Back to Journals » Journal of Inflammation Research » Volume 16
Correlation Between Systemic Immune-Inflammation Index and Suicide Attempts in Children and Adolescents with First-Episode, Drug-Naïve Major Depressive Disorder During the COVID-19 Pandemic
Authors Cui S , Liu Z, Liu Y, Yao G, Wu Y, Li J, Sun F, Sun L, Sun L
Received 1 August 2023
Accepted for publication 27 September 2023
Published 9 October 2023 Volume 2023:16 Pages 4451—4460
DOI https://doi.org/10.2147/JIR.S433397
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Shu Cui,1,* Zhiwei Liu,1,* Yun Liu,1 Gaofeng Yao,1 Yanhai Wu,1 Juanjuan Li,1 Feng Sun,1,2 Liang Sun,1,2 Longlong Sun1,2
1Department of Psychiatry, Third People’s Hospital of Fuyang, Fuyang, Anhui, 236000, People’s Republic of China; 2School of Mental Health and Psychological Sciences, Anhui Medical University, Hefei, Anhui, 238000, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Gaofeng Yao; Yanhai Wu, Department of Psychiatry, Third People’s Hospital of Fuyang, Wenxing Road, Fuyang, Anhui, 236000, People’s Republic of China, Email [email protected]; [email protected]
Objective: This study aims to investigate the association between the systemic immune-inflammatory index (SII) and suicide attempt (SA) in children and adolescents with first-episode, drug-naïve Major Depressive Disorder (MDD) during the COVID-19 pandemic.
Methods: A retrospective study was conducted on 263 MDD patients hospitalized at the Third Hospital of Fuyang City between 2020 and 2022. Patients were categorized into two groups based on the presence of previous SA. The study compared the differences in SII and clinical characteristics between the two groups and used the receiver operating characteristic (ROC) curve to determine the optimal critical value of SII and the area under the curve. Binary logistic regression was used to analyze the independent risk factors for SA.
Results: Compared with the patients without SA history, the patients with a personal history of SA had a higher mean HDRS scores (Z=− 2.369, p=0.018), higher mean neutrophil count (Z=− 2.870, p=0.004), higher mean platelet count (Z=− 2.155, p=0.031), and higher mean SII (Z=− 3.170, p=0.002). The optimal critical SII determined by the ROC curve was 548.15 (sensitivity = 63.2%, specificity = 83.1%), and the area under the curve was 0.661. After adjusting for gender, age, BMI, illness duration and HDRS score, the risk of total SA in patients with high SII was 8.296 times higher than in those with low SII (OR = 8.296, 95% CI: 3.803– 18.095, P < 0.001), The risk of recent SA was 13.922 times higher in patients with high SII than in those with low SII (OR = 13.922, 95% CI: 5.587– 34.693, p < 0.001). However, high SII was not a risk factor for past SA (OR = 0.547, 95% CI: 0.062– 4.842, P=0.587).
Conclusion: SII may be an inexpensive, easily accessible strategy that can assist in determining suicide risk in adolescents with MDD.
Keywords: major depressive disorder, suicide attempt, children and adolescents, systemic immune-inflammation index, first-episode
Introduction
Suicide is a multifaceted public health problem that affects people worldwide, resulting in approximately one million deaths each year.1 Suicide accounts for 12% of all deaths among young US adults aged 18–24 years.2 Suicide is categorized into suicidal ideation, suicidal planning, and suicide attempts. Additionally, newly available data point to deteriorating patterns in suicide behaviors since the start of COVID-19. When compared to the same period the year before, emergency department visits for suspected suicide attempts among girls aged 12 to 17 were 50.6% higher from February 21 to March 20, 2021, while they climbed by 3.7% among boys. Suicide has become the main cause of mortality in various regions.3 Having a depressive disorder is a major risk for suicidal behavior and suicide attempts in adolescents (10–19 years old).4,5
The intervention time between the emergence of suicidal thoughts and the completion of a suicide attempt is usually short, with one study showing that 47.6% of patients reported a duration of just 10 minutes or less between the first suicidal thought and the actual attempt.6 Although treatment began before suicidal behavior occurred in >55% of cases, treatment failed to prevent suicidal behavior from occurring.7 About one-third of adolescents with suicidal thoughts will continue to attempt suicide in the following 12 months.7 Recognizing past SA can help identify high-risk populations and assist mental health service agencies in tracking individuals with SA, which is key to preventing future suicide. However, there is currently no effective algorithm for predicting SA because suicide is associated with different risk factor variables in different countries, genders, and age groups.8–10 Exploring biological markers of prior SA in adolescents with first-episode drug-naïve MDD is important for suicide prevention.
