Back to Journals » Journal of Multidisciplinary Healthcare » Volume 14
COVID-19 Prevention Practices and Determinant Factors Among Healthcare Professionals Working in Hospitals of South Gondar Zone, Northwestern Ethiopia
Authors Walle Z , Berihun G , Keleb A , Teshome D , Berhanu L
Received 21 June 2021
Accepted for publication 23 July 2021
Published 22 August 2021 Volume 2021:14 Pages 2287—2298
DOI https://doi.org/10.2147/JMDH.S325127
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Zebader Walle,1 Gete Berihun,2 Awoke Keleb,2 Daniel Teshome,3 Leykun Berhanu2
1Department of Public Health, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia; 2Department of Environmental Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia; 3Department of Anatomy, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
Correspondence: Gete Berihun Email [email protected]
Background: Coronavirus disease 2019 (COVID-19) has been a global public health crisis since December 2019. Health care professionals (HCP) are highly vulnerable for contracting the disease. Due to the absence of known treatment, prevention is the best option for controlling its transmission.
Objective: The study aimed to assess COVID-19 prevention practices and determinant factors among HCP working in hospitals of South Gondar ZoneH, Northwestern Ethiopia.
Methods: Institution-based cross-sectional study design was used from July 1 to 30, 2020 among 372 HCPs. The participants were selected on random sampling technique basis. Data were entered into Epi data version 3.1 and exported to Statistical Package for Social Science (SPSS V.25) software for data cleaning and analysis. Binary logistic regression analysis was used to assess the association between independent variables and prevention practice of COVID-19.
Results: A total of 372 HCPs participated in the study with a response rate of 94.9%. Less than one-third 112 (30.1%) of the participants were females. About 308 (82.8%), 285 (76.6%), and 224 (60.2%) of the participants had good knowledge, positive attitude, and good prevention practice towards COVID-19, respectively. Being male (AOR =2.68; 95% CI (confidence interval): 1.50,4.81), 2– 5 years working experience (AOR= 4.61; 95% CI: 1.70,12.47), greater than five years working experience (AOR= 5.86; 95% CI: 2.01,17.05), age of 31– 40 years old (AOR= 2.49; 95% CI; 1.41,4.41), above 40 years (AOR= 6.94; 95% CI: 2.33– 20.71), use of COVID-19 guideline (AOR= 4.79; 95% CI: 2.17– 10.53), and using peers as sources of information about COVID-19 (AOR= 2.06; 95% CI: 1.07– 3.94) were factors of COVID-19 prevention practices.
Conclusion: Less than two-thirds of the participants had good COVID-19 prevention practices. Sex, work experience, age, use of COVID-19 guideline, and using peers as sources of information were factors of COVID-19 prevention practices. Hence, continuous information dissemination and experience sharing on COVID-19 prevention should be done continuously.
Keywords: COVID-19, prevention practices, healthcare professionals, Ethiopia
Introduction
Coronavirus disease 2019 (COVID-19) is a communicable respiratory disease caused by a new strain of coronavirus of Severe Acute Respiratory Syndrome (SARS-CoV-2) that causes illness in humans.1 Healthcare professionals (HCP) are part of the frontline in the struggle against COVID-19.2 The disease was initially reported in December 2019 in Wuhan, Hubei Province, China.3–5 COVID-19 was declared as a pandemic by the World Health Organization (WHO) on March 11, 2020.6
The disease transmits through droplets, airborne transmission, and contact between humans during airway maneuvers when a patient is infected, especially during tracheal intubation. Fever, dry cough, weakness, myalgia, shortness of breath, and dyspnoea are the common signs and symptoms of COVID-19 infection.7 Elders and patients with chronic medical conditions like hypertension, cardiac disease, lung disease, cancer, or diabetes have been identified as potential risk factors for disease severity and mortality. Although successful treatment is not developed yet, early identification of symptoms and timely seeking of supportive care enhances recovery from illness.8
Healthcare professionals (HCPs) are part of the frontline in the struggle against the disease.2 They are highly vulnerable to SARS-COV-2 infection due to their clinical role in the healthcare settings.6 The problem is severe mainly in low and middle-income countries where the health care facilities were overburdened before the occurrence of the pandemic by routine activities.9 Therefore, in such areas addressing shortages of hospital beds, oxygen, ventilators, and personal protective equipment (PPE) as primary response measures might not be feasible.10 They are usually working in isolation units, critical care units, intensive care units (ICUs), emergency units, working in frontline positions, and having contact with suspected and confirmed cases of COVID-19.6 According to WHO report as of May 21, 2021 an estimated of more than 115,000 HCPs have paid the ultimate value in the service of others.11
As of July 13, 2021, 12.25 pm, COVID-19 has spread to more than 222 countries and a total of 188,119,516 confirmed cases of COVID-19 were reported globally. Of these, 172,052,948 had recovered while 4,056,847 had died due to the disease.12 The first case of the disease in Ethiopia was reported on March 13 2020.13,14 Since then a total of 277,137 confirmed cases of COVID-19 were reported as of July 13, 2021. Of these, 262,022 had recovered while 4343 persons had died due to the disease.15
Microorganism contamination of healthcare workers’ hands contributes to the spread of Hospital acquired infections (HAIs) in hospital settings, and errors in hygiene procedures are at the base of self-contamination. During the COVID-19 pandemic, several Infection Prevention and Control (IPC) measures have been implemented to reduce nosocomial infection.16,17 Guidelines for healthcare workers and online refreshment training have been developed by WHO, CDC, and various governmental organizations in various countries to boost the knowledge and prevention practices of COVID-19.18 Furthermore, use of facemasks, respiratory hygiene, stay of at home are also implemented as prevention measures.1
