Back to Journals » ClinicoEconomics and Outcomes Research » Volume 13
Cost-Effectiveness of Domiciliary High Flow Nasal Cannula Treatment in COPD Patients with Chronic Respiratory Failure
Authors Sørensen SS , Storgaard LH , Weinreich UM
Received 24 March 2021
Accepted for publication 13 May 2021
Published 18 June 2021 Volume 2021:13 Pages 553—564
DOI https://doi.org/10.2147/CEOR.S312523
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Dean Smith
Sabrina Storgaard Sørensen,1 Line Hust Storgaard,2 Ulla Møller Weinreich2,3
1Danish Center for Health Care Improvements, Department of Clinical Medicine, Aalborg University, Aalborg, Denmark; 2Department of Respiratory Diseases, Aalborg University Hospital, Aalborg, Denmark; 3Department of Clinical Medicine, Aalborg University, Aalborg, Denmark
Correspondence: Sabrina Storgaard Sørensen
Danish Center for Healthcare Improvements (DCHI), Department of Clinical Medicine, Aalborg University, Aalborg, Denmark
Tel +45 9940 2710
Email [email protected]
Purpose: To evaluate the cost-effectiveness of long-term domiciliary high flow nasal cannula (HFNC) treatment in COPD patients with chronic respiratory failure.
Patients and Methods: A cohort of 200 COPD patients were equally randomized into usual care ± HFNC and followed for 12 months. The outcome of the analysis was the incremental cost per quality-adjusted life-year (QALY) gained, and the analysis was conducted from a healthcare sector perspective. Data on the patients’ health-related quality of life (HRQoL), gathered throughout the trial using the St. George’s Respiratory Questionnaire (SGRQ), was converted into EQ-5D-3L health state utility values. Costs were estimated using Danish registers and valued in British pounds (£) at price level 2019. Scenario analyses and probabilistic sensitivity analyses were conducted to assess the uncertainty of the results.
Results: The adjusted mean difference in QALYs between the HFNC group and the control group was 0.059 (95% CI: 0.017; 0.101), and the adjusted mean difference in total costs was £ 212 (95% CI: − 1572; 1995). The analysis resulted in an incremental cost-effectiveness ratio (ICER) of £ 3605 per QALY gained. At threshold values of £ 20.000– 30.000 per QALY gained, the intervention had an 83– 92% probability of being cost-effective. The scenario analyses all revealed ICERs below the set threshold value and demonstrated the robustness of the main result.
Conclusion: This is the first cost-effectiveness study on domiciliary HFNC in Europe. The findings demonstrate that long-term domiciliary HFNC treatment is very likely to be a cost-effective addition to usual care for COPD patients with chronic respiratory failure. The results must be interpreted in light of the uncertainty associated with the indirect estimation of health state utilities.
Keywords: economic evaluation, quality-adjusted life years, QALY, health state utilities, EQ-5D, high flow heated and humidified oxygen, HFNC
Introduction
Chronic obstructive pulmonary disease (COPD) is a highly disabling disease characterized by persistent airflow limitation.1 The disease is the single most important respiratory disease globally, affecting approximately 384 million people worldwide.1 COPD has many well-documented negative impacts on the health status of the patients and health-care resources. Due to the irreversible decline in lung function, the disease impairs patients’ health-related quality of life (HRQoL)2–4 and results in numerous contacts to the health-care system, absenteeism, and an increasing need for help to carry out activities of daily living.5 Because of this, COPD is a disease with a high socio-economic impact. In Denmark, COPD is estimated to account for approximately 10% of total health-care costs for treating patients of 40 years or more, amounting to closely 2.5 billion Danish Kroner per year.6,7 The high costs are primarily driven by COPD exacerbations (AECOPD) requiring hospitalization,6,8–12 but also the use of primary care resources are considerable,13 and escalate with an increase in disease severity.14,15 Furthermore, expenses for home care are significantly higher in COPD patients compared to their peers.16,17
COPD is progressive by nature, however, early diagnosis and appropriate treatment can slow down the deteriorative process.18 Recently, it has been indicated that even in severely ill COPD patients with chronic respiratory failure, procrastination of disease progression can be obtained using long-term, domiciliary treatment with humidified high flow nasal cannula (HFNC).19,20 HFNC has been shown to reduce the number of exacerbations and number of hospitalizations and stabilize the quality of life in COPD patients.19,21,22 In addition, with long-term use, HFNC leads to a reduction in hypercapnia.23 However, the evidence of the cost-effectiveness of HFNC is less clear and has to date only been assessed in two studies; one being a study with only short-term follow-up and the other a study on a population of patients with various obstructive lung diseases.21,24
The purpose of the present study was to provide further evidence on the cost-effectiveness of domiciliary HFNC treatment by presenting the results of a post hoc cost-utility analysis of HFNC as an add-on treatment for patients with COPD and chronic hypoxic failure. The study was based on data from the only long-term, randomized controlled trial on domiciliary HFNC for this patient group19 and is the first study to assess the cost-effectiveness of domiciliary HFNC in a European setting.
