Back to Journals » Clinical Ophthalmology » Volume 16
Costs and Healthcare Resource Utilization Associated with Posterior Capsule Opacification After Cataract Surgery with Five Different Intraocular Lenses: An Economic Analysis for Spain
Authors Belda JI, Placeres J, Elvira JC, Puig X, Pérez-Vives C, Zou M, Sun S, Yu J, O'Boyle D
Received 12 November 2021
Accepted for publication 21 January 2022
Published 31 March 2022 Volume 2022:16 Pages 993—1001
DOI https://doi.org/10.2147/OPTH.S349003
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
José I Belda,1 Javier Placeres,1 Juan Carlos Elvira,2 Xavier Puig,3 Caridad Pérez-Vives,4 Ming Zou,5 Shaohui Sun,5 Jing Yu,5 Derek O’Boyle6
1Hospital Universitario de Torrevieja, Torrevieja, Alicante, Spain; 2Hospital Universitario del Vinalopó, Elche, Alicante, Spain; 3Alcon Healthcare, S.A, Barcelona, Spain; 4Alcon Management SA, Cointrin, Switzerland; 5IQVIA Real World Solutions, Basel, Switzerland; 6Alcon Laboratories Ireland Ltd., Cork, Ireland
Correspondence: Derek O’Boyle, Alcon Laboratories Ireland Ltd., Cork, Ireland, Email [email protected]
Purpose: To estimate the economic impact of neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy and its related complications for five different intraocular lenses (IOLs) from the payer and hospital perspectives in Spain.
Materials and Methods: The three-year incidence rates of Nd:YAG laser capsulotomy after cataract surgery with five different single-piece acrylic monofocal IOLs (AcrySof IOLs, AJL LLASY60, IOL Tech Stabibag, Medicontur Bi-flex, Zeiss Asphina) for 8293 patients were derived from odds ratios of multivariate analysis adjusted for age, gender, and diabetic retinopathy. A cost-consequence model for a hypothetical cohort of 2000 eyes was then developed to quantify the potential impact of Nd:YAG capsulotomy in terms of costs and time for each of the included IOLs, from the payer and hospital perspectives.
Results: The adjusted three-year Nd:YAG laser capsulotomy incidence was 5.0% (95% CI 3.9 to 6.1) for AcrySof and ranged from 26.0% to 44.0% for the other four IOLs. The average costs of Nd:YAG treatment and related complications were € 261.90 for payers and € 19.99 for hospitals. The average time needed for Nd:YAG treatment and related complications was 32.82 minutes. Model estimates based on 2000 hypothetical cataract surgeries showed that AcrySof IOLs could lead to cost savings between € 110,259.90 and € 205,591.50 for payers. For hospitals, time, and cost savings with AcrySof ranged from 230.29 hours and € 8415.79 compared to Zeiss Asphina to 429.40 hours and € 15,692.15 compared to AJL LLASY60 IOLs.
Conclusion: Post cataract surgery, AcrySof IOLs were associated with a significantly lower incidence of Nd:YAG treatment and its subsequent complications compared to other IOLs. Our analysis shows that IOL choice is an important factor that can reduce the burden for patients, payers, and hospitals.
Keywords: cost, resources, Nd:YAG capsulotomy, cataract, PCO, IOL
Plain Language Summary
Why carry out this study?
- Neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy is used to treat Posterior Capsule Opacification, however, can cause complications that increase the burden for patients and healthcare systems.
- Real world evidence (RWE) informed cost consequence analysis of Nd:YAG laser capsulotomy can support intraocular lens (IOL) choice to lower economic costs and burden to patients.
- RWE insights are still limited and prior economic studies mostly focused on the economic cost for payers, but did not consider additional time required to care for patients with complications from the perspective of hospitals, which is vital with respect to planning of healthcare resources.
