Back to Journals » Clinical Interventions in Aging » Volume 18
Correlation Between MMP9 Promoter Methylation and Transient Ischemic Attack/Mild Ischemic Stroke with Early Cognitive Impairment
Authors Miao M , Lyu M, Zhong C , Liu Y
Received 18 May 2023
Accepted for publication 22 July 2023
Published 1 August 2023 Volume 2023:18 Pages 1221—1232
DOI https://doi.org/10.2147/CIA.S421830
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Meng Miao,1 Mingyang Lyu,2 Chi Zhong,1 Ying Liu3
1Department of Neurology, Qilu Hospital (Qingdao), Cheeloo College of Medicine, Shandong University, Qingdao, Shandong, People’s Republic of China; 2Haihe Laboratory of Cell Ecosystem, Tianjin, People’s Republic of China; 3Department of Neurology, Qilu Hospital of Shandong University, Jinan, Shandong, People’s Republic of China
Correspondence: Ying Liu, Department of Neurology, Qilu Hospital of Shandong University, Jinan, Shandong, 250012, People’s Republic of China, Tel +8618005316460, Email [email protected] Chi Zhong, Department of Neurology, Qilu Hospital (Qingdao), Cheeloo College of Medicine, Shandong University, 758 Hefei Road, Qingdao, Shandong, 266035, People’s Republic of China, Tel +8618561817360, Email [email protected]
Background/Objective: Dyskinesia caused by transient ischemic attack (TIA) and mild ischemic stroke (MIS) is mild and short-lived; however, cognitive impairment (CI) can occur in the acute phase and be easily overlooked. DNA methylation is an epigenetic phenomenon that can affect gene expression through gene silencing. Blood levels of matrix metalloproteinase (MMP) 9 are elevated in ischemic stroke patients and is associated with the destruction of the blood-brain barrier and the occurrence of CI. No studies have investigated the relationship between MMP9 gene methylation and TIA/MIS with early cognitive impairment (ECI). As such, the purpose of the present study was to investigate the correlation between MMP9 gene methylation and TIA/MIS with ECI.
Methods: Data from 112 subjects were collected, including 84 with TIA/MIS (National Institutes of Health Stroke Scale < 5 points) and 28 non-stroke control subjects. Patients were evaluated within 7 days of TIA/MIS onset according to four single-domain cognitive scales. Whole blood DNA methylation was detected using MethylTarget sequencing technology. Comparison of MMP9 gene methylation levels among subgroups was performed using statistical methods.
Results: The site S33-79 in the TIA/MIS group was hypomethylated compared with the control group, and sites S33-25 and S33-30 in TIA/MIS with ECI was hypomethylated compared with TIA/MIS without ECI. Compared with the small artery occlusion group, MMP9 gene, S33-25, 30, 39, 53, 58, 73, 79, 113 and 131 sites in the large artery atherosclerosis group were hypomethylated.
Conclusion: MMP9 gene hypomethylation sites were associated with TIA/MIS and TIA/MIS with ECI, and there was a strong correlation between MMP9 gene hypomethylation and atherosclerotic TIA/MIS. MMP9 gene methylation can reflect the severity of TIA/MIS. MMP9 gene hypomethylation sites may be used as potential biomarkers and therapeutic targets for TIA/MIS and TIA/MIS with ECI.
