Back to Journals » Infection and Drug Resistance » Volume 17
CTX-M, TEM, and SHV Genes in Escherichia coli, Klebsiella pneumoniae, and Enterobacter spp Isolated from Hematologic Cancer Patients with Bacteremia in Uganda
Authors Lubwama M , Kateete DP, Katende G, Kigozi E, Orem J, Phipps W, Bwanga F
Received 30 September 2023
Accepted for publication 8 February 2024
Published 16 February 2024 Volume 2024:17 Pages 641—653
DOI https://doi.org/10.2147/IDR.S442646
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Margaret Lubwama,1 David P Kateete,2 George Katende,1 Edgar Kigozi,2 Jackson Orem,3 Warren Phipps,4,5 Freddie Bwanga2
1Department of Medical Microbiology, School of Biomedical Sciences, College of Health Sciences, Makerere University, Kampala, Uganda; 2Department of Immunology and Molecular Biology, School of Biomedical Sciences, College of Health Sciences, Makerere University, Kampala, Uganda; 3Uganda Cancer Institute, Kampala, Uganda; 4Vaccine and Infectious Disease Division, Fred Hutchinson Cancer Center, Seattle, WA, USA; 5Allergy and Infectious Diseases Division, Department of Medicine, University of Washington, Seattle, WA, USA
Correspondence: Margaret Lubwama, Department of Medical Microbiology, School of Biomedical Sciences, College of Health Sciences, Makerere University, P. O Box 7072, Kampala, Uganda, Tel +256 774 440 332, Email [email protected]
Purpose: We determined the phenotypic resistance to third-generation cephalosporins, phenotypic extended spectrum beta-lactamase (ESBL) prevalence, and genotypic prevalence of ESBL-encoding genes blaCTX-M, blaTEM, and blaSHV in Enterobacteriaceae isolated from hematologic cancer patients with febrile neutropenia and bacteremia at the Uganda Cancer Institute (UCI).
Patients and Methods: Blood cultures from hematologic cancer patients with febrile neutropenia were processed in BACTEC 9120. E. coli, K. pneumoniae, and Enterobacter spp. isolates were identified using conventional biochemical methods. Antimicrobial susceptibility tests, phenotypic ESBL characterization, and genotypic characterization of the ESBL-encoding genes blaCTX-M, blaTEM, and blaSHV were determined for pure isolates of E. coli, K. pneumoniae, and Enterobacter spp.
Results: Two hundred and two patients were included in the study. Median age of patients was 19 years (IQR: 10– 30 years). Majority (N=119, 59%) were male patients. Sixty (30%) of the participants had at least one febrile episode due to Enterobacteriaceae. Eighty-three organisms were isolated with E. coli being predominant (45, 54%). Seventy-nine (95%) Enterobacteriaceae were multidrug resistant. The ESBL phenotype was detected in 54/73 (74%) of Enterobacteriaceae that were resistant to third-generation cephalosporins. A higher proportion of Enterobacteriaceae with ESBL-positive phenotype were resistant to piperacillin-tazobactam (p=0.024), gentamicin (p=0.000), ciprofloxacin (p=0.000), and cotrimoxazole (p=0.000) compared to Enterobacteriaceae, which were sensitive to third-generation cephalosporins. The organisms were more susceptible to carbapenems and chloramphenicol than resistant. ESBL-encoding genes (blaCTX-M, blaTEM, and blaSHV) were detected in 55 (75%) of the 73 Enterobacteriaceae that were resistant to third-generation cephalosporins. BlaCTX-M, was the most common ESBL-encoding gene identified with 50 (91%).
Conclusion: ESBL-producing Enterobacteriaceae are a predominant cause of bacteremia in hematologic cancer patients at UCI. The most common ESBL-encoding gene identified in the ESBL-PE was blaCTX-M. Resistance to imipenem and meropenem was low.
Keywords: antimicrobial resistance, extended spectrum beta-lactamases, enterobacteriaceae, CTX-M, Uganda, cancer
Introduction
Bacteremia is a cause of significant morbidity and mortality in patients with hematologic malignancies. This has been worsened over the past decades by an increase in the number of infections caused by multidrug resistant (MDR) strains, which have been associated with increased morbidity, mortality, and hospital costs.1 The emergence and spread of MDR bacteria make antibiotics inefficient and infectious diseases more difficult to treat. This threatens the ability to perform life-saving procedures, including providing chemotherapy to cancer patients.2 Among the organisms listed as the main cause of bacteremia are the extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-PE), including E. coli, K. pneumoniae, Enterobacter spp., Citrobacter spp., and Proteus spp.3–8 ESBL-PE are listed by the World Health Organization (WHO) in the critical group as one of the priority pathogens for research and development of new antibiotics.9 The Centers for Disease Control and Prevention (CDC) has listed them as serious threats. According to the CDC, cases of ESBL-PE have increased since 2012, with 197,400 estimated cases in hospitalized patients in 2017 and 9100 estimated deaths in the same year. The attributable health-care costs at that time were 1.2 billion US dollars.10 According to the WHO Global AMR and Use Surveillance System (GLASS) Report, low- and middle-income countries observed significantly higher rates of Enterobacteriaceae resistance to third-generation cephalosporins compared to high-income countries (58.3% vs 17.53%, respectively).11
Extended spectrum beta-lactamases (ESBLs) belong to the class A beta-lactamase Ambler classification or 2be functional classification scheme by Bush et al.12 They confer resistance to beta-lactam antibiotics including expanded spectrum cephalosporins and monobactams (aztreonam), but not to carbapenems (imipenem, meropenem, and ertapenem) and cephamycins (cefoxitin and cefotetan), and are inhibited by beta-lactamase inhibitors such as clavulanic acid.13 The main ESBL genes from which ESBLs are transcribed include blaSHV, blaTEM, and blaCTX-M, which is the most common in recent years.13
The genetic environment of the ESBL-encoding genes indicates that they are harbored on mobile genetic elements such as plasmids, transposons, and insertion sequences.13–15 This contributes to horizontal dissemination of enzymes within bacterial species and interspecies, thus spreading resistance. Additionally, in ESBL-producing Enterobacteriaceae (ESBL-PE), co-resistance has been observed between β-lactams and other antibiotics including fluoroquinolones, aminoglycosides, and trimethoprim/sulfamethoxazole, leading further to multidrug resistance.16 Furthermore, loss of the outer membrane porin and simultaneous production of CTX-M enzymes, and changes in amino acid substitutions in some CTX-M enzymes have been associated with carbapenem resistance.17,18 Resistance to carbapenems is a major setback in management of ESBL-PE since carbapenems are the treatment of choice for ESBL-PE.