- This study brings new RWE insights into the economic burden associated with post-operative Nd:YAG capsulotomy treatment outcomes associated with five commonly used IOLs from both the perspective of payers and hospitals in Spain.
What was learned from the study?
- AcrySof IOLs were associated with a significantly lower incidence of Nd:YAG laser capsulotomy and subsequent complications compared to four different IOLs.
- Among the investigated IOLs, AcrySof IOLs were the most cost effective for both payers and hospitals.
Introduction
The global leading cause of partial and complete blindness is cataract.1,2 The most commonly performed procedure for the medical treatment of cataracts is a surgery with lens replacement.3,4 In 2019, there were 450,247 cataract surgeries performed in Spain, making it the most frequently performed surgical procedure nationally.5 While safe and effective,6 the cataract surgery may cause posterior capsule opacification (PCO), which can lead to impaired contrast sensitivity, glare disabilities and reduced visual acuity.7,8 PCO is treated with neodymium-doped yttrium aluminum garnet (Nd:YAG) laser capsulotomy.7 This treatment, in turn, can be associated with further complications, including cystoid macular oedema (CME), late onset endophthalmitis, posterior vitreous detachment, reduction in vision, retinal detachment (RD), or uveitis,9–11 all of which affect patients’ function of vision and quality of life. Thus, PCO increases the burden to patients and healthcare systems due to the necessary Nd:YAG treatment and possible complications that require further specialist consultation and treatment.7,12 Given the sheer volume of cataract surgeries being performed annually,5 even small differences in costs per patient add up to significant overall costs to the healthcare system.13 It is therefore important for patients and for healthcare systems more generally to minimize PCO.
Prior studies reported that the incidence of PCO was associated with patient characteristics, such as age and ocular comorbidities, and with factors related to surgical procedures and technique, as well as IOL material and design characteristics.14,15 There have been a number of studies examining the effects of different IOL types on the incidence rate of PCO following cataract surgery.16 Across these studies lower Nd:YAG capsulotomy rates after cataract surgery were consistently associated with hydrophobic acrylic IOLs compared to hydrophilic acrylic IOLs. Recent studies conducted in Scandinavia and the UK showed that AcrySof hydrophobic IOLs were associated with lower PCO incidence and Nd:YAG laser capsulotomy compared to other hydrophobic or hydrophilic acrylic IOLs during three to five years after IOL placement.17–20 It has been suggested that superior outcomes could be due to the IOL material composition and the edge design of hydrophobic acrylic IOLs.14,15,21–23
While there are numerous studies examining the association between IOL type and incidence rate of PCO and Nd:YAG laser capsulotomy, real world evidence (RWE) insights into costs related to the placement of different IOLs are still limited. One study that followed up the patients for approximately 3.5 years after cataract surgery, showed that the average costs were significantly lower for hydrophobic IOLs compared to the hydrophilic IOLs, due to the decreased PCO risk.20 Several health economic studies from European countries that followed patients up for three to five years after cataract surgery found that AcrySof IOLs were generally most cost-effective compared to other IOLs, and could save millions of Euros in costs.24–26
Most of these previous studies focused on the economic costs for the payers and did not consider additional time and resources required to care for patients with complications from the perspective of hospitals. Such insights are vital with respect to the planning of healthcare resources.
More RWE from different perspectives is therefore needed to understand economic costs and resource use associated with different IOLs. Furthermore, while previous work has been published which compares PCO related costs associated with hydrophobic and hydrophilic IOLs,20 this analysis adds comparative evidence relating to IOLs with a lens material classified as hydrophilic with a hydrophobic surface (Zeiss Asphina).