The relationship between inflammation and depression has been extensively studied.11,12 The inflammation theory is one of the theories currently available about the pathogenesis of depression.13 Clinical trials have shown that patients with depression exhibit a widespread activation of immune inflammatory response.11,12 It is worth noting that the blood parameters of suicidal patients show significantly higher levels of inflammation compared to non-suicidal patients.14 In addition, some studies have found that people with inflammatory diseases are more likely to suffer from depression and suicide.15–17 A study evaluating the interaction of Compensatory Immune Response System (CIRS) and Inflammatory Response System (IRS) in MDD adolescents revealed that enhanced IL-6 trans signaling and pro-inflammatory TNF-α signaling were associated with increased IL-4 and IL-10-mediated anti-inflammatory activity.18 This study showed that women with MDD exhibited increased levels of IL-10 and TNF-α compared to healthy control women. In contrast, men with MDD exhibited increased levels of IL-4, IL-10, sIL-6R, Treg + Th2, and TNF-α / TNF-R1 compared to healthy control men.18 Several systematic reviews have described the close relationship between inflammation and adolescent depression and have shown subtle evidence of inflammatory dysregulation in adolescent depression. Among them, longitudinal studies support the positive association between depression and concurrent and future inflammation, suggesting a possible bidirectional link between depression and pro-inflammatory states.19,20
The systemic immune-inflammation index (SII) is a hematological indicator that is calculated based on the counts of peripheral blood lymphocytes, platelets, and neutrophils, and can reflect the systemic immune-inflammatory status. Previous studies have shown that SII is a potential inflammatory biomarker for predicting depression.21–23 For example, SII is significantly positively correlated with depression and anxiety scores in COVID-19 recovery patients.22 SII measured in the emergency department can predict more severe self-reported depression and post-traumatic stress disorder.23
Despite the potential of the SII in predicting depression, studies on its correlation with SA are limited, especially in Chinese children and adolescents during the COVID-19 pandemic. The present study investigated the correlation between SII and previous SA in Chinese children and adolescents with first-episode, drug-naïve MDD to investigate whether SII, a simple and easily available indicator of inflammation, is a biomarker of previous SA in children and adolescents with MDD.
Methods
Study Design and Participators
This retrospective study included children and adolescents with drug-naïve major depressive disorder (MDD) who were admitted to the Third People’s Hospital in Fuyang City, Anhui Province from January 2020 to December 2022 for their first depressive episode. China’s COVID-19 outbreak begins in December 2019 and ends in December 2022. The inclusion criteria were: (1) aged ≤18 years; (2) diagnosed with Major Depressive Disorder (MDD) according to the diagnostic criteria in the 10th edition of the International Classification Disease (ICD-10); (3) MDD patients with the first depressive episode. The exclusion criteria were: (1) having other psychiatric disorders that meet the criteria of other mental disorders in the ICD-10; (2) obesity (BMI> 30 kg/m2); (3) smoking ≥10 cigarettes/day; (4) having serious physical diseases such as tumors and diabetes; (5) current treatment with immunosuppressive or anti-inflammatory medications; (6) have taken antidepressants for more than 1 week in the last 3 month; (7) patients diagnosed with COVID-19 infection were excluded. The study was approved by the Ethics Committee of the Third People’s Hospital of Fuyang City and complied with the ethical principles of the Helsinki Declaration (Ethics Approval No.: 2019–340-07). Eligible patients and their parents provided written informed consent and were free to withdraw from the study at any time. Initially, 302 cases were included, of which 37 were excluded due to meeting the exclusion criteria, and 2 were excluded due to insufficient clinical data. Finally, 263 patients were included in the study.
Measurement of Suicide Attempt
Whether they had attempted suicide and whether these events had occurred in the 1 year prior to admission was recorded as a dichotomous variable (present or absent). Positive responses were reconfirmed by assessing the time, subjective severity, and frequency of suicide attempts. Recent SA is defined as one in which the most recent SA occurred within 7 days, and past SA is defined as one in which the most recent SA occurred before 7 days.24,25 In this study, the time period of 7 days is considered to be a relatively reasonable timeframe, neither so short as to consider only events in the short term, nor so long as to include too many past events.