Keywords: early cognitive impairment, hypomethylation, amyloid β-protein, blood-brain barrier, MMP9 gene
Introduction
China has a high incidence of ischemic stroke. Although the dyskinetic symptoms of transient ischemic attack/minor ischemic stroke (TIA/MIS) can recover quickly, cognitive impairment (CI) in the early stages can be easily ignored. Early cognitive impairment (ECI) is highly correlated with a persistent decline in cognitive function.1–4 As an epigenetic form, methylation can affect gene expression without altering the gene sequence, and abnormal methylation of multiple genes has been found.5–10 The blood-brain barrier (BBB) is a highly selective membrane structure composed of endothelial cells, tight connections, basement membranes, and astrocytes. It can separate blood from the brain tissue of the central nervous system, selectively pass through water, gas, and liposoluble substances, block macromolecular substances and toxic substances from entering the brain,11 and maintain the stability of the central nervous system.12 Ischemic stroke can destroy the blood-brain barrier, the degree of which is related to the severity and prognosis of the stroke.13 After an ischemic stroke, brain edema appears rapidly. It leads to transport dysfunction, and the infiltration of inflammatory cells and the entry of inflammatory molecules lead to secondary inflammatory reactions, which can further aggravate the damage of the blood-brain barrier and brain injury.14
Damage to cognitive function caused by the destruction of the blood-brain barrier is likely related to amyloid β-protein (Aβ) transportation.15 Under normal circumstances, a large part of the outward transportation of Aβ is through the blood-brain barrier.16,17 After an ischemic stroke, the blood-brain barrier is damaged, and the deposition of Aβ in the brain tissue and blood vessel walls is increased because of the abnormal Aβ transportation. At the same time, inflammation and oxidative stress reactions are secondary after stroke and can cause cognitive function damage under joint action.15 Matrix metalloproteinases (MMP) is a large protease family and a kind of metallo-zinc-dependent protease family, which plays an important role in maintaining the stability of the blood-brain barrier. MMP mainly hydrolyzes tight junctions and matrix membranes, causing damage to the blood-brain barrier and affecting brain function.
MMP9 is a gelatinase. Research has shown that MMP9 increases in the acute stage of ischemic cerebrovascular disease and participates in blood-brain barrier destruction. The increased serum MMP9 level is related to an adverse prognosis after ischemic stroke.18,19 MMP9 inhibitors can reduce the volume of infarcted lesions and the symptoms of stroke20–22 and reduce the risk of hemorrhagic transformation.23 Therefore, MMP9 can serve as both a biomarker and a potential target for treatment. No research has confirmed the relationship between MMP9 methylation and TIA/MIS, and there is no research on the relationship between MMP9 methylation and TIA/MIS with ECI. Therefore, we speculated that MMP9 methylation relates to TIA/MIS and TIA/MIS with ECI.
Materials and Methods
Participants
This study included 84 patients with TIA and MIS (NIHSS <5 points) who were hospitalized in the Department of Neurology of Qilu Hospital (Qingdao) of Shandong University from June 2019 to July 2020. In the control group, 28 healthy volunteers or dizziness/headache patients without TIA, ischemic stroke, and cerebral hemorrhage were collected in the same period. The TIA/MIS patients enrolled meet the following criteria: age 18–75; the NIHSS score is less than 5 points, and the cognitive scale assessment is completed within 7 days after the onset; TOAST classification was large artery atherosclerosis and small artery occlusion and confirmed by magnetic resonance imaging (MRI), computed tomography (CT), or both and vascular examination; no deafness, blindness, severe hemiplegia, severe depression, and anxiety; no acute cerebral hemorrhage, epilepsy, malignant tumor, degenerative disease, severe kidney and liver dysfunction, etc.; signed the informed consent form. Basic clinical data of all subjects were collected, including age, gender, education level, history (mainly including diabetes, coronary atherosclerotic heart disease, hypertension, hyperlipidemia), blood examination results (including low-density lipoprotein, high-density lipoprotein, uric acid, homocysteine, and vitamin B12), smoking history, alcohol history, and Fazekas score.
Cognitive Scales
The enrolled TIA/MIS patients were tested using the Boston Naming Test (BNT), Audit Verbal Learning Test (AVLT), Trail Making Test (TMT)-A, and TMT-B single-domain cognitive scales, and their language, memory, visuospatial, and executive function24–31 respectively. The criteria for the existence of abnormalities were as follows: having been educated for > 9 years with a score≤21.5 (if educated for≤9 years, the score≤19.5 points), indicating that there is a language barrier. An AVLT score <5 indicated memory dysfunction. TMT-A: if age is 50–64 years, visuospatial function≥80.5 s; age is 65–74 years, visuospatial function≥90.5 s; Age≥75 years, visuospatial function≥101.5 s. TMT-B: if age is 50–64 years, executive dysfunction≥150.5 s; age is 65–74 years, executive dysfunction≥165.5; Age ≥75 years, executive dysfunction≥199.5 s. CI was determined by≥1 scale abnormality.24 Two neurologists with at least 5 years of experience completed the scale evaluation in this study.