HCPs implement different COVID-19 prevention practices. A study conducted in Ethiopia showed that majority of them used handwashing with water and soap or alcohol-based hand rub and wearing of face masks. But, lower number of HCPs cover their mouth and nose while sneezing and properly disposed of mouth covering materials, avoid hand shaking, avoid touching of eye, nose, and mouth by unwashed hands, and avoid travelling to a crowded place as prevention measures.19 Another study also supported that wearing of face masks and restricting from going to crowded place were implemented as prevention measures.20
Different scholars revealed that the COVID-19 prevention practice is affected by different factors. A study conducted in Ethiopia showed that sex education level20,21 profession, service year, availability of personal protective equipment, and knowledge level were factors of COVID-19 prevention practices.19–21 In addition to these, residence, health facility type, access to infection prevention (IP) training, presence of IP guidelines, having chronic illness, lack of personal protective equipments, and high work loads were factors of COVID-19 prevention practices.19 Furthermore, attitude of the HCPs was another factor of COVID-19 prevention practices.20
Although different prevention measures are implemented against the transmission of the COVID-19, the number of new cases registered across the world is not reduced to the expected level. HCPs are the most exposed groups for contracting the disease. As a result, frequent assessment of the COVID-19 prevention practices among HCPs plays a vital role in reducing the transmission of the disease.22 Therefore, the study aimed to assess prevention practices towards COVID-19 and determinant factors among HCPs working in the hospitals of South Gondar Zone, Northwestern Ethiopia.
Materials and Methods
Study Design, Period, and Setting
An institutional-based cross-sectional study design was conducted among HCPs working in the hospitals of South Gondar Zone, Northwestern Ethiopia from July 1 to 30, 2020. South Gondar is one of the 13 administrative zones in the Amhara Regional State, Ethiopia. Debre Tabor is the capital city of the South Gondar Zone which is located 597 km away from Addis Ababa. Based on the central statistical agency (CSA) 2007 of Ethiopia, the total population of the South Gondar Zone was 2,051,738.23,24 The zone has one general hospital, seven district hospitals, and 93 health centers.24 According to the report of South Gondar Zone health department, there were more than 2500 registered HCPs available during data collection.
Source and Study Population
All HCPs who were working in hospitals of the South Gondar zone at the time of data collection were the source population whereas all HCPs who were working in three randomly selected hospitals (Debre Tabor, Mekane Eyesus, and Andabet) were the study population.
Inclusion and Exclusion Criteria
All clinical staff, namely, medical doctors, nurses, pharmacists, midwives, anesthetics, health officers, and medical laboratory professionals were included in the study. HCPs who were critically ill, did not volunteer to participate, and were absent during the data collection were excluded from the study.
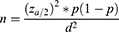
Sample Size Determination
The sample size was determined using the single population proportion formula considering the following assumptions.
Zα/2 is the standard normal variable value at (1-α) % confidence level (α is 0.05 with 95% CI, Zα/2 = 1.96), an estimate of the proportion of good COVID-19 prevention practices, 63.5% taken from other study conducted in Ethiopia22 and margin of error, 5%. As a result, the sample size becomes 356, and with adding of 10% non-response rate, the final sample size becomes 392.
Sampling Techniques and Procedures
After selecting the three hospitals randomly out of the eight hospitals, we proportionally allocated a sample size based on HCPs available during the data collection time. Hence, 225 samples were collected from Debre Tabor general hospital, 87 from Mekane Eyesus, and the remaining 60 samples were collected from Andabet hospital. The participants were selected randomly using the lottery method by taking the lists of all HCPs from a human resource office of their respective hospitals.
Outcome and Explanatory Variables
The outcome variable was COVID-19 prevention practices (good/poor). The explanatory variables were socio-demographic variables of the respondents, knowledge about COVID-19, behavioral variables, pre-existing medical condition, and sources of information towards COVID-19.
Operational Definitions
HCPs
Any member of the health care unit that includes medical doctor, pharmacist, physiotherapist, or nursing professions or any other person who in the course of his or her professional activities who may prescribe, administer, or dispense a medicinal product to an end-user.25
Knowledge
Knowledge was measured using 16 questions consisting of signs and symptoms, risk groups and prognosis, method of transmission, and prevention methods of COVID-19. Each question was responded as either yes or no. Respondents who answered correctly were given 1 point while others were given 0 points. The total knowledge score ranges from 0 to 16 and a cut-off level of ≥12 (75% and above) was considered as having good knowledge while <12 (75%) was considered as having poor knowledge.26
Attitude
The attitude was measured using 14 items and the response was categorized based on 3 scale measurements with agree (3 points), neutral (2 points), and disagree (1 point). The total score of attitude varies from 14 to 42, with an overall mean score of ≥34 (80%) was considered as a positive attitude while less than <34 (80%) was considered as a negative attitude towards COVID-19.