Clinical Data Collection
Baseline demographic characteristics, discharge diagnosis, 17-item Hamilton Depression Rating Scale (HDRS) scores, and hematologic data were collected from medical records for this study. Suicide attempts and HDRS assessments in this study were performed by psychiatrists who had received uniform training, which contributed to the reliability of the results. Peripheral venous blood (fasting) was collected on the second day of hospitalization from 6:00 a.m. to 8:00 a.m. Blood samples were collected from the head vein and preserved in EDTA tubes. Total blood cell counts, including neutrophil, lymphocyte, and platelet counts, were analyzed using a Mindray BC-5380/BC-5180 hematology analyzer (Shenzhen, China). The SII formula was calculated as SII=neutrophil count (10^9/L) × platelet count (10^9/L) / lymphocyte count (10^9/L).
Statistical Analysis
All data were analyzed using SPSS 24.0 software. Frequency and proportion were used for categorical variables, while mean and standard deviation were used for continuous variables to describe the baseline characteristics of participators. Student’s t-test, Mann–Whitney U, or chi-square tests were used to compare groups’ differences. Using participators’ SA history as the gold diagnostic standard, the receiver operating characteristic curve (ROC) was used to determine the area under the curve (AUC) for judging the occurrence of SA in children and adolescents with MDD based on their SII at admission, and the optimal cutoff value of SII was determined by Youden’s index. Patients were divided into high SII and low SII groups based on the cut-off value. Finally, binary logistic regression analysis was used to explore the relationship between SA and SII level at admission, with age, gender, HDRS score, and SII level as independent variables. P < 0.05 was considered statistically significant.
Results
Sociodemographic and Clinical Characteristics
A total of 263 patients with depression were included based on the inclusion and exclusion criteria, among whom 85 (32.3%) were male and 178 (67.7%) were female. The age range was 9–18 years with a mean age of (14.77±1.79) years. Of the total patients, 38 (14.4%) had SA in the past, while 225 (85.6%) did not. In the patients with a personal history of SA, the number of SA was 1.16 ±0.44, 29 (76.3%) were female and 9 (23.7%) were male. The age range was 12–18 years with a mean age of (14.87±1.89) years. Of these, 31 patients’ SA occurred within seven days, defined as recent SA, and seven patients’ SA occurred before seven days, defined as past SA, as shown in Table 1.
 |
Table 1 Sociodemographic and Clinical Characteristics of Each Group |
Compared with the patients without SA history, the patients with a personal history of SA had a higher mean HDRS scores (Z=−2.369, p=0.018), higher mean neutrophil count (Z=−2.870, p=0.004), higher mean platelet count (Z=−2.155, p=0.031), and higher mean SII (Z=−3.170, p=0.002). There were no statistically significant differences between the two groups in terms of age, gender, BMI, and lymphocyte count (p>0.05), as shown in Table 1.
Variables Associated with SII
SII was significantly associated with depression severity (r =0.131, p = 0.034), number of SA (r = 0.204, p = 0.001), and BMI (r = 0.241, p< 0.001). Conversely, SII was negative associated with duration of illness (r =−0.138, p =0.026). No association was found between SII and age (r = 0.052, p = 0.402, Table 2).
 |
Table 2 Spearman Correlation Analysis for SII |
Gender Differences in Sociodemographic and Clinical Characteristics
Compared with male patients, female patients had lower age (t=3.141, P=0.035) and higher SII scores (Z=−2.432, P=0.015), and there was no statistically significant difference between the two groups in terms of BMI and other clinical test indices (P>0.05), as shown in Table 3.
 |
Table 3 Gender Differences in Sociodemographic and Clinical Characteristics |
Area Under the ROC Curve and Optimal Cutoff Value of SII
The ROC curve showed an area under the curve of 0.661 (95% CI: 0.550–0.772, p = 0.002). Based on the maximum Youden index, the optimal cutoff value of SII for predicting SA in children and adolescents with MDD was 548.15, with a sensitivity of 63.2% and a specificity of 83.1%, and a Youden index of 0.463, as shown in Figure 1 and Table 4. Based on this optimal cut-off value, patients were divided into a high SII group (n=62, 23.6%) and a low SII group (n=201, 76.4%).
