Back to Journals » Infection and Drug Resistance » Volume 14
COVID-19 Vaccination Acceptance and Its Associated Factors in Sodo Town, Wolaita Zone, Southern Ethiopia: Cross-Sectional Study
Authors Mesele M
Received 21 May 2021
Accepted for publication 15 June 2021
Published 24 June 2021 Volume 2021:14 Pages 2361—2367
DOI https://doi.org/10.2147/IDR.S320771
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Molalegn Mesele
School of Midwifery, College of Health Science and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
Correspondence: Molalegn Mesele Tel +251-932214732
Email [email protected]
Background: Coronavirus disease (COVID-19) pandemic has still affected many countries around the world. The COVID-19 vaccine has been presented as the perfect solution for solving the current pandemic. Understanding the willingness of the community to receive the COVID-19 vaccine will help in the development and implementation of effective COVID-19 vaccination promotion programs. The aim of this study was to assess the COVID-19 vaccination acceptance and its associated factors in Sodo town, Wolaita zone, Southern Ethiopia.
Methods: A community-based cross-sectional study was conducted among 415 participants in Wolaita Sodo, from April 1 to 30, 2021. To collect data, structured interviewer administered questionnaire was used. A p-value ≤ 0.05 in a multivariable logistic regression model was considered statistically significant.
Results: Of 415 participants, 189 (45.5%) of them accepted of COVID-19 vaccines if available. Sex (AOR=2.15, 95% CI: 1.29, 3.56), educational status (AOR=3.09, 95% CI: 1.50, 6.37), mass media (AOR=1.97, 95% CI: 1.06, 3.63), received any vaccination during childhood (AOR=5.16, 95% CI: 2.44, 10.92), family members have been diagnosed with COVID-19 (AOR=4.40, 95% CI: 2.1, 9.25), friends have been diagnosed with COVID-19 (AOR=3.91, 95% CI: 1.52, 10.04), and respondents have tested for COVID-19 (AOR=4.40, 95% CI: 1.70, 11.36) were significantly associated with acceptance of COVID-19 vaccine.
Conclusion: The prevalence of COVID-19 vaccination acceptance was law. To enhance the acceptance of COVID-19 vaccine, the government with different stakeholders should strengthen public education using mass media about the advantage of getting COVID-19 vaccination.
Keywords: acceptance, COVID-19, vaccine, Sodo town, Ethiopia
Introduction
After the World Health Organization (WHO) declared COVID-19 an international public health emergency (pandemic) on February 11, 2020, COVID-19 vaccines were produced within a year. COVID-19 vaccines were developed in the shortest time in vaccine history, due to remarkable determination in vaccine research, development, and manufacturing.1 Vaccines against COVID-19 are considered very important to prevent and manage COVID-19 since vaccination is one of the most active and cost-effective health strategies for preventing infectious diseases.2,3
More than 200 additional vaccine candidates are being developed, with more than 60 of them in clinical trials. COVAX is a component of the ACT Accelerator, which WHO and collaborators launched in 2020 with aims to bring the COVID-19 pandemic’s acute phase to an end.4 Although substantial progress is being made, there are still significant obstacles in the way of a possible COVID-19 vaccine, one of which is public acceptance. Vaccine acceptance reflects the general public’s overall understanding of disease risk, vaccine attitudes, and demand, all of which are important for vaccinations to achieve high vaccination coverage rates, especially for newly emerging infectious diseases.5–7
COVID-19 not only has a significant health impact but it also has a significant economic impact that should not be underestimated.8 It has resulted in a significant decline in workforces and a rise in global unemployment. These negative consequences have prompted pharmaceutical firms to produce a vaccine as soon as possible. Several vaccines to prevent COVID-19 infection were approved in December 2020.8,9
Ethiopian authorities choose to employ the Astra Zeneca COVID-19 vaccination through the COVAX Facility. On March 7, 2021, Ethiopia received 2.184 million doses of COVID-19 vaccination.10 On March 13, 2021, the Ethiopian Ministry of Health officially launched the COVID-19 vaccine at a high-level national event held at Eka Kotebe COVID-19 Hospital, where front-line health workers were vaccinated to kick of the vaccination campaign.11
Hopes to reduce the negative repercussions of COVID-19 was largely dependent on the timely development of efficacious vaccines and their distribution in an equitable manner.12,13 The COVID-19 vaccination trials’ rapid development and approval phases resulted in the emergency-use authorization of many safe and successful vaccines, at least for the time being.14–16 In the midst of the pandemic crisis, the deployment of COVID-19 vaccines was a ray of hope. However, having access to vaccine programs is one thing, and successfully implementing a mass vaccination campaign is another.17 COVID-19 vaccination could be jeopardized by issues such as mass production, global distribution, and cost.18
