Back to Journals » Infection and Drug Resistance » Volume 15
Cylindrical Tube Stethoscopes: The Value of Practical Equipment in the Management of Patients with Infectious Diseases
Authors Zhu J , Jiang CY, Huang B, Hu JM, Fang SZ, Huang K, Gao YH, Yu J
Received 4 April 2022
Accepted for publication 28 June 2022
Published 7 July 2022 Volume 2022:15 Pages 3611—3618
DOI https://doi.org/10.2147/IDR.S369305
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jian Zhu,1,* Chuan-Yang Jiang,2,* Bin Huang,3,* Ji-Min Hu,4 Si-Zhen Fang,5 Ke Huang,1 Yan-Hong Gao,6 Jiao Yu7
1Department of Thoracic Cardiovascular Surgery, General Hospital of Central Theater Command of People’s Liberation Army, Wuhan, 430070, People’s Republic of China; 2College of Mechanical Engineering, Liaoning Petrochemical University, Fushun, 113001, People’s Republic of China; 3The First School of Clinical Medicine, Southern Medical University, Guangzhou, 510515, People’s Republic of China; 4Science Technology and Standards Center, Jiangsu Testing and Inspection Institute for Medical Devices, Nanjing, 210019, People’s Republic of China; 5Spectris Instrumentation & Systems Shanghai Ltd. Guangzhou Branch, Guangzhou, 510620, People’s Republic of China; 6Department of Ultrasound, General Hospital of Central Theater Command of People’s Liberation Army, Wuhan, 430070, People’s Republic of China; 7College of Science, Liaoning Petrochemical University, Fushun, 113001, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jiao Yu, College of Science, Liaoning Petrochemical University, Fushun, 113001, People’s Republic of China, Email [email protected] Yan-Hong Gao, Department of Ultrasound, General Hospital of Central Theater Command of People’s Liberation Army, Wuhan, 430070, People’s Republic of China, Email [email protected]
Background: The COVID-19 pandemic has continued for more than two years since its outbreak. Due to the clinical auscultation needs of doctors when wearing airtight protective clothing, a cylindrical tube stethoscope was proposed to address this problem. However, the idea has been questioned by some experts.
Methods: To address these questions, we performed three-part experiments using cylindrical tube stethoscopes. First, we performed laboratory tests to detect the sound intensity from a cylindrical tube stethoscope. Second, we improved the cylindrical tube stethoscope to achieve better results. Third, we revealed the difference in the auscultation effects of the cylindrical tube stethoscope and a conventional professional 3 M stethoscope.
Results: From these experiments, we found that a narrow cylindrical tube with a diameter of 4.2 cm and a length of 20 cm equipped with a silicone gasket better auscultation of heart sounds. A cylindrical tube stethoscope and a 3 M stethoscope were used to perform stethoscope tests on 10 volunteers. The alveolar lung sounds were 44.478 decibels vs 49.529 decibels, the heart sounds were 46.631 decibels vs 41.109 decibels, and the intestinal sounds were 40.132 decibels vs 43.787 decibels, respectively.
Conclusion: This improved cylindrical tube stethoscope can meet the auscultation requirements for cardiorespiratory and abdominal diagnosis during infectious disease pandemics.
Keywords: stethoscope, auscultation, COVID-19, SARS-CoV-2, acoustic optimization
Introduction
Coronavirus disease 2019 (COVID-19) poses a serious threat to global public health, resulting in extensive challenges to the management of patients.1,2 In COVID-19 pandemic areas, it is highly recommended that all medical staff, whether in the outpatient clinic or the ward, wear protective clothing to avoid SARS-CoV-2 infection. However, this protective clothing interferes with auscultation, one of the most common physical examinations for the heart, lungs, and abdomen of patients. The reason is that the stethoscope could not be inserted completely into the ears when wearing protective clothing.
To solve these problems, we used a potato chip canister and A4 paper to make a simple stethoscope that was convenient and practical.3 After the experience of using simple stethoscope paper was published, it received widespread attention from the mass media. On the academic side, the majority of peer experts supported our views on the simple stethoscope, including cost savings for COVID-19 patients, solving actual problems, sharing our anti-epidemic experience without reservation, avoiding contact with ultrasound doctors, saving anti-epidemic materials, etc. However, the idea has also been questioned by some experts. These experts questioned whether this method was suited to performing auscultation. They questioned whether sound could be heard through the cylindrical tube stethoscope. Additionally, they stated that the stethoscope we made was a random tool created from a snack container, not a scientific diagnostic tool from a medical manufacturer.