Adding to this, there are only limited previous investigations in Spain, where the most recent study, which focused on the cost only, was conducted more than ten years ago.25 We therefore conducted a study that extends our previous RWE investigation on Nd:YAG incidence after cataract surgery and provides an economic assessment of the financial costs and time investment for payers and hospitals in Spain.27 The objective was to estimate the health economic impact of five different single-piece, acrylic monofocal IOLs (Alcon AcrySof (hydrophobic), AJL LLASY60, Medicontur Bi-flex, IOL Tech Stabibag (all hydrophilic) and Zeiss Asphina (hydrophilic with a hydrophobic surface) and the costs associated with PCO and the Nd:YAG procedure, as well subsequent complications from both the perspective of payers and hospitals in Spain.
Materials and Methods
Patient Population
The original study (Belda et al, 2021) was conducted in two large Spanish regional hospitals of the Ribera Salud group in the Torrevieja-Vinalopó healthcare area, which are the primary providers of ophthalmic procedures in this Alicante region.27 We followed 14,519 eyes from 9545 patients (47% male, mean age = 75± 5.9 years) up for three years after cataract surgery to monitor Nd:YAG capsulotomy events. Of these, a total of 1647 further eyes were followed for up to six months to assess subsequent complications following Nd:YAG capsulotomy treatment. The data were fully anonymized and compliant with the Spanish data protection rules governing use of patient-level healthcare data, including anonymization of physician names in the dataset (as defined in the newly enforced EU General Data Protection Regulation, 25 May 2018). The study received ethical approval from Ribera Salud’s Clinical Research Ethics Committee (CEIC) and was in compliance with the Declaration of Helsinki. Due to anonymization of all patient level data at the participating sites prior to analysis and the retrospective nature of the study, informed consent was not required from the institution’s ethics committee. The details of the study population have been described elsewhere.27 The modelling analysis assumed a hypothetical cohort of 2000 annual cataract procedures, conducted in the Spanish National Health System.
Data Extraction
Data were extracted from medical records for patients who had cataract surgery with five different IOLs, including Alcon AcrySof, AJL LLASY60, Medicontur Bi-flex, IOL Tech Stabibag and Zeiss Asphina.27 The specific of intra- and post- Nd:YAG capsulotomy procedure complications that were extracted are illustrated in Table 1. All data were coded using system wide Ribera Salud proprietary procedure codes, along with procedure descriptors and International Classification of Disease-10 diagnosis codes.27,28
 |
Table 1 Average Time and/or Cost Required from Payers and Hospitals for the Nd:YAG Treatment and Related Complications a |
Analysis
We first computed odds ratios (OR) and three-year incidence rates of Nd:YAG capsulotomy by IOL type. Subsequently, a similar cost-consequence model to the one reported by Dhariwal et al (2019)26 was used to quantify the health care resource utilization and cost impact of Nd:YAG capsulotomy by IOL type (AcrySof, LLASY60, Bi-flex, Stabibag and CT Asphina). Costs associated with Nd:YAG treatment and its related complications up to three years after cataract surgery were analyzed from the perspective of payers. Efficiency gains and potential costs associated with time spent carrying out Nd:YAG treatment and other PCO related procedures were also estimated from a hospital perspective. In our analysis it was assumed that the five included IOLs shared the same prices, because in the Spanish National Healthcare System the cataract surgery tariff include the IOL costs. Thus, the general costs of cataract surgery are equivalent regardless of the type of IOL that is used. All analyses were performed using Microsoft Excel.