Furthermore, there are some ambiguities concerning some aspects of the COVID-19 vaccine, such as: Uncertainty about long-term security and the need for regular reformulation amid evidence of SARS-CoV-2 evolution and the appearance of genetic variants.19,20 Despite this, people continue to have doubts about vaccine safety and efficacy, including the durability of COVID-19 defense, as many cases of reinfection have been recorded.21,22 Vaccine hesitancy and resistance are major issues around the world, causing the World Health Organization (WHO) to list them among the top ten health risks for 2019.23 Vaccine apprehension has been linked to religious values, personal beliefs, and safety issues based on widespread misconceptions, such as the connection between vaccines and autism, brain injury, and other disorders, according to various reports.24
Understanding the communities preparedness to receive a COVID-19 vaccination, as well as the major factors affecting their acceptance of the vaccination, would contribute to the development and implementation of efficient COVID-19 vaccination promotion strategies, as well as the current alarming increase in infection. In Ethiopia, this research is the first study conducted to assess the acceptance of vaccination against COVID-19 in my knowledge; no previously published work has been in Ethiopia even if the vaccine does become available. The objective of this study was to measure the level of acceptance of COVID-19 vaccination and its associated factors in Sodo town, Wolaita zone, Southern Ethiopia.
Methods and Materials
Study Setting and Design
In Sodo town, a community-based cross-sectional study was conducted from April 1 to 30, 2021. Sodo town has a population of 250,521. Males account for 79,871 (52%) of the population, while females account for 73,650 (48%). The city has three sub-cities, 18 kebeles, three health centers, one Ministry of health-owned hospital, and one private hospital. The city is 160 km from Hawassa, the regional city of South Nation Nationality of people regional state, and 327 km from Addis Ababa, Ethiopia’s capital city.25
Source and Study Population
All individuals aged ≥18 years who lived in Sodo town, Wolaita zone, Southern Ethiopia, were source population and all randomly selected individuals were the study population.
Inclusion and Exclusion Criteria
Individuals aged ≥18 years were included in this study, and people who were seriously ill during the period of data collection and those not willing to participate in the study were excluded.
Sample Size Determination
Since there has been no prior research on acceptance COVID-19 vaccine in Ethiopia, the best estimate (P) would be 50%. With the following considerations in mind, sample size was calculated using the single population proportion formula with a marginal error of 0.05, a 95% confidence interval, and a p-value of 0.5. Assume a 10% non-response rate for this study, the final sample size of 424 participants was estimated.
Sampling Procedure
Six kebele were chosen from a total of 18 kebele in Sodo town using a simple random sampling technique by lottery method. A systematic random sampling procedure was used to choose households from the six kebele that were chosen; the first household was selected using a simple random sampling technique, and then others were selected at regular intervals until the required sample size was reached. If there were more than one individual who fulfills the inclusion criteria, one respondent was selected with simple random sampling technique.
Study Variables
The dependent variable in this study was the intention to accept COVID-19 vaccines. Structured interviewer administers questionnaire was used to collect data. There were three components of the independent variables: 1) socio-demographic factors such as age, gender, religion, educational attainment, and marital status, and place of residence. 2) COVID-19 experience includes, contact with a COVID-19 patient, a member of the household who has been diagnosed with COVID-19, relatives who have been diagnosed with COVID-19, have you been vaccinated for COVID-19, heard about the COVID-19 vaccine, friends who have been diagnosed with COVID-19. 3) Reasons for non-acceptance of COVID-19 vaccines. Questions were adopted from previously published studies.26
Data Processing and Analysis
Before being moved to SPSS window version 21 for analysis, the data was coded, cleaned, recoded, and entered into epi-data version 3.1. A table and statement were used to present the data. The relationship between independent and dependent variables was investigated using bivariate logistic regression analysis. To control for possible confounding, all variables in the bivariate logistic regression model with a p-value <0.25 were added to the multivariable logistic regression model, and variables in the multiple logistic regression model with a p-value ≤0.05 were considered statistically significant.