To address these issues, we performed three-part experiments with cylindrical tube stethoscopes. First, we performed laboratory tests to detect the intensity of the sound from the cylindrical tube stethoscope. The effectiveness of hearing or collecting sounds from the lungs, heart, and intestines by using a cylindrical tube stethoscope while wearing protective clothing was investigated. Second, we showed the specific usage and practical effect of the cylindrical tube stethoscope in the management of COVID-19 patients. Moreover, we improved the stethoscope to obtain a better effect. Third, we explained the difference between the auscultation effects of the improved cylindrical tube stethoscope and a conventional professional 3M stethoscope.
Method
Composition of the Cylindrical Tube Stethoscope
The cylindrical tube stethoscope made by our team was based on the following principles: a vertical tube, a monaural nature, and a smooth inner wall. The stethoscope was constructed of a potato chip canister and A4 paper attached to the surface of the packaging barrel (diameter: 6.5 cm, length: 20 cm, thickness: 0.2 cm). In addition, each cylindrical tube stethoscope was equipped with a silicone gasket matched with the barrel (Figure 1). The silicone gasket ensured that there was no distance between the cylindrical tube stethoscope and the chest wall. This also addressed the problem of airtightness in the case of thin patients. To distinguish it from other cylindrical stethoscopes, we named this potato chip tube stethoscope the cylindrical tube stethoscope.
Application Process in Clinical Work
The cylindrical tube stethoscope was placed in front of the inpatient bed and in the clinic room. It was sprayed with 500 mg/L chlorine dioxide or other chlorine-containing disinfectants every day. During auscultation, the doctor or nurse turned their back to the patients to choose the left or right ear listening. The bottom of the cylindrical tube stethoscope tightly covered the skin of the patient’s auscultation area. Patients with thin bodies needed silicone gaskets. The end of the cylindrical tube stethoscope was covered over the outer ear, and the protective clothing over the outer ear was maintained in a state of tension.
Acoustic Tests and Analyses
The auscultations were performed for 10 volunteers using a cylindrical stethoscope with a regular tube (diameter: 6.5 cm, length: 20 cm), a stethoscope with narrow tube for cardiac auscultation (diameter: 4.2 cm, length: 20 cm), and an acoustic stethoscope (3 M Littmann Lightweight S.E. Stethoscope, 3 M Health Care, MN, USA). The signals were measured by a sound level metre (type-2250, Brüel & Kjær, Nærum, Denmark) with a microphone preamplifier (ZC-0032) and a prepolarized microphone (type-4189) that was omnidirectional and had a flat frequency response in the entire considered frequency range. The acquired signals were saved as wave files and then processed by BK Connect 2019 software (Brüel & Kjær, Nærum, Denmark). An A-weighting filter was applied to simulate the sensitivity of the human ear to different frequency bands of sound, and a standardized constant percentage bandwidth filter was used to convert the time data to a 1/3 octave spectrum.
In the measurement, each of the ten volunteers was tested twice in succession at each auscultation site, including the apex area of the heart, the triangle of auscultation of the lungs and McBurney’s point of the intestines. The corresponding frequency range of interest for each auscultation site is 20–115 Hz for heart sounds and 20–1000 Hz for lung sounds and intestinal sounds.4,5 With the stethoscope mentioned above pressed to the surface of the body, each auscultation lasted for one minute. Subsequently, the mean sound-pressure level spectrum for each stethoscope was obtained by taking the average of the twenty measurements at each auscultation site. Given that medical staff need to keep their ears close to the cylindrical tube stethoscope to acquire clear sound signals and to prevent sound leaks and ambient noise interference, sponge rubber sheaths were utilized for sound insulation in the experimental environment. Furthermore, to reflect the situation of auscultation in which medical workers wear protective clothing, a small piece of material cut off from a suit of protective clothing was employed to completely wrap the front end of the microphone, whose body was inserted into the sponge rubber sheath. When auscultations were carried out using the 3 M stethoscope, the corresponding signals were recorded by the prepolarized microphone capsule placed in one of the earpieces, with the other earpiece completely sealed. All the measurements were conducted using identical settings and hardware setups.