Cost-Consequence Model Analysis
Clinical Inputs
The incidence rates of Nd:YAG capsulotomy three years after cataract surgery with 95% confidence intervals (CIs) were attained from the data available from the previously published original RWE study, where ORs were adjusted for age, gender and diabetic retinopathy in multivariate analysis for each IOL with AcrySof as the reference group.27 The different types of complications, with their associated costs, and consultation time among 1647 cases were analysed based on RWE data.27
Cost Inputs
The costs were estimated from the payer and hospital perspectives. All the analyses took the direct treatment costs into account. For payers these included Nd:YAG laser capsulotomy costs and costs for the treatment of related complications (Table 2), expressed in euros (€). The direct costs were sourced from publically available healthcare costs statistics for the Valencian Community.29
 |
Table 2 Adjusted Nd:YAG Capsulotomy Incidence Rates for Different IOL Groups at Three Years Post-Cataract Surgery (Derived from Odd Ratios)26 |
For hospitals, we analysed specialist staff consultation time (expert clinical opinion) for Nd:YAG laser capsulotomy and its related complications. We estimated the total cost savings for hospitals depending on IOL type, based on the costs of a specialist per minute.30
Model Outputs
We report the estimated reduction in Nd:YAG capsulotomy events, costs and specialist staff time spent in relation to Nd:YAG capsulotomy with 95% CIs. The estimated incidence rate of Nd:YAG capsulotomy procedures was utilized for calculating the lower and upper values of number reduction between AcrySof and the four other IOLs. The total cost savings were assessed with respect to reduction in Nd:YAG laser capsulotomy events with the AcrySof IOL compared to the other IOLs, from the payer and hospital perspectives. Moreover, total time savings were estimated only considering the hospital perspective.
Sensitivity Analysis
A sensitivity analysis was conducted to obtain the minimum and maximum savings for the comparisons between AcrySof and the other four IOLs to evaluate the robustness of the economic analysis. The lower and upper values for Nd:YAG capsulotomy event reduction was derived from the available CI values. A ±10% variation in costs was applied to the lower and upper values of all events to derive the minimum and maximum cost differences between AcrySof and the other four IOLs.
Results
Clinical Results
Table 2 shows the ORs and three-year incidence rates of Nd:YAG capsulotomy by IOL type from the original clinical research which underpinned the economic analysis.27 The multivariate analysis showed that odds for Nd:YAG laser capsulotomy were significantly higher for AJL LLASY60, Medicontur Bi-flex, IOL Tech Stabibag and Zeiss Asphina compared to Alcon AcrySof, with ORs of 8.85, 5.86, 5.74, and 5.21 respectively. Using the OR, the three-year incidence of Nd:YAG after cataract surgery was estimated to be 5% (95% CI 3.9 to 6.1) for Alcon AcrySof, while it ranged from 21.2% to 31.1% for the other four IOLs.
Cost Results
Table 1 illustrates costs and time associated with Nd:YAG treatment with related complications for 1647 Nd:YAG eyes within three years from the payer and hospital perspectives. The cost of each Nd:YAG treatment was €242.48, which comprised a specialist’s consultation fee and Nd:YAG laser capsulotomy cost. From the payer’s perspective, the cost of each Nd:YAG treatment with related complications was €261.90. From the hospital’s perspective, the estimated specialist time for each Nd:YAG treatment with related complications was 32.82 minutes. The cost for hospital HCP per Nd:YAG treatment with related complications amounted to €19.99. The detailed estimates for staff time for Nd:YAG treatment and its subsequent complications are shown in Supplementary Table 1.
The cost-consequence analysis results from the payer and hospital perspectives are presented in Tables 3 and 4, respectively. For the hypothetical cohort of 2000 cataract eyes the estimation from the payer perspective shows that the cost savings estimates ranged from €110,259 (AcrySof compared to Zeiss Asphina) to €205,591 (AcrySof compared to LLASY60). Similarly, for the hospital HCP the estimation shows that time and costs savings with AcrySof IOLs could range from 230.29 hours and €8,415.79 compared to CT Asphina up to 429.40 hours and €15,692.15 compared to AJL LLASY60 (Table 4).
