function of the hypercapnic patients with OSAHS were impaired, in terms of both accuracy and speed.
Our previous study found that short-term memory and execution function in young Patients with OSAHS were impaired.35 In the present study, patients with OSAHS were young (mean age =40.07, SD = 7.06), yet one-third of patients complained of memory decline. In addition, no difference was observed in self-reported memory impairment between the hypercapnic and normocapnic groups, while the test batteries in the study demonstrated a significant cross-group difference in working memory. This suggests that the patients are unaware of the working memory impairment, or the measured impairment has little noticeable impact on their quality of life. Moreover, the hypercapnic patients with OSAHS complained more of severe morning fatigue and daytime sleepiness. This is in alignment with previous studies. For example, David Wang et al found that hypercapnia is a key correlate of sleep-disordered breathing (SDB)-related daytime sleepiness in a study of 55 patients with hypercapnic SDB.36
Traditionally, previous studies suggested that repeated nocturnal intermittent hypoxia and sleep fragmentation are the main causes of cognitive impairment in patients with OSAHS.11–14 In our study, there were no clear cross-group differences in terms of sleep structure. Although the hypoxia indicators including AHI, ODI and TS90 were higher in the hypercapnic group, which could lead to cognitive dysfunction by damaging the blood-brain barrier, brain micro-environment, synaptic plasticity neuron,37,38 our results indicated a much greater role for the hypercapnia-mediated cognitive impairment maybe over that by hypoxia or sleep fragmentation. Specifically, our results showed that daytime hypercapnia was a clear independent performance predictor in all verbal working memory and spatial memory tasks except the PRM task, with the odds ratios ranging from 2 to 5. On the other hand, no hypoxic parameters or indicators of sleep fragmentation were shown to be independently predictive of task performance. This clearly demonstrates the serious implications of daytime hypercapnia on the working memory of patients with OSAHS. This is in line with previous studies similarly emphasizing the prominent effect of hypercapnia on the cognitive function over that of nocturnal hypoxia or sleep fragmentation.39,40 This hypercapnia-mediated damage tended to be overlooked by previous research emphasizing the role of hypoxia and sleep fragmentation, possibly due to the less accessible nature of invasive CO2 measurements. However, based on previous studies, the influence of hypoxia on cognitive function cannot be ruled out. In the future, it may be necessary to develop different animal models to test the influence of hypercapnia or hypoxia on cognitive function respectively.
Some studies have suggested potential mechanisms through which the hypercapnic damage occurs. Animal experiments found that hypercapnia impairs cognitive function through neuroinflammation, increasing neuronal cell death, and damaging the permeability of the Blood-Brain Barrier in the hypoxemic environment.18,41 Wang et al found that hypercapnia can lead to EEG slowing with an increased delta/alpha ratio in healthy participants, OHS patients, and overlap syndrome (COPD+OSA) patients, and the effect was found to be independent of hypoxia.36,40 Sivam S et al found that delta/alpha ratio was negatively correlated with performance in psychomotor alertness tests in OSA patients and OHS patients.42 These show that hypercapnia may cause memory and execution function decline via EEG slowing. Additionally, both Wang and Sivam S. found that PAP treatment partially reversed the EEG slowing.36,42 As such, further mechanistic studies are needed to corroborate and complement the current findings to obtain a fuller picture of the hypercapnia-mediated cognitive impairment.
There are several limitations to our study. Although we had strict inclusion criteria that excluded hypercapnia due to other respiratory diseases, the lack of pulmonary function test in enrolled patients is a limitation of this study. We did not evaluate the changes in working memory after PAP treatment to investigate its potential effects. We did not include patients with OSA combined with sleep-related hypoventilation disorder. Admittedly, given the present study was conducted at a single center, further research is needed to provide evidence for these severe hypercapnia-mediated cognitive impairments.
Conclusion
In conclusion, young and middle-aged Patients with OSAHS with daytime hypercapnia exhibit clear evidence of visual, verbal, and spatial working memory impairment. Future research should place an equal emphasis on the hypercapnia-mediated processes alongside those of hypoxia and sleep fragmentation when studying the cognitive function of OSA patients. With non-invasive techniques such as transcutaneous CO2 measurement, it presents an increasingly compelling case to recommend routine monitoring of CO2 in patients with OSAHS.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
Approved by the Research Ethics Committee of the Second Affiliated Hospital of Soochow University, Suzhou, China (JD-LK-2018-004-02). Our study was conducted in accordance with the Declaration of Helsinki.
Consent for Participation and Publication
Informed consent was sought from all patients involved, with the understanding that anonymized data could be used for research and publications.
Acknowledgments
The authors thank technicians in department of Sleeping Center at the Second Affiliated Hospital of Soochow University for technical assistance throughout the study.