Result
Socio-Demographic Characteristics
There were a total of 415 who participated in this study with 98% response rate. The mean (± Standard Deviation [SD]) of respondents was 28.2 (±7). Of the 415 respondents more than half 219 (52.8%) were aged 18–29. The majority of participants were male 231 (55.6%) and 193 (46.5%) of participants protestant religious followers. Regarding educational attainment, the highest proportion 199 (48%) of respondents had college and above education level. Related marital status, majority 301 (72.5%) married (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Respondents in Sodo town, Southern Ethiopia, 2021 (N=415) |
Participants Experience with COVID-19
The majority of the respondents 332 (80%) had never contacted with COVID-19 patient. Three hundred and sixty-two (87.2%) of the 415 respondents said no one in their household had been diagnosed with COVID-19, and 9 of 10 (90.4%) said that no relatives had been diagnosed with COVID-19 (Table 2).
 |
Table 2 Participants’ Experience with COVID-19 in Sodo town, Southern Ethiopia, 2021 (N=415) |
Acceptance of COVID-19 Vaccines
Out of 415 people who took part in the survey, less than half (45.5%) said they would accept COVID-19 vaccines if available, and more than half (54.5%) said they would not.
Reasons for Non-Acceptance of COVID-19 Vaccines
Of the 226 participants who were unwilling to accept the COVID-19 vaccines, 134 (59.27%) and 48 (21.2%) were concerned about insufficient data about the vaccines and fear adverse effects of the vaccine (Table 3).
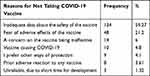 |
Table 3 Reasons for Non-Acceptance of COVID-19 Vaccines Among Respondents in Sodo town, Southern Ethiopia, 2021 (N=415) |
Factors Associated with Acceptance of COVID-19 Vaccines
Sex, educational status, use of mass media, received any vaccine during childhood, member of household diagnosed with COVID-19, friends have been diagnosed with COVID-19, and have tested for COVID-19 were all found to be significantly correlated with acceptance of the COVID-19 vaccines in a multivariable logistic regression. COVID-19 vaccines were more likely to be accepted by males than females (AOR=2.15, 95% CI: 1.29, 3.56). Another factor linked to COVID-19 vaccine acceptance was one’s educational level. Those with a college or higher education degree were three times more likely than those with a primary education to accept the COVID-19 vaccine (AOR=3.09, 95% CI: 1.50, 6.37). Respondents who had access to the media were more likely to accept the COVID-19 vaccine than those who did not (AOR=1.97, 95% CI: 1.06, 3.63). Participants who received any vaccine during childhood were more likely to accept COVID-19 vaccine (AOR=5.16, 95% CI: 2.44, 10.92) than who did not receive any vaccine during childhood. Participants who had a family member diagnosed with COVID-19 were more likely to accept the vaccine (AOR=4.40, 95% CI: 2.10, 9.25) than those who did not have a family member diagnosed with COVID-19. Participants whose friends had been diagnosed with COVID-19 were more likely than those whose friends had not been diagnosed with COVID-19 to accept the vaccine (AOR=3.91, 95% CI: 1.52, 10.04). Respondents who had tested for COVID-19 were more likely to accept the vaccine than those who had not tested for COVID-19 (AOR=4.40, 95% CI: 1.70, 11.36) (Table 4).
 |
Table 4 Factors Associated with Acceptance of COVID-19 Vaccine in Sodo town, Southern Ethiopia, 2021 (N=415) |
Discussion
COVID-19 vaccines have been launched “the perfect cure” for bringing the current pandemic to an end. Several clinical trials with positive results have recently been released, leading to a number of countries approving specific vaccines for use in Ethiopia vaccination programs.11 One of the first estimates of COVID-19 vaccine acceptance in Ethiopia is presented in this study. These findings may be used to predict COVID-19 vaccines acceptance.
The result of the current study reveals that, 189 (45.5%) of participants willing to accept COVID-19 vaccines if available and more than half 226 (54.5%) indicated non-acceptance of COVID-19 vaccines if available. The result of this study was in line with a study done in four states in the United States of America 44.9%.27 The acceptability of the COVID-19 vaccine was higher in this study than in other countries, with 36.8% in Jordan,28 37.2% in Hong Kong,29 and 34.9% among Jordanian university students.30 The probable reason for the discrepancy between the current result and other studies may be due to socio-demographic, socio-economic, or time differences.