 |
Table 4 Area Under the ROC Curve |
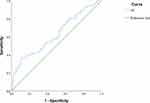 |
Figure 1 Receiver operating characteristic (ROC) curve of SII for predicting SA in children and adolescents with MDD. |
Binary Logistic Regression Analysis of Factors Affecting SA in Patients with Depressive Disorder
Binary multivariate logistic regression analyses were performed with SA (using total SA, recent SA, and past SA, respectively) as the dependent variable (positive = 1, negative = 0), and gender (male = 1, female = 2), age (years), BMI, illness duration (months), HDRS scores, and SII levels (high SII = 1, low SII = 0) as independent variables. After adjusting for gender, age, BMI, illness duration and HDRS score, the risk of total SA in patients with high SII was 8.296 times higher than in those with low SII (OR = 8.296, 95% CI: 3.803–18.095, P < 0.001), The risk of recent SA was 13.922 times higher in patients with high SII than in those with low SII (OR = 13.922, 95% CI: 5.587–34.693, p < 0.001). However, high SII was not a risk factor for past SA (OR = 0.547, 95% CI: 0.062–4.842, P=0.587). The logistic regression analysis models are shown in Table 5.
 |
Table 5 Binary Logistic Regression Analysis of Factors Influencing Suicide Attempt |
Discussion
The purpose of this study was to investigate the relationship between SII and suicide attempts in children and adolescents with first-episode, drug-naïve MDD. After controlling for confounding factors such as age, gender, HDRS score, and BMI, our study results showed that the risk of SA in patients with high SII was 8.296 times higher than in those with low SII. The high level of SII at admission was a significant independent risk factor for SA in children and adolescents with MDD. Based on our research findings, we recommend setting the optimal threshold value for SII at 548.15, which provides a sensitivity of 63.2% and a specificity of 83.1%. Previous studies showed that antidepressants have the effect of reducing the level of systemic inflammation in patients.26,27 Therefore, this study investigated children and adolescents with first-episode MDD because this reduces the effect of antidepressants on inflammatory markers in patients and is more clinically relevant.
A close relationship between suicide and different chronic inflammatory states has been found. Autoimmune diseases such as systemic lupus erythematosus and multiple sclerosis (MS) have been linked to an increased risk of death by suicide.16,28,29 Studies have indicated that the risk of suicidal behavior is higher in patients with immune activation, possibly due to increased neurotoxicity caused by inflammation and oxidative stress.30 Increased levels of inflammatory cytokines and their pro-inflammatory effects were strongly associated with depression and suicidal behavior,31–36 and levels of cytokines and chemokines were higher in blood and postmortem brain samples from suicidal patients than in non-suicidal patients and healthy controls.37,38
The relationship between depression and inflammation is bidirectional, and early adverse life experiences or chronic stress have been identified as important factors in establishing a link between inflammation and depressive symptoms. Several longitudinal studies have clearly demonstrated the role of IL-6, CRP, and TNF-α in minor MDD, but this role was mainly seen in individuals with more depressive episodes, higher severity of depressive symptoms, and the presence of preexisting risk factors such as adverse childhood experiences.39–42 In addition to this, higher baseline IL-6 and TNF-α changes predicted higher follow-up depressive symptoms at follow-up.43
Inflammation produces cytokines that affect 5-hydroxytryptamine and glutamate concentrations, which ultimately negatively affect basal ganglia and cortical reward and motor circuits, leading to depressive behavior and suicide.44–49 Studies have shown that there are two pathophysiological mechanisms by which nervous system inflammation affects depression and suicide: First, serotonin synthesis requires the involvement of the enzyme cofactor tetrahydrobiopterin (BH4), and inflammation and cytokines have been shown to reduce the availability of BH4.44 In addition, the inflammatory role is also associated with increased Nitric oxide synthase (NOS) activity and accelerated the breakdown of BH4.50,51 Increased oxidative stress leads to less BH4 available for the synthesis of monoamines such as serotonin, resulting in reduced production of a variety of monoamine neurotransmitters including serotonin in the nervous system.50 Another pathway by which inflammation of the nervous system leads to depression and suicide lies in the glutamate pathway, and cytokines and inflammation have been shown to increase glutamate concentrations in the nervous system by affecting microglia and astrocytes. A large body of literature has shown that inflammatory cytokines reduce the expression of glutamate transporters in astrocytes and increase glutamate release in astrocytes and activated microglia.45–48 Notably, glutamate released by glia may also preferentially enter the extra-synaptic n-methyl-D-aspartate receptor, which results in reduced production of trophic factors including brain-derived neurotrophic factor.52,53 Eventually, excess glutamate accumulates between nerve cells, and protective brain-derived neurotrophic factor decreases, leading to nerve cell poisoning and abnormal function.