The Ethics Committee of Qilu Hospital (Qingdao) of Shandong University approved the study.
Methylation Sequencing
A reagent kit (Tianjin Biotech, Beijing, China) was used to extract the frozen whole blood DNA. DNA methylation was detected by Genesky Biotechnologies Inc. (Shanghai, China) using MethylTarget sequencing technology, which is based on second-generation sequencing and can accurately calculate the methylation level of each CpG site.32,33 The EZ DNA Calculation ™- GOLD Kit (ZYMO, CA, USA) reagent kit performed multiple sulfite treatments on the extracted DNA. GeneCpG software was used to analyze the genome of the region of interest and the bisulfite-treated sequence. Primer3 is used to design primers for the bisulfite-treated sequence (http://primer3.ut.ee/). The following table for primer designs (Table 1). Finally, after multiple PCR amplifications (HotStarTaq polymerase kit, TaKaRa, Dalian, China) and specific tag sequences were added to the samples, high-throughput sequencing (Illumina, CA, USA) was performed using the Illumina Hiseq platform.34
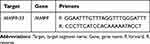 |
Table 1 Primer Information |
Statistical Methods
R software (version; R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analyses. Continuous data and categorical data are presented as mean ± standard deviation (x±s) and percentages (n [%]) respectively. The Student’s t-test was used for continuous variables with normal distribution and homogeneous variance to compare observations between both study groups, and the Wilcoxon test was used otherwise. The percentage test, including the chi-square test and Cochran–Armitage trend test, was used to determine whether there was a significant statistical difference between the percentage data. The chi-square test was used to test nominal classification variables, and the Cochran–Armitage trend test was used to test ordinal classification variables. Statistical significance was set at P < 0.05.
Results
We tested the target region (Table 2) methylation of the whole blood MMP9 gene in 112 samples (Figures 1–3), including 84 TIA/MIS patients and 28 control samples (Supplementary Table 1). The incidence of CI in TIA/MIS patients was 65.5% (55/84), and the incidence of CI was higher in patients with large atherosclerotic TIA/MIS (78.8%, 26/33) (Supplementary Table 2). The basic clinical data of all the cases are shown in the Supplementary material.
 |
Table 2 Information on Target DNA Methylation Sequencing |
 |
Figure 2 A heatmap based on the methylation levels of CpG sites in samples in groups LA and SA. |
 |
Figure 3 A heatmap based on the methylation levels of CpG sites in samples in groups A and B. |
Differences Between TIA/MIS and the Control Group in MMP9 Gene Methylation
We found that the methylation level of MMP9 gene in the whole blood of the TIA/MIS group (Group J) was significantly lower than that of the control group (Group C) (Groupdiff <0) (P<0.05) through sequencing methylation in the target region in 84 TIA/MIS patients and 28 control groups (Figure 4) (Supplementary Table 1). After analyzing the methylation levels at various sites between the TIA/MIS group and the control group, we found that the TIA/MIS group also had hypomethylation at sites S33-39, S33-53, S33-58, S33-73, S33-79 and S33-156 (Groupdiff <0), and there was a significant statistical difference compared with the control group (P<0.05). However, after adjustment for age, sex, and Fazekas score (Supplementary Table 1), only S33-79 showed a statistically significant difference between the two groups (P<0.05) (Table 3), respectively.
 |
Table 3 Differences in MMP9 Methylation Levels and Methylation Sites Between TIA/MIS and Control Groups |
 |
Figure 4 The difference in MMP9 methylation levels between group J and group C. The MMP9 gene was relatively hypomethylated in group J. |
Differences Between TIA/MIS Groups with Large Atherosclerosis and Small-Artery Occlusion in MMP9 Gene Methylation
We analyzed the methylation of the MMP9 gene between the two groups of large atherosclerosis (Group LA) and small artery occlusion (Group SA) TIA/MIS (Supplementary Table 3). We found that the methylation of the MMP9 gene at sites S33-25, S33-30, S33-39, S33-58, S33-73, S33-79, S33-113, and S33-131 in the LA group was significantly lower than that in the SA group (Groupdiff <0) (P<0.05) (Figure 5). There were still statistical differences in gene and site methylation levels between the two groups after adjusting for age, sex, and Fazekas score (Table 4) (Supplementary Table 3), respectively.
