Back to Journals » International Journal of General Medicine » Volume 14
Correlation Between Serum Tumor Marker Levels and Connective Tissue Disease-Related Interstitial Lung Disease
Authors Bao Y , Zhang W, Shi D, Bai W, He D, Wang D
Received 18 March 2021
Accepted for publication 3 June 2021
Published 15 June 2021 Volume 2021:14 Pages 2553—2560
DOI https://doi.org/10.2147/IJGM.S310917
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yunqi Bao,1 Wei Zhang,1 Dandan Shi,2 Weili Bai,1 Dongdong He,1 Dan Wang1
1Department of Rheumatology, Xi’an Fifth Hospital, Xian, 710000, Shaanxi, People’s Republic of China; 2Department of Radiology, Xi’an Fifth Hospital, Xian, 710000, Shaanxi, People’s Republic of China
Correspondence: Dan Wang
Department of Rheumatology, Xi’an Fifth Hospital, 112 Xiguanzheng Street, Lianhu District, Xian, 710000, Shaanxi, People’s Republic of China
Email [email protected]
Objective: The main aims of this study were to explore the relationships between serum tumor markers and connective tissue disease-related interstitial lung disease (CTD-ILD) and to evaluate the clinical value of tumor markers for investigating interstitial lung disease (ILD) in patients with connective tissue disease (CTD).
Methods: The study included 235 patients with CTD (90 CTD without ILDs, 145 CTD-ILD). Clinical information and the levels of inflammatory and tumor markers, including carbohydrate antigen (CA) 19– 9, CA125, carcinoembryonic antigen (CEA), CA153, and cytokeratin 19 fragments (CYFRA21-1), were obtained in all the patients.
Results: A significant difference between CTD with or without ILD and higher levels of tumor markers was observed in the CTD-ILD group, including CA19-9 (p< 0.001), CEA (p< 0.001), CA153 (p< 0.001), and CYFRA21-1 (p< 0.001). There was no significant difference in serum tumor marker levels in the various types of CTD (rheumatoid arthritis, systemic lupus erythematosus, Sjogren’s syndrome, inflammatory myositis, systemic sclerosis, and mixed connective tissue disease). The levels of CA153 [odds ratio (OR)=1.159] and CYFRA21-1 (OR=2.269) were clearly related to the risk of CTD-ILD. The diagnostic value of CA153 [area under receiver operating characteristic curve (AUC)=0.736] and CYFRA21-1 (AUC=0.718) was confirmed for ILDs in CTD patients, at cut-off values of 9.45 U/mL and 2.13 ng/mL, respectively.
Conclusion: There is a positive correlation between serum tumor marker levels and CTD-ILD. Higher levels of CA153 and CYFRA21-1 suggest an increased risk of developing ILD and may therefore be useful as biomarkers for detecting CTD-ILD in the clinical setting.
Keywords: connective tissue disease, tumor markers, interstitial lung disease
Introduction
Interstitial lung disease (ILD) is a heterogeneous group of diseases that mainly affect the lung interstitium, causing pulmonary restriction and impaired gas exchange.1 ILD is often associated with connective tissue diseases (CTD) including rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), Sjogren’s syndrome (SS), inflammatory myositis (IM), systemic sclerosis (SSc), and mixed connective tissue disease (MCTD). Patients with CTDs-related interstitial lung diseases (CTD-ILD) usually have a decline in their quality of life, a reduced life expectancy, and increased mortality.2–4 It is therefore essential to accurately diagnose ILD, with high-resolution computed tomography (HRCT) currently considered as a well-established standard method for detecting and evaluating early ILDs.5
In recent years, circulating biomarkers have been actively investigated as a supplement to HRCT for evaluating ILDs. These biomarkers include Krebs von den Lungen-6 (KL-6), surfactant protein-A (SP-A), surfactant protein-D (SP-D), CC-chemokine ligand 18 (CCL18), and matrix metalloproteinase 7 (MMP7)6–12 and provide an efficient, rapid, and noninvasive method for investigating CTD-ILD. Measurement of these biomarkers can therefore be used for diagnosis, evaluating the severity of disease, prediction of progression, and monitoring treatment responses.13 In addition, these markers also avoid operator bias when reading lung images obtained by HRCT.