Our study has both strengths and limitations. On the one hand, we studied children and adolescents with first-episode drug-naïve MDD and excluded patients with multiple episodes of MDD or repeated use of antidepressants to ensure the reliability of the results. This is because previous studies have found that antidepressants affect systemic levels of immune inflammation. On the other hand, we excluded patients with a BMI of more than 30, while controlling for age, gender, and depression severity to ensure the reliability of the results. Finally, our study focuses on suicidal behaviors of children with MDD during the COVID-19 epidemic, which is a research topic that is topical. The COVID-19 epidemic has had a tremendous impact on society, and our study contributes to the understanding of the impact of the epidemic on the mental health of children and adolescents, providing some insight into prevention and treatment in the aftermath of the epidemic. This study has the following limitations: (1) As a cross-sectional study, this study could not determine causality, but only provide correlation evidence. (2) This study did not consider the influence of individual differences, environmental factors, psychological factors, and other factors, which may have an impact on the results. (3) As a single-center study, the results have high internal validity, although the study design and data collection are relatively easy to control and standardize. However, the disadvantage is that the sample size is small, the results may not be representative enough, and the scope of application may be relatively small. (4) Although we documented the occurrence or non-occurrence of suicide attempts and further assessed participants who responded positively, the lack of use of the Beck Suicide Intentions Inventory (SSI) or a similarly standardized assessment tool may have compromised our overall measure and understanding of suicidal ideation. Future studies may consider the use of a more standardized suicidal ideation assessment tool to provide more accurate suicidal ideation assessment results.
Our findings suggest that high SII (SII>548.15) is an independent risk factor for SA (especially SA in the last 7 days) in first-episode, drug-naïve adolescent MDD patients. Therefore, the importance of systemic inflammation levels needs to be considered when assessing suicide risk in this population. Studies have also indicated that identifying subgroups of patients with both SA and immune dysregulation symptoms is a prerequisite for developing individualized treatment strategies.54 Therefore, detection of SII to identify subgroups of patients with SA and immune disorder symptoms could help physicians develop more effective and personalized suicide prevention and depression treatment strategies. This study chose to study SA in first-episode depressed children and adolescents rather than multiple episodes, which will help to better develop more effective early intervention strategies for this population, which is an important means of suicide prevention. The future research direction needs to comprehensively consider the characteristics of SII index and the current research progress in inflammatory treatment, formulate targeted inflammatory treatment strategies for high SII populations, and evaluate and observe the treatment effect, to provide more effective methods and means for clinical treatment.
Acknowledgments
We are grateful to all participators in our current study and those researchers who have contributed to the discipline.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; All authors gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Fuyang Municipal Health Commission Research Project [grant numbers FY2020xg14]; Fuyang Municipal Health Commission Research Project [grant numbers FY2021-147]. This source had no further role in this study design, in the data analysis, in the writing of the report, and in the decision to submit the paper for publication.
Disclosure
All authors report no conflicts of interest in this work.
References
1. World Health Organization. Public Health Action for Prevention of Suicide: A Framework. 2012
2. Eaton DK, Kann L, Kinchen S, et al. Youth risk behavior surveillance--United States, 2007. Morbidity Mortality Weekly Rep Surveillance Summaries. 2008;57(4):1–131.