 |
Table 4 Differences in MMP9 Methylation Levels and Methylation Sites Between LA and SA Groups |
 |
Figure 5 The difference in MMP9 methylation levels between group LA and group SA. The MMP9 gene was relatively hypomethylated in group LA. |
Differences Between TIA/MIS with and without ECI in MMP9 Gene Methylation
After sequencing the methylation of the target region of 55 TIA/MIS patients with ECI (Group A) and 29 patients without ECI (Group B) (Supplementary Table 2), we found that although the average methylation level of the group with ECI was lower than that of the group without ECI (Groupdiff<0), there was no statistically significant difference between the two groups in MMP9 gene methylation level (P>0.05), even after adjusting for age, sex, education level, and Fazekas score (P>0.05) (Table 5 and Figure 6) (Supplementary Table 2).
 |
Table 5 Differences in MMP9 Methylation Levels and Methylation Sites Between TIA/MIS with and without ECI Groups |
 |
Figure 6 The difference in MMP9 methylation levels between group A and group B. The MMP9 gene was relatively hypomethylated in group A. |
However, after analyzing the methylation level of the whole blood MMP9 gene sites between the two groups, we found that the methylation levels of S33-25 and S33-30 were lower in the ECI group (Groupdiff <0), and there was a statistically significant difference between the two groups (P<0.05), even after adjusting for age, sex, education level, and Fazekas score (P<0.05) (Table 5) (Supplementary Table 2).
Discussion
The incidence of TIA/MIS with ECI was high, and our study found an incidence of 65.5%. These results are similar to those obtained by screening with MoCA and other scales.1,3 The cognitive function evaluation of TIA/MIS should not be ignored. The specific scale selection can be determined according to the patient’s actual situation. MMP9 can be used to reflect the degree of blood-brain barrier damage. There has been no research on the methylation of MMP9 after ischemic stroke. This study focused on the relationship between MMP9 methylation and TIA/MIS in ECI.
Hypomethylation of the MMP9 gene can lead to the upregulation of gene expression and an increase in MMP9 levels. Our study confirmed the overall hypomethylation of the MMP9 gene in the TIA/MIS group compared with the control group, and there was a significant statistical difference at sites S33-79. There is a clear correlation between MMP9 and ischemic stroke,18,35,36 and the destruction of the blood-brain barrier mainly causes the impact on ischemic stroke.20–23 Studies have shown that MMP2 and MMP9 can increase significantly during the early stages of ischemic stroke.22,35 Planas et al found in animal models that the levels of MMP2 and MMP9 in the brain tissue increased after ischemic stroke, but MMP9 increased more obviously in the early stage,36 and MMP9 played a greater role in the destruction of the blood-brain barrier in the later stage.35 Zhong et al found that increasing MMP9 in the serum of patients with acute ischemic stroke can increase the risk of poor prognosis.18 Some studies have confirmed that adding an MMP9 inhibitor can reduce the lesion volume, damage the blood-brain barrier,20–22 and reduce the risk of bleeding,23 showing that the intervention of MMP9 can affect the prognosis of ischemic stroke. These findings are consistent with our findings. MMP2 and MMP9 are gel-like enzymes. Lin et al found that MMP2 is hypomethylated in ischemic stroke,6 but there has been no research on the relationship between MMP9 methylation and ischemic stroke. This study confirmed that MMP9 gene site methylation relates to TIA/MIS.