Methods
In the study, 200 COPD patients with chronic hypoxic failure living in the North Jutland Region of Denmark were included between December 2013 and July 2015. Inclusion criteria were chronic hypoxic failure (ie, three arterial blood gasses (ABG) during stable conditions demonstrating hypoxemia)25 and previously prescribed long-term oxygen therapy (LTOT) by a Pulmonary Medicine specialist. Exclusion criteria were malignant disease, terminal nonmalignant disease, unstable psychiatric disease, and long-term non-invasive ventilation (LT NIV). For further detail of the recruiting- and inclusion process, please see.19 Patients were randomized to either usual care, including LTOT as previously prescribed, or usual care plus HFNC (myAirvo™ 2 Humidified High Flow System (Fisher & Paykel Healthcare Ltd, Auckland, New Zealand)), which they were advised to use 8 hours per day, preferably during sleep. All patients were followed for 12 months. During the study, the patients had access to all their usual health-care services and medications.
Patients were informed according to the Helsinki Declaration and written informed consent was obtained before inclusion. Study approval was obtained from the North Jutland Ethical Committee (N-20,110,057), the Danish Data Protection Agency (2008–58-0028), and the study was registered at ClinicalTrials.gov (NCT 02731872).
Outcome Measure and Data Collection
Cost-effectiveness was assessed using a cost-utility analysis (CUA), where the outcome measures used were healthcare sector costs and quality-adjusted life-years (QALYs). QALY is a combined measure that takes both the quality and quantity of life lived into account.26 The analysis was conducted as a within-trial analysis and was performed in accordance with international guidelines.26,27 The time horizon of the CUA followed that of the clinical trial, ie 12 months; hence, no discounting was performed. All costs were calculated in 2019 values by use of the Danish Consumer price index. Costs were first calculated in Danish Kroner (DKK) but later converted to British pounds sterling (£) using an exchange rate of 877DKK per £100, as per December 31, 2019.28
Measure of Effectiveness
Information on the patients’ health-related quality of life (HRQoL) was gathered during the clinical trial using the St. George’s Respiratory Questionnaire (SGRQ), which is a disease-specific 40-item questionnaire designed to measure the HRQoL of COPD patients.29 The patients completed the questionnaire at scheduled in-clinic visits at baseline and after six and 12 months. Using a validated mapping algorithm,30 total SGRQ scores at the three time points were converted to health state utility values (EQ-5D-3L utility values) to calculate QALYs. Patients dying during the study received an EQ-5D-3L utility value of zero at the time of death. QALY was calculated using linear interpolation. Demographic data, such as age, sex, smoking status, etc., were also collected at baseline. Days of treatment were registered by diary cards and were validated by data from the oxygen company. In case patients ceased using HFNC, they were asked to stay in the study during the 12 months.
Healthcare Service Use and Healthcare Costs
The analysis applied a Danish healthcare sector perspective; hence, the analysis included all costs related to primary care (general practice), secondary care (inpatient and outpatient hospital care), municipality-based health and social care (home nurse care, in-home assistance, household cleaning, and rehabilitation), costs associated with purchases of prescription medicine, and intervention costs. Costs borne by the patient or relatives were not included. The analysis only included disease-specific costs, except for general practice care and municipality-based care costs. It was not possible to distinguish between disease-specific and general resource use within those settings. Costs were gathered 12 months pre-study and during the 12 months study period. An overview of the different costs included in the analysis can be seen in Appendix A.
The patient-specific cost data were extracted from validated Danish registries using a unique personal identification number that each Danish citizen has. The personal identification number makes it possible to link individual data between registries. Data on primary and secondary healthcare resource use were extracted from the Northern Jutland Region registry. As for general practice, the date for each contact and type of service provided was listed in the register, and each contact was valued based on fees negotiated in a collective agreement with the Danish Medical Association.31 In the register, it was not possible to identify the cause of contact to general practice; hence, all contacts were included in the analysis. As for contacts in the secondary healthcare sector, the register provided information on the date of each contact, the diagnosis leading to the contact, procedures performed, and length of stay in case of an admission. Each contact was classified and valued according to the Danish diagnosis-related grouping (DRG) system.32
Data on the patients’ use of prescribed inhalation medicine (long-acting muscarinic agonist (LAMA) plus long-acting β2 agonist (LABA) plus inhaled corticosteroid (ICS); LAMA/LABA; LAMA/ICS or LABA/ICS; LAMA; LABA; ICS; SABA only); oral corticosteroids and antibiotics was gathered from the Danish Prescription Registry. The Anatomical Therapeutic Chemical Classification System (ACT) numbers included in the analysis are provided in Appendix B. The data included information on the date the medicine was redeemed at the pharmacy and type, number of packages issued, and cost of the medicine. The cost for prescription medicine was valued according to standardized pharmacy consumer prices and did not include the out-of-pocket expenses paid by the patients.33
The resource use of community care was estimated based on registrations from Aalborg Municipality, which is the largest municipality in the Region of Northern Jutland. Of the patients included in the study, 54% (n=108) lived in Aalborg Municipality during the trial, and the patients were equally distributed between the two groups. The registered time consumption for each care category was valued using average national effective hourly wage rates to increase generalizability to other Danish settings.34
Intervention Costs
Costs for the myAIRVO™ 2 and consumables were estimated in collaboration with the manufacturer (Fisher & Paykel Healthcare Ltd, Auckland, New Zealand), and the costs represented mean European prices. The cost for the myAIRVO™ 2 device was annuitized using an interest rate of 4% and assuming a 5-year lifetime of the device, as estimated by the manufacturer. The yearly cost for consumables included six breathing tubes, six autofill chambers, and 12 OptiflowTM nasal cannulas. Additional intervention costs included cost for setup, service, and an oxygen stand, delivered by the patients’ usual oxygen supply company (AGA Linde HealthCare, Fredericia, Denmark), based on Danish prices. The yearly cost for setup and service was calculated as an average of prices paid over the last five years. The oxygen stand was likewise annuitized using an interest rate of 4% and assuming a 5-year lifetime. The intervention costs did not include costs for LTOT, as this was similar in both the HFNC-group and controls. In Denmark, the cost for oxygen use is not per liter of oxygen used but for the service of oxygen delivery to the patient. Costs for water and electricity were considered insignificant and, hence, not included in the analysis.