Patients in intensive care units including cancer centers are at an increased risk of infections and mortality caused by ESBL-PE due to their requirement for prolonged hospitalization and frequent exposure to antibiotics.19–21 Moreover, among cancer patients, ESBL-PE infections are frequently observed in patients with hematologic malignancies.19,22 High-income countries have reported ESBL-PE rates in their different cancer populations ranging from as low as 6% to 34%.19,23,24 In Middle Eastern countries and Asia, the proportion of ESBL-PE isolates identified was 50.5% in India and 42.8% in Iran.25,26 Studies in China and Iran further demonstrated the high prevalence of blaCTX-M genes.26,27
Only a few cancer centers in Africa have demonstrated the phenotypic presence of ESBL among the isolated Enterobacteriaceae. In Egypt, the proportion of ESBL-producing bacteria among hematopoietic stem cell transplant pediatric patients with bloodstream infections was 45%.28 Another study in Egypt showed resistance to third-generation cephalosporins ranging from 67% to 94%, with a predominance of blaCTX-M genes.29 In Ethiopia, one study surprisingly showed only one-third of E. coli were resistant to third-generation cephalosporins, while another showed no resistance to ceftriaxone.30,31 In a study carried out at the Uganda Cancer Institute (UCI) in 2014, 41% of multidrug resistant Enterobacteriaceae isolated from febrile cancer patients were ESBL-PE; however, it did not determine the presence of ESBL-encoding genes.32
Assessing the local epidemiology of ESBL-PE especially in cancer units is necessary to not only inform hospital infection prevention and control strategies but also to guide prioritization of “last resort” antibiotics, which cover ESBL-PE infections. Therefore, given the limited data in the magnitude of ESBL-PE and ESBL genes responsible for resistance in cancer patients in Africa, the aim of this study was to determine the phenotypic resistance to third-generation cephalosporins, phenotypic extended spectrum beta-lactamase (ESBL) prevalence, and genotypic prevalence of ESBL-encoding genes blaCTX-M, blaTEM, and blaSHV in Enterobacteriaceae isolated from febrile neutropenic hematologic cancer patients with bacteremia at the UCI.
Materials and Methods
Study Design, Site, and Setting
This was a laboratory-based cross-sectional study conducted from November 2017 to December 2021 at the Makerere University College of Health Sciences (MakCHS) Clinical Microbiology Laboratory of the Department of Medical Microbiology (MUCML), and the Genomics and Molecular Biology Laboratory of the Department of Immunology & Molecular Biology, MakCHS. The Clinical Microbiology Laboratory is a College of Pathologists (CAP) accredited (No.7225593) laboratory, which processes human samples, identifies disease-causing organisms accurately and timely, and carries out antibiotic susceptibility testing, according to the Clinical and Laboratory Standards Institute (CLSI). The Genomics and Molecular Biology Laboratory of the Department of Immunology & Molecular Biology, MakCHS is facilitated to carry out basic and applied molecular studies in infectious diseases.
Study Population
We evaluated blood cultures collected as part of a prospective cohort study, which included hematologic cancer patients with febrile neutropenia and ESBL-PE bacteremia at UCI.
Sample Size
Using the Kish Leslie formula for cross-sectional studies, assuming a prevalence of ESBL-PE in the total population to be 5.3%32 and a margin error of 5% and 95% confidence, a minimum sample size of 77 was calculated for determining the prevalence of ESBL-PE in the total population of hematologic cancer patients with febrile neutropenia. We, therefore, included all hematologic cancer patients with febrile neutropenia that were enrolled in the prospective cohort study during the study period. Participants were enrolled consecutively throughout the study period.
Laboratory Methods
Blood Culture Processing
Blood samples obtained from febrile hematologic cancer patients from November 2017 to December 2021 at the UCI were processed in MUCML. The samples were processed in the BACTEC 9120 blood culture system according to manufacturer’s instructions and laboratory’s standard operating procedures (SOPs). Positive cultures were Gram stained, subcultured onto chocolate, blood, and MacConkey agars (Becton-Dickinson, New Jersey, USA), and incubated at 35–37ºC for 18–24 hr.