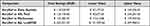 |
Table 3 Cost Savings per 2000 Cataract Eyes for the IOL Groups from the Payer Perspective |
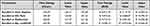 |
Table 4 Time and Cost Savings per 2000 Cataract Eyes for the IOL Groups from the Hospital Perspective |
Discussion
To our knowledge our study is the first economic analysis based on a longitudinal cohort study that investigated the economic impact of Nd:YAG capsulotomy after cataract surgery with five different single-piece, monofocal, acrylic IOLs from a Spanish healthcare perspective. When considering not only the cost of the cataract surgery but also its related complications over three years, we estimated that AcrySof IOLs could substantially reduce the economic burden for payers (from €110,259.90 to €205,591.50) and save the health care resources in terms of time and money for hospitals (from 230.29 to 429.40 hours and €8415 to €15,692), when compared to four other IOLs, including AJL LLASY60, IOL Tech Stabibag, Medicontur Bi-flex and Zeiss Asphina. In line with previous work,20,24–26 our findings highlight the importance of IOL choice with respect to economic costs and resources for both payers and hospitals.
The three-year incidence of Nd:YAG capsulotomy in this expanded RWE study showed the overall incidence rate after cataract surgery was approximately 14%, and rates were significantly lower for AcrySof IOLs (5%) compared to the other included IOLs (for a detailed report see27). Our subsequent cost-consequence analysis estimated that IOL choice also reduces the burden on resources for health care providers. This is important, particularly seen through the prism of the COVID-19 pandemic;31 avoidance of PCO means that patients will have fewer hospital visits and as such, resources can be liberated to elsewhere in eye-care services,32 as well as reducing the risk of infection for patients and healthcare professionals.
Our study showed cost and time savings for the hydrophobic compared to the hydrophilic IOLs. The savings were the largest for AcrySof compared to AJL LLASY60 IOLs, which had the highest risk for Nd:YAG incidence among the investigated IOLs.27 Our findings are in line with a previous study which was conducted in UK, Italy and Denmark which showed that hydrophobic IOLs were associated with a lower risk of PCO and Nd:YAG capsulotomy, resulting in a lower costs in total compared to hydrophilic IOLs.26 Economic studies comparing costs related to cataract surgery with hydrophobic and hydrophilic IOLs in Poland, Germany and Netherlands showed similar results.33–35 In the current study the difference in Nd:YAG incidence rate between hydrophilic IOLs with hydrophobic surface and without hydrophobic surface was slightly lower. This is reflected in comparatively smaller cost and time savings for AcrySof vs Zeiss Asphina. Previous research indicates that hydrophobic IOLs are associated with a substantially lower incidence of Nd:YAG compared to other IOL material types.17–20,36,37 Our work and the work of others25,26 suggests that they will be associated with substantially lower costs. It has been hypothesized that a lower water content and higher fibronectin bio-adhesion properties of hydrophobic acrylic IOLs may account for the beneficial effects with respect to PCO incidence and related complications.16
The current results need to be interpreted in the light of some methodological considerations. Firstly, we assumed the price is the same for AcrySof IOLs and other IOLs. However, in a healthcare system where service is not universally provided for free, the prices of the IOLs may differ from each other and become an important factor in selecting IOLs for the hospital.33 Under such a scenario, our assumption may not hold and the surcharge caused by different IOLs may need to be taken into account. Furthermore, while our study quantified direct costs for the IOLs, as well as for subsequent complications associated with the IOLs, other costs to patients, their relatives and health care systems have not been considered.38,39 For example, indirect costs might arise due to the challenges related to loss of full binocular vision, that are associated with a reduced quality of vision and life, and with an increased risk of falling and traffic accidents.40–43 Future studies could include such indirect costs in the evaluation of the economic impact of PCO, to produce more holistic cost estimates. Future studies should also consider the direct and indirect costs associated with IOL choice and PCO over longer follow-up durations to gain better insights into the long-term economic effects.
Conclusion
This study is the first to report on Nd:YAG capsulotomy treatment related economic impact and to report costs in relation to five different IOL types harnessing RWE data from Spain. Our study showed that from the payer and hospital perspectives IOL choice is an important economic factor. AcrySof IOLs are associated with lower costs for both payers and hospital HCP, due to substantial lower Nd:YAG capsulotomy rates and a lower risk for complications in three years after cataract surgery.