Statistical Analysis
The analysis was conducted using the principles of intention-to-treat. Missing data were assumed to be missing at random (MAR), and multiple imputation was applied according to guideline.35 A description of the imputation model can be found in Appendix C.
Participant baseline data were provided as mean ± the associated standard deviation (SD) or absolute numbers. Raw between-group differences were evaluated at a significance level of p <0.05.
The cost-effectiveness of HFNC treatment was assessed by calculating the incremental cost-effectiveness ratio (ICER), ie, calculating the mean difference in costs divided by the mean difference in QALYs between the HFNC group and the control group.26 The incremental estimates of QALYs and costs were assessed using regression analysis, more specifically generalized linear models (GLMs).36 Several GLMs with different distributions and link functions were tested for QALYs and costs to ensure the most appropriate model fit. For QALYs, a GLM with Gaussian distribution and identity-link (ie ordinary least squares model) turned out to be the best fit as data followed a normal distribution. Due to the right-skewed distribution of the cost data, a GLM with gamma distribution and identity-link was chosen. To heighten the precision of the QALY and cost point estimates, baseline covariates were applied to the regression models. A patient’s baseline utility is highly correlated with his or her QALYs over the given follow-up period, and failure to correct for any imbalance in baseline mean utilities, irrespective of whether the differences are statistically significant or not, will lead to incorrect results.37 As such, in the base case analysis QALYs were corrected for baseline EQ-5D-3L utility, and total costs were corrected for baseline total costs in the 12 months before recruitment, as prescribed by published literature.37,38 Additionally, both outcomes were corrected for days of HFNC treatment in the study. Should the results of the unadjusted analyses be of interest to the reader, they can be assessed at.39
In addition to the base case analysis, four scenario analyses were performed to assess the uncertainty surrounding the point estimates of QALYs and costs. Like the base case analysis, the four scenario analyses were performed using GLM regression analysis. Except for scenario analysis one, all analyses were corrected for the same covariates as the base case analysis. Scenario analysis one was conducted to assess the impact of correcting for treatment days. As such, QALYs were only corrected for baseline EQ-5D-3L utility value, and total costs were only corrected for baseline total costs in the 12 months before recruitment in scenario one. The second and third scenario analysis assessed how much it influenced results if the intervention cost was 30% lower vs 30% higher, respectively than the estimate used in the base case analysis. The fourth scenario analysis was conducted as a complete case analysis to assess the impact of the imputation model on results.
To evaluate the decision uncertainty, probabilistic sensitivity analysis (PSA) was performed on the base case analysis and the scenario analyses by drawing 10,000 random trial simulations. A PSA is used to assess the impact of various uncertainties in parameter values on the probability of the intervention being cost-effective at different cost-effectiveness threshold values.36 Variance-covariance matrices were extracted from the regression of QALYs and costs, and Cholesky’s decomposition was applied to ensure correlation between the random draws. The simulations were used to generate incremental cost-effectiveness scatter plots and cost-effectiveness acceptability curves. The results of the PSA were presented at assumed cost-effectiveness threshold values of £20,000–30,000 per QALY gained.
All statistical analyses were performed in STATA version 15.1 and Microsoft Excel® 2016.
Results
All 200 recruited patients were included in the analysis. Patient baseline characteristics are listed in Table 1. No significant differences were seen between the two groups except for mMRC, where the HFNC group demonstrated a significantly higher score than the control group. Overall, the HFNC group presented with a considerably higher total mean cost in the year preceding recruitment when compared to the control group. The baseline variables with missing data were SGRQ (2% missing) and municipality costs (50% missing, including eight patients living in Aalborg Municipality). Patients from Aalborg Municipality did not differentiate on any demographic data from patients from the other participating municipalities.