Tumor markers are therefore essential tools for screening and diagnosing various common cancers, including gastric, ovarian, breast, prostate and liver cancers, in addition to a number of other types of tumors.14,15 The value of tumor markers for investigating ILDs has also been supported by the findings of several recent studies, especially for diagnosing and evaluating the risk of developing this condition.16–20
The aims of this retrospective study were to investigate the association between serum tumor marker levels and CTD-ILD and assess the clinical value of these markers for this condition.
Methods
Patients
The participants in this retrospective study were recruited from patients with different types of CTD treated at Xi’an Fifth Hospital between January 2019 and December 2020. The study included 235 patients who had been diagnosed with RA (n = 151), SS (n = 30), SLE (n = 26), IM (n = 11), or another CTD (n = 17), including SSc (n = 7) and MCTD (n = 10). Clinical information including age, gender, and pulmonary symptoms was collected. Exclusion criteria in the study were overlapping syndromes or multiple autoimmune diseases, malignant disease, sarcoidosis, amyloidosis, severe infection, severe liver and kidney dysfunction, or a history of malignancy. This study was performed in compliance with the Declaration of Helsinki and was approved by the Institutional Review Board of Xi’an Fifth Hospital (IRB#:2021–04).
Clinical Evaluation of ILD
Chest HRCT scans were performed in all patients in the study. One trained radiologist examined the HRCTs and was blinded to the original diagnosis, clinical history, and follow-up information. The HRCT scans were reconstructed using a high spatial frequency algorithm with a collimation of 1.25 mm, interspace of 1.2 mm and digitalized at window settings appropriate for viewing the lung parenchyma (window center, −600 HU; window width, 1500 HU).
Collection of Laboratory Data
All patients underwent biochemical assessment and measurement of serum tumor marker levels, including carbohydrate antigen (CA) 19–9, CA125, carcinoembryonic antigen (CEA), CA153, and cytokeratin 19 fragments (CYFRA21-1). The normal values of these tumor markers were set at; CA19-9 <25 U/mL, CA125 <23 U/mL, CEA <5.00 ng/mL, CA153 <15 U/mL, and CYFRA21-1 <3.3 ng/mL.
In addition to the tumor markers, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) were evaluated as inflammatory markers.
Statistical Analysis
According to the distribution of the data, the results of continuous variables were expressed as either mean ± standard deviation (SD) or median and range. Categorical data were expressed as numbers with percentages (%). Differences in clinical characteristics between patients with or without ILD were evaluated using the chi-square, Mann–Whitney U, and t-test, while the Kruskal Wallis test was used to compare the tumor markers levels in the different types of CTD groups. The strength of the association between tumor markers levels and other variables was analyzed using the Spearman correlation coefficient, followed by construction of a logistic regression model using the probabilities of the tumor markers as the independent variable and ILDs as the dependent variables. Receiver operating characteristic (ROC) curve analysis was performed to analyze the discriminatory power of the different tumor markers. We then evaluated the performance of the model based on the 95% confidence intervals (CI) for specificity, sensitivity, cut-off value, and area under the receiver operating characteristic curve (AUC). R version 4.0.3 software was used for the statistical analyses. p values <0.05 were considered statistically significant.