Funding
National Natural Science Foundation of China (Grant/Award Number: 81770085,82070095); Discipline Construction Program of the Second Affiliated Hospital of Soochow University (Grant/Award Number XKTJ-TD202003).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi:10.1056/NEJM199304293281704
2. Salman LA, Shulman R, Cohen JB. Obstructive Sleep Apnea, Hypertension, and Cardiovascular Risk: epidemiology, Pathophysiology, and Management. Curr Cardiol Rep. 2020;22(2):6.
3. Bucks RS, Olaithe M, Eastwood P. Neurocognitive function in obstructive sleep apnoea: a meta-review. Respirology. 2013;18(1):61–70.
4. Ahuja S, Chen RK, Kam K, Pettibone WD, Osorio RS, Varga AW. Role of normal sleep and sleep apnea in human memory processing. Nat Sci Sleep. 2018;10:255–269.
5. Bubu OM, Andrade AG, Umasabor-Bubu OQ, et al. Obstructive sleep apnea, cognition and Alzheimer’s disease: a systematic review integrating three decades of multidisciplinary research[J]. Sleep Med Rev. 2020;50:101250.
6. Baddeley A. Working memory: theories, models, and controversies. Annu Rev Psychol. 2012;63:1–29.
7. Greve DN, Duntley SP, Larson-Prior L, et al. Effect of armodafinil on cortical activity and working memory in patients with residual excessive sleepiness associated with CPAP-Treated OSA: a multicenter fMRI study. J Clin Sleep Med. 2014;10(2):143–153.
8. Archbold KH, Borghesani PR, Mahurin RK, Kapur VK, Landis CA. Neural activation patterns during working memory tasks and OSA disease severity: preliminary findings. J Clin Sleep Med. 2009;5(1):21–27.
9. Felver-Gant JC, Bruce AS, Zimmerman M, Sweet LH, Millman RP, Aloia MS. Working memory in obstructive sleep apnea: construct validity and treatment effects. J Clin Sleep Med. 2007;3(6):589–594.
10. Sweet LH, Jerskey BA, Aloia MS. Default network response to a working memory challenge after withdrawal of continuous positive airway pressure treatment for obstructive sleep apnea. Brain Imaging Behav. 2010;4(2):155–163.
11. Bucks RS, Olaithe M, Rosenzweig I, Morrell MJ. Reviewing the relationship between OSA and cognition: where do we go from here? Respirology. 2017;22(7):1253–1261. doi:10.1111/resp.13140
12. He Y, Chen R, Wang J, et al. Neurocognitive impairment is correlated with oxidative stress in patients with moderate-to-severe obstructive sleep apnea hypopnea syndrome. Respir Med. 2016;120:25–30.
13. Alomri RM, Kennedy GA, Wali SO, Ahejaili F, Robinson SR. Differential associations of hypoxia, sleep fragmentation, and depressive symptoms with cognitive dysfunction in obstructive sleep apnea. Sleep. 2021;44(4):zsaa213.
14. Dewan NA, Nieto FJ, Somers VK. Intermittent hypoxemia and OSA: implications for comorbidities. Chest. 2015;147(1):266–274.
15. Quan SF, Chan CS, Dement WC, et al. The association between obstructive sleep apnea and neurocognitive performance--The Apnea Positive Pressure Long-term Efficacy Study (APPLES). Sleep. 2011;34(3):303–314B.
16. Martin MS, Sforza E, Roche F, Barthélémy JC, Thomas-Anterion C; PROOF study group. Sleep breathing disorders and cognitive function in the elderly: an 8-year follow-up study. the proof-synapse cohort. Sleep. 2015;38(2):179–187.
17. Lutsey PL, Bengtson LG, Punjabi NM, et al. Obstructive Sleep Apnea and 15-Year Cognitive Decline: the Atherosclerosis Risk in Communities (ARIC) Study. Sleep. 2016;39(2):309–316.
18. Liu X, Ding H, Li X, et al. Hypercapnia Exacerbates the Blood-Brain Barrier Disruption Via Promoting HIF-1a Nuclear Translocation in the Astrocytes of the Hippocampus: implication in Further Cognitive Impairment in Hypoxemic Adult Rats. Neurochem Res. 2020;45(7):1674–1689.
19. Kung SC, Shen YC, Chang ET, Hong YL, Wang LY. Hypercapnia impaired cognitive and memory functions in obese patients with obstructive sleep apnoea. Sci Rep. 2018;8(1):17551.
20. Berry RB, Albertario CL, Harding SM, et al. The AASM Manual for the Scoring of Sleep and Associated Events. Am Acad Sleep Med. 2018;176:2012.
21. Kawata N, Tatsumi K, Terada J, et al. Daytime hypercapnia in obstructive sleep apnea syndrome. Chest. 2007;132(6):1832–1838.