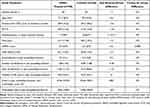 |
Table 1 Background Information on Total Study Population at Baseline |
HFNC treatment was on average used for 248 days, six hours/day, during the 12 months study period. Within the first month, 14% of the HFNC treated patients stopped using the device, and of those, 3% left the study. On average, the remaining 86% used HFNC for 286 days, 7 hours/day. By the end of the study, 33% of the HFNC group and 29% of the control group had left the study, including those who died. The mortality was similar between the two groups, with 15 deaths in the HFNC group and 12 deaths in the control group. Further details from the clinical study can be found elsewhere.19
Table 2 presents the raw non-imputed and unadjusted EQ-5D utility values for the HFNC group and the control group at baseline, six months, and 12 months. As demonstrated, the amount of missing data increased to 23% and 20% at six and 12 months. At baseline, the HFNC group had a somewhat lower utility value than the control group; however, at six and 12 months of follow-up, the utility values for the HFNC group were higher than the mean utility value in the control group. Both groups, however, suffered a decline in HRQoL during the study period, except at six months, where the mean utility value was stagnant for the HFNC group.
 |
Table 2 Non-Imputed and Unadjusted EQ-5D-3L Utility Values for the HFNC-Treated Group and the Control Group at Baseline, Six Months, and 12 Months of Follow-Up |
Except for municipality data, there were no missing data on costs as data were drawn from personally identifiable registers. Table 3 lists the resource consumption within the 12 months of follow-up and associated unit costs. As demonstrated, no significant differences could be observed between the HFNC group and the control group. It is also evident from the table that patients in both groups experienced almost no emergency room visits in the follow-up period. Table 4 presents the mean unadjusted costs per person in each group for all cost categories within the 12 months of follow-up. Compared to the control group, the HFNC group presented with a somewhat higher mean cost for hospital admission, but at the same time presented with a lower municipality cost. When including the intervention cost of £1235,85 per patient, the mean unadjusted total costs were higher in the HFNC group than in the control group, leading to a total raw difference of £788.57 per year.
 |
Table 3 Non-Imputed and Unadjusted Mean Resource Utilization per Patient for the HFNC-Treated Group and the Control Group Over the 12-Month Follow-Up and Applied Unit Costs |
 |
Table 4 Unadjusted Mean Costs (£) per Patient in the HNFC-Treated Group and the Control Group Over the 12-Month Follow-Up Presented into Cost Categories |
Cost-Effectiveness
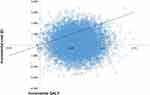
Table 5 presents the cost-effectiveness results of the base case analysis and the scenario analyses. When adjusting for baseline imbalances in the base case analysis, the difference in QALYs between the HFNC group and the control group was 0.059 (95% CI: 0.017; 0.101), indicating a significant mean gain in HRQoL for patients receiving HFNC treatment. The adjusted difference in costs was £212 (95% CI: −1572; 1995), indicating a non-significant increase in total mean costs per patient in the HFNC group. The base case analysis resulted in an ICER of £3605 per QALY gained, which is considered cost-effective at the given cost-effectiveness threshold value of £20.000–30.000 per QALY gained. The incremental cost-effectiveness scatter plot in Figure 1 presents the result of the PSA. The simulations are primarily plotted in the northeast and southeast quadrants, which agree with the HFNC treatment leading to a significant QALY gain at a small and insignificant increase in costs. The PSA of the base case analysis revealed that HFNC treatment was found to be cost-effective in 83% to 92% of the simulations at cost-effectiveness threshold values of £20.000–30.000 per QALY gained, respectively.
 |
Table 5 Incremental Cost-Effectiveness Ratios (ICERs) for the Base Case Analysis and Scenario Analyses |
The scenario analyses all found HFNC treatment to be associated with a gain in QALYs, and all except scenario analysis 1 found the QALY gain to be significant. The HFNC treatment was associated with a slight insignificant increase in cost for all analyses, except scenario analysis two that found the intervention to be cost-saving when compared to the control group. The cost-effectiveness result was relatively robust across the scenario analyses, demonstrating ICERs below the set cost-effectiveness threshold values and high probabilities of being cost-effective based on the PSA.
Discussion
This study evaluated the cost-effectiveness of HFNC treatment for patients with severe COPD and persistent respiratory failure in a Danish setting. This is the first cost-effectiveness study on HFNC in Europe and, to our knowledge, the first long-term study in COPD patients. The base case analysis resulted in an ICER of £3605 per QALY gained, and an 83–92% probability of being cost-effective at threshold values of £20.000–30.000 per QALY gained. Hence, HFNC treatment was demonstrated to be highly cost-effective when compared to usual practice. The findings from the scenario analyses were consistent with the result of the base case analysis, with all analyses demonstrating ICERs way below the set cost-effectiveness threshold.