Results
The Effectiveness and Theoretical Understanding of the Cylindrical Tube Stethoscope
The mean frequency spectra of the measured acoustic signals of all ten volunteers at the auscultation sites of the lungs, hearts, and intestines are shown in Figure 2. The sound pressure levels measured at the auscultation sites of lungs (Figure 2A), hearts (Figure 2B), and intestines (Figure 2C) were 44.478 dB, 46.631 dB, and 40.132 dB, respectively. These tested sound pressure levels were 20.898 dB, 27.840 dB, and 16.553 dB higher than the ambient noise, respectively. According to the fundamentals of the quantitative measures of sound and the threshold of audibility for people without acute hearing loss,6–8 the sound pressure levels obtained through the cylindrical tube stethoscope, which ranged from approximately 40 dB to 47 dB, could be heard by medical practitioners with normal hearing and applied for pulmonary, cardiac and intestinal auscultation in the corresponding frequency range of interest.
In Figure 2A, considering the frequency range of interest for pulmonary sounds, it is essential to explain the cause of the apparent concave shape of the original tube curve at approximately 500 Hz. According to the fundamental theory of acoustic waveguides with a constant cross section,9 the cut-off frequency of the plane wave in the cylindrical tube stethoscope is
where c is the speed of sound in air and d is the diameter of the circular cross section of the cylindrical tube stethoscope. Note that the frequencies of the physiologically important pulmonary sounds (20 Hz-1000 Hz) are obviously less than the cut-off frequency fc in Eq. (1), the sounds used for lung auscultations will propagate in plane-wave mode given a virtual source plane. The sound pressure in the cylindrical waveguide is theoretically expressed as
where k is the wavenumber, P0 is the sound pressure of the sound source, and x is the distance between the sound source and the sound receiver. The mean pulmonary sound pressure level of all the volunteers, directly measured at each volunteer’s triangle of auscultation by using the type-2250 sound level metre, was 33.917 dB, and therefore P0=9.93×10−4 Pa was taken into calculation.
According to Eq. (2), the pulmonary sound pressure level measured and calculated at the position of the microphone head (16 cm) of the cylindrical tube stethoscope are compared in Figure 3. Figure 3 shows that the trend of the theoretical value is basically consistent with the experimental measurement from 250 Hz to 1000 Hz, especially at approximately 500 Hz, where both curves reach the rock bottom. Similarly, for intestinal sounds in Figure 2(C), the concavity of the frequency spectra in the range of 250 Hz to 1000 Hz can be explained in the same way. Theoretically, the location of the valley point is determined by the distance between the sound source and the receiver, and the concavity moves towards a higher frequency by reducing the tube length.
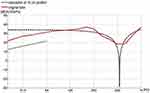 |
Figure 3 The measured and calculated pulmonary sound pressure levels of the cylindrical tube stethoscope. |
In the low-frequency range of 20 Hz to 63 Hz in Figure 3, the frequency spectrum of the average pulmonary sound-pressure level almost increases linearly. The corresponding wavelength for the low-frequency range (20 Hz–63 Hz) is from 5.46 m to 17.2 m, which is much greater than the radius of the original tube stethoscope. Therefore, the low-frequency approximation is suitable in the present research. Additionally, in view of the natural curvature of the human body surface, along with the elasticity of muscles and skin, a slightly curved skin surface will form within the chestpiece of the tube when the cylindrical stethoscope is pressed onto the surface of the patient’s body. According to the fundamentals of sound radiation from radially oscillating spheres,10 the sound pressure is in direct proportion to sound frequency in the low-frequency approximation mentioned above. A virtual spherical source oscillating radially gives a trend line similar to the thin black solid line at low frequency in Figure 3, where the magnitude information of the trend line should be dismissed since the vibration velocity of the spherical source is unknown. The spherical source assumption can be employed to account for the quasi-linear growth of the pulmonary sound-pressure level in the low-frequency range of 20 Hz to 63 Hz. The measured pulmonary, cardiac and intestinal sound plots do not level off at low frequency, which is very likely to result from the sound source that is not an ideal plane source. Taking lung auscultation as an example, the lung sounds transmitted through intercostal spaces may be deemed as a small spherical source with a size to a certain extent smaller than the bore of the tube.