22. Kaw R, Hernandez AV, Walker E, Aboussouan L, Mokhlesi B. Determinants of hypercapnia in obese patients with obstructive sleep apnea: a systematic review and metaanalysis of cohort studies. Chest. 2009;136(3):787–796.
23. Chaouat A, Weitzenblum E, Krieger J, Ifoundza T, Oswald M, Kessler R. Association of chronic obstructive pulmonary disease and sleep apnea syndrome. Am J Respir Crit Care Med. 1995;151(1):82–86.
24. Krieger J, Sforza E, Apprill M, Lampert E, Weitzenblum E, Ratomaharo J. Pulmonary hypertension, hypoxemia, and hypercapnia in obstructive sleep apnea patients. Chest. 1989;96(4):729–737.
25. Akashiba T, Kawahara S, Kosaka N, et al. Determinants of chronic hypercapnia in Japanese men with obstructive sleep apnea syndrome. Chest. 2002;121(2):415–421.
26. Laks L, Lehrhaft B, Grunstein RR, Sullivan CE. Pulmonary hypertension in obstructive sleep apnoea. Eur Respir J. 1995;8(4):537–541.
27. Spelten O, Fiedler F, Schier R, Wetsch WA, Hinkelbein J. Transcutaneous PTCCO2 measurement in combination with arterial blood gas analysis provides superior accuracy and reliability in ICU patients. J Clin Monit Comput. 2017;31(1):153–158.
28. Lermuzeaux M, Meric H, Sauneuf B, et al. Superiority of transcutaneous CO2 over end-tidal CO2 measurement for monitoring respiratory failure in nonintubated patients: a pilot study. J Crit Care. 2016;31(1):150–156.
29. Aarrestad S, Tollefsen E, Kleiven AL, Qvarfort M, Janssens JP, Skjønsberg OH. Validity of transcutaneous PCO2 in monitoring chronic hypoventilation treated with non-invasive ventilation. Respir Med. 2016;112:112–118.
30. Johnson DC, Batool S, Dalbec R. Transcutaneous carbon dioxide pressure monitoring in a specialized weaning unit. Respir Care. 2008;53(8):1042–1047.
31. Laaban JP, Chailleux E. Daytime hypercapnia in adult patients with obstructive sleep apnea syndrome in France, before initiating nocturnal nasal continuous positive airway pressure therapy. Chest. 2005;127(3):710–715.
32. Chen R, Xiong KP, Huang JY, et al. Neurocognitive impairment in Chinese patients with obstructive sleep apnoea hypopnoea syndrome. Respirology. 2011;16(5):842–848.
33. Lawrence AD, Sahakian BJ, Hodges JR, Rosser AE, Lange KW, Robbins TW. Executive and mnemonic functions in early Huntington’s disease. Brain. 1996;119(Pt 5):1633–1645.
34. Baldacchino A, Tolomeo S, Balfour DJ, Matthews K. Profiles of visuospatial memory dysfunction in opioid-exposed and dependent populations. Psychol Med. 2019;49(7):1174–1184.
35. Li Q, Li NZ, Li TT, Sun YQ, Wang J, Chen R. The characteristics and determining factors of attention and short-term memory impairment in young patients with obstructive sleep apnea-hypopnea syndrome. Zhonghua Jie He He Hu Xi Za Zhi. 2019;42(6):419–425.
36. Wang D, Piper AJ, Yee BJ, et al. Hypercapnia is a key correlate of EEG activation and daytime sleepiness in hypercapnic sleep disordered breathing patients. J Clin Sleep Med. 2014;10(5):517–522.
37. Lim DC, Pack AI. Obstructive sleep apnea and cognitive impairment: addressing the blood-brain barrier. Sleep Med Rev. 2014;18(1):35–48.
38. Kerner NA, Roose SP. Obstructive Sleep Apnea is Linked to Depression and Cognitive Impairment: evidence and Potential Mechanisms. Am J Geriatr Psychiatry. 2016;24(6):496–508.
39. Wang D, Thomas RJ, Yee BJ, Grunstein RR. Hypercapnia is more important than hypoxia in the neuro-outcomes of sleep-disordered breathing. J Appl Physiol. 2016;120(12):1484.
40. Wang D, Yee BJ, Wong KK, et al. Comparing the effect of hypercapnia and hypoxia on the electroencephalogram during wakefulness. Clin Neurophysiol. 2015;126(1):103–109.
41. Ding HG, Deng YY, Yang RQ, et al. Hypercapnia induces IL-1β overproduction via activation of NLRP3 inflammasome: implication in cognitive impairment in hypoxemic adult rats. J Neuroinflammation. 2018;15(1):4.
42. Sivam S, Poon J, Wong KKH, et al. Slow-frequency electroencephalography activity during wake and sleep in obesity hypoventilation syndrome. Sleep. 2020;43(2):zsz214.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




