Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Correlation between pain response and improvements in patient-reported outcomes and health-related quality of life in duloxetine-treated patients with diabetic peripheral neuropathic pain
Authors Ogawa K, Fujikoshi S, Montgomery W, Alev L
Received 30 April 2015
Accepted for publication 9 July 2015
Published 18 August 2015 Volume 2015:11 Pages 2101—2107
DOI https://doi.org/10.2147/NDT.S87665
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Wai Kwong Tang
Kei Ogawa,1 Shinji Fujikoshi,2 William Montgomery,3 Levent Alev1
1Medical Science, 2Statistical Science, Eli Lilly Japan K.K., Kobe, Japan; 3Global Patient Outcomes and Real World Evidence, Eli Lilly Australia Pty Ltd, West Ryde, NSW, Australia
Objective: We assessed whether quality of life (QoL) improvement in duloxetine-treated patients with diabetic peripheral neuropathic pain (DPNP) correlates with the extent of pain relief.
Methods: Pooled data from three multicountry, double-blind, 12-week, placebo-controlled trials of duloxetine-treated (duloxetine 60 mg once daily; total number =335) patients with DPNP were analyzed. Based on improvement in 24-hour average pain scores, patients were stratified into four groups. Improvement in QoL, which was measured as the change from baseline in two patient-reported health outcome measures (Short Form [SF]-36 and five-dimension version of the EuroQol Questionnaire [EQ-5D]), was evaluated and compared among the four groups. Pearson’s correlation coefficient was calculated to assess the correlation between improvement in pain scores and improvement in QoL.
Results: The group with more pain improvement generally showed greater mean change from baseline in all of the SF-36 scale scores and on the EQ-5D index. Pearson’s correlation coefficients ranged from 0.114 to 0.401 for the SF-36 scale scores (P<0.05), and it was 0.271 for the EQ-5D (P<0.001).
Conclusion: Improvement in pain scores was positively correlated with improvement in QoL and patient-reported outcomes in duloxetine-treated patients.
Keywords: diabetic peripheral neuropathic pain, duloxetine, efficacy, function, quality of life
Introduction
Pain symptoms associated with diabetic peripheral neuropathic pain (DPNP) have a negative effect on functioning and quality of life (QoL).1 Furthermore, DPNP is often unreported,2 and although the prevalence of DPNP is high, almost one-quarter of patients with DPNP do not receive any treatment for pain symptoms.3 Important goals in the treatment of DPNP are to not only reduce pain, but also to improve overall patient functional outcomes and QoL.
Duloxetine is a serotonin and norepinephrine reuptake inhibitor that was approved in Japan for the management of DPNP in 2012. The pain inhibitory action of duloxetine is believed to result from potentiation of descending inhibitory pain pathways within the central nervous system.4 Duloxetine has demonstrated efficacy and has been associated with improvement in QoL and functionality in patients with DPNP in three placebo-controlled studies.5–8
There are limited data on the correlation between the degree of pain response and the improvement in patient QoL for duloxetine-treated patients with DPNP. The purpose of these analyses is to assess whether improvements in QoL and patient-reported outcomes (PRO) in duloxetine-treated patients with DPNP correlate with the extent of pain relief.
Methods
Study designs and patients
The data used in this analysis were derived from studies that were reviewed and approved by the applicable organizational ethical review boards and were conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and are consistent with the International Conference on Harmonization good clinical practice guidelines. Pooled data from three randomized, double-blind, placebo-controlled, multicountry studies of duloxetine for the management of DPNP were analyzed. Patients received either duloxetine or placebo: study 1 (total number [N]=457 [duloxetine, number [n]=342; placebo, n=115]),5 study 2 (N=334 [duloxetine, n=226; placebo, n=108]),6 and study 3 (N=348 [duloxetine, n=232; placebo, n=116]).7 The treatment period for all three trials was 12 weeks; studies 2 and 3 included 1 week for drug tapering after the treatment period. Since the approved dose of duloxetine in Japan for the management of DPNP is 60 mg once daily, only patients randomized to placebo (N=330) and duloxetine 60 mg once daily (N=335) were included in the current analyses.