The Narrow Tube Stethoscope Compared with the Cylindrical Tube Stethoscope
In real cardiac auscultations for cases with respiratory diseases, we repeatedly tested different cylindrical tube stethoscopes and analysed the cut-off frequency, sound power transmission coefficient, and sound wave propagation in the uniform lossless waveguide. Considering the individual physical differences and murmurs in the abdominal cavity, the heart sounds were chosen for the diameter selection analysis because the heart sounds are not only relatively loud compared to other bioacoustic signals but also regular and not consciously controlled.11 Theoretically, our previous investigation12 suggested that the narrow tube stethoscope, with a diameter of 3.3–4.4 cm, possesses moderately better audio performance than the cylindrical tube stethoscope. This is related to the following factors that influence sensing sounds and vibration, including the sound power transmission coefficient and the curvature of the surface of the human body.12 Thus, a representative value of diameter (4.2 cm), which was approximately equal to the dimensions of the chestpiece of the 3 M Littmann lightweight stethoscope we used, was selected in laboratory testing for a better comparison.
Laboratory testing also verified the above theory. Figure 4 shows a comparison of the frequency spectra of various stethoscopes. Figure 4B shows that the sound-pressure level of the narrow tube stethoscope was approximately 2 dB higher than that of the cylindrical tube stethoscope. This indicated that the narrow tube stethoscope had relatively better acoustic performance in the auscultation of the apex area of the heart in the frequency range of interest from 20 Hz to 115 Hz.4,5
The Cylindrical Tube Stethoscope Compared with the 3 M Stethoscope
Figure 4 presents a comparison of the frequency spectra of the 3 M Littmann lightweight stethoscope and the cylindrical tube stethoscope in terms of quantitative sound-pressure levels. The sound-pressure levels of the 3 M acoustic stethoscope at the auscultation sites of the lungs (Figure 4A), hearts (Figure 4B), and intestines (Figure 4C) were 49.529 dB, 41.109 dB, and 43.787 dB, respectively, in the corresponding frequency ranges of interest. In the lung and intestine auscultations, the sound-pressure levels of the 3 M acoustic stethoscope were 3 dB to 5 dB higher than those of the cylindrical tube stethoscope. In cardiac auscultations, the sound-pressure levels of the 3 M acoustic stethoscope were 5.5 dB to 7.5 dB lower than those of the cylindrical tube stethoscope. In terms of the sound pressure levels, the cylindrical tube stethoscope was better than the 3 M Littmann lightweight stethoscope for cardiac auscultations. The mean spectrograms of the heart sound signals of all ten volunteers measured using the cylindrical tube stethoscope and the 3 M stethoscope are shown in Figure 5A and B, respectively. The periodic heartbeat is more clearly visible along the timeline for the cylindrical tube stethoscope. However, the 3 M Littmann lightweight stethoscope obtained a relatively flat frequency response, which was consistent with stable audio performance.
 |
Figure 5 Spectrogram of heart sound signals of all ten volunteers measured using stethoscope (A) the cylindrical tube stethoscope. (B) the 3 M stethoscope. |
Discussion
In 1816, Dr. Rene Laennec directly attached his ear to the patient’s chest to obtain information about the lung lesions, which might be the first documentation of auscultation.13 Consequently, the idea of using a cylindrical tube stethoscope seemed to solve these issues during the COVID-19 pandemic. In lung auscultation, one of the outstanding contributions of the cylindrical tube stethoscope during the COVID-19 epidemic has been the recognition of loud rales crackles. Compared with re-examining chest computerized tomography to understand the progress of pneumonia, the cylindrical tube stethoscope has been faster, timelier and more economical. The other contribution of the cylindrical tube stethoscope is that can pick up high-pitched rales and other lung sounds, especially under the breasts and in the infrascapular region. In heart auscultation, the cylindrical tube stethoscope has been effective. There were no problems with collecting the heart rate using the cylindrical tube stethoscope. It can be used to find premature beats and atrial fibrillation. For heart murmurs, it was easy to identify whether a patient had murmurs with the cylindrical tube stethoscope. However, it has been difficult to differentiate systolic murmurs or diastolic murmurs caused by valvular disease. In abdominal auscultation, 3 M Littmann lightweight stethoscopes have been mainly used to check bowel sounds and vascular murmurs. The cylindrical tube stethoscope can also hear the purring of intestinal peristalsis. In addition, the cylindrical tube stethoscope has played a role in listening to the sound of gas in the stomach impacting water during the COVID-19 pandemic, which has provided a convenient way to determine whether a gastric tube has been successfully placed in critically ill patients.