Abbreviations
DRG, diagnosis-related groups; HCP, healthcare personnel; IOLs, intraocular lenses; Nd:YAG, neodymium-doped yttrium aluminum garnet; OR, odds ratio; PCO, Posterior Capsule Opacification; RWE, real-world evidence.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors would like to thank Tatiana Padilla Sanchez from Ribera Salud IT Department for help with the data extraction. Editorial assistance in the preparation of this article was provided by Anne-Kathrin Fett from IQVIA.
Funding
This study was sponsored by Alcon Management SA (Geneva, Switzerland). Alcon is the market Authorisation holder of AcrySof® IOLs. Ribera Salud received payment for the data extraction. IQVIA received financial support from Alcon to conduct this study.
Disclosure
JIB reports grants from Alcon, during the conduct of the study. JP reports personal fees from AVI (Allergan) for presentation/Webinar, outside the submitted work. DOB, XP, and CPV are employees of Alcon. MZ, JY and SS are employees of IQVIA. The authors report no other conflicts of interest in this work.
References
1. Jacobs D, Trobe J, Park L. Cataract in adults; 2011.
2. Thylefors B, Negrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull World Health Organ. 1995;73(1):115–121.
3. Lum F, Feder RS, McLeod SD, Parke DW. The preferred practice pattern guidelines in ophthalmology. Ophthalmology. 2016;123(5):928–929. doi:10.1016/j.ophtha.2016.01.024
4. NICE. Cataracts in adults: management; 2017.
5. European Commission. Surgical operations and procedures statistics. 2018. European Commission; 2020.
6. Sheard RM, Goodburn SF, Comer MB, Scott JD, Snead MP. Posterior vitreous detachment after neodymium: yAGlaser posterior capsulotomy. J Cataract Refract Surg. 2003;29(5):930–934. doi:10.1016/S0886-3350(02)01837-0
7. Karahan E, Er D, Kaynak S. An overview of Nd: YAGLaser capsulotomy. Med Hypothesis Discov Innov Ophthalmol. 2014;3(2):45–50.
8. Maedel S, Buehl W, Findl O. Intraocular lens optic edge design for the prevention of posterior capsule opacification after cataract surgery. Cochrane Database Syst Rev. 2017;2017. doi:10.1002/14651858.CD012516.pub2
9. Lundstrom M, Barry P, Henry Y, Rosen P, Stenevi U. Evidence-based guidelines for cataract surgery: guidelines based on data in the European registry of quality outcomes for cataract and refractive surgery database. J Cataract Refract Surg. 2012;38(6):1086–1093. doi:10.1016/j.jcrs.2012.03.006
10. Bhargava R, Kumar P, Sharma SK, Kaur A. A randomized controlled trial of peeling and aspiration of Elschnig pearls and neodymium: yttrium-aluminium-garnet laser capsulotomy. Int J Ophthalmol. 2015;8(3):590–596. doi:10.3980/j.issn.2222-3959.2015.03.28
11. Ge J, Wand M, Chiang R, Paranhos A, Shields MB. Long-term effect of Nd: YAGlaser posterior capsulotomy on intraocular pressure. Arch Ophthalmol. 2000;118(10):1334–1337. doi:10.1001/archopht.118.10.1334
12. Boureau C, Lafuma A, Jeanbat V, Smith AF, Berdeaux G. Cost of cataract surgery after implantation of three intraocular lenses. Clin Ophthalmol. 2009;3:277–285. doi:10.2147/opth.s4890
13. Behndig A, Montan P, Stenevi U, Kugelberg M, Lundstrom M. One million cataract surgeries: Swedish national cataract register 1992–2009. J Cataract Refract Surg. 2011;37(8):1539–1545. doi:10.1016/j.jcrs.2011.05.021
14. Vasavada AR, Raj SM, Shah GD, Nanavaty MA. Posterior capsule opacification after lens implantation: incidence, risk factors and management. Expert Rev Ophthalmol. 2013;8(2):141–149. doi:10.1586/eop.12.80