Bacterial Identification
We included E. coli, K. pneumoniae, and Enterobacter spp. isolates in this study. Pure isolates were identified using conventional biochemical methods including Gram stain, colony morphology on agar plates, triple sugar iron (TSI), sulphur indole and motility (SIM), citrate, urease tests, and oxidase tests (Becton-Dickinson, New Jersey, USA).33 The biochemical tests for each organism were as follows: E. coli: acid production in both slant and deep on triple sugar iron with gas production and no hydrogen sulfide, indole positive, citrate utilization negative, urease production negative, oxidase negative, and motile; K. pneumoniae: acid production in both slant and deep on triple sugar iron with gas production and no hydrogen sulfide, indole negative, citrate utilization positive, urease production positive, oxidase negative, and nonmotile; Enterobacter spp: acid production in both slant and deep on triple sugar iron with gas production and no hydrogen sulfide, indole negative, citrate utilization positive, urease production negative, oxidase negative, and motile.33,34 Pure colonies were stored at −80ºC until characterization of ESBL genotypes was carried out.
Antimicrobial Susceptibility Tests
Antimicrobial susceptibility tests and ESBL phenotype test were carried out using the Kirby Bauer disc diffusion method, and the zone diameters of inhibition were measured and interpreted according to the Clinical & Laboratory Standards Institute (CLSI) guidelines.35 Antibiotic discs (Becton-Dickinson, New Jersey, USA) used included amoxicillin-clavulanate (ANC) 20/10µg, piperacillin-tazobactam (TPZ) 100/10µg, ceftriaxone (CRO) 30µg, cefotaxime (CTX) 30µg, ceftazidime (CAZ) 30µg, cefepime (FEP) 30µg, aztreonam (AZT) 30µg, ertapenem (ERT) 10µg, imipenem (IMP) 10µg, meropenem (MER) 10µg, gentamycin (GM) 10µg, ciprofloxacin (CIP) 5µg, trimethoprim/sulfamethoxazole (SXT)1.25/23.75µg, and chloramphenicol (CAF) 30µg. The ESBL test was performed for isolates, which exhibited a zone of inhibition for at least one of the following: cefotaxime zone ≤27 mm, ceftriaxone ≤25 mm, ceftazidime ≤22 mm, and aztreonam ≤27 mm. The combination disc confirmatory method was used. Discs used in the test were ceftazidime (30µg), ceftazidime-clavulanate (30/10µg), cefotaxime (30µg), and cefotaxime-clavulanate (30/10µg). Evidence for the presence of ESBL production (a positive test) was determined by a ≥5 mm increase in zone diameter for ceftazidime or cefotaxime in combination with clavulanate vs the zone of diameter of ceftazidime or cefotaxime alone.35 Multidrug resistance (MDR) was defined as an isolate being non-susceptible to at least one agent in ≥3 antimicrobial categories. Extensively drug resistance (XDR) was defined as an isolate being non-susceptible to at least one agent in all but two or fewer antimicrobial categories. Pan drug resistance (PDR) was defined as an isolate being non-susceptible to all agents in all antimicrobial categories.36
Quality Control
Known quality control strains tested in parallel with the Enterobacteriaceae isolates included Escherichia coli ATCC 25922, Klebsiella pneumoniae ATCC 700603, Pseudomonas aeruginosa ATCC 27853. They were used to quality control the tests performed including Gram staining and quality and performance of culture media. Biochemical identification tests, and antimicrobial susceptibility tests.
Identification of ESBL Genotypes
The presence of the ESBL-encoding genes blaCTX-M, blaTEM, and blaSHV was determined using conventional PCR. DNA extraction was performed using the previously described Cetyltrimethyl Ammonium Bromide (CTAB) method at the Genomics and Molecular Biology Laboratory of the Department of Immunology & Molecular Biology, MakCHS.37 For each of the genes blaCTX-M, blaTEM, and blaSHV, Taq DNA Polymerase contained in 2X Taq master mix and respective primers were used for amplification in the respective amplification conditions (Table 1).
 |
Table 1 Primer Sequences, PCR Conditions, and Product Sizes for the blaCTX-M, blaTEM, blaSHV ESBL Genes |
The PCR products were analyzed on 0.8% agarose gel electrophoresis with ethidium bromide staining (0.5 µg/mL) for 60 min at 130 V. The bands were visualized on the Bio imager screen. The product sizes included 600 bp for blaCTX-M, 404 bp for blaTEM, and 900 bp for blaSHV (Figure 1). A negative extraction control (NEC), no template control (NC), and a positive control (PC) were used for quality control.
Statistical Analysis
Continuous data was described as median (IQR) and mean (SD). Categorical data were described as proportions. Comparison of the significance of difference in distribution was analyzed using chi-square test. P-values of ≤0.05 were considered to be statistically significant. Statistical analysis was performed using Stata Version 16.0
Results
Demographics
Two hundred and two hematologic cancer patients with febrile neutropenia at the UCI were included in the study. Median and mean ages of patients were 19 years (IQR: 10–30 years) and 22 years (SD 16), respectively; 119 (59%) patients were male; 127 (63%) were in the adult ward; and 155 (77%) had leukemia (acute or chronic). Of the patients with acute leukemia, 77 (54%) had acute myeloid leukemia (AML), while 65 (46%) had acute lymphocytic leukemia. Sixty (30%) of the participants had at least one febrile episode due to Enterobacteriaceae. Nine participants (4%) had polymicrobial bacteremia caused by Enterobacteriaceae. There were no significant differences between positive and negative cultures for the categories sex, ward, and cancer type (Table 2).
 |
Table 2 Characteristics of Patients Showing Positive Cultures Caused by Enterobacteriaceae for the Total Population |
Identification of Enterobacteriaceae Isolated
A total of 83 organisms were isolated. More than half (N=45, 54%) of the organisms were E. coli (Figure 2).