This study’s finding was lower than those of other studies conducted around the world. Knowledge, attitude, and practice towards COVID-19 vaccination acceptance in West India (64.5%),31 and three researches looked at public acceptance of COVID-19 in China (83.3–91.3).32 COVID-19 vaccine was accepted by 79% of the people in Israel.33 A global survey of potential acceptance of a COVID-19 vaccine with 71.5%,31 63.5% respondents in the United Kingdom willing to accept COVID-19 vaccine if available,34 and more than half (52.2%) of the respondents accepts the COVID-19 vaccine in China.35
According to the results of this study, men were more likely than women to accept the COVID-19 vaccine if it was available. Males are more likely than females to accept COVID-19 vaccines, according to other observational studies.26,32,33 The educational level was also a significant factor in COVID-19 vaccine acceptance. Participants with a college diploma or higher were more likely to accept the COVID-19 vaccine. The possible reason might be, those with a higher level of education (college and above) would have a better chance of accessing knowledge and comprehending it and as a result they will respond and accept the COVID-19 vaccine. Respondents who had access to the mainstream media were more likely to accept the COVID-19 vaccine than those who did not. Most of the time, the COVID-19 vaccine was promoted through the media; those who were informed about the vaccine had a better chance of accepting it, as some respondents said that they do not take the vaccine because there is insufficient information about vaccine and its safety.
When compared to participants who had not received any vaccination during childhood, respondents who had received any vaccination during childhood were more likely to accept the COVID-19 vaccine if it became available. One possible reason is that people who have received any vaccine have gained more experience and knowledge about the benefits of vaccination; that help participants accept the vaccine to protect them from COVID-19. In comparison to respondents whose member of the household was not diagnosed with COVID-19, the current study showed that participants whose member of the household was diagnosed with COVID-19 were more likely to accept the COVID-19 if it was available.
Another significant factor was that participants’ friends who had been diagnosed with COVID-19 were more likely than participants’ friends who had not been diagnosed with COVID-19 to accept the COVID-19 vaccine if it became available. Participants who were tested for COVID-19 were more likely than those who were not to accept the vaccine if it became available. Participants who were tested for COVID-19, participants whose members of the household tested for COVID-19, and respondents’ friends who have been diagnosed with COVID-19 may have learned about COVID-19 and its effects on human health, prompting them to seek protection from the COVID-19 vaccine.
The findings of the current study showed that participants were unwilling to accept the COVID-19 vaccine due to the main reason; concerns about insufficient data about the vaccine’s and fear of adverse effects. The results are consistent with those of other research.26,32–36 In a report in Ghana, for example, insufficient evidence about the vaccine’s safety and vaccine side effects were the key reasons for people refusing to accept COVID-19 vaccines.26
The limitation of this study is that it is cross-sectional in nature, making it difficult to draw long-term conclusions. The results of this research were solely based on quantitative techniques, with no other tools such as focus group discussions or in-depth interviews being used to supplement the findings.
Conclusion
The findings of this study suggest that the acceptance of a COVID-19 vaccine was low. Acceptance of the COVID-19 vaccine was significantly correlated with sex, educational status, use of mass media, received any vaccine during childhood, member of household diagnosed with COVID-19, friends diagnosed with COVID-19, and have tested for COVID-19. To increase public acceptance of the COVID-19 vaccine, the government should work with various stakeholders implementing public education through the mass media about the benefits of getting the COVID-19 vaccine.
Data Sharing Statement
All data are available for this study.
Ethical Consideration
Ethical clearance was obtained from the Ethical review board of Wolaita Sodo University College of Health Sciences and Medicine. Informed consent was obtained from participants, and this study was conducted in accordance with the declaration of Helsinki. Anonymity and confidentiality were ensured.
Acknowledgment
I would like to express my heartfelt thanks for Wolaita Sodo University, all individual for their contribution and cooperation.
Funding
This study did not obtain any particular funding from government, commercial, or non-profit funding agencies.
Disclosure
The author reports no competing interests in this work.
References
1. Glanville D. COVID-19 vaccines: development, evaluation, approval and monitoring [Internet]. Eur Med Agency. 2020;2021.
2. Lurie N, Saville M, Hatchett R, Halton J. Developing Covid-19 vaccines at pandemic speed. J Med. 2020;(382):1969–1973.
3. Yang Y, Peng F, Wang R, et al. The deadly coronaviruses: the 2003 SARS pandemic and the 2020 novel coronavirus epidemic in China. J Autoimmun. 2020;102434:109.
4. WHO. 19 March 2021 statement of the WHO Global Advisory Committee on Vaccine Safety (GACVS) COVID-19 subcommittee on safety signals related to the AstraZeneca COVID-19 vaccine. 2021.
5. Nguyen T, Henningsen KH, Brehaut JC, Hoe E, Wilson K. Acceptance of a pandemic influenza vaccine: a systematic review of surveys of the general public. Infect Drug Resist. 2011;4:197–207. doi:10.2147/IDR.S23174
6. Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1–11. doi:10.1016/j.socscimed.2014.04.018
7. Dubé E, MacDonald NE. vaccine acceptance: barriers, perceived risks, benefits, and irrational beliefs. In: Bloom BR, Lambert P, editors. The Vaccine Book, Chapter 26.
8. Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–193. doi:10.1016/j.ijsu.2020.04.018
9. CDC. Different COVID-19 vaccines | CDC; 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines.html.
10. WHO. 2.2 million COVID-19 vaccines allocated by the COVAX Facility arrive in Ethiopia, marking the start of the country’s COVID-19 vaccination campaign. 2021.
11. WHO. Ethiopia introduces COVID-19 vaccine in a national launching ceremony. 2021.
12. Kissler SM, Tedijanto C, Goldstein E, Grad YH, Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science (New York, N.Y.). 2020;368(6493):860–868. doi:10.1126/science.abb5793
13. Reperant LA, Osterhaus A. COVID-19: losing battles or winning the war? One Health Outlook. 2020;2:9. doi:10.1186/s42522-020-00019-2
14. Rawat K, Kumari P, Saha L. COVID-19 vaccine: a recent update in pipeline vaccines, their design and development strategies. Eur J Pharmacol. 2021;892:173751. doi:10.1016/j.ejphar.2020.173751
15. Voysey M, Clemens SA, Madhi SA, et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet Glob. 2021;397:99–111.
16. Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi:10.1056/NEJMoa2034577
17. Marco V. COVID-19 vaccines: the pandemic will not end overnight. Lancet Microbe. 2020;2.
18. Mellet J, Pepper MSA. COVID-19 vaccine: big strides come with big challenges. Vaccines. 2021;9(1):39. doi:10.3390/vaccines9010039
19. Korber B, Fischer WM, Gnanakaran S, et al. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182:812–827. doi:10.1016/j.cell.2020.06.043
20. Tang X, Wu C, Li X, et al. On the origin and continuing evolution of SARS-CoV-2. Natl Sci Rev. 2020;7:1012–1023. doi:10.1093/nsr/nwaa036
21. Reuters. South Korea reports more recovered coronavirus patients testing positive again; 2021. Available from: https://www.reuters.com/article/us-health-coronavirus-southkorea-idUSKCN21V0JQ.
22. Chen D, Xu W, Lei Z, Huang Z, Liu JGZ. Recurrence of positive SARS-CoV-2 RNA in COVID-19: a case report. Int J Infect Dis. 2020;93:297–299. doi:10.1016/j.ijid.2020.03.003
23. Geoghegan S, O’Callaghan KP, Pa O. Vaccine safety: myths and misinformation. Front Microbiol. 2020;11:372. doi:10.3389/fmicb.2020.00372
24. McKee C, Bohannon K. Exploring the reasons behind parental refusal of vaccines. J Pediatr Pharmacol Ther. 2018;21:104–109. doi:10.5863/1551-6776-21.2.104
25. Wolaita Zone Finance. Socio economic and population report. 2017/2018. p 49.
26. Martin WA, Grace FA, Frank KA, Bright A. Acceptability of COVID-19 vaccination among health care workers in Ghana. Hindawi Adv Public Health. 2021. doi:10.1155/2021/9998176
27. Stern MF, Piasecki AM, Strick LB, et al. Willingness to receive a COVID-19 vaccination among incarcerated or detained persons in correctional and detention facilities — four states, 2020. Morbid Mortal Wkly Rep. 2021;70(13).
28. Al-Qerem WA, Jarab AS. COVID-19 vaccination acceptance and its associated factors among a middle eastern population. Front Public Health. 2021;9:632914. doi:10.3389/fpubh.2021.632914
29. Wong MC, Wong EL, Huang J, et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021.
30. Sallam M, Dababseh D, Eid H, et al. Low COVID-19 vaccine acceptance is correlated with conspiracy beliefs among university students in Jordan. Int J Environ Res Public Health. 2021;18:2407. doi:10.3390/ijerph18052407
31. Bhartiya S, Kumar N, Singh T, et al. Knowledge, attitude and practice towards COVID-19 vaccination acceptance in West India. Int J Commun Med Public Health. 2021;8(3):1170–1176. doi:10.18203/2394-6040.ijcmph20210481
32. Shaw J, Stewart T, Anderson KB, et al. Assessment of US health care personnel (HCP) attitudes towards COVID-19 vaccination in a large University health care system. Clin Infect Dis. 2021.
33. Dror AA, Eisenbach N, Taiber S, et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–779. doi:10.1007/s10654-020-00671-y
34. Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Regional Health. 2020.
35. Wang J, Jing R, Lai X, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. 2020;8:482. doi:10.3390/vaccines8030482
36. Shekhar R, Sheikh AB, Upadhyay S, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. 2021;9(2):119. doi:10.3390/vaccines9020119
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