Preventin Practices
The prevention practices was measured using 12 items and those who respond as yes were given 1 point while no was marked as 0 values. The total prevention practices score ranges from 0 to 12 and a score with a cut-off ≥9 (75%) was considered as having a good prevention practices while <9 (75%) was considered as a poor prevention practices towards COVID-19.27,28
Data Collection, Management, and Quality Assurance
The data were collected using a validated structured questionnaire which was adapted from published articles, other related literatures, and WHO guidelines.29–34 The questionnaire consists of four sections including: socio-demographic characteristics of the participants and sources of information towards COVID-19 (Supplementary Table 1), knowledge towards COVID-19 (Supplementary Table 2), attitude of HCPs towards COVID-19 (Supplementary Table 3) and prevention practices of COVID-19 (Supplementary Table 4). The questionnaire was prepared in the English version and translated to the native language (Amharic) and re-translated back to English to ensure consistency. A pre-test was conducted using 5% of the sample size in Central Gondar zone hospital (Belesa district hospital) to establish the validity of the questionnaire, and amendment was done accordingly. Two days of training was given to data collectors and supervisors on the objective of the study and on the overall contents of the questionnaire. The data were collected by three BSc nurse professionals using a self-administered questionnaire. Supervision was carried out on a daily basis, and appropriate corrections were taken timely. Furthermore, double data entry was done to control data entry errors. The reliability coefficient of Cronbach’s alpha was 0.74 which is an acceptable range.
Statistical Analysis
The data were entered using Epi-Data version 3.1 and exported to the Statistical Package of the Social Science (SPSS) version 25.0 software for data cleaning and analysis. Descriptive statistics such as frequencies and percentage were used for categorical variables whereas mean and standard deviations for continuous variables. Bivariable (crude odds ratio [COR]) and multivariable (adjusted odds ratio [AOR]) were determined using binary logistic regression at 95% Confidence Interval (CI). In the bivariable analysis, variables with p <0.25 were entered for multivariable analysis. In multivariable analysis, variables with a significance level of p <0.05 were taken as statistically significant at 95% CI and independently associated with the prevention practice of HCPs towards COVID-19. The presence of multi-collinearity among independent variables was checked using standard error at the cutoff value of -/+ 2 and the maximum standard error was 1.25. Model fitness was checked using the Hosmer and Lemeshow test, which had a p-value of 0.86, showing the model was fit.
Ethical Consideration
This study was conducted in accordance with Helsinki Declaration. The study was approved by the ethical review committee of the College of Health Sciences, Debre Tabor University with a reference number of HSC2087/2012. Permission to conduct the study was obtained from the respective hospitals. Prior to the data collection, the overall aim of the study was explained for data collectors and the supervisors. The participation in the study was based on their voluntary decision. Prior to the data collection, written consent was obtained from each particiant. Those who volunteered to participate in the study were informed that they had the option to withdraw from the study at any stage. The confidentiality of the study participants were ensured by avoiding possible identifiers (Supplementary File).
Results
Socio-Demographic Characteristics of the Respondents
A total of 372 HCPs participated in the study with a response rate of 94.9%. The majority of the respondents were males, 31–40 years old, married, and orthodox with 260 (69.9%), 172 (46.2%), 232 (62.4%), and 302 (81.2%), respectively. Nearly one-third, 120 (32.3%) of HCPs were nurses and a similar number of HCPs took training towards COVID-19. Furthermore, less than a quarter 88 (23.7%) of the HCPs reported that there was a sufficient PPE supply (Table 1).
 |
Table 1 Socio-Demographic Characteristics of Health Care Professionals Working in Hospitals of South Gondar Zone, Northwestern Ethiopia in July 1-30, 2020 (n=372) |
Knowledge of HCPs About COVID-19 Prevention
More than three-quarter, 308 (82.8%; 95% CI: 79.0–86.8%) of the HCPs had good knowledge while the remaining 64 (17.2%; 95% CI: 13.2–21.0%) had a poor knowledge about COVID-19. The overall mean knowledge score of the respondents was 12.16±1.69. All respondents replied that dyspnea was a major sign and symptom of COVID-19 followed by dry cough and fever with 368 (98.8%). Similarly, 328 (88.2%) of the respondents knew that the elderly and peoples with chronic medical illnesses are at higher risk of developing severe cases of COVID-19 infection. Furthermore, two-thirds 248 (66.7%) of the respondents knew that persons with COVID-19 virus can transmit the virus to others even in the absence of fever. Less than two-thirds 224 (60.2%) of the HCPs knew that children and young adults should take necessary measures to prevent COVID-19 infection (Table 2).
 |
Table 2 Knowledge About COVID-19 Among Healthcare Professionals Working in Hospitals of South Gondar Zone, North Western Ethiopia in July 2020 (n=372) |
Attitude of HCPs Towards COVID-19 Prevention
This finding revealed that about three-fourths 285 (76.6%; 95% CI: 71.8–80.6%) of the respondents had a positive attitude while 87 (23.4%; 95% CI: 19.4–28.2%) respondents had a negative attitude towards COVID-19 prevention. Less than one-third 113 (30.4%) of the respondents agreed that black race was not protected against the infection of COVID-19. Furthermore, less than a quarter, 85 (22.8%) of the participants agreed that Ethiopia is in a good position to control the transmission of COVID-19 within a short time. Similarly, less than two-thirds, 230 (61.8%) of the respondents agreed that COVID-19 is not a stigma and they should not hide their infection if they contract COVID-19. Furthermore, nearly one-third 133 (35.8%) of the respondents agreed that COVID-19 is a fatal disease (Table 3).