In this study, the raw cost for COPD-related hospital admissions was higher in the HFNC group than in the control group within the 12 months of follow-up. Previously, a reduction in COPD-related admissions was found with increased use of HFNC.19 As the use of HFNC treatment varied much, and 14% of the patients stopped using the device within the first month after initiating treatment, correction for treatment days is believed to be of utmost importance when evaluating the cost-effectiveness of HFNC. It is worth noting; however, that cost-effectiveness was still demonstrated in scenario analysis 1, where no correction for treatment days was made.
The complete case analysis revealed an incremental QALY estimate that was relatively higher than for the base case analysis and the other scenario analyses. In a complete case analysis, it is assumed that data are missing completely at random and that the included patients are representative of those with missing data. However, a descriptive analysis of the missing data revealed that data were more likely to be missing at random. On these grounds, it was chosen to use the imputed dataset for the base case analysis, as the complete case analysis most likely provides a result that is not representative of the entire study population.
The vigilant reader will have noticed a discrepancy between the developments in HRQoL presented in the original study vs in the present study. Even though the analyses are based on the same data, the findings cannot be directly compared for two reasons. First, the HRQoL data presented in the original study had been adjusted for the use of HFNC, whereas the data listed in Table 2 are presented as raw data. Second, the HRQoL data in Table 2 includes the patients who died during the study. Those patients were assigned an EQ-5D-3L utility value of zero at the time of death, as it is the practice in calculating QALYs. This naturally affects the estimated HRQoL in both groups.
Both patient groups had very few emergency room (ER) visits in the year before inclusion and during the trial period. This is inconsistent with previous findings in COPD patients.40,41 There may be several, possibly inter-related explanations for this. For one, in the North Jutland Region of Denmark, where the trial was carried out, telehealth care (THC) is commonly used in the care of COPD patients. THC has, in a recent review by O’Connor, been suggested to reduce ER visits.42 Secondly, in Denmark, patients should be referred to the ER by the general practitioners, who also have an on-call shared duty out of office hours. Moderate exacerbations will, therefore, often be handled in this setting. Please note that costs for the on-call visits are included in general practitioner expenses in this analysis. Thirdly, most contacts to the ER lead to hospital admissions in this cohort of severely ill COPD patients, and as such, were not registered as ER visits.
A particular strength of the study was the nearly complete data on resource use. Most data were retrieved from well-validated Danish registries, which enables the estimation of costs with great accuracy. Municipality costs were estimated based on register data from Aalborg Municipality due to difficulties in retrieving data on resource use from the other municipalities. As more than half the patients included in the study lived in Aalborg Municipality, and they did not differ demographically at baseline from patients living in the other participating municipalities, multiple imputation was used to generate plausible imputed data for the entire population.
Economic evaluation of devices often raises methodological challenges that are overlooked by international guidelines for economic evaluation, as they have been written with pharmaceuticals in mind.43 One of such challenges is the estimation of the cost of the device, as prices often change over time due to iterative product developments, market dynamics, and differences in how devices are procured in healthcare systems. Changes in costs may affect cost-effectiveness and, ultimately, decisions about adoption. Another strength of this study was, therefore, the examination of how price variation of the device and associated service affected the estimate of cost-effectiveness in scenario analysis 2 and 3. When the intervention cost was lowered by 30%, HNFC was a dominant treatment strategy compared to usual practice. Applying a 30% higher intervention cost resulted in an ICER of £10,146 per QALY gained, which is still considered cost-effective at the given cost-effectiveness threshold value. It should also be highlighted that the price of the device represented mean European prices, which is believed to improve the generalizability of the findings to other European settings. Even though efforts were made, it was not possible to obtain European prices for service due to different providers and setups. As such, the cost for service was estimated based on Danish prices. Generalizability of cost-effectiveness analyses to other countries can also be challenging due to differences in, eg, healthcare costs and organization of healthcare. Denmark has a well-established public healthcare system and a very systematic and well-developed system for COPD management, and costs for COPD care are therefore considerable. However, due to the transparent reporting of the methods used in this study, it is believed that decision-makers will be able to recognize similarities and differences in costs and thereby determine whether the findings can relate to their setting.
In this study, the study population consisted of patients with severe COPD and persistent respiratory failure; the patients had on average suffered from chronic respiratory failure for about two-and-a-half years and were therefore approaching palliative care. A cost-effective treatment for this disease severity is rarely seen. To date, only one other study by Milne et al24 has assessed the costs of long-term domiciliary HFNC. The modest-sized study, including patients with different obstructive lung diseases of mixed severity, using the device for an average of 1.6 hours per day, found domiciliary HFNC to be moderately cost-effective.24 The present study, including more than twice as many patients using the device on average six hours per day, is, therefore, a strong improvement in evidence of the cost-effectiveness of domiciliary HFNC. In domiciliary non-invasive ventilation, another add-on treatment for severely ill COPD patients, there are indications of cost-utility.44,45 The few studies that exist, however, are small, of variable quality or merely theoretical.44,45 Domiciliary HFNC is an emerging add-on to COPD patients with persistent respiratory failure, with strong indications of reducing dyspnea, reduction in exacerbation rates, and improved HRQoL.19,21,46–48 In contrast to domiciliary non-invasive ventilation,49 guidelines do not recommend using HFNC as an add-on treatment for severely ill COPD patients, and indications of cost-utility are therefore of utmost importance. This paper is therefore considered a sound contribution for possible future recommendations of HFNC.