3. Yard E, Radhakrishnan L, Ballesteros MF, et al. Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12-25 Years Before and During the COVID-19 Pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 2021;70(24):888–894. doi:10.15585/mmwr.mm7024e1
4. Barbeito S, Vega P, Sánchez-Gutiérrez T, Becerra JA, González-Pinto A, Calvo A. A systematic review of suicide and suicide attempts in adolescents with psychotic disorders. Schizophr Res. 2021;235:80–90. doi:10.1016/j.schres.2021.07.029
5. DeVylder JE, Lukens EP, Link BG, Lieberman JA. Suicidal ideation and suicide attempts among adults with psychotic experiences: data from the Collaborative Psychiatric Epidemiology Surveys. JAMA Psychiatry. 2015;72(3):219–225. doi:10.1001/jamapsychiatry.2014.2663
6. Deisenhammer EA, Ing CM, Strauss R, Kemmler G, Hinterhuber H, Weiss EM. The duration of the suicidal process: how much time is left for intervention between consideration and accomplishment of a suicide attempt? J Clin Psychiatry. 2009;70(1):19–24. doi:10.4088/JCP.07m03904
7. Nock M, Green J, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA psychiatry. 2013;70(3):300–310. doi:10.1001/2013.jamapsychiatry.55
8. O’Connor R, Nock M. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1(1):73–85. doi:10.1016/s2215-0366(14)70222-6
9. Afifi T, Enns M, Cox B, Asmundson G, Stein M, Sareen J. Population attributable fractions of psychiatric disorders and suicide ideation and attempts associated with adverse childhood experiences. Am J Public Health. 2008;98(5):946–952. doi:10.2105/ajph.2007.120253
10. Franklin J, Ribeiro J, Fox K, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull. 2017;143(2):187–232. doi:10.1037/bul0000084
11. Köhler C, Freitas T, Stubbs B, et al. Peripheral Alterations in Cytokine and Chemokine Levels After Antidepressant Drug Treatment for Major Depressive Disorder: systematic Review and Meta-Analysis. Mol Neurobiol. 2018;55(5):4195–4206. doi:10.1007/s12035-017-0632-1
12. Hernández M, Mendieta D, Martínez-Fong D, et al. Variations in circulating cytokine levels during 52 week course of treatment with SSRI for major depressive disorder. Eur Neuropsychopharmacology. 2008;18(12):917–924. doi:10.1016/j.euroneuro.2008.08.001
13. Gałecki P, Talarowska M. Inflammatory theory of depression. Psychiatr Pol. 2018;52(3):437–447. doi:10.12740/pp/76863
14. Ucuz İ, Kayhan Tetik B. Can suicide behavior and seasonality of suicide be predicted from inflammatory parameters in adolescents? Med Hypotheses. 2020;143:110061. doi:10.1016/j.mehy.2020.110061
15. Sher L. Post-COVID syndrome and suicide risk. QJM. 2021;114(2):95–98. doi:10.1093/qjmed/hcab007
16. Rafiei S, Raoofi S, Pashazadeh Kan F, et al. Global prevalence of suicide in patients living with HIV/AIDS: a systematic review and meta-analysis. J Affect Disord. 2023;323:400–408. doi:10.1016/j.jad.2022.11.061
17. Facanali CBG, Sobrado Junior CW, Fraguas Junior R, et al. The relationship of major depressive disorder with Crohn’s disease activity. Clinics. 2023;78:100188. doi:10.1016/j.clinsp.2023.100188
18. Ferencova N, Visnovcova Z, Ondrejka I, et al. Evaluation of Inflammatory Response System (IRS) and Compensatory Immune Response System (CIRS) in Adolescent Major Depression. J Inflamm Res. 2022;15:5959–5976. doi:10.2147/jir.S387588
19. Toenders YJ, Laskaris L, Davey CG, et al. Inflammation and depression in young people: a systematic review and proposed inflammatory pathways. Mol Psychiatry. 2022;27(1):315–327. doi:10.1038/s41380-021-01306-8
20. Colasanto M, Madigan S, Korczak DJ. Depression and inflammation among children and adolescents: a meta-analysis. J Affect Disord. 2020;277:940–948. doi:10.1016/j.jad.2020.09.025