 |
Table 3 Attitude towards COVID-19 among Health Care Professionals Working in Hospitals of South Gondar Zone, North Western Ethiopia in July 2020 (n=372) |
Prevention Practices of HCPs Towards COVID-19
The finding revealed that less than two-thirds 224 (60.2%; 95% CI: 55.5–65.3%) of respondents had good prevention practices while 148 (39.8%; 95% CI: 34.7–44.5%) of the respondents had poor prevention practices towards COVID-19. The overall prevention practice score of the respondents towards COVID-19 was 8.81±1.64. More than three-fourth, 312 (83.9%) of the respondents washed their hands with water and soap for about 20 seconds before touching patients. But, a lower number of the respondents 160 (43%) used PPE during performing their routine activities. Furthermore, more than one-third, 148 (39%) of respondents applied the recommended physical distancing of 2 meters away from others when they went to a public crowded area. Finally, nearly two-thirds, 240 (64.5%) of the participants used face masks frequently when they leave their homes (Table 4).
 |
Table 4 Prevention Practices towards COVID-19 among Health Care Professionals Working in Hospitals of South Gondar Zone, Northwestern Ethiopia in July 2020 (n=372) |
Factors Associated with Prevention Practices Towards COVID-19
The multivariable logistic regression analysis showed that age, sex, use of COVID-19 prevention guideline, working experience, and use of peers as sources of information towards COVID-19 were factors significantly associated with the prevention practices of COVID-19 at 95% (CI). Being males had 2.68 (1.50–4.81) more likely to have good prevention practices towards COVID-19 than females. Similarly, working experience of 2–5 years 4.61 (1.70–12.47) and above five years 5.86 (2.01–17.05) were more likely to have good prevention practices towards COVID-19 than who were less than 2 years of working experience. Similarly, the age of the respondents with 31–40 years was 2.49 (1.41–4.41) and above 40 years old 6.94 (2.33–20.71) times more likely to have a good COVID-19 prevention practice than those who were at the age of 20–30 years old. HCPs who used COVID-19 prevention guidelines were 4.79 (2.17–10.43) times more likely to have COVID-19 prevention practice than those who did not use the guidelines. Finally, participants who used peers as sources of information towards COVID-19 were 2.06 (1.07–3.94) times more likely to have good COVID19 prevention practices than those who did not use it (Table 5).
 |
Table 5 Factors Associated with COVID-19 Prevention Practices Among HCPs Working in Hospitals of South Gondar Zone, Northwestern Ethiopia, July 2020 (n = 372) |
Discussion
COVID-19 infection is has become one of the most serious global health concerns.35 Therefore, assessment of COVID-19 prevention practices among HCPs plays an important role in controlling the transmission of the disease. Institution-based cross-sectional study design was applied to assess prevention practices towards COVID-19 and determinant factors among HCPs working in hospitals of South Gondar Zone, Northwestern Ethiopia.
More than three-quarters (82.8%; 95% CI; 79.0–86.8%) of the HCPs had good knowledge about COVID-19 which was in line with the findings in Pakistan (84%)36 and Nigeria (83.7%).37 The finding was higher than the finding in United Arab Emirates (UAE)38 and Sierra Leon (72.7%)39 but lower than the findings in Ethiopia (94.2%),40 (92.4),25 Pakistan (90.7%).41 (93.2%).5 The possible justification for this variation may be due to a change in the study period, setting, and method of data collection. The overall knowledge score of the participants was 76% which was in line with the finding in Ethiopia (78.8%)42 but lower than the findings in China (89%),43 Pakistan (90.7%),5 and Uganda (82.4%).18 This variation may be explained due to a change in information dissemination towards COVID-19 and provision of training on COVID-19. Therefore, education and training through continuous professional education and journal clubs, particularly on symptoms and transmission are essential in improving the knowledge of HCPs about COVID-19 is essential.18 About 90% of the HCPs used social media as a source of information about COVID-19 which was consistent with a finding in China (91.1%).26 On the contrary, it was higher than the finding in UAE (60%).38 The possible reason may be due to the variation in the accessibility of the internet and culture of the participants.
Most of the respondents (88.2%) knew that the elderly and those who have a chronic illness were more likely to develop severe cases of COVID-19 which was higher than the finding in Ethiopia (72.5%).44 This difference may be due to the change of educational background of the study subjects and study period. On the other hand, less than two-thirds 60.2% of HCP knew that children and young adults need to take COVID-19 prevention measures. Neglecting these high-risk groups of the populations may create good opportunities for the transmission of the disease.
Three-quarter (76.6%; 95% CI; 71.8–80.6%) of the participants had a positive attitude towards COVID-19 which was in line with the findings in Ethiopia (72%)45 and Nigeria (79.5%),46 (78.9%).37 However, it was higher than the findings in Bangladesh (48%),47 Uganda (21%)18 and Ethiopia (54.0%),48 (64%).25 On the contrary, it was lower than the findings in Ethiopia (94.7%)22 and Pakistan (82.16%),49 (90%).5 The possible justification for this variation may be due to a change in the study period, heterogeneity of study participants, and study setting.
Less than a quarter 22.8% of the respondents agreed that Ethiopia will control COVID-19 within a short time which was lower than a finding in China (97.1%).26 This variation may be due to the change in the health care system, commitment of the governments towards prevention of the disease, and budget deficiency. Furthermore, less than two-thirds 61.8% of the respondents agreed that COVID-19 does not lead to the stigma which was lower than the findings in Ethiopia (77%),22 and 83.8%.38 The presence of stigma towards COVID-19 may lead to under-reporting of cases. As a result, the rate of mortality and morbidity due to COVID-19 will be increased proportionally.