There are, of course, limitations to this study. Theoretically, care organization may differ between municipalities, which could influence municipality costs; however, care orchestration in Denmark is generally very much aligned. The main limitation of this study was, however, the use of mapping to estimate EQ-5D-3L utility values from the SGRQ. The use of mapping poses a degree of uncertainty on its own. As such, it is generally advised that utility scores are measured as accurately as possible by the collection of HRQoL data during the clinical trial using a utility-based measure such as the EQ-5D.30 At present, there exists no mapping algorithm from SGRQ to EQ-5D for Denmark, and instead, a validated mapping algorithm based on UK EQ-5D-3L population preferences was used.30 Country-specific value sets should preferably be used to evaluate treatment effects, as differences can exist between countries on how value sets are generated and populations’ preferences for health states.50,51 However, high and significant correlations have been demonstrated between the UK, and the Danish EQ-5D-3L value sets,52 which supports the use of the algorithm in a Danish context.
Conclusion
This study demonstrates that domiciliary HFNC is likely to be highly cost-effective for patients with severe COPD and persistent respiratory failure compared to usual practice. Despite the uncertainties associated with the indirect estimation of health state utility values, the study delivers a robust estimate for possible future recommendations of domiciliary HFNC treatment in these severely ill patients.
Data Sharing Statement
The data could be obtained upon reasonable request from the corresponding author.
Acknowledgments
The authors would like to thank consultant Sophie Rokkedahl Jensen and data manager Dorthe Bruun Jakobsen from Aalborg Municipality for their assistance with the retrieval of patient-specific data on municipality-based resource use.
Author Contributions
Sabrina Storgaard Sørensen participated in the design of the economic evaluation, performed the analyses, and drafted the manuscript for publication. Line Hust Storgaard and Ulla Møller Weinreich were responsible for the execution of the clinical trial, participated in the design of the economic evaluation, acquired the data, and critically reviewed and recommended revisions to the manuscript. All authors contributed to data analysis, interpretation of findings, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The study received funding from the company Fisher & Paykel Healthcare Ltd and the North Jutland Region, Denmark. Fisher & Paykel Healthcare Ltd provided the HFNC devices (myAIRVO™ 2) and consumables used in the study and some administration costs. None of the funders had any role in data analysis, data interpretation, or writing of the manuscript. The authors report no other conflicts of interest in this work.
References
1. Augusti A, Beasley R, Celli BR, et al. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnoses, management, and prevention of COPD. 2020. Available from: http://www.goldcopd.org.
2. Jones PW. Issues concerning health-related quality of life in COPD. Chest. 1995;107(5 Suppl):187S–193S. doi:10.1378/chest.107.5_Supplement.187S
3. Duiverman ML, Wempe JB, Bladder G, Kerstjens HAM, Wijkstra PJ. Health-related quality of life in COPD patients with chronic respiratory failure. Eur Respir J. 2008;32(2):379–386. doi:10.1183/09031936.00163607
4. Ståhl E, Lindberg A, Jansson SA, et al. Health-related quality of life is related to COPD disease severity. Health Qual Life Outcomes. 2005;3(56):1–8. doi:10.1186/1477-7525-3-56
5. Quaderi SA, Hurst JR. The unmet global burden of COPD. Glob Health Epidemiol Genom. 2018;3(e4):2018–2020.
6. Bilde L, Rud Svenning A, Dollerup J, Bække Borgeskov H, Lange P. The cost of treating patients with COPD in Denmark - a population study of COPD patients compared with non-COPD controls. Respir Med. 2007;101(3):539–546. doi:10.1016/j.rmed.2006.06.020
7. Flachs EM, Eriksen LKM, Ryd JT, Dibba E, Skov-Ettrup LJK. Sygdomsbyrden I Danmark - Sygdomme [The Disease Burden in Denmark - Diseases]. Sundhedsstyrelsen. 2015.