In some critical moments, clinicians need to make quick judgements to deal with emergencies. For instance, when a critical COVID-19 patient with tracheal intubation was suddenly blocked by sputum, we could use the cylindrical tube stethoscope to identify and quickly remove it. Additionally, when a severe COVID-19 patient experienced an acute bronchial asthma attack, we could employ the cylindrical tube stethoscope to accurately determine and quickly relieve the fatal condition of the severe COVID-19 patient. Ultrasound diagnosis, however, appeared to be comparatively helpless in such an emergency.
We conducted extensive acoustic tests on cylindrical tube stethoscopes and 3 M Littmann lightweight stethoscopes. The cylindrical tube stethoscope could sufficiently amplify sounds from the lungs, hearts, and intestines. The cylindrical tube stethoscope, which can completely cover the ear, can meet the needs of auscultation during the COVID-19 pandemic. If the inner wall of the tube was smooth and the tube had a silicone gasket matched with the barrel, we could obtain a better audio performance. Although there was little difference for different diameters of the cylindrical tube stethoscope, tube diameters between 4.0 cm and 6.5 cm could meet our auscultation needs. If the diameter was too small, the tube could not cover the ear. In contrast, if the diameter was too large, the sound could leak. A narrow tube stethoscope with a diameter of approximately 4.2 cm seemed to be more suitable for picking up heart sounds and contributing to sound transmission to the external auditory canal of the medical practitioner. Combined with our first-line experience, a gap of several decibels in sound pressure levels could be accepted and would not affect the clinical applications of the cylindrical tube stethoscope. From all aspects, the cylindrical tube stethoscope was a valuable and viable alternative to traditional acoustic stethoscopes in the dynamic diagnosis of conditions during the COVID-19 pandemic.
There was no doubt that many of the advantages of the 3 M Littmann lightweight stethoscope could not be achieved by cylindrical tube stethoscopes. Although the sound pressure levels were similar, we could sense the reduction in the surrounding sound interference, and the auscultation performance of the 3 M stethoscope was more stable than that of the cylindrical tube stethoscope. The design of the earpieces of the 3 M Littmann lightweight stethoscope played an important role in the collection of sound and resistance against interference during auscultation. The 3 M Littmann lightweight stethoscope could even obtain different sounds of low frequency and high frequency through only a change in the pressure on the diaphragm. Cylindrical tube stethoscopes seemed to have an advantage only for low-frequency sounds. Nevertheless, based on our first-line practice and experimental tests, the effectiveness of the cylindrical tube stethoscope was confirmed both clinically and experimentally. Additionally, note that cylindrical tube stethoscopes, which are easy to carry, could be employed not only in infectious isolation wards but also in some special situations where medical staff must wear protective clothing, such as battlefield emergency rescue in polluted environments. Additionally, some vital medical equipment, such as tourniquets and scarf bandages, can be stored in cylindrical tube stethoscopes and easily removed in special emergency rescues. Therefore, this cylindrical tube stethoscope can not only meet the demand for emergency auscultation but also become a practical container for first-aid supplies. Hopefully, the acoustic performance of cylindrical tube stethoscopes can be further investigated and improved by optimizing the overall geometric configuration and effectively reducing the frictional loss of sound at the inner surface of the device.
Additionally, some new auscultation devices need to be recognized. Ear-contactless electronic stethoscopes allow real-time recording and playback of auscultation sounds. However, they are more expensive than cylindrical tube stethoscopes.14 On the other hand, a Bluetooth stethoscope requires two cycles of acoustic and electrical changes, and the sound in one’s ear is different from that of a conventional stethoscope. Its noise level is higher than that of the conventional stethoscope.15 In this paper, we present the hope that scientists and engineers can develop stethoscopes that can also be worn with airtight protective clothing and transmit auscultation sounds directly to the ear.