 |
Figure 2 Proportion of Enterobacteriaceae isolated from hematologic cancer patients. |
Antimicrobial Susceptibility Tests for Enterobacteriaceae Isolated
Overall, 79 (95%) of the Enterobacteriaceae isolated in this study were MDR, 47 (57%) were XDR and 3 (4%) were PDR. Specifically, 44/45 (98%) of E. coli, 30/32 (94%) of K. pneumoniae, and 5/6 (83%) of Enterobacter spp. were MDR, while 26/45 (58%) of E. coli, 18/32 (56%) of K. pneumoniae, and 3 (50%) of Enterobacter spp. were XDR. Only 1/45 (2%) of E. coli and 2/32 (6%) of K. pneumoniae were PDR. None of the Enterobacter spp. were PDR. Seventy-three of the 83 (88%) Enterobacteriaceae were resistant to third-generation cephalosporins. Forty (89%) of E. coli, 29 (91%) of K. pneumoniae, and 4 (67%) of Enterobacter spp. were resistant to third-generation cephalosporins. Overall, the ESBL phenotype was detected in 54/73 (74%) of Enterobacteriaceae that were resistant to third-generation cephalosporins. Among the organisms that were resistant to third-generation cephalosporins, 30/40 (75%) E. coli and 24/29 (83%) K. pneumoniae showed the ESBL phenotype. None of the Enterobacter spp. strains showed positive results for ESBL phenotypically (Table 3). Table 4 shows the comparison of antimicrobial susceptibility tests between Enterobacteriaceae sensitive to third-generation cephalosporins and resistant to third-generation cephalosporins with ESBL-positive phenotype. A significantly higher proportion of Enterobacteriaceae with ESBL-positive phenotype were resistant to piperacillin-tazobactam (p=0.024), gentamicin (p=0.000), ciprofloxacin (p=0.000), and cotrimoxazole (p=0.000) compared to Enterobacteriaceae, which were sensitive to third-generation cephalosporins. In both groups, the Enterobacteriaceae were more susceptible to carbapenems and chloramphenicol than resistant. Nineteen (26%) of Enterobacteriaceae that were resistant to third-generation cephalosporins were ESBL-negative. Of the 19 ESBL-negative Enterobacteriaceae that were resistant to third-generation cephalosporins, 18 (95%), 16 (84%), and 17 (89%), were resistant to ertapenem, imipenem, and meropenem, respectively.
 |
Table 3 Antimicrobial Susceptibility Tests for Enterobacteriaceae Isolates |
ESBL-Encoding Genes
Overall, ESBL-encoding genes (blaCTX-M, blaTEM, and blaSHV) were detected in 55 (75%) of the 73 Enterobacteriaceae that were resistant to third-generation cephalosporins. Twenty-six out of 40 (65%) E. coli, 26/29 (90%) K. pneumoniae, and 3/4 (75%) Enterobacter spp that were resistant to third-generation cephalosporins had ESBL-encoding genes. All three ESBL-encoding genes assessed were found in all three species. Most of the E. coli (15/26, 58%) and K. pneumoniae (21/26, 81%) had more than one ESBL-encoding gene. Only 1/3 (33%) of Enterobacter spp. had more than one ESBL-encoding gene (Table 5).
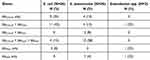 |
Table 5 ESBL-Encoding Genes Detected in Isolated Enterobacteriaceae |
Overall, 50 (91%), 38 (69%), and 23 (42%) of the 55 organisms with ESBL-encoding genes had blaCTX-M, blaTEM and blaSHV respectively. Twenty-four out of 26 (92%) E. coli had blaCTX-M. Twenty-five out of 26 (96%) K. pneumoniae had blaCTX-M. Only 1 (25%) of the three Enterobacter spp had blaCTX-M. (Figure 3).
 |
Figure 3 Proportion of blaCTX-M, blaTEM and blaSHV in isolated Enterobacteriaceae. |
Discussion
Bacteremia is a cause of significant morbidity and mortality in patients with hematologic malignancies, especially when caused by MDR strains. This has been worsened over the past decades by an increase in the number of infections caused by MDR strains, which have been associated with increased morbidity, mortality, and hospital costs.1 Among the organisms listed as the main causes of bacteremia are the ESBL-PE, which are listed as priority pathogens by the WHO. This study aimed to determine the phenotypic and genotypic prevalence of ESBL-determining genes found in Enterobacteriaceae isolated from hematologic cancer patients with bacteremia at UCI. Ninety-five percent of Enterobacteriaceae were MDR, the most common being E. coli. This was a slight increase from 85%, which was observed in a previous study carried out in the same institute.32 Similarly, high rates of resistance have been reported in other health facilities in Uganda and surrounding regions.34
In this study, the overall prevalence of ESBL-PE phenotype was 74%. We previously reported a prevalence of 41%; however, at that time the number of organisms were fewer than in the present study.32 The proportion of ESBL-PE in our study is higher than that found in intensive care unit (ICU) patients at Mulago Hospital, which observed the ESBL phenotype in 31% E. coli and K. pneumoniae.41 The number of organisms isolated in that study was few. Similarly, it was higher than 62% observed in ESBL-PE isolates obtained from samples collected from patients in various wards of Mulago Hospital.42 Moreover, that study only had 2 out of 3 (40%) blood samples that were ESBL phenotype positive. However, our ESBL proportion was lower than 81%, which was observed in patient population with surgical site infections at Mulago Hospital.34 In cancer centers in other LMICs, the proportion of ESBL was shown to range from 23% to 64.1% while in HIC, rates as high as 34% have been reported.19,23–26,28–31 MDR has been reported to be higher in LMIC compared to HIC.43 Among the drivers of ESBL production are overuse and misuse of third-generation cephalosporins in LMICs.44 Unlike HIC which have robust antimicrobial stewardship programs, LMICs lack adequate antimicrobial surveillance mechanisms.45 Dissemination of MDR strains including ESBL-PE negatively impacts patient outcomes by limiting therapeutic options available. Moreover, this demonstrates the need for robust infection prevention and control practices in cancer centers where majority of patients are immunocompromised.