8. Qureshi H, Sharafkhaneh A, Hanania NA. Chronic obstructive pulmonary disease exacerbations: latest evidence and clinical implications. Ther Adv Chronic Dis. 2014;5(5):212–227. doi:10.1177/2040622314532862
9. Toy EL, Gallagher KF, Stanley EL, Swensen AR, Duh MS. The economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a review. J Chron Obstruct Pulmon Dis. 2010;7(3):214–228. doi:10.3109/15412555.2010.481697
10. Geitona M, Hatzikou M, Steiropoulos P, Alexopoulos EC, Bouros D. The cost of COPD exacerbations: a university hospital-based study in Greece. Respir Med. 2011;105(3):402–409. doi:10.1016/j.rmed.2010.09.020
11. Perera PN, Armstrong EP, Sherrill DL, Skrepnek GH. Acute exacerbations of COPD in the United States: inpatient burden and predictors of costs and mortality. J Chron Obstruct Pulmon Dis. 2012;9(2):131–141. doi:10.3109/15412555.2011.650239
12. Press VG, Konetzka RT, White SR. Insights about the economic impact of chronic obstructive pulmonary disease readmissions post implementation of the hospital readmission reduction program. Curr Opin Pulm Med. 2018;24(2):138–146. doi:10.1097/MCP.0000000000000454
13. Punekar YS, Shukla A, Müllerova H. COPD management costs according to the frequency of COPD exacerbations in UK primary care. Int J COPD. 2014;9:65–73. doi:10.2147/COPD.S54417
14. Faes K, De Frène V, Cohen J, Annemans L. Resource use and health care costs of COPD patients at the end of life: a systematic review. J Pain Symptom Manage. 2016;52(4):588–599. doi:10.1016/j.jpainsymman.2016.04.007
15. García-Polo C, Alcázar-Navarrete B, Ruiz-Iturriaga LA, et al. Factors associated with high healthcare resource utilisation among COPD patients. Respir Med. 2012;106(12):1734–1742. doi:10.1016/j.rmed.2012.09.009
16. Persson HL, Lyth J, Wiréhn AB, Lind L. Elderly patients with COPD require more health care than elderly heart failure patients do in a hospital-based home care setting. Int J COPD. 2019;14:1569–1581. doi:10.2147/COPD.S207621
17. FitzGerald JM, Haddon JM, Bradley-Kennedy C, et al. Resource use study in COPD (RUSIC): a prospective study to quantify the effects of COPD exacerbations on health care resource use among COPD patients. Can Respir J. 2007;14(3):145–152. doi:10.1155/2007/921914
18. Welte T, Vogelmeier C, Papi A. COPD: early diagnosis and treatment to slow disease progression. Int J Clin Pract. 2015;69(3):336–349. doi:10.1111/ijcp.12522
19. Storgaard LH, Hockey H, Laursen BS, Weinreich UM. Long-term effects of oxygen-enriched nasal high flow treatment in COPD with chronic hypoxemic respiratory failure. Int J Chron Obstruct Pulmon Dis. 2018;13:1195–1205. doi:10.2147/COPD.S159666
20. Elshof J, Duiverman ML. Clinical evidence of nasal high-flow therapy in chronic obstructive pulmonary disease patients. Respiration. 2020;99(2):140–153. doi:10.1159/000505583
21. Nagata K, Kikuchi T, Horie T, et al. Domiciliary high-flow nasal cannula oxygen therapy for patients with stable hypercapnic chronic obstructive pulmonary disease a multicenter randomized crossover trial. Ann Am Thorac Soc. 2018;15(4):432–439. doi:10.1513/AnnalsATS.201706-425OC
22. Rea H, McAuley S, Jayaram L, et al. The clinical utility of long-term humidification therapy in chronic airway disease. Respir Med. 2010;104(4):525–533. doi:10.1016/j.rmed.2009.12.016
23. Storgaard LH, Hockey HU, Weinreich UM. Development in PaCO2 over 12 months in patients with COPD with persistent hypercapnic respiratory failure treated with high-flow nasal cannula - post-hoc analysis from a randomised controlled trial. BMJ Open Respir Res. 2020;7:1. doi:10.1136/bmjresp-2020-000712
24. Milne RJ, Hockey H, Rea H. Long-term air humidification therapy is cost-effective for patients with moderate or severe chronic obstructive pulmonary disease or bronchiectasis. Value Health. 2014;17(4):320–327. doi:10.1016/j.jval.2014.01.007
25. Hardinge M, Annandale J, Bourne S, et al. British Thoracic Society guidelines for home oxygen use in adults: accredited by NICE. Thorax. 2015;70(suppl 1):i1–i43. doi:10.1136/thoraxjnl-2015-206865
26. Drummond MF, Schulpher M, Claxton K, Stoddart GL, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes.
27. Ramsey SD, Willke RJ, Glick H, et al. Cost-effectiveness analysis alongside clinical trials II—an ISPOR good research practices task force report. Value Health. 2015;18(2):161–172. doi:10.1016/j.jval.2015.02.001
28. Valutakurser [Exchange rates]. Valutakurser. 2019. Available from: https://valutakurser.dk/.
29. Jones PW, Quirk FH, Baveystock CM. The St George’s respiratory questionnaire. Respir Med. 1991;85:25–31. doi:10.1016/S0954-6111(06)80166-6
30. Starkie HJ, Briggs AH, Chambers MG, Jones P. Predicting EQ-5D values using the SGRQ. Value Health. 2011;14(2):354–360. doi:10.1016/j.jval.2010.09.011
31. Honorartabel [Fee table]. Lægeforeningen. 2018. Available from: https://www.laeger.dk/sites/default/files/overenskomst_om_almen_praksis_ok18_endelig_udgave.pdf.
32. Afregning og finansiering (DRG) [Reimbursement and financing (DRG)]. Sundhedsdatastyrelsen. Available from: https://sundhedsdatastyrelsen.dk/da/afregning-og-finansiering.