The adaption of prevention practices is the only solution to control the COVID-19, as to date, there is no specific treatment for the novel coronavirus.5 But, insufficient PPEs for HCWs and isolation facilities, environmental contamination and overcrowding have worsened COVID-19 response and management strategies in various localities mainly in developing countries.37 The current finding revealed that less than two-thirds (60.2%; 95% CI; 55.5–65.3%) of the participants had good prevention practices towards COVID-19 which was consistent with the study in Ethiopia22,28, (55%).25 The finding was higher than the study in Ethiopia (41.6%),50 (10.4%),51 49%,52 (40.70%),53 (49%).27 On the contrary, it was lower than the findings in UAE (86.5%),54 Pakistan (73.4%),55 Uganda (74%),18 Nigeria (77.6%).37 The possible reason for the variation may be due to the change in respondents’ personal and environmental characteristics, accessibility of facilities, monitoring and follow up, training coverage, strength of health care systems, sample size, and study period. The overall mean score of prevention practice score was 8.81±1.64 (73.4%) which was higher than the finding in Ethiopia.28
Nearly, three-quarters 74% of the respondents practiced handwashing with water and soap for about 20 seconds which was higher than the finding in Ethiopia (61.3%)25 but lower than the finding in Ethiopia (82.6%),56 Uganda (96%),18 Malaysia (87.8%),57 and Rwanda (95%).58 The possible justification for this variation may be due to a change in availability and accessibility of handwashing facilities in the health care setting, and handwashing behaviors. Access of essential facilities mainly in healthcare setting plays a vital role in tackling the transmission of HAIs infection including COVID-19. In the present finding only one-third 34.4% of the participants used a single pair of gloves for each patient. This finding was supported with the fact that more than three quarters of the participants replied as there was shortage of PPE including gloves. Less than two-thirds 64.5% of the HCPs always wore a mask when coming in contact with the patients which was in line with the finding in Ethiopia22 but lower than the finding in Ethiopia (54.7%).25 The present study finding was lower than the finding in Pakistan,5 and China (98.0%)43 but higher than in Uganda (54%).18 The possible reason for this variation may be due to a change in availability and accessibility of facilities, affordability of face masks, perception towards face masks, and commitment of the HCPs on tackling the transmission of the disease.
According to the current finding, male HCPs had 2.68 (1.50–4.81) times more likely to have good prevention practices on COVID-19 which was supported with the finding in Ethiopia20 and China.59 Working experience of HCPs was another factor of COVID-19 prevention practice. HCPs who had more experience had implemented better COVID-19 prevention measures. This may be due to the fact that in history there were a number of epidemics such as influenza with similar features with the current pandemic. Different organizations including WHO has designed different COVID-19 prevention guidelines mainly in healthcare setting to enhance the prevention measures of COVID-19 among HCPs. But, most of them may not use these guidelines due to different reasons. Hence, the current finding of the study revealed that HCPs who used these guidelines were 1.45 more likely to have a good COVID-19 prevention practice than the corresponding group. This finding was consistent with the finding in Ethiopia.28 The age of the HCPs was another factor which affects the prevention practices of COVID-19. Based on the current finding, the higher age 31–40 and above 40 years old were 2.49 and 6.94 time more likely to have good prevention practice respectively than the corresponding age groups of less than 30 years old. The present study findings were consistent with the findings in Ethiopia,60 and Uganda.18 Increasing age may lead the development of immune-compromised. Therefore, such types of situations may activate individuals to practice better COVID-19 prevention measures which was supported by other findings.61
HCPs are at the frontline of COVID-19 pandemic response and are exposed to dangers like pathogen exposure, long working hours, psychological distress, fatigue, occupational burnout and stigma, and physical violence. A poor understanding of the disease among HCPs can result in delayed identification and treatment leading to rapid spread of infections.18 Knowledge greatly reflects the practice of individuals as it provides a base for good practice. Although the level of knowledge and attitude was good, less than two-thirds of the HCPs had implemented good COVID-19 prevention practices. The overall prevention of the COVID-19 highly depends mainly on the implementation of COVID-19 prevention measures by HCPs. But, in this finding the prevention practice was below expected. Hence, the time required for the control of the disease from the world may need more than years than the expected time. Therefore, more effort is required from HCPs to be accepted by the general population.Therefore, implementation of proper Infection Prevention and Control (IPC) measures mainly in healthcare setting will have been implemented to reduce nosocomial microorganism transmission mainly in healthcare setting even after the elimination of the pandemic.
Conclusion
Generally, less than two-thirds of the participants had good prevention practices about COVID-19. Being male, higher age groups, more working experience, use of COVID-19 prevention guidelines, use of peers as sources of information towards COVID-19, and a positive attitude towards COVID-19 were factors affecting COVID-19 prevention practices.Therefore, continuous information dissemination using different strategies should be conducted on the overall prevention practices of COVID-19. Furthermore, higher officials of the healthcare facilities should establish a continuous meeting in their healthcare setting to create a good opportunity for sharing of good prevention practices among the HCPS. The healthcare facilities should establish functional infection prevention committee to monitor and follow up the prevention practices of COVID-19 and taking appropriate measures in collaboration of the officials of the healthcare facilities and the zonal and regional health office; finally, we want to recommend longitudinal and qualitative studies should be conducted.