Patients in the three studies were aged 18 years and older and they presented with pain for at least 6 months’ duration, which was due to bilateral peripheral neuropathy caused by type 1 or type 2 diabetes mellitus. Pain had to start in the feet and it should have had a relatively symmetrical onset. Diagnosis was confirmed by a score ≥3 on the Michigan Neuropathy Screening Instrument. Patients also had to have a score ≥4 of average pain severity for 24 hours on an 11-point Likert scale, and they had to have stable glycemic control.
Measures
For pain, 24-hour average pain severity scores were daily recorded by the patient in a diary using an 11-point Likert scale (0 [no pain] to 10 [worst possible pain]). The weekly mean of these scores was used for the analysis.
PRO were evaluated using the Short Form (SF)-36 version 1.0,9 the three-level, five-dimension version of the EuroQol Questionnaire (EQ-5D),10 and the Patient Global Impression of Improvement (PGI-I) for the patient-rated global assessment of response to treatment.11
Assessments
To assess the efficacy of duloxetine compared with placebo to reduce pain severity in patients with DPNP, the 24-hour average pain severity scores were used. Patients were stratified into four groups (ie, ≥50%, ≥30%–<50%, ≥15%–<30%, and <15% improvement) based on the degree of pain improvement in 24-hour average pain scores. Stratification was conducted based on the percentage change at 12 weeks from baseline. Improvement in QoL and PRO measures was assessed as the change from baseline to 12 weeks on the PRO measures of the SF-36 scale scores, the EQ-5D index, and the PGI-I compared with placebo-treated patients. The correlation between the percentage improvement in 24-hour average pain scores and improvement in QoL and PRO measures was also assessed for the duloxetine group.
Statistical analysis
Post hoc analyses were conducted. Missing data were inputed according to the last observation carried forward methodology. Treatment comparison in the model was assessed using Fisher’s exact test or analysis of covariance for treatment, investigator, and baseline. In the duloxetine group, Pearson’s correlation coefficient was calculated for the correlation between the percentage improvements in 24-hour average pain scores and improvements in each QoL and PRO measure. A two-sided 5% significance level was used, and no adjustments were made for multiplicity.
Results
Demographics and baseline characteristics
Patient demographics and disease characteristics were similar between the duloxetine and placebo groups (Table 1).
  | Table 1 Patient demographics and disease characteristics at baseline |
Efficacy of duloxetine for DPNP
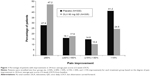
The distribution of patients into the four groups, based on the degree of improvement in their 24-hour average pain score, is shown in Figure 1. Significantly, more patients treated with duloxetine compared with placebo achieved ≥50% improvement (47.2% versus 27.9%, respectively; odds ratio [OR]: 2.31), ≥30% improvement (65.1% versus 43.9%, respectively; OR: 2.38), and ≥15% improvement (75.5% versus 58.8%, respectively; OR: 2.16) in 24-hour average pain scores (P<0.001 for all groups).
QoL and PRO measures
There were significant differences between the duloxetine and placebo groups for all SF-36 scale scores, the EQ-5D, and the PGI-I (all P<0.05) (Table 2).
Relationship between QoL, PRO measures, and pain improvement
Baseline data were similar among the duloxetine-treated patients in the four pain improvement categorized groups for all of the SF-36 scale scores and the EQ-5D. For the SF-36 scale scores (Figure 2) and the EQ-5D (Figure 3), a group with more pain improvement generally showed a greater mean change from baseline. The ≥50% improvement group demonstrated the greatest change from baseline (improvement) among the four groups. For the PGI-I, a group with more pain improvement generally demonstrated a lower (better) mean score among the four groups (Figure 4).
Pearson’s correlation coefficients ranged from 0.114 to 0.401 for the SF-36 scale scores (P<0.05) (Figure 2); the correlation coefficient was 0.271 for the EQ-5D (P<0.001) (Figure 3) and −0.565 for the PGI-I (P<0.001) (Figure 4).