More than half of the ESBL-PE in our study had resistance to gentamicin, ciprofloxacin, and trimethoprim/sulfamethoxazole. Different mechanisms of antimicrobial resistance have been demonstrated in Enterobacteriaceae including modifying enzymes, mutations, and presence of efflux pumps.46 However, studies have shown an association between ESBL phenotypes/genotypes and resistance to fluoroquinolones and aminoglycosides.16 In Ethiopia, a study showed that 63% of ESBL-PE were non-susceptible to gentamicin, 89.8% to trimethoprim-sulfamethoxazole, and 69% to ciprofloxacin.4 Similar findings have been observed in studies in Burkina Faso, Ghana, and Israel.47–49 This could be due to being encoded on a single plasmid that favors co-transmission. Co-resistance limits the number of available antibiotics, which work against ESBL-PE.
We also noted non-susceptibility of Enterobacteriaceae to carbapenems (ertapenem, imipenem, and meropenem), albeit the proportions of non-susceptibility were lower when compared to other antibiotics. Resistance to carbapenems was higher among isolates that were resistant to third-generation cephalosporins with ESBL phenotype negative compared to those that were resistant to third-generation cephalosporins with ESBL phenotype positive. In our previous study carried out at UCI, we found 36.4% E. coli and 57.1% K. pneumoniae to be resistant to a carbapenem.32 Previous studies have only tested imipenem and included few organisms. Other cancer centers in Africa and worldwide have also reported resistance to carbapenems. The treatment of choice for infections caused by ESBL-producers is carbapenems.50 Unfortunately, carbapenems are prohibitively expensive, especially for LMIC.51 Furthermore, the increased spread of carbapenem-resistant Enterobacteriaceae strains complicates the choice of therapy for these infections, leading to poor patient outcomes.
Notably, 65% of ESBL-PE were susceptible to chloramphenicol. A study carried out in India showed 68% of the MDR Gram-negative bacilli isolates were found to be sensitive to chloramphenicol.52 Chloramphenicol may play a role as a therapeutic option for MDR strains, especially in LMIC.52 With no new antibiotics currently available, there has been a shift in focus to reevaluate older antibiotics, including chloramphenicol.53,54 Chloramphenicol use was abandoned due to side effects including aplastic anemia and bone marrow suppression.55 Perhaps, this warrants its cautious use in a hematologic cancer unit. However, not only does it have good oral bioavailability and tissue penetration, but it is also relatively cheap and affordable.56,57
The most common ESBL-encoding gene we identified in this study was blaCTX-M followed by blaTEM and blaSHV which was the least identified. Few studies in Uganda have characterized the ESBL genes in Enterobacteriaceae. In Western Uganda, one study carried out in various patient populations showed a predominance of blaCTX-M (70%) compared to blaTEM (47%) and blaSHV (34%), while another in a different hospital showed a predominance of blaSHV (42%) compared to blaTEM (27.3%) and blaCTX-M (22.4%).58,59 Our findings are comparable with those from a cancer center in Egypt, which found a predominance of blaCTX-M (55.7%). However, unlike our study, blaSHV was more predominant than blaTEM (44.3% vs 31.4%).29 Furthermore, as seen in other studies, coproduction of all three genes was reported in our study.60 Importantly, when combined with other resistance mechanisms including loss of outer membrane porins, presence of ESBL genes, most especially blaCTX-M, has been associated with resistance to ertapenem.17,18 This could explain the resistance to ertapenem observed in our study compared to imipenem and meropenem.
This is among the few studies in SSA that have described the magnitude of ESBL-PE in a cohort of hematologic cancer patients who are at risk for an ESBL infection because of their weakened immune systems. However, the sample size of the ESBL-PE evaluated is small warranting continuous surveillance of MDR, XDR, and PDR bacteria over time. Furthermore, our study was limited to the three most reported ESBL-encoding genes (blaCTX-M, blaTEM, blaSHV). We did not investigate the presence of other ESBL genes. We also did not determine other possible resistance mechanisms responsible for resistance to third-generation cephalosporins, such as AmpC. While we demonstrated possible presence of co-resistance between ESBL-PE and aminoglycosides, fluoroquinolones, and sulfonamide, as well as resistance to carbapenems, it is important to determine the molecular resistance mechanisms responsible for the observed phenotype as a step towards genomic surveillance.
Conclusion
Our study shows the predominance of ESBL-PE as a cause of bacteremia in hematologic cancer patients at the UCI. The most common ESBL-encoding gene identified in the ESBL-PE was blaCTX-M. Resistance to imipenem and meropenem was low, and therefore, carbapenems remain the recommended drug of choice for ESBL-PE at the UCI. We recommend continuous surveillance over time to assess the clinical features, risk factors, and outcomes of ESBL-PE bacteremia in immunosuppressed cancer patients. In addition, describing the genetic environment of ESBL-PE, including exploring associated resistance mechanisms, sequence types, and relatedness is important to inform infection prevention and control and antimicrobial stewardship protocols in cancer centers, which rely heavily on antibiotics for supportive management especially for patients who are on chemotherapy.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author.