Results
Clinical Characteristics of the Patients
The mean age of the 145 patients with CTD-ILD was 58.52 (11.88) years and that of the 90 patients with CTD without ILD was 56.17 (15.16) years (p=0.213). Both of these groups contained a greater but statistically insignificant proportion of females (67.6% vs 72.2%, respectively, p=0.546). The frequency of the different types of CTDs are shown in Table 1 (p=0.082). Notably, all 11 IM patients in the study had ILD. There was no difference in mean ESR (p=0.776) and CRP level (p=0.591) between the CTD-ILD and CTD without ILD groups (Table 1).
 |
Table 1 Demographic and Clinical Characteristics of Study Participants |
Levels of Tumor Markers
The results showed that the levels of tumor markers in the CTD-ILD group were significantly higher than that observed in the CTD without ILD group, including CA19-9 (p<0.001), CEA (p<0.001), CA153 (p<0.001), and CYFRA21-1 (p<0.001). However, there was no obvious difference in the level of CA125 (p=0.146) (Table 2 and Figure 1).
 |
Table 2 Comparison of Tumor Markers Levels Among Two Groups |
 |
Figure 1 Levels of tumor markers in patients with CTDs with or without ILDs, including CA19-9 (A), CA125 (B), CEA (C), CA153 (D), and CYFRA21-1 (E). |
When the CTD-ILD group was stratified by the type of CTD, no significant difference was observed in the specific CTD subgroups of CA19-9 (p=0.080), CA125 (p=0.346), CEA (p=0.142), CA153 (p=0.686) and CYFRA21-1 (p=0.938) (Table 3).
 |
Table 3 Tumor Markers According to the Presence of ILDs in Each CTDs |
These results suggest that the level of these markers was independent of the level of inflammatory markers (Table 4).
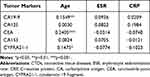 |
Table 4 Spearman Correlation Coefficient Values of Tumor Markers and Disease Characteristics of CTDs |
Clinical Values of the Tumor Markers
We observed a significant association of CTD-ILD with CA153 [OR=1.159, 95% CI= (1.064, 1.276)] and CYFRA21-1 [OR=2.269, 95% CI= (1.482, 3.619)]. As shown in Table 5, higher levels of CA153 and CYFRA21-1 correlated strongly with the risk of CTD-ILD.
 |
Table 5 Logistic Regression Analysis of the Association of Tumor Markers and CTD-ILD |
ROC assessment was used to determine the diagnostic value of the tumor markers and indicated that the diagnostic potential of CA153 [AUC=0.736, 95% CI (0.672, 0.801)] and CYFRA21-1 [AUC=0.718, 95% CI (0.649, 0.786)] was superior to that of the other tumor markers. To detect the presence of CTD-ILD, a CA153 level of 9.45 U/mL had a sensitivity of 58.6% and specificity of 86.7%, while a CYFRA21-1 level of 2.13 ng/mL had a sensitivity of 60.7% and specificity of 85.6%) (Table 6 and Figure 2).
 |
Table 6 AUC, Cut-Off Value, and Sensitivity and Specificity of Tumor Markers Level for Diagnosis of ILDs Using a ROC Curve |
Discussion
This retrospective study investigated the possible association between the levels of tumor markers and interstitial lung disease in patients with CTD and showed that, as expected, these levels were higher in patients with CTD-ILD than those without ILD. These findings are consistent with those reported by previous studies. For example, Dai et al observed elevated levels of CEA and CA125 in ILD patients without cancer,21 while Dobashi et al found the levels of CYFRA21-1 in both serum and bronchoalveolar lavage fluid (BALF) were increased in these patients.22 Zheng et al reported that the serum levels of CA19-9, CA125 and CEA were also elevated in RA-ILD and showed a strong association with the severity of the disorder.16 Similarly, Shi et al showed that SS-ILD patients had elevated serum levels of tumor markers, including NSE, CEA, CA125, and CA153,18 while Wong et al reported that IM-ILD patients without cancer had elevated levels of CA153.19 Sargin et al considered that RA patients with an increase in tumor markers especially CA153 and CA125 should be suspected of having an ILD.23 CYFRA21-1, as shown by Gui et al, has potential as a useful serum indicator for the presence of IM-ILD, while Wang et al suggested CA19-9 and CA125 had value for diagnosing RA-ILD.24 However, to date no study has investigated differences in the level of these markers in a variety of CTDs.