15. Thom H, Ender F, Samavedam S, et al. Effect of AcrySof versus other intraocular lens properties on the risk of Nd: YAGcapsulotomy after cataract surgery: a systematic literature review and network meta-analysis. PLoS One. 2019;14(8):e0220498. doi:10.1371/journal.pone.0220498
16. Perez-Vives C. Biomaterial influence on intraocular lens performance: an overview. J Ophthalmol. 2018;2018:2687385. doi:10.1155/2018/2687385
17. Auffarth GU, Brezin A, Caporossi A, et al. Comparison of Nd: YAG capsulotomy rates following phacoemulsification with implantation of PMMA, silicone, or acrylic intra-ocular lenses in four European countries. Ophthalmic Epidemiol. 2004;11(4):319–329. doi:10.1080/09286580490515116
18. Lindholm JM, Laine I, Tuuminen R. Five-year cumulative incidence and risk factors of Nd: YAGCapsulotomy in 10 044 hydrophobic acrylic 1-piece and 3-piece intraocular lenses. Am J Ophthalmol. 2019;200:218–223. doi:10.1016/j.ajo.2019.01.010
19. Johansson B. Clinical consequences of acrylic intraocular lens material and design: Nd: YAG-laser capsulotomy rates in 3 x 300 eyes 5 years after phacoemulsification. Br J Ophthalmol. 2010;94(4):450–455. doi:10.1136/bjo.2009.166181
20. Cullin F, Busch T, Lundstrom M. Economic considerations related to choice of intraocular lens (IOL) and posterior capsule opacification frequency - A comparison of three different IOLs. Acta Ophthalmol. 2014;92(2):179–183. doi:10.1111/aos.12026
21. Zhao Y, Yang K, Li J, Huang Y, Zhu S. Comparison of hydrophobic and hydrophilic intraocular lens in preventing posterior capsule opacification after cataract surgery: an updated meta-analysis. Medicine. 2017;96(44):e8301. doi:10.1097/MD.0000000000008301
22. Li Y, Wang J, Chen Z, Tang X. Effect of hydrophobic acrylic versus hydrophilic acrylic intraocular lens on posterior capsule opacification: meta-analysis. PLoS One. 2013;8(11):e77864. doi:10.1371/journal.pone.0077864
23. Cheng JW, Wei RL, Cai JP, et al. Efficacy of different intraocular lens materials and optic edge designs in preventing posterior capsular opacification: a meta-analysis. Am J Ophthalmol. 2007;143(3):428–436. doi:10.1016/j.ajo.2006.11.045
24. Aaronson A, Grzybowski A, Tuuminen R. The health economic impact of posterior capsule opacification in Finland comparing the two single-piece intraocular lenses: a cost-consequence analysis. Acta Ophthalmol. 2019;97(8):e1152–e3. doi:10.1111/aos.14139
25. Smith AF, Lafuma A, Berdeaux G, et al. Cost-effectiveness analysis of PMMA, silicone, or acrylic intra-ocular lenses in cataract surgery in four European countries. Ophthalmic Epidemiol. 2005;12(5):343–351. doi:10.1080/09286580500180598
26. Dhariwal M, Bouchet C, Jawla S. Comparing the long-term impact on health care resources utilization and costs due to various single-piece acrylic monofocal intraocular lens implantation during cataract surgery: a cost-consequence analysis for the United Kingdom, Italy, and Denmark. Clin Ophthalmol. 2019;13:169–176. doi:10.2147/OPTH.S190754
27. Belda J, Placeres J, Elvira J, et al. Nd:YAG capsulotomy incidence associated with five different single-piece monofocal intraocular lenses: a three-year Spanish real-world evidence study of 8293 eyes. Eye. 2021. doi:10.1038/s41433-021-01828-z
28. World Health Orgnization. International Statistical Classification of Diseases and Related Health Problems. 10th Revision.