Discussion
Studies have reported that DPNP is associated with poor QoL outcomes.1 Duloxetine is effective in reducing pain and has been associated with significant improvement in health outcome measures in the management of DPNP.5–8 In the current study, patients treated with duloxetine had superior improvement in pain and all QoL and PRO measures examined compared with placebo-treated patients. As in other duloxetine trials for chronic pain treatment,12 a consistent relationship was seen between an average of 0 and 10 numeric rating scale scores for pain intensity and PGI-I.
However, the correlation between the degree of pain response and the improvement in patient QoL in duloxetine-treated patients with DPNP has not been investigated in detail. In the current analyses, the group with more pain improvement generally showed greater mean change from baseline (improvement) for all QoL and PRO measures. The correlation between pain relief and QoL improvement was strong, particularly in the SF-36 subscale scores of bodily pain (correlation coefficient, r=0.401) and vitality (r=0.324), and in the PGI-I (r=−0.565).
Regarding the SF-36 scale scores, in the ≥50% improvement group, the physical component summary score numerically improved more than the mental component summary score, and the greatest change from baseline (improvement) was seen in the bodily pain and role–physical subscale scores. Similar results were also seen for the EQ-5D and the PGI-I, where the greatest improvement was seen in the ≥50% improvement group. Overall, patients achieving ≥50% pain improvement at the end of the study reported some SF-36 scale scores that were comparable with the general US population: vitality, mean baseline: 47.1, mean endpoint: 60.6, US norm: 60.9; social functioning, mean baseline: 72.3, mean endpoint: 84.5, US norm: 83.3; role–emotional, mean baseline: 70.4, mean endpoint: 84.3, US norm: 81.3; mental health, mean baseline: 71.4, mean endpoint: 79.7, US norm: 74.7; and general health: mean baseline: 49.2, mean endpoint: 58.1, US norm: 72.0.13 Similar results were seen in a study of pregabalin, which also reported that improvement in functional outcomes and QoL correlated with the amount of pain relief (mental health was not described in the discussion).14
The 0.19 change seen in the EQ-5D associated with duloxetine treatment represents a considerable improvement that is well in excess of the minimally important difference reported for this instrument (0.074).15 The EQ-5D endpoint score of 0.78 in the ≥50% improvement group is higher than that of a previous report of patients with diabetes having an EQ-5D score of 0.668.16
Higher levels of pain correspond with decreases in physical and mental functioning,17 and patients with diabetes score poorly on QoL measures.18 This current study shows that among duloxetine-treated patients, the greatest improvement was seen in the group with ≥50% improvement in the SF-36 scale scores, the EQ-5D, and the PGI-I. For the SF-36 scale scores, the greatest change from baseline was seen in the bodily pain and role–physical scale scores, both of which are subscales within the physical component summary of the SF-36 model. In this 12-week study, improvement in QoL and PRO in duloxetine-treated patients with DPNP was correlated with the extent of pain relief.
Limitations
Some limitations to these analyses need to be considered when interpreting the findings. This was a post hoc analysis. The results are based on an acute treatment duration of 12 weeks and may not be generalizable to longer periods of treatment. In addition, the generalizability of the results to all patients with DPNP may be affected by the inclusion and exclusion criteria of the individual trials. Finally, the SF-36 and EQ-5D are general health-related QoL instruments that are not specific for DPNP.
Conclusion
In the current results, significantly more patients treated with duloxetine compared with placebo achieved improvement in 24-hour average pain scores. Patients with the greatest improvement in pain scores had the greatest improvement in functionality, QoL, and PRO.
Acknowledgments
Ms Aki Yoshikawa, a full-time employee of Eli Lilly Japan K.K., provided writing, editorial, and logistical support. Medical writing assistance was provided by Dr Deborah D’Souza, a full-time employee of Ventiv Health Clinical, LLC. Eli Lilly Japan K.K. contracted inVentiv Health Clinical for writing and editorial support.
Author contributions
All authors participated in the drafting, critical revision, and approval of the final version of the manuscript. SF conducted the data analysis, and all authors were involved in the interpretation of the data. All authors critically revised the manuscript for important intellectual content and approved the final version.