Ethics Approval and Informed Consent
The study was conducted in accordance with the Declaration of Helsinki. The study received ethical and scientific approval from the Institutional Review Board (IRB) of the School of Biomedical Sciences (SBS), College of Health Sciences, Makerere University (SBS 396); from the Uganda National Council of Science and Technology (HS 2217); and from Fred Hutchinson Cancer Research Center IRB (FHCC #: 8433). Informed consent was obtained from all subjects involved in the study. Parents of children under 18 years provided informed consent.
Acknowledgments
The authors would like to acknowledge and thank Uganda Cancer Institute, Hutchison Centre Research Institute Uganda, Makerere University clinical Microbiology Laboratory, and Genomics and Molecular Biology Laboratory of the Department of Immunology & Molecular Biology for their administrative and technical support.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by D43 TW009759 NCI Training Grant; UCI-AfDB Training Scholarship (ADM 342/411/01); and Alliance for Global Health and Science Small Grants award, Center for Emerging & Neglected Diseases, University of California, Berkeley.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Murray CJL, Ikuta KS, Sharara F, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. doi:10.1016/S0140-6736(21)02724-0
2. Salam MA, Al-Amin MY, Salam MT, et al. Antimicrobial Resistance: a Growing Serious Threat for Global Public Health. Healthcare. 2023;11(13). doi:10.3390/healthcare11131946
3. Coudron PE, Moland ES, Sanders CC. Occurrence and detection of extended-spectrum beta-lactamases in members of the family Enterobacteriaceae at a veterans medical center: seek and you may find. J Clin Microbiol. 1997;35(10):2593–2597. doi:10.1128/jcm.35.10.2593-2597.1997
4. Teklu DS, Negeri AA, Legese MH, Bedada TL, Woldemariam HK, Tullu KD. Extended-spectrum beta-lactamase production and multi-drug resistance among Enterobacteriaceae isolated in Addis Ababa, Ethiopia. Antimicrob Resist Infect Control. 2019;8(1):39. doi:10.1186/s13756-019-0488-4
5. Kayastha K, Dhungel B, Karki S, et al. Extended-Spectrum β-Lactamase-Producing Escherichia coli and Klebsiella Species in Pediatric Patients Visiting International Friendship Children’s Hospital, Kathmandu, Nepal. Infectious Dis. 2020;13:1178633720909798. doi:10.1177/1178633720909798
6. Vance MK, Cretella DA, Ward LM, Vijayvargiya P, Garrigos ZE, Wingler MJB. Risk Factors for Bloodstream Infections Due to ESBL-Producing Escherichia coli, Klebsiella spp., and Proteus mirabilis. Pharmacy. 2023;11(2):74. doi:10.3390/pharmacy11020074
7. Tzelepi E, Giakkoupi P, Sofianou D, Loukova V, Kemeroglou A, Tsakris A. Detection of extended-spectrum beta-lactamases in clinical isolates of Enterobacter cloacae and Enterobacter aerogenes. J Clin Microbiol. 2000;38(2):542–546. doi:10.1128/JCM.38.2.542-546.2000
8. Dziri R, Klibi N, Alonso CA, et al. Characterization of extended-spectrum β-lactamase (ESBL)-producing Klebsiella, Enterobacter, and Citrobacter obtained in environmental samples of a Tunisian hospital. Diagnostic Microbiol Infectious Dis. 2016;86(2):190–193. doi:10.1016/j.diagmicrobio.2016.07.013
9. Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–327. doi:10.1016/S1473-3099(17)30753-3
10. Available from: https://www.cdc.gov/drugresistance/pdf/threats-report/esbl-508.pdf.
11. WHO. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report 2022. Geneva: World Health Organization; 2022.
12. Bush K, Jacoby GA. Updated functional classification of beta-lactamases. Antimicrob Agents Chemother. 2010;54(3):969–976. doi:10.1128/AAC.01009-09
13. Castanheira M, Simner PJ, Bradford PA. Extended-spectrum β-lactamases: an update on their characteristics, epidemiology and detection. JAC-Antimicrob Resist. 2021;3(3). doi:10.1093/jacamr/dlab092
14. Cantón R, González-Alba JM, Galán JC. CTX-M Enzymes: origin and Diffusion. Front Microbiol. 2012;3:110. doi:10.3389/fmicb.2012.00110
15. Awosile BB, Agbaje M. Genetic environments of plasmid-mediated bla CTXM-15 beta-lactamase gene in Enterobacteriaceae from Africa. Microbiol Res. 2021;12(2):383–394. doi:10.3390/microbiolres12020026
16. Masoud SM, El-Baky RM A, Aly SA, Ibrahem RA. Co-Existence of Certain ESBLs, MBLs and Plasmid Mediated Quinolone Resistance Genes among MDR E. coli Isolated from Different Clinical Specimens in Egypt. Antibiotics. 2021;10(7):835. doi:10.3390/antibiotics10070835
17. Jacoby GA, Mills DM, Chow N. Role of beta-lactamases and porins in resistance to ertapenem and other beta-lactams in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2004;48(8):3203–3206. doi:10.1128/AAC.48.8.3203-3206.2004
18. Poulou A, Voulgari E, Vrioni G, et al. Outbreak caused by an ertapenem-resistant, CTX-M-15-producing Klebsiella pneumoniae sequence type 101 clone carrying an OmpK36 porin variant. J Clin Microbiol. 2013;51(10):3176–3182. doi:10.1128/JCM.01244-13