21. Hu J, Wang L, Fan K, et al. The Association Between Systemic Inflammatory Markers and Post-Stroke Depression: a Prospective Stroke Cohort. Clin Interv Aging. 2021;16:1231–1239. doi:10.2147/cia.S314131
22. Mazza M, De Lorenzo R, Conte C, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. 2020;89:594–600. doi:10.1016/j.bbi.2020.07.037
23. Benedetti F, Palladini M, Paolini M, et al. Brain correlates of depression, post-traumatic distress, and inflammatory biomarkers in COVID-19 survivors: a multimodal magnetic resonance imaging study. Brain Behavior Immunity. 2021;18:100387. doi:10.1016/j.bbih.2021.100387
24. Velasco Á, Rodríguez-Revuelta J, Olié E, et al. Neutrophil-to-lymphocyte ratio: a potential new peripheral biomarker of suicidal behavior. Eur Psychiatry. 2020;63(1):e14. doi:10.1192/j.eurpsy.2019.20
25. Alacreu-Crespo A, Guillaume S, Richard-Devantoy S, Cazals A, Olié E, Courtet P. Clinical Dimensions Associated With Psychological Pain in Suicidal Patients: one-Year Follow-up Study. J Clin Psychiatry. 2022;83(2). doi:10.4088/JCP.21m14065
26. Tomaz VS, Chaves Filho AJM, Cordeiro RC, et al. Antidepressants of different classes cause distinct behavioral and brain pro- and anti-inflammatory changes in mice submitted to an inflammatory model of depression. J Affect Disord. 2020;268:188–200. doi:10.1016/j.jad.2020.03.022
27. Mello BSF, Chaves Filho AJM, Custódio CS, et al. Doxycycline at subantimicrobial dose combined with escitalopram reverses depressive-like behavior and neuroinflammatory hippocampal alterations in the lipopolysaccharide model of depression. J Affect Disord. 2021;292:733–745. doi:10.1016/j.jad.2021.05.083
28. Brønnum-Hansen H, Stenager E, Nylev Stenager E, Koch-Henriksen N. Suicide among Danes with multiple sclerosis. J Neurol Neurosurg Psychiatry. 2005;76(10):1457–1459. doi:10.1136/jnnp.2004.056747
29. Zakeri Z, Shakiba M, Narouie B, Mladkova N, Ghasemi-Rad M, Khosravi A. Prevalence of depression and depressive symptoms in patients with systemic lupus erythematosus: Iranian experience. Rheumatol Int. 2012;32(5):1179–1187. doi:10.1007/s00296-010-1791-9
30. Vasupanrajit A, Jirakran K, Tunvirachaisakul C, Maes M. Suicide attempts are associated with activated immune-inflammatory, nitro-oxidative, and neurotoxic pathways: a systematic review and meta-analysis. J Affect Disord. 2021;295:80–92. doi:10.1016/j.jad.2021.08.015
31. Li W, Ali T, Zheng C, et al. Anti-depressive-like behaviors of APN KO mice involve Trkb/BDNF signaling related neuroinflammatory changes. Mol Psychiatry. 2022;27(2):1047–1058. doi:10.1038/s41380-021-01327-3
32. Vai B, Mazza MG, Cazzetta S, et al. Higher Interleukin 13 differentiates patients with a positive history of suicide attempts in major depressive disorder. J Affective Disorders Reports. 2021;6:100254. doi:10.1016/j.jadr.2021.100254
33. Porter GA, O’Connor JC. Brain-derived neurotrophic factor and inflammation in depression: pathogenic partners in crime? World j Psychiatry. 2022;12(1):77–97. doi:10.5498/wjp.v12.i1.77
34. Keaton SA, Madaj ZB, Heilman P, et al. An inflammatory profile linked to increased suicide risk. J Affect Disord. 2019;247:57–65. doi:10.1016/j.jad.2018.12.100
35. Oh KY, Van Dam NT, Doucette JT, Murrough JW. Effects of chronic physical disease and systemic inflammation on suicide risk in patients with depression: a hospital-based case-control study. Psychol Med. 2020;50(1):29–37. doi:10.1017/s0033291718003902
36. Serafini G, Parisi VM, Aguglia A, et al. A Specific Inflammatory Profile Underlying Suicide Risk? Systematic Review of the Main Literature Findings. Int J Environ Res Public Health. 2020;17(7):2393. doi:10.3390/ijerph17072393
37. Black C, Miller B. Meta-Analysis of Cytokines and Chemokines in Suicidality: distinguishing Suicidal Versus Nonsuicidal Patients. Biol Psychiatry. 2015;78(1):28–37. doi:10.1016/j.biopsych.2014.10.014