After further analysis of the TIA/MIS group, we found that the whole blood MMP9 gene methylation level of TIA/MIS patients caused by large atherosclerosis was significantly lower than that of TIA/MIS patients caused by small arterial occlusion. The high expression of MMP9 caused by hypomethylation can aggravate damage to the blood-brain barrier. Patients with large atherosclerotic stenosis have a longer period of hypoperfusion in the brain tissue before the onset of stroke. Inflammation and oxidative stress reactions secondary to hypoperfusion can also lead to activation of the MMP family37,38 and aggravate damage to the blood-brain barrier. We consider that patients with large atherosclerotic stenosis were more likely to have larger defects and more lesions than patients with smaller artery occlusion, resulting in more severe blood-brain barrier damage, consistent with the trend of lower methylation levels of the MMP9 gene. In addition, in the analysis of this subgroup, we found that the statistical difference between the two groups was the most obvious, regardless of the total gene aspect or detected sites. This shows that hypomethylation of the MMP9 gene plays an important role in the pathogenesis of large atherosclerotic TIA/MIS. They strongly correlate and indirectly reflect the extent of TIA/MIS blood-brain barrier damage. MMP9 methylation can potentially become a biomarker for predicting the severity of TIA/MIS.
In this study, we found that the overall methylation level of MMP9 in the TIA/MIS group with ECI was lower than that in the group without ECI. Although there was no statistical difference, these results were consistent with the trend of previous research results and the process of MMP9 participating in pathology. We found that S33-25 and S33-30 of the MMP9 gene showed statistically significant differences between the groups with and without ECI, showing hypomethylation. Previous studies have found that increased serum MMP9 level in the acute phase of ischemic stroke is related to CI after 3 months.39 Bruno et al also found that the level of MMP9 in the brain tissue of patients with mild cognitive impairment (MCI) increased and speculated that the cause of CI might be related to the degradation mediated by MMP9.40 Adair et al found that the level of MMP9 in the cerebrospinal fluid of patients with vascular dementia was higher than that in patients with Alzheimer’s disease and the control group.41 In another study of patients with subcortical ischemic cerebrovascular disease, the overall level of MMP9 in the case group was higher. However, there was no significant difference between the levels of MMP9 in the cerebrospinal fluid of the case and control groups.42 Previous research results are consistent with those of TIA/MIS with ECI. Simultaneously, we also found two sites with statistical differences, which confirmed the correlation between lower methylation of the MMP9 gene site and TIA/MIS with ECI. The cause of CI caused by the increase in MMP9 levels is not completely clear, which may be related to the aggravation of blood-brain barrier damage. Thus affecting the transportation of toxic substances such as Aβ, causing Aβ accumulation in the brain, and the oxidative stress reaction is secondary. In general, this study showed that hypomethylation of MMP9 gene sites was associated with TIA/MIS with ECI, which was likely to be generated through the destruction of the blood-brain barrier and the secondary influence on Aβ transportation. Methylation of MMP9 gene sites can potentially become a biomarker and intervention target for TIA/MIS in patients with ECI.
Subgroup analysis of TIA/MIS with large atherosclerosis and small artery occlusion confirmed that hypomethylation of MMP9 has a stronger correlation with TIA/MIS with large atherosclerosis. In contrast, the subgroup analysis with and without ECI found that hypomethylation of MMP9 was associated with TIA/MIS with ECI. However, in stroke patients, the combination of large artery atherosclerotic stenosis and ECI is often associated with poor prognosis.1,43 The analysis between the two groups also indicated that the lower methylation of MMP9 was related to the poor prognosis of TIA/MIS to a certain extent.
This study also has some shortcomings. First, the number of patients in this study was small and not completely matched according to age and sex. However, when we conducted statistical research, we corrected for age and sex to minimize their impact on the study. Second, because this study aimed to find biomarkers in whole blood, the methylation level of the MMP9 gene in whole blood was detected. However, it cannot be confirmed that the methylation level of genes in whole blood is consistent with that in brain tissue. However, we consider that changes in the level of MMP9 in whole blood can also affect the blood-brain barrier. Blood samples could be easily obtained for dynamic monitoring if it was used as a biomarker or intervention target. Third, we studied just China’s population of stroke, can not full reflect the correlation between MMP9 methylation and TIA/MIS in other ethnic groups and races. Therefore, more researches may be needed in other ethnic groups and races.