19. Gudiol C, Calatayud L, Garcia-Vidal C, et al. Bacteraemia due to extended-spectrum beta-lactamase-producing Escherichia coli (ESBL-EC) in cancer patients: clinical features, risk factors, molecular epidemiology and outcome. J Antimicrob Chemother. 2010;65(2):333–341. doi:10.1093/jac/dkp411
20. Kallel H, Houcke S, Resiere D, et al. Epidemiology and Prognosis of Intensive Care Unit-Acquired Bloodstream Infection. Am J Trop Med Hyg. 2020;103(1):508–514. doi:10.4269/ajtmh.19-0877
21. Shamsrizi P, Gladstone BP, Carrara E, et al. Variation of effect estimates in the analysis of mortality and length of hospital stay in patients with infections caused by bacteria-producing extended-spectrum beta-lactamases: a systematic review and meta-analysis. BMJ Open. 2020;10(1):e030266. doi:10.1136/bmjopen-2019-030266
22. Marin M, Gudiol C, Ardanuy C, et al. Bloodstream infections in neutropenic patients with cancer: differences between patients with haematological malignancies and solid tumours. J Infect. 2014;69(5):417–423. doi:10.1016/j.jinf.2014.05.018
23. Szymankiewicz M, Stefaniuk E, Baraniak A, Nowikiewicz T. Clinical and Molecular Findings of Infections Caused by Extended-Spectrum β-Lactamase-Producing Enterobacterales in Patients with Solid Tumors: a Single-Center Study. Microbial Drug Resistance. 2021;27(11):1470–1481. doi:10.1089/mdr.2020.0530
24. Mikulska M, Viscoli C, Orasch C, et al. Aetiology and resistance in bacteraemias among adult and paediatric haematology and cancer patients. J Infection. 2014;68(4):321–331. doi:10.1016/j.jinf.2013.12.006
25. Bhat S, Muthunatarajan S, Mulki SS, Archana Bhat K, Kotian KH. Bacterial Infection among Cancer Patients: analysis of Isolates and Antibiotic Sensitivity Pattern. Int J Microbiol. 2021;2021:8883700. doi:10.1155/2021/8883700
26. Abbasi Montazeri E, Khosravi AD, Saki M, Sirous M, Keikhaei B, Seyed-Mohammadi S. Prevalence of Extended-Spectrum Beta-Lactamase-Producing Enterobacteriaceae Causing Bloodstream Infections in Cancer Patients from Southwest of Iran. Infect Drug Resist. 2020;13:1319–1326. doi:10.2147/IDR.S254357
27. Zhang Q, Gao HY, Li D, et al. Clinical outcome of Escherichia coli bloodstream infection in cancer patients with/without biofilm formation: a single-center retrospective study. Infect Drug Resist. 2019;12:359–371. doi:10.2147/IDR.S192072
28. Youssef A, Hafez H, Madney Y, et al. Incidence, risk factors, and outcome of blood stream infections during the first 100 days post-pediatric allogeneic and autologous hematopoietic stem cell transplantations. Pediatric Transplantation. 2020;24(1):e13610. doi:10.1111/petr.13610
29. Tohamy ST, Aboshanab KM, El-Mahallawy HA, El-Ansary MR, Afifi SS. Prevalence of multidrug-resistant Gram-negative pathogens isolated from febrile neutropenic cancer patients with bloodstream infections in Egypt and new synergistic antibiotic combinations. Infect Drug Resist. 2018;11:791–803. doi:10.2147/IDR.S163293
30. Fentie A, Wondimeneh Y, Balcha A, Amsalu A, Adankie BT. Bacterial profile, antibiotic resistance pattern and associated factors among cancer patients at University of Gondar Hospital, Northwest Ethiopia. Infect Drug Resist. 2018;11:2169–2178. doi:10.2147/IDR.S183283
31. Worku M, Belay G, Tigabu A. Bacterial profile and antimicrobial susceptibility patterns in cancer patients. PLoS One. 2022;17(4):e0266919. doi:10.1371/journal.pone.0266919
32. Lubwama M, Phipps W, Najjuka CF, et al. Bacteremia in febrile cancer patients in Uganda. BMC Res Notes. 2019;12(1):464. doi:10.1186/s13104-019-4520-9
33. Procop GW, Church DL, Hall GS, Janda WM. Koneman’s Color Atlas and Textbook of Diagnostic Microbiology. Jones & Bartlett Learning; 2020.
34. Seni J, Najjuka CF, Kateete DP, et al. Antimicrobial resistance in hospitalized surgical patients: a silently emerging public health concern in Uganda. BMC Res Notes. 2013;6(1):298. doi:10.1186/1756-0500-6-298
35. CLSI. Performance Standards for Antimicrobial Susceptibility Testing.
36. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infection. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
37. William S, Feil H, Copeland A. Bacterial genomic DNA isolation using CTAB. Sigma. 2012;50:6876.
38. Boyd DA, Tyler S, Christianson S, et al. Complete nucleotide sequence of a 92-kilobase plasmid harboring the CTX-M-15 extended-spectrum beta-lactamase involved in an outbreak in long-term-care facilities in Toronto, Canada. Antimicrob Agents Chemother. 2004;48(10):3758–3764. doi:10.1128/AAC.48.10.3758-3764.2004
39. Bali EB, Acik L, Sultan N. Phenotypic and molecular characterization of SHV, TEM, CTX-M and extended-spectrum beta-lactamase produced by Escherichia coli, Acinobacter baumannii and Klebsiella isolates in a Turkish hospital. Afr J Microbiol Res. 2010;4(8):650–654.
40. Rafiee R, Eftekhar F, Tabatabaii SA. Extended-Spectrum Beta-Lactamases in Cystic Fibrosis Isolates of Klebsiella pneumoniae. Jundishapur J Microbiol. 2018;11(1):56.