Disclosure
This manuscript was sponsored by Eli Lilly Japan K.K. KO, SF, and LA are employees of Eli Lilly Japan K.K. WM is an employee of Eli Lilly Australia Pty Ltd. SF and LA are minor stockholders of Eli Lilly and Company. The authors report no other conflicts of interest in this work.
References
Davies M, Brophy S, Williams R, Taylor A. The prevalence, severity, and impact of painful diabetic peripheral neuropathy in type 2 diabetes. Diabetes Care. 2006;29(7):1518–1522. | ||
Daousi C, MacFarlane IA, Woodward A, Nurmikko TJ, Bundred PE, Benbow SJ. Chronic painful peripheral neuropathy in an urban community: a controlled comparison of people with and without diabetes. Diabet Med. 2004;21(9):976–982. | ||
Berger A, Dukes EM, Oster G. Clinical characteristics and economic costs of patients with painful neuropathic disorders. J Pain. 2004;5(3):143–149. | ||
Perahia DG, Pritchett YL, Desaiah D, Raskin J. Efficacy of duloxetine in painful symptoms: an analgesic or antidepressant effect? Int Clin Psychopharmacol. 2006;21(6):311–317. | ||
Goldstein DJ, Lu Y, Detke MJ, Lee TC, Iyengar S. Duloxetine vs placebo in patients with painful diabetic neuropathy. Pain. 2005;116(1–2):109–118. | ||
Wernicke JF, Pritchett YL, D’Souza DN, et al. A randomized controlled trial of duloxetine in diabetic peripheral neuropathic pain. Neurology. 2006;67(8):1411–1420. | ||
Raskin J, Pritchett YL, Wang F, et al. A double-blind, randomized multicenter trial comparing duloxetine with placebo in the management of diabetic peripheral neuropathic pain. Pain Med. 2005;6(5):346–356. | ||
Armstrong DG, Chappell AS, Le TK, et al. Duloxetine for the management of diabetic peripheral neuropathic pain: evaluation of functional outcomes. Pain Med. 2007;8(5):410–418. | ||
Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston, MA: New England Medical Center, the Health Institute; 1993. | ||
EuroQol Research Foundation [homepage on the Internet]. EQ-5D. Rotterdam, the Netherlands: EuroQol Research Foundation; 2015. Available from: http://www.euroqol.org/. Accessed June 10, 2015. | ||
Guy W. ECDEU Assessment Manual for Psychopharmacology – Revised. Rockville, MD: US Department of Health, Education and Welfare, ADAMHA, MIMH Psychopharmacology Research Branch; 1976. | ||
Farrar JT, Pritchett YL, Robinson M, Prakash A, Chappell A. The clinical importance of changes in the 0 to 10 numeric rating scale for worst, least, and average pain intensity: analyses of data from clinical trials of duloxetine in pain disorders. J Pain. 2010;11(2):109–118. | ||
Hoffman DL, Dukes EM. The health status burden of people with fibromyalgia: a review of studies that assessed health status with the SF-36 or the SF-12. Int J Clin Pract. 2008;62(1):115–126. | ||
Vinik A, Emir B, Cheung R, Whalen E. Relationship between pain relief and improvements in patient function/quality of life in patients with painful diabetic peripheral neuropathy or postherpetic neuralgia treated with pregabalin. Clin Ther. 2013;35(5):612–623. | ||
Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14(6):1523–1532. | ||
Saarni SI, Härkänen T, Sintonen H, et al. The impact of 29 chronic conditions on health-related quality of life: a general population survey in Finland using 15D and EQ-5D. Qual Life Res. 2006;15(8):1403–1414. | ||
Gore M, Brandenburg NA, Dukes E, Hoffman DL, Tai KS, Stacey B. Pain severity in diabetic peripheral neuropathy is associated with patient functioning, symptom levels of anxiety and depression, and sleep. J Pain Symptom Manage. 2005;30(4):374–385. | ||
Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989;262(7):907–913. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.