38. Shinko Y, Otsuka I, Okazaki S, et al. Chemokine alterations in the postmortem brains of suicide completers. J Psychiatr Res. 2020;120:29–33. doi:10.1016/j.jpsychires.2019.10.008
39. Copeland WE, Shanahan L, Worthman C, Angold A, Costello EJ. Cumulative depression episodes predict later C-reactive protein levels: a prospective analysis. Biol Psychiatry. 2012;71(1):15–21. doi:10.1016/j.biopsych.2011.09.023
40. Rohleder N, Miller GE. Acute deviations from long-term trait depressive symptoms predict systemic inflammatory activity. Brain Behav Immun. 2008;22(5):709–716. doi:10.1016/j.bbi.2007.10.012
41. Gill H, El-Halabi S, Majeed A, et al. The Association Between Adverse Childhood Experiences and Inflammation in Patients with Major Depressive Disorder: a Systematic Review. J Affect Disord. 2020;272:1–7. doi:10.1016/j.jad.2020.03.145
42. Mac Giollabhui N, Ng TH, Ellman LM, Alloy LB. The longitudinal associations of inflammatory biomarkers and depression revisited: systematic review, meta-analysis, and meta-regression. Mol Psychiatry. 2021;26(7):3302–3314. doi:10.1038/s41380-020-00867-4
43. Khandaker GM, Pearson RM, Zammit S, Lewis G, Jones PB. Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life: a population-based longitudinal study. JAMA Psychiatry. 2014;71(10):1121–1128. doi:10.1001/jamapsychiatry.2014.1332
44. Neurauter G, Schröcksnadel K, Scholl-Bürgi S, et al. Chronic immune stimulation correlates with reduced phenylalanine turnover. Curr Drug Metab. 2008;9(7):622–627. doi:10.2174/138920008785821738
45. Dantzer R, Walker AK. Is there a role for glutamate-mediated excitotoxicity in inflammation-induced depression? J Neural Transm. 2014;121(8):925–932. doi:10.1007/s00702-014-1187-1
46. Tilleux S, Hermans E. Neuroinflammation and regulation of glial glutamate uptake in neurological disorders. J Neurosci Res. 2007;85(10):2059–2070. doi:10.1002/jnr.21325
47. Ida T, Hara M, Nakamura Y, Kozaki S, Tsunoda S, Ihara H. Cytokine-induced enhancement of calcium-dependent glutamate release from astrocytes mediated by nitric oxide. Neurosci Lett. 2008;432(3):232–236. doi:10.1016/j.neulet.2007.12.047
48. Takaki J, Fujimori K, Miura M, Suzuki T, Sekino Y, Sato K. L-glutamate released from activated microglia downregulates astrocytic L-glutamate transporter expression in neuroinflammation: the ‘collusion’ hypothesis for increased extracellular L-glutamate concentration in neuroinflammation. J Neuroinflammation. 2012;9(1):275. doi:10.1186/1742-2094-9-275
49. Felger JC. Imaging the Role of Inflammation in Mood and Anxiety-related Disorders. Curr Neuropharmacol. 2018;16(5):533–558. doi:10.2174/1570159x15666171123201142
50. Cunnington C, Channon KM. Tetrahydrobiopterin: pleiotropic roles in cardiovascular pathophysiology. Heart. 2010;96(23):1872–1877. doi:10.1136/hrt.2009.180430
51. Xia Y, Tsai AL, Berka V, Zweier JL. Superoxide generation from endothelial nitric-oxide synthase. A Ca2+/calmodulin-dependent and tetrahydrobiopterin regulatory process. J Biol Chem. 1998;273(40):25804–25808. doi:10.1074/jbc.273.40.25804
52. Hardingham GE, Fukunaga Y, Bading H. Extrasynaptic NMDARs oppose synaptic NMDARs by triggering CREB shut-off and cell death pathways. Nat Neurosci. 2002;5(5):405–414. doi:10.1038/nn835
53. Haydon PG, Carmignoto G. Astrocyte control of synaptic transmission and neurovascular coupling. Physiol Rev. 2006;86(3):1009–1031. doi:10.1152/physrev.00049.2005
54. Pape K, Tamouza R, Leboyer M, Zipp F. Immunoneuropsychiatry - novel perspectives on brain disorders. Nat Rev Neurol. 2019;15(6):317–328. doi:10.1038/s41582-019-0174-4
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