Limitation of the Study
This study has limitations. First, since this is a cross-sectional analysis, the temporal significance of our results can shift over time or as large-scale preventive initiatives are implemented. Second, the study was a self-reported survey, respondents could have chosen socially desirable options rather than their real knowledge attitude and prevention practices.
Abbreviations
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; COVID-19, coronavirus disease-2019; ETB, Ethiopian birr; HAIs, hospital acquired infection; HCPs, health care professionals; PPE, personal protective equipment; SARS-COV-2, Severe Acute Respiratory Syndrome- Corona Virus-2; WHO, World Health Organization.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We would like to express our heartfelt gratitude to Debre Tabor University for providing us necessary material for conducting this research. We also to extend our thanks to the study participants who gave us valuable information and their kind cooperation. We also want to express our appreciation for all data collectors and supervisors for their commitment and collaboration.
Disclosure
The authors declare that they have no conflicts of interest for this work.
References
1. African Union, African CDC. Coronavirus disease 2019 (COVID-19) latest updates on the COVID-19 crisis from Africa CDC. Available from: https://africacdc.org/covid-19.
2. Erdema H, Lucey DR. Healthcare worker infections and deaths due to COVID-19: a survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis. 2021;102:239–241. doi:10.1016/j.ijid.2020.10.064
3. Elhadi M, Msherghi A, Alkeelani M. Assessment of healthcare workers’ levels of preparedness and awareness regarding COVID-19 infection in low-resource settings. Am J Trop Med Hyg. 2020;103(2):828–833. doi:10.4269/ajtmh.20-0330
4. WHO Regional Office for Africa. COVID-19 situation update for WHO African region, external situation report 15 / 2020; 2020. Available from: https://apps.who.int/iris/handle/10665/332321. Accessed March 20, 2021.
5. Saqlain M, Munir MM, Ur Rehman S, et al. Knowledge, attitude, practice and perceived barriers among healthcare professionals regarding COVID-19: a cross-sectional survey from Pakistan. J Hosp Infection. 2020;105(3):419–423. doi:10.1016/j.jhin.2020.05.007
6. Deressa W, Worku A, Abebe W, Gizaw M, Amogne W. Risk perceptions and preventive practices of COVID-19 among healthcare professionals in public hospitals in Addis Ababa, Ethiopia. PLoS One. 2021;16(6):e0242471. doi:10.1371/journal.pone.0242471
7. Ssebuufu R, Katembo Sikakulya F, Binezero SM, et al. Knowledge, Attitude, and Self-Reported Practice Toward Measures for Prevention of the Spread of COVID-19 Among Ugandans: A Nationwide Online Cross-Sectional Survey. Front Public Health. 2020;8:618731. doi:10.3389/fpubh.2020.618731
8. World Health Organization. COVID-19 Strategic Preparedness and Response Plan Operational Planning Guideline to Support Country Preparedness and Response. 2020.
9. Shreffler J, Petery J, Huecker M. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. West J Emerg Med. 2020;21(5):1059–1066. doi:10.5811/westjem.2020.7.48684.
10. Lau LL, Hung N, Joy D, Ferma J, Dodd W, Wei X. Knowledge, attitudes and practices of COVID-19 among income-poor households in the Philippines: a Cross-Sectional Study. J Glob Health. 2020;10(1):11. doi:10.7189/jogh.10.011007
11. WHO. Director-General's opening remarks at the World Health Assembly - 24 May 2021. Available from: https://www.who.int/director-general/speeches/detail/director-general-s-opening-remarks-at-the-world-health-assembly---24-may-2021.
12. Worldometer report COVID-19 cases in the world; 2020. Available from: https://www.worldometers.info/coronavirus.
13. Lone SA, Ahmad A. COVID-19 pandemic – an African perspective. Emerg Microbes Infect. 2020;9:10.
14. Baye K. COVID-19 Prevention Measures in Ethiopia Current Realities and Prospects. The Federal Democratic Republic of Ethiopia Policy Studies Institute; 2020.
15. Worldometer report COVID-19 cases in Ethiopia; 2020. Available from: https://www.worldometers.info/coronavirus/country/ethiopia.
16. Bentivegna E, Luciani M, Arcari L, Santino I, Simmaco M, Martelletti P. Reduction of multidrug-resistant (MDR) bacterial infections during the COVID-19 pandemic: a retrospective study. Int J Environ Res Public Health. 2021;18(3):1003. doi:10.3390/ijerph18031003
17. Bentivegna E, Giuliano Alessio G, Spuntarelli V, et al. Impact of COVID-19 prevention measures on risk of health care associated Clostridium difficile infection. Am J Infect Control. 2021;49(5):540–542. doi:10.1016/j.ajic.2020.09.010
18. Olum R, Chekwech G, Wekha G, Nassozi DR, Bongomin F. Coronavirus disease-2019: knowledge, attitude, and practices of health care workers at Makerere University Teaching Hospitals, Uganda. Front Public Health. 2020;8:181. doi:10.3389/fpubh.2020.00181
19. Asemahagn MA. Factors determining the knowledge and prevention practice of healthcare workers towards COVID-19 in Amhara region, Ethiopia: a cross-sectional survey. Trop Med Health. 2020;48(1):72. doi:10.1186/s41182-020-00254-3
20. Fetansa G, Etana B, Tolossa T, et al. Knowledge, attitude, and practice of health professionals in Ethiopia toward COVID-19 prevention at early phase. SAGA Open Med. 2021;9:1–9.