Tumor markers can be used as both risk factors and diagnostic indicators for CTD-ILD. Based on the results of the current study we suggest that increased levels of CA153 and CYFRA21-1 are associated with a higher risk of ILD and that both markers also have potential diagnostic value for CTD-ILD. Moreover, our study is the first to point out that levels of CA153 >9.45 U/mL and CYFRA21-1 >2.13 ng/mL indicate the presence of ILD. However, the level of tumor markers may be affected by several confounding factors, such as cancer and ethnic variability14 and therefore further prospective and longitudinal studies are needed to determine the CA153 and CYFRA21-1 levels that more accurately screen and diagnose CTD-ILD.
Tumor markers are synthesized and secreted by tumor cells and other cells in tumor tissue and are classified into different categories according to their source of production and their biology. Mucin glycoproteins carrying specific glycan structures such as MUC1 (CA15-3), MUC16 (CA125), and Lewis antigens (CA19-9) that can be detected in different types of cancer15 and are therefore often used for diagnosing, monitoring, and predicting the presence of cancer. In addition, mucin glycoproteins can be detected in the serum of patients with ILDs. One of these proteins, KL-6 known as human mucin-1 (MUC1) has been shown to have high sensitivity and accuracy for diagnosing ILDs and appears to be a good biomarker that reflects disease severity.6,7 Another marker YKL-40, a chitinase-3-like 1 glycoprotein, is present in patients with multiple myeloma and cholangiocarcinoma25,26 and as suggested by some studies, higher levels of this marker are associated with a worse prognosis in patients with ILDs.27 Both these markers are secreted by damaged epithelial cells and because repeated chronic epithelial or vascular injuries lead to alveolar epithelial cell destruction and unregulated repair in ILDs these damaged cells secrete several cytokines and proteins.28 Therefore, over expression of glycoproteins suggests that ILDs and cancers might be triggered by the same signaling pathways.
CYFRA21-1 is expressed in respiratory bronchiolar and alveolar epithelial cells and is therefore useful for diagnosing and monitoring lung carcinoma, especially squamous cell carcinoma.29 Previous studies have also suggested that CYFRA21-1 could be a possible marker of epithelial cell damage in ILDs.22,30 However, the mechanism for the increase in CYFRA21-1 remains unclear. Some studies have suggested it may be a consequence of injury due to proteinases and oxidants produced by both eosinophils and neutrophils.30 Further research on this possibility is therefore warranted.
There were several limitations in our study. First, no further prognostic information of the patients was collected because of the retrospective observational design of the study. We were therefore unable to follow-up the occurrence of cancer in the preceding years and accordingly longitudinal and prospective cohort studies are required. Second, although we found that the levels of tumor markers were not significantly different in the various types of CTDs, this may have been a consequence of the relatively small number of other CTDs compared to that of RA. Third, there was a paucity of pulmonary function test data for all patients and HRCT scores for patients with ILD. These data would be valuable for evaluating the severity of ILDs. Finally, comparison with other candidate biomarkers for CTD-ILD, such as KL-6 is lacking. A prospective study involving measurement of the level of tumor markers and other circulating biomarkers, pulmonary function tests, and chest HRCT scoring would supplement future investigations in this area.
Conclusion
There is a positive correlation between the levels of serum tumor markers and CTD-ILD. Higher levels of CA153 and CYFRA21-1 suggest an increased risk of developing ILD and may be useful biomarkers for detection of CTD-ILD in the clinical setting.
Ethics Approval and Consent to Participate
The present study was approved by the Ethics Committee of Xi’an Fifth Hospital. The study was carried out in accordance with the principles stated in the Declaration of Helsinki (IRB#:2021-04). All patients provided written, informed consent to participate in the study, including consent for publication of the study.
Acknowledgments
The authors would like to express their gratitude to EditSprings (https://www.editsprings.com/) for the expert linguistic services provided.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
All authors declare no conflicts of interest.