41. Agaba P, Tumukunde J, Tindimwebwa JVB, Kwizera A. Nosocomial bacterial infections and their antimicrobial susceptibility patterns among patients in Ugandan intensive care units: a cross sectional study. BMC Res Notes. 2017;10(1):349. doi:10.1186/s13104-017-2695-5
42. Kateregga JN, Kantume R, Atuhaire C, Lubowa MN, Ndukui JG. Phenotypic expression and prevalence of ESBL-producing Enterobacteriaceae in samples collected from patients in various wards of Mulago Hospital, Uganda. BMC Pharmacol Toxicol. 2015;16(1):14. doi:10.1186/s40360-015-0013-1
43. El-Mahallawy H, Sidhom I, El-Din NH, Zamzam M, El-Lamie MM. Clinical and microbiologic determinants of serious bloodstream infections in Egyptian pediatric cancer patients: a one-year study. Int j Infectious Dis. 2005;9(1):43–51. doi:10.1016/j.ijid.2003.11.010
44. Wacharachaisurapol N, Jitrungruengnij N, Janewongwirot P, et al. High prescribing rates of third-generation cephalosporins in children hospitalized with acute lower respiratory infections at a university hospital. Inter J Infect Dis. 2021;102:369–374. doi:10.1016/j.ijid.2020.10.105
45. Shamas N, Stokle E, Ashiru-Oredope D, Wesangula E. Challenges of implementing antimicrobial stewardship tools in Low to Middle Income Countries (LMICs). Infect Prevention Practice. 2023;5(4):100315. doi:10.1016/j.infpip.2023.100315
46. Ruppé É, Woerther PL, Barbier F. Mechanisms of antimicrobial resistance in Gram-negative bacilli. Ann Intens Care. 2015;5(1):61. doi:10.1186/s13613-015-0061-0
47. Schwaber MJ, Navon-Venezia S, Schwartz D, Carmeli Y. High levels of antimicrobial coresistance among extended-spectrum-beta-lactamase-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2005;49(5):2137–2139. doi:10.1128/AAC.49.5.2137-2139.2005
48. Ouedraogo AS, Sanou M, Kissou A, et al. High prevalence of extended-spectrum ß-lactamase producing Enterobacteriaceae among clinical isolates in Burkina Faso. BMC Infect Dis. 2016;16:326. doi:10.1186/s12879-016-1655-3
49. Obeng-Nkrumah N, Twum-Danso K, Krogfelt KA, Newman MJ. High levels of extended-spectrum beta-lactamases in a major teaching hospital in Ghana: the need for regular monitoring and evaluation of antibiotic resistance. American JTrop Med Hyg. 2013;89(5):960–964. doi:10.4269/ajtmh.12-0642
50. Freifeld AG, Bow EJ, Sepkowitz KA, et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin Infectious Dis. 2011;52(4):e56–93. doi:10.1093/cid/cir073
51. Cox JA, Vlieghe E, Mendelson M, et al. Antibiotic stewardship in low- and middle-income countries: the same but different? Clin Microbiol Infect. 2017;23(11):812–818. doi:10.1016/j.cmi.2017.07.010
52. Sood S. Chloramphenicol - A Potent Armament Against Multi-Drug Resistant (MDR) Gram Negative Bacilli? J Clin Diagn Res. 2016;10(2):65.
53. Abdul Rahim N, Cheah S-E, Johnson MD, et al. Synergistic killing of NDM-producing MDR Klebsiella pneumoniae by two ‘old’ antibiotics—polymyxin B and chloramphenicol. J Antimicrob Chemother. 2015;70(9):2589–2597. doi:10.1093/jac/dkv135
54. Jonsson M. Is chloramphenicol the drug of choice for the treatment of enteric fever? Infection. 1974;2(3):145–151. doi:10.1007/BF01642235
55. Burton CW, Williams DM. Aplastic Anemia Associated with Parenteral Chloramphenicol: review of 10 Cases, including the Second Case of Possible Increased Risk with Cimetidine. Rev Infect Dis. 1988;10(5):1048–1051. doi:10.1093/clinids/10.5.1048
56. Ambrose PJ. Clinical pharmacokinetics of chloramphenicol and chloramphenicol succinate. Clin. Pharmacokinet. 1984;9(3):222–238. doi:10.2165/00003088-198409030-00004
57. Madhavan H, Bagyalakshmi R. Farewell, chloramphenicol? Is this true?: a review. J Microbiol Biotechnol. 2013;3:13–26.
58. Moses A, Bwanga F, Boum Y, Bazira J. Prevalence and Genotypic Characterization of Extended-Spectrum Beta-Lactamases Produced by Gram Negative Bacilli at a Tertiary Care Hospital in Rural South Western Uganda. Br Microbiol Res J. 2014;4(12):1541–1550. doi:10.9734/BMRJ/2014/9792
59. Mbyemeire H, Ssekatawa K, Kato CD, Wampande EM. Molecular characterization and distribution of cephalosporin resistance determinants in Escherichia coli and Klebsiella pneumoniae isolated from patients attending Kampala International University Teaching Hospital in Bushenyi, Western Uganda. Alexandria J Med. 2021;57(1):205–214. doi:10.1080/20905068.2021.1952821
60. Kaur M, Aggarwal A. Occurrence of the CTX-M, SHV and the TEM Genes Among the Extended Spectrum β-Lactamase Producing Isolates of Enterobacteriaceae in a Tertiary Care Hospital of North India. J Clin Diagn Res. 2013;7(4):642–645. doi:10.7860/JCDR/2013/5081.2872
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