21. Tsegaye D, Shuremu M, Oljira D, Dubale S, Befekadu G, Bidira K. COVID – 19 related knowledge and preventive practices early in the outbreak among health care workers in selected public health facilities of Illu aba Bor and Buno Bedelle zones, Southwest Ethiopia. BMC Infectious Diseases. 2021;21:490.
22. Jemal B, Ferede ZA, Mola S, et al. Knowledge, attitude, and practice of healthcare workers towards COVID-19 and its prevention in Ethiopia: a multicenter study. Int J Risk Safe Med. 2020;preprint. doi:10.21203/rs.3.rs-29437/v1
23. Alemayehu TY, Tiruneh Boled A, Taye MG, Kibret S, Habtie M. Assessment of emergency and essential surgical service in primary hospitals of South Gondar Zone, Amhara Region, Ethiopia. Int J Surg Open. 2019;23:35–38. doi:10.1016/j.ijso.2020.02.003
24. Abate BA, Ahunie MA. Basic emergency maternal and neonatal care status of South Gon- Dar Zone, North Central Ethiopia: institutional descriptive survey. Ethiop J Reprod Health. 2017;9(1):11.
25. Bitew G, Sharew M, Belsti Y. Factors associated with knowledge, attitude, and practice of COVID-19 among health care professional’s working in South Wollo Zone Hospitals, Northeast Ethiopia. SAGA Open Med. 2021;9:1–8.
26. Giao H, Han NTN, Van KT, Ngan VK. Knowledge and attitude toward COVID-19 among healthcare workers at district 2 hospital, Ho Chi Minh City. Asian Pac J Trop Med. 2020;13:260.
27. Defar A, Molla G, Abdella S. Knowledge, practice and associated factors towards the prevention of COVID-19 among high-risk groups: a cross-sectional study in Addis Ababa, Ethiopia. PLoS One. 2021;16(3):1–14. doi:10.1371/journal.pone.0248420
28. Asemahagn MA. Factors determining the knowledge and prevention practice of healthcare workers towards COVID-19 in Amhara region, Ethiopia: a cross-sectional survey. Trop Med Health. 2020;3:1.
29. WHO E. Survey Tool and Guidance Rapid, Simple, Flexible Behavioral Insights on COVID-19. 2020.
30. Ahmad NA, Ahmad W, Arman R, Rahimi W, Ahmadi A, Vijay Raghavan SMS. Community Perception Survey – COVID 19 Knowledge, Attitude and Practice Survey in Kabul, Kunduz, and Khost Province. The Johanniter International Assistance; 2020.
31. FMOH E. National Comprehensive Covid19 Management Handbook. 2020:162
32. National Institute of Environmental Health Science. COVID-19 OBSSR Research Tools. U.S National Library of Medicine; 2020. Available from: https://www.coursehero.com/file/93872128/COVID-19-BSSR-Research-Toolspdf/. Accessed January 15, 2021.
33. Homes R. COVID-19: Infection Prevention and Control Checklist for Long-Term Care and Retirement Homes. Ontario Agency for Health Protection and Promotion; 2020:1–15.
34. World Health Organization. COVID-19 Infection Prevention and Control Sameeksha. 2020.
35. Ahmed N, Shakoor M, Vohra F, Abduljabbar T, Mariam Q, Rehman MA. Knowledge, awareness, and practice of health care professionals amid SARS-CoV-2, corona virus disease outbreak. Pak J Med Sci. 2020;36(COVID19-S4):S49–S56. doi:10.12669/pjms.36.COVID19-S4.2704..
36. Hussain I, Majeed A, Saeed H, et al. A national study to assess pharmacists’ preparedness against COVID-19 during its rapid rise period in Pakistan. PLoS One. 2020;15(11):e0241467. doi:10.1371/journal.pone.0241467
37. Tsiga-Ahmed FI, Amole TG, Musa BM, et al. COVID 19: evaluating the knowledge, attitude and preventive practices of healthcare workers in Northern Nigeria. Int J Matern Child Health AIDS. 2021;10(1):88–97. doi:10.21106/ijma.418
38. Bhagavathula AS, Aldhaleei WA, Rahmani J, Mahabadi MA, Bandari DK. Knowledge and Perceptions of COVID-19 Among Health Care Workers: Cross-Sectional Study. JMIR Public Health Surveill. 2020;6(2):e19160. doi:10.2196/19160
39. Kanu S, James PB, Bah AJ, et al. Healthcare workers’ knowledge, attitude, practice and perceived health facility preparedness regarding COVID-19 in Sierra Leone. J Multidiscip Healthc. 2021;14:67–80. doi:10.2147/JMDH.S287156
40. Shibabaw T, Teferi B. Knowledge and practice toward prevention of SARS-COV-2 among healthcare workers at delghi primary hospital during a massive test campaign in northwest Gondar, Ethiopia: institution-based descriptive cross-sectional survey. Infect Drug Resist. 2021;14:381–390. doi:10.2147/IDR.S289965
41. Hussain I, Majeed A, Imran I, et al. Knowledge, attitude, and practices toward COVID‑19 in primary healthcare providers: a cross‑sectional study from three tertiary care hospitals of Peshawar, Pakistan. J Community Health. 2021;46(3):441–449. doi:10.1007/s10900-020-00879-9
42. Bekele D, Tolossa T, Tsegaye R, Teshome W. The knowledge and practice towards COVID-19 pandemic prevention among residents of Ethiopia: an online cross-sectional study. PLoS One. 2021;. doi:10.1371/journal.pone.0234585