33. Priser på medicin [Prices on medicines]. Lægemiddelstyrelsen. 2020. Available from: https://laegemiddelstyrelsen.dk/da/tilskud/priser/#.
34. Statistikbanken - LONS20: løn efter arbejdsfunktion, sektor, aflønningsform, lønmodtagergruppe, lønkomponenter og køn [Statistikbanken - LONS20: wages estimated based on job function, sector, payment form, employment group, wage component and gender]. Danmarks Statistik. 2019. Available from: www.statistikbanken.dk.
35. Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. Pharmacoeconomics. 2014;32(12):1157–1170. doi:10.1007/s40273-014-0193-3
36. Gray A, Wordsworth S, Wolstenholme JL, Clarke PM. Applied Methods of Cost-Effectiveness Analysis in Healthcare. Oxford University Press; 2010.
37. Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14:487–496. doi:10.1002/hec.944
38. van Asselt AD, van Mastrigt GA, Dirksen CD, Arntz A, Severens JL, Kessels AGH. How to deal with cost differences at baseline. Pharmacoeconomics. 2009;27(6):519–528. doi:10.2165/00019053-200927060-00007
39. Sabrina Storgaard Sørensen. Additional analyses of cost-effectiveness of domiciliary high flow nasal cannula treatment in COPD patients with chronic respiratory failure. 2021. Available from: https://vbn.aau.dk/ws/portalfiles/portal/410910107/Additional_analyses_of_Cost_effectiveness_of_Domiciliary_High_Flow_Nasal_Cannula_treatment_in_COPD_patients.pdf.
40. Patel JG, Coutinho AD, Lunacsek OE, Dalal AA. COPD affects worker productivity and health care costs. Int J COPD. 2018;13:2301–2311. doi:10.2147/COPD.S163795
41. Foo J, Landis SH, Maskell J, et al. Continuing to confront COPD international patient survey: economic impact of COPD in 12 countries. PLoS One. 2016;11(4):e0152618. doi:10.1371/journal.pone.0152618
42. O’Connor S. Tele-health-monitoring may decrease emergency room visits and hospitalisation in patients with COPD. Evid Based Nurs. 2020;23:18. doi:10.1136/ebnurs-2019-103080
43. Sorenson C, Tarricone R, Siebert M, Drummond M. Applying health economics for policy decision making: do devices differ from drugs? Europace. 2011;13:ii54–ii58. doi:10.1093/europace/eur089
44. Dretzke J, Blissett D, Dave C, et al. The cost-effectiveness of domiciliary non-invasive ventilation in patients with end-stage chronic obstructive pulmonary disease: a systematic review and economic evaluation. Health Technol Assess (Rockv). 2015;19(81):1–246.
45. Nicolini A, Stieglitz S, Bou-khalil P, Esquinas A. Cost-utility of non-invasive mechanical ventilation: analysis and implications in acute respiratory failure. A brief narrative review. Respir Investig. 2018;56(3):207–213. doi:10.1016/j.resinv.2017.12.011
46. Bräunlich J, Mauersberger F, Wirtz H. Effectiveness of nasal highflow in hypercapnic COPD patients is flow and leakage dependent. BMC Pulm Med. 2018;18(14). doi:10.1186/s12890-018-0576-x
47. Braunlich J, Seyfarth H-J, Wirtz H. Nasal high-flow versus non-invasive ventilation in stable hypercapnic COPD: a preliminary report. Multidiscip Respir Med. 2015;10(27):1–3. doi:10.4081/mrm.2015.299
48. Pisani L, Betti S, Biglia C, et al. Effects of high-flow nasal cannula in patients with persistent hypercapnia after an acute COPD exacerbation: a prospective pilot study. BMC Pulm Med. 2020;20(12):1–9. doi:10.1186/s12890-020-1048-7
49. Crimi C, Noto A, Princi P, et al. Domiciliary non-invasive ventilation in COPD: an international survey of indications and practices. J Chron Obstruct Pulmon Dis. 2016;13(4):483–490. doi:10.3109/15412555.2015.1108960
50. Xie F, Gaebel K, Perampaladas K, Doble B, Pullenayegum E. Comparing EQ-5D valuation studies: a systematic review and methodological reporting checklist. Med Decis Mak. 2014;34(1):8–20. doi:10.1177/0272989X13480852
51. Gerlinger C, Bamber L, Leverkus F, et al. Comparing the EQ-5D-5L utility index based on value sets of different countries: impact on the interpretation of clinical study results. BMC Res Notes. 2019;12(18). doi:10.1186/s13104-019-4067-9
52. Wittrup-Jensen K, Lauridsen J, Pedersen K. Modelling Danish EuroQol (EQ-5D) tariffs by applying the time trade-off method. Health Econ Pap Ser. 2008. Available from: http://static.sdu.dk/mediafiles/Files/Om_SDU/Centre/c_ist_sundoke/Forskningsdokumenter/publications/Workingpapers/20084.pdf. Accessed May 27, 2021.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.