Conclusion
The incidence of TIA/MIS with ECI is high, and cognitive function should be routinely screened in such patients. Hypomethylation of MMP9 was associated with TIA/MIS and TIA/MIS with ECI. Hypomethylation of MMP9 was strongly associated with TIA/MIS with large artery atherosclerosis. Methylation of MMP9 is involved in the pathogenesis of TIA/MIS and can reflect the severity of TIA/MIS. The methylation site of MMP9 can be used as a potential biomarker and therapeutic target for TIA/MIS and TIA/MIS with ECI.
Data Sharing Statement
The sequence data had been uploaded to the National Genomics Data Center. The raw sequence data reported in this paper have been deposited in the Genome Sequence Archive44 in National Genomics Data Center,45 China National Center for Bioinformation / Beijing Institute of Genomics, Chinese Academy of Sciences (GSA-Human: HRA004471) that are publicly accessible at https://ngdc.cncb.ac.cn/gsa-human.
Ethics Statement
The Ethics Committee of Qilu Hospital (Qingdao) of Shandong University approved the study. All patients provided written informed consent. The study complies with the Declaration of Helsinki.
Acknowledgments
We would like to thank Genesky Biotechnologies Inc. (Shanghai, China) for methylation sequencing and Editage for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Qingdao Key Health Discipline Development Fund and Scientific Research Foundation of Qilu Hospital of Shandong University (Qingdao) (No.QDKY2019ZD02).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Suda S, Nishimura T, Ishiwata A, et al. Early cognitive impairment after minor stroke: associated factors and functional outcome. J Stroke Cerebrovasc Dis. 2020;29(5):104749. doi:10.1016/j.jstrokecerebrovasdis.2020.104749
2. Pendlebury ST, Wadling S, Silver LE, Mehta Z, Rothwell PM. Transient cognitive impairment in TIA and minor stroke. Stroke. 2011;42(11):3116–3121. doi:10.1161/STROKEAHA.111.621490
3. Blackburn DJ, Bafadhel L, Randall M, Harkness KA. Cognitive screening in the acute stroke setting. Age Ageing. 2013;42(1):113–116. doi:10.1093/ageing/afs116
4. Godefroy O, Fickl A, Roussel M, et al. Is the Montreal cognitive assessment superior to the mini-mental state examination to detect poststroke cognitive impairment? A study with neuropsychological evaluation. Stroke. 2011;42(6):1712–1716. doi:10.1161/STROKEAHA.110.606277
5. Qin X, Li J, Wu T, et al. Overall and sex-specific associations between methylation of the ABCG1 and APOE genes and ischemic stroke or other atherosclerosis-related traits in a sibling study of Chinese population. Clin Epigenetics. 2019;11(1):189. doi:10.1186/s13148-019-0784-0
6. Lin HF, Hsi E, Huang LC, Liao YC, Juo SH, Lin RT. Methylation in the matrix metalloproteinase-2 gene is associated with cerebral ischemic stroke. J Investig Med. 2017;65(4):794–799. doi:10.1136/jim-2016-000277
7. Wei Y, Sun Z, Wang Y, et al. Methylation in the TP53 promoter is associated with ischemic stroke. Mol Med Rep. 2019;20(2):1404–1410. doi:10.3892/mmr.2019.10348
8. Lin RT, Hsi E, Lin HF, Liao YC, Wang YS, Juo SH. LINE-1 methylation is associated with an increased risk of ischemic stroke in men. Curr Neurovasc Res. 2014;11(1):4–9. doi:10.2174/1567202610666131202145530
9. Zhou S, Zhang Y, Wang L, et al. CDKN2B methylation is associated with carotid artery calcification in ischemic stroke patients. J Transl Med. 2016;14(1):333. doi:10.1186/s12967-016-1093-4