43. Zhong B, Luo W, Li H, Zhang Q, Liu X, Li W. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci. 2020;16(10):1745–1752. doi:10.7150/ijbs.45221
44. Kebede Y, Yitayih Y, Birhanu Z, Mekonen S, Ambelu A. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma University medical center visitors, Southwest Ethiopia. PLoS One. 2020;15(5):1–15. doi:10.1371/journal.pone.0233744
45. Tadesse DB, Gebrewahd GT, Demoz GT. Knowledge, attitude, practice, and psychological response toward COVID-19 among nurses during the COVID-19 outbreak in Northern Ethiopia. New Microbes New Infect. 2020;38:100787. doi:10.1016/j.nmni.2020.100787
46. Christopher R, Margaret R, Dauda MAD, Saleh A, Ene P. Knowledge, attitudes and practices towards COVID - 19: an epidemiological survey in north - central Nigeria. J Community Health. 2020. doi:10.1007/s10900-020-00881-1
47. Ferdous MZ, Islam MS, Sikder MT, Mosaddek ASM. Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: an online-based cross-sectional study. PLoS One. 2020;15(10):1–17. doi:10.1371/journal.pone.0239254
48. Angelo AT, Alemayehu DS, Dacho AM. Knowledge, attitudes, and practices toward covid-19 and associated factors among university students in Mizan Tepi University. Infect Drug Resist. 2021;14:349–360. doi:10.2147/IDR.S299576
49. Hussain I, Majeed A, Imran I, et al. Knowledge, attitude, and practices toward COVID - 19 in primary healthcare providers: a cross-sectional study from three tertiary care hospitals of Peshawar, Pakistan. J Community Health. 2021;46(3):441–449. doi:10.1007/s10900-020-00879-9
50. Abate H, Mekonnen CK. Knowledge, attitude, and precautionary measures towards covid-19 among medical visitors at the University of Gondar comprehensive specialized hospital northwest Ethiopia. Infect Drug Resist. 2020;13:4355–4366. doi:10.2147/IDR.S282792
51. Taye GM, Bose L, Beressa TB, et al. COVID-19 knowledge, attitudes, and prevention practices among people with hypertension and diabetes mellitus attending public health facilities in Ambo, Ethiopia. Infect Drug Resist. 2020;13:4203–4214. doi:10.2147/IDR.S283999
52. Tigabu Desie E, Tekalign Amera B, Sheganew Fetene T, Abraham Tsedalu A, Nigusie Solomon T, Chalie Marew T. Assessment of knowledge, practice and associated factors towards prevention of novel coronavirus among clients attending at Debre Tabor General Hospital, Debre Tabor Town, North West Ethiopia, institutional based cross-sectional study. Int J Community Med Public Health. 2020;1(1):26–34. doi:10.29328/journal.jcmhs.1001004
53. Amsalu B, Guta A, Seyoum Z, et al. Practice of COVID-19 prevention measures and associated factors among residents of dire DAWA city, eastern Ethiopia: community-based study. J Multidiscip Healthc. 2021;14:219–228. doi:10.2147/JMDH.S292409
54. Srivastava KC, Shrivastava D, Sghaireen MG, et al. Knowledge, attitudes and practices regarding COVID-19 among dental health care professionals: a cross-sectional study in Saudi Arabia. J Int Med Res. 2020;48(12):030006052097759. doi:10.1177/0300060520977593
55. Salman M, Mustafa ZU, Asif N, Zaidi HA, Shehzadi N. Knowledge, attitude and preventive practices related to COVID-19 among health professionals of Punjab Province of Pakistan. Drugs Ther Perspect. 2020;36(7):319–25.
56. Nigussie TF, Azmach NN. Knowledge, attitude and practice towards COVID-19 among Arba Minch Town residents, Southern Ethiopia. GSJ. 2020;8(6). ISSN 2320-9186.
57. Azlan AA, Hamzah MR, Jen T, Id S, Hadi S, Id A. Public knowledge, attitudes and practices towards COVID-19: a cross-sectional study: A cross-sectional study in Malaysia. PloS One. 2020;1–15. doi:10.1371/journal.pone.0233668
58. Pacifique N, Menelas N, Nadia H, David T, Ernest N, Fidele B. Knowledge, attitudes and preventive practices towards COVID-19 among frontline healthcare workers in Rwanda. Public Health Bull. 2020;2(1):16–21.
59. Zheng L, Wang X, Zhou C, et al. Analysis of the infection status of healthcare workers in Wuhan during the COVID-19 outbreak: a cross-sectional study. Cllin Infect Dis. 2020;71(16):2109–2113. doi:10.1093/cid/ciaa588
60. Dagne H, Alemu KA, Dagnew B, et al. Prevention Practice and Associated Factors of Coronavirus Disease 2019 (COVID-19) Outbreak Among Educated Ethiopians: An Online Based Cross-Sectional Survey. 2020;preprint. doi:10.21203/rs.3.rs-34504/v1
61. Priyadarsini SL, Suresh M. Factors influencing the epidemiological characteristics of pandemic COVID 19: a TISM approach. Int J Healthcare Manag. 2021;11:89–98. doi:10.1080/20479700.2020.1755804
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.