References
1. Fischer A, Du Bois R. Interstitial lung disease in connective tissue disorders. Lancet. 2012;380(9842):689–698. doi:10.1016/S0140-6736(12)61079-4
2. Bongartz T, Nannini C, Medina-Velasquez YF, et al. Incidence and mortality of interstitial lung disease in rheumatoid arthritis: a population-based study. Arthritis Rheum. 2010;62(6):1583–1591. doi:10.1002/art.27405
3. Atzeni F, Gerardi MC, Barilaro G, Masala IF, Benucci M, Sarzi-Puttini P. Interstitial lung disease in systemic autoimmune rheumatic diseases: a comprehensive review. Expert Rev Clin Immunol. 2018;14(1):69–82. doi:10.1080/1744666X.2018.1411190
4. Schnabel A, Hellmich B, Gross WL. Interstitial lung disease in polymyositis and dermatomyositis. Curr Rheumatol Rep. 2005;7(2):99–105. doi:10.1007/s11926-005-0061-4
5. Mathai SC, Danoff SK. Management of interstitial lung disease associated with connective tissue disease. BMJ. 2016;352:h6819. doi:10.1136/bmj.h6819
6. Oguz EO, Kucuksahin O, Turgay M, et al. Association of serum KL-6 levels with interstitial lung disease in patients with connective tissue disease: a cross-sectional study. Clin Rheumatol. 2016;35(3):663–666. doi:10.1007/s10067-015-3167-8
7. Lee JS, Lee EY, Ha Y-J, Kang EH, Lee YJ, Song YW. Serum KL-6 levels reflect the severity of interstitial lung disease associated with connective tissue disease. Arthritis Res Ther. 2019;21(1):58. doi:10.1186/s13075-019-1835-9
8. Ohnishi H, Yokoyama A, Kondo K, et al. Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. Am J Respir Crit Care Med. 2002;165(3):378–381. doi:10.1164/ajrccm.165.3.2107134
9. Yanaba K, Hasegawa M, Takehara K, Sato S. Comparative study of serum surfactant protein-D and KL-6 concentrations in patients with systemic sclerosis as markers for monitoring the activity of pulmonary fibrosis. J Rheumatol. 2004;31(6):1112–1120.
10. Hant FN, Ludwicka-Bradley A, Wang H-J, et al. Surfactant protein D and KL-6 as serum biomarkers of interstitial lung disease in patients with scleroderma. J Rheumatol. 2009;36(4):773–780. doi:10.3899/jrheum.080633
11. Hoffmann-Vold A-M, Tennøe AH, Garen T, et al. High level of chemokine CCL18 is associated with pulmonary function deterioration, lung fibrosis progression, and reduced survival in systemic sclerosis. Chest. 2016;150(2):299–306. doi:10.1016/j.chest.2016.03.004
12. Doyle TJ, Patel AS, Hatabu H, et al. Detection of rheumatoid arthritis-interstitial lung disease is enhanced by serum biomarkers. Am J Respir Crit Care Med. 2015;191(12):1403–1412. doi:10.1164/rccm.201411-1950OC
13. Elhai M, Avouac J, Allanore Y. Circulating lung biomarkers in idiopathic lung fibrosis and interstitial lung diseases associated with connective tissue diseases: where do we stand? Semin Arthritis Rheum. 2020;50(3):480–491. doi:10.1016/j.semarthrit.2020.01.006
14. Duffy MJ, O’Byrne K. Tissue and blood biomarkers in lung cancer: a review. Adv Clin Chem. 2018;86:1–21. doi:10.1016/bs.acc.2018.05.001
15. Silsirivanit A. Glycosylation markers in cancer. Adv Clin Chem. 2019;89:189–213. doi:10.1016/bs.acc.2018.12.005
16. Zheng M, Lou A, Zhang H, Zhu S, Yang M, Lai W. Serum KL-6, CA19-9, CA125 and CEA are diagnostic biomarkers for rheumatoid arthritis-associated interstitial lung disease in the Chinese population. Rheumatol Ther. 2021;8(1):517–527. doi:10.1007/s40744-021-00288-x
17. Wang T, Zheng X-J, Ji Y-L, Liang Z-A, Liang B-M. Tumour markers in rheumatoid arthritis-associated interstitial lung disease. Clin Exp Rheumatol. 2016;34(4):587–591.