10. Zhou S, Cai B, Zhang Z, et al. CDKN2B Methylation and Aortic Arch Calcification in Patients with Ischemic Stroke. J Atheroscler Thromb. 2017;24(6):609–620. doi:10.5551/jat.36897
11. Hawkins BT, Davis TP. The blood-brain barrier/neurovascular unit in health and disease. Pharmacol Rev. 2005;57(2):173–185. doi:10.1124/pr.57.2.4
12. Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Dis. 2010;37(1):13–25. doi:10.1016/j.nbd.2009.07.030
13. Jiang X, Andjelkovic AV, Zhu L, et al. Blood-brain barrier dysfunction and recovery after ischemic stroke. Prog Neurobiol. 2018;163–164:144–171. doi:10.1016/j.pneurobio.2017.10.001
14. Huang J, Upadhyay UM, Tamargo RJ. Inflammation in stroke and focal cerebral ischemia. Surg Neurol. 2006;66(3):232–245. doi:10.1016/j.surneu.2005.12.028
15. Goulay R, Mena Romo L, Hol EM, Dijkhuizen RM. From stroke to dementia: a comprehensive review exposing tight interactions between stroke and amyloid-β formation. Transl Stroke Res. 2020;11(4):601–614. doi:10.1007/s12975-019-00755-2
16. Hawkes CA, Jayakody N, Johnston DA, Bechmann I, Carare RO. Failure of perivascular drainage of β-amyloid in cerebral amyloid angiopathy. Brain Pathol. 2014;24(4):396–403. doi:10.1111/bpa.12159
17. Tarasoff-Conway JM, Carare RO, Osorio RS, et al. Clearance systems in the brain-implications for Alzheimer disease. Nat Rev Neurol. 2015;11(8):457–470. doi:10.1038/nrneurol.2015.119
18. Zhong C, Yang J, Xu T, et al. Serum matrix metalloproteinase-9 levels and prognosis of acute ischemic stroke. Neurology. 2017;89(8):805–812. doi:10.1212/WNL.0000000000004257
19. Rodríguez-Yáñez M, Castellanos M, Blanco M, et al. New-onset hypertension and inflammatory response/poor outcome in acute ischemic stroke. Neurology. 2006;67(11):1973–1978. doi:10.1212/01.wnl.0000247064.53130.91
20. Cui J, Chen S, Zhang C, et al. Inhibition of MMP-9 by a selective gelatinase inhibitor protects neurovasculature from embolic focal cerebral ischemia. Mol Neurodegener. 2012;7:21. doi:10.1186/1750-1326-7-21
21. Yang Y, Thompson JF, Taheri S, et al. Early inhibition of MMP activity in ischemic rat brain promotes expression of tight junction proteins and angiogenesis during recovery. J Cereb Blood Flow Metab. 2013;33(7):1104–1114. doi:10.1038/jcbfm.2013.56
22. Romanic AM, White RF, Arleth AJ, Ohlstein EH, Barone FC. Matrix metalloproteinase expression increases after cerebral focal ischemia in rats: inhibition of matrix metalloproteinase-9 reduces infarct size. Stroke. 1998;29(5):1020–1030. doi:10.1161/01.str.29.5.1020
23. Turner RJ, Sharp FR. Implications of MMP9 for blood brain barrier disruption and hemorrhagic transformation following ischemic stroke. Front Cell Neurosci. 2016;10:56. doi:10.3389/fncel.2016.00056
24. Tian JZ, Xie HG, Qin B, et al. Screening and diagnostic framework of vascular dementia in Chinese population. Zhonghua Nei Ke Za Zhi. 2019;58(1):10–16. doi:10.3760/cma.j.issn.0578-1426.2019.01.003
25. Hao L, Xing Y, Li X, et al. Risk Factors and neuropsychological assessments of subjective cognitive decline (plus) in Chinese memory clinic. Front Neurosci. 2019;13:846. doi:10.3389/fnins.2019.00846
26. Ma J, Zhang Y, Guo Q. Comparison of vascular cognitive impairment--no dementia by multiple classification methods. Int J Neurosci. 2015;125(11):823–830. doi:10.3109/00207454.2014.972504
27. Xu Y, Chen K, Zhao Q, Li F, Guo Q. Short-term delayed recall of auditory verbal learning test provides equivalent value to long-term delayed recall in predicting MCI clinical outcomes: a longitudinal follow-up study. Appl Neuropsychol Adult. 2020;27(1):73–81. doi:10.1080/23279095.2018.1481067