29. Diari Oficial de la Generalitiat Valenciana. Num. 8020/ 30.12.2017. Available from: https://dogv.gva.es/datos/2017/12/30/pdf/2017_12159.pdf.
30. General Directorate of Professionals. Remuneration of the staff of Health Centers and Institutions. Exercise; 2019.
31. Toro MD, Brezin AP, Burdon M, et al. Early impact of COVID-19 outbreak on eye care: insights from EUROCOVCAT group. Eur J Ophthalmol. 2021;31(1):5–9. doi:10.1177/1120672120960339
32. The Lancet Microbe. COVID-19 vaccines: the pandemic will not end overnight. Lancet Microbe. 2021;2(1):e1. doi:10.1016/S2666-5247(20)30226-3
33. Raulinajtys-Grzybek M, Grabska-Liberek I, Opala A, Slomka M, Chrobot M. Budget impact analysis of lens material on the posterior capsule opacification (PCO) as a complication after the cataract surgery. Cost Eff Resour Alloc. 2020;18(1):19. doi:10.1186/s12962-020-00214-y
34. Kossack N, Schindler C, Weinhold I, et al. German claims data analysis to assess impact of different intraocular lenses on posterior capsule opacification and related healthcare costs. Z Gesundh Wiss. 2018;26(1):81–90. doi:10.1007/s10389-017-0851-y
35. Bosgra OJ, Busutil R, de Ruiter L, Vives C, O’Boyle D. PMD42 The direct costs associated with posterior capsule opacification in the Netherlands: a payer perspective. Value Health. 2019;22:S676–S7. doi:10.1016/j.jval.2019.09.1455
36. Ursell PG, Dhariwal M, Majirska K, et al. Three-year incidence of Nd: yAGcapsulotomy and posterior capsule opacification and its relationship to monofocal acrylic IOL biomaterial: a UK Real World Evidence study. Eye. 2018;32(10):1579–1589. doi:10.1038/s41433-018-0131-2
37. Ursell PG, Dhariwal M, O’Boyle D, Khan J, Venerus A. 5 year incidence of YAG capsulotomy and PCO after cataract surgery with single-piece monofocal intraocular lenses: a real-world evidence study of 20,763 eyes. Eye. 2020;34(5):960–968. doi:10.1038/s41433-019-0630-9
38. Janati A, Farough Khosravi M, Imani A, Javadzadeh A, Mazhar Gharamaleki M. Cost analysis of eye surgeries and comparison with approved governmental tariffs. Health Scope. 2017;6:e39948.
39. Sach TH, Foss AJ, Gregson RM, et al. Second-eye cataract surgery in elderly women: a cost-utility analysis conducted alongside a randomized controlled trial. Eye. 2010;24(2):276–283. doi:10.1038/eye.2009.112
40. Cetinkaya S, Cetinkaya YF, Yener HI, Dadaci Z, Ozcimen M, Acir NO. The influence of size and shape of Nd: yAGcapsulotomy on visual acuity and refraction. Arq Bras Oftalmol. 2015;78(4):220–223. doi:10.5935/0004-2749.20150057
41. Koch C, Santos B, Correia A, Paredes R, Braz L, Kara-Junior N. Evaluation of quality of life and visual acuity after posterior capsulotomy with neodymium: YAG laser in adults. Rev Bras Oftalmol. 2020;79:42–45.
42. Menezes C, Vilaça KHC, Menezes RLD. Falls and quality of life of people with cataracts. Rev Bras Oftalmol. 2016;75(1):40–44. doi:10.5935/0034-7280.20160009
43. Servat JJ, Risco M, Nakasato YR, Bernardino CR. Visual impairment in the elderly: impact on functional ability and quality of life. Clin Geriatr. 2011;19:49–56.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