Conclusions
In conclusion, the cylindrical tube stethoscope, which is an effective and convenient substitute for the conventional acoustic stethoscope, enables medical staff to perform auscultations of heart, lung, and intestine sounds during the COVID-19 pandemic. Acoustic experiments and theoretical analyses were performed to understand the audio performance of the cylindrical tube stethoscopes, and a narrow tube design of the stethoscope gave a better auscultation effect for heart sounds. Applying and optimizing this simple device may allow the development of a better stethoscope that can be used when wearing airtight protective clothing, enabling direct sound transmission to the ear.
Ethics Approval and Consent to Participate
This report complies with the guidelines for human studies and is in accordance with the Declaration of Helsinki. Written informed consent was obtained from the patient and ten volunteers in accordance with the Declaration of Helsinki for the purpose of publication of the present report and any relevant images. The General Hospital of Central Theater Command of People’s Liberation Army allowed ethical exemptions since it was a life-saving diagnosis, not an experiment for treatment.
Informed Consent for Publication
Written informed consent was provided by the patient to participate in this study and for the publication of this paper.
Acknowledgments
We are indebted to Drs. Jia-Qi Zhao and Da-Wei Wang for their contributions to the scholarly discussions and technical support in the research. Jian Zhu, Chuan-Yang Jiang, and Bin Huang are co-first authors for this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was financially supported by the National Natural Science Foundation of China (Grant No. 12074160), the Natural Science Foundation of Liaoning Province of China (Grant No. 2019-MS-219), and the Liaoning Revitalization Talents Program (Grant No. XLYC1907034).
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
1. Zhu J, Zhang Y, Gao XH, Xi EP. Coronavirus disease 2019 or lung cancer: a differential diagnostic experience and management model from Wuhan. J Thorac Oncol. 2020;15:e141–e142. doi:10.1016/j.jtho.2020.04.030
2. Razai MS, Doerholt K, Ladhani S, Oakeshott P. Coronavirus disease 2019 (covid-19): a guide for UK GPs. BMJ. 2020;368:m800. doi:10.1136/bmj.m800
3. Zhu J, Tan Y, Huang B, Zhu Y, Gao XH. Don’t throw the stethoscope away! Eur Heart J. 2021;42:10–12. doi:10.1093/eurheartj/ehaa343
4. Callahan D, Waugh J, Mathew GA, Granger WM. Stethoscopes: what are we hearing? Biomed Instrum Technol. 2007;41:318–323. doi:10.2345/0899-8205(2007)41[318:SWAWH]2.0.CO;2
5. Dawson JB. Auscultation and the stethoscope. Practitioner. 1964;193:315–322.
6. Pierce AD. Acoustics: An Introduction to Its Physical Principles and Applications. Melville, New York: The Acoustical Society of America; 1989:60–63.
7. Stevens SS, Fred W. Sound and Hearing. Alexandria, Virginia: Life Science Library, Time-Life Books; 1965:173.
8. Fletcher H. Auditory patterns. Rev Mod Phys. 1940;12:47. doi:10.1103/RevModPhys.12.47
9. Pierce AD. Acoustics: An Introduction to Its Physical Principles and Applications. Melville, New York: The Acoustical Society of America; 1989:315–317.
10. Pierce AD. Acoustics: An Introduction to Its Physical Principles and Applications. Melville, New York: The Acoustical Society of America; 1989:153–156.
11. Nowak LJ, Nowak KM. Acoustic characterization of stethoscopes using auscultation sounds as test signals. J Acoust Soc Am. 2017;141:1940. doi:10.1121/1.4978524
12. Jiang CY, Zhao JQ, Huang B, Zhu J, Yu J. A basic investigation into the optimization of cylindrical tubes used as acoustic stethoscopes for auscultation in COVID-19 diagnosis. J Acoust Soc Am. 2021;149:66–69. doi:10.1121/10.0002978
13. Singh VP. Stethoscope: a short autobiography. Int J Cardiol. 2018;250:1–3. doi:10.1016/j.ijcard.2017.09.013
14. Yang C, Zhang W, Pang Z, et al. Ear-contactless electronic stethoscope powered by raspberry Pi for auscultation of patients with COVID-19: prototype development and feasibility study. JMIR Med Inform. 2021;9(1):e22753. doi:10.2196/22753
15. Jain A, Sahu R, Jain A, Gaumnitz T, Sethi P, Lodha R. Development and validation of a low-cost electronic stethoscope: DIY digital stethoscope. BMJ Innov. 2021;7(4):45. doi:10.1136/bmjinnov-2021-000715
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.