28. Llinàs-Reglà J, Vilalta-Franch J, López-Pousa S, Calvó-Perxas L, Torrents Rodas D, Garre-Olmo J. The trail making test. Assessment. 2017;24(2):183–196. doi:10.1177/1073191115602552
29. Sánchez-Cubillo I, Periáñez JA, Adrover-Roig D, et al. Construct validity of the Trail Making Test: role of task-switching, working memory, inhibition/interference control, and visuomotor abilities. J Int Neuropsychol Soc. 2009;15(3):438–450. doi:10.1017/S1355617709090626
30. Wei M, Shi J, Li T, et al. Diagnostic accuracy of the Chinese version of the trail-making test for screening cognitive impairment. J Am Geriatr Soc. 2018;66(1):92–99. doi:10.1111/jgs.15135
31. Gorelick PB, Counts SE, Nyenhuis D. Vascular cognitive impairment and dementia. Biochim Biophys Acta. 2016;1862(5):860–868. doi:10.1016/j.bbadis.2015.12.015
32. Ashktorab H, Daremipouran M, Goel A, et al. DNA methylome profiling identifies novel methylated genes in African American patients with colorectal neoplasia. Epigenetics. 2014;9(4):503–512. doi:10.4161/epi.27644
33. Wilmot B, Fry R, Smeester L, Musser ED, Mill J, Nigg JT. Methylomic analysis of salivary DNA in childhood ADHD identifies altered DNA methylation in VIPR2. J Child Psychol Psychiatry. 2016;57(2):152–160. doi:10.1111/jcpp.12457
34. Masser DR, Berg AS, Freeman WM. Focused, high accuracy 5-methylcytosine quantitation with base resolution by benchtop next-generation sequencing. Epigenetics Chromatin. 2013;6(1):33. doi:10.1186/1756-8935-6-33
35. Yang Y, Estrada EY, Thompson JF, Liu W, Rosenberg GA. Matrix metalloproteinase-mediated disruption of tight junction proteins in cerebral vessels is reversed by synthetic matrix metalloproteinase inhibitor in focal ischemia in rat. J Cereb Blood Flow Metab. 2007;27(4):697–709. doi:10.1038/sj.jcbfm.9600375
36. Planas AM, Solé S, Justicia C. Expression and activation of matrix metalloproteinase-2 and −9 in rat brain after transient focal cerebral ischemia. Neurobiol Dis. 2001;8(5):834–846. doi:10.1006/nbdi.2001.0435
37. Stamatovic SM, Johnson AM, Keep RF, Andjelkovic AV. Junctional proteins of the blood-brain barrier: new insights into function and dysfunction. Tissue Barriers. 2016;4(1):e1154641. doi:10.1080/21688370.2016.1154641
38. Lenglet S, Montecucco F, Mach F, Schaller K, Gasche Y, Copin JC. Analysis of the expression of nine secreted matrix metalloproteinases and their endogenous inhibitors in the brain of mice subjected to ischaemic stroke. Thromb Haemost. 2014;112(2):363–378. doi:10.1160/TH14-01-0007
39. Zhong C, Bu X, Xu T, et al. Serum matrix metalloproteinase-9 and cognitive impairment after acute ischemic stroke. J Am Heart Assoc. 2018;7(1):e007776. doi:10.1161/JAHA.117.007776
40. Bruno MA, Mufson EJ, Wuu J, Cuello AC. Increased matrix metalloproteinase 9 activity in mild cognitive impairment. J Neuropathol Exp Neurol. 2009;68(12):1309–1318. doi:10.1097/NEN.0b013e3181c22569
41. Adair JC, Charlie J, Dencoff JE, et al. Measurement of gelatinase B (MMP-9) in the cerebrospinal fluid of patients with vascular dementia and Alzheimer disease. Stroke. 2004;35(6):e159–e162. doi:10.1161/01.STR.0000127420.10990.76
42. Candelario-Jalil E, Thompson J, Taheri S, et al. Matrix metalloproteinases are associated with increased blood-brain barrier opening in vascular cognitive impairment. Stroke. 2011;42(5):1345–1350. doi:10.1161/STROKEAHA