18. Shi L, Han X-L, Guo H-X, et al. Increases in tumor markers are associated with primary sjögren’s syndrome-associated interstitial lung disease. Ther Adv Chronic Dis. 2020;11:2040622320944802. doi:10.1177/2040622320944802
19. Wong RCW, Klingberg S, Wilson R. CA15-3 and cancer associated serum antigen assays are alternatives to the KL-6 assay for measuring serum MUC-1 levels in patients with interstitial lung disease associated with polymyositis/dermatomyositis. J Rheumatol. 2002;29(9):
20. Celeste S, Santaniello A, Caronni M, et al. Carbohydrate antigen 15.3 as a serum biomarker of interstitial lung disease in systemic sclerosis patients. Eur J Intern Med. 2013;24(7):671–676. doi:10.1016/j.ejim.2013.04.004
21. Dai H, Liu J, Liang L, et al. Increased lung cancer risk in patients with interstitial lung disease and elevated CEA and CA125 serum tumour markers. Respirology. 2014;19(5):707–713. doi:10.1111/resp.12317
22. Dobashi N, Fujita J, Ohtsuki Y, et al. Elevated serum and BAL cytokeratin 19 fragment in pulmonary fibrosis and acute interstitial pneumonia. Eur Respir J. 1999;14(3):574–578. doi:10.1034/j.1399-3003.1999.14c15.x
23. Sargin G, Köse R, Şentürk T. Tumor-associated antigens in rheumatoid arthritis interstitial lung disease or malignancy? Arch Rheumatol. 2018;33(4):431–437. doi:10.5606/ArchRheumatol.2018.6691
24. Gui X, Ma M, Ding J, et al. Cytokeratin 19 fragment is associated with severity and poor prognosis of interstitial lung disease in anti-MDA5 antibody-positive dermatomyositis. Rheumatology. 2021. doi:10.1093/rheumatology/keaa843
25. Mylin AK, Abildgaard N, Johansen JS, et al. Serum YKL-40: a new independent prognostic marker for skeletal complications in patients with multiple myeloma. Leuk Lymphoma. 2015;56(9):2650–2659. doi:10.3109/10428194.2015.1004168
26. Thongsom S, Chaocharoen W, Silsirivanit A, et al. YKL-40/chitinase-3-like protein 1 is associated with poor prognosis and promotes cell growth and migration of cholangiocarcinoma. Tumour Biol. 2016;37(7):9451–9463. doi:10.1007/s13277-016-4838-z
27. Korthagen NM, van Moorsel CHM, Zanen P, Ruven HJ, Grutters JC. Evaluation of circulating YKL-40 levels in idiopathic interstitial pneumonias. Lung. 2014;192(6):975–980. doi:10.1007/s00408-014-9647-9
28. Spagnolo P, Distler O, Ryerson CJ, et al. Mechanisms of progressive fibrosis in connective tissue disease (CTD)-associated interstitial lung diseases (ILDs). Ann Rheum Dis. 2021;80(2):143–150. doi:10.1136/annrheumdis-2020-217230
29. Kanazawa H, Yoshikawa T, Yamada M, et al. CYFRA 21-1, a cytokeratin subunit 19 fragment, in bronchoalveolar lavage fluid from patients with interstitial lung disease. Clin Sci. 1998;94(5):531–535. doi:10.1042/cs0940531
30. Vercauteren IM, Verleden SE, McDonough JE, et al. CYFRA 21.1 in bronchoalveolar lavage of idiopathic pulmonary fibrosis patients. Exp Lung Res. 2015;41(8):459–465. doi:10.3109/01902148.2015.1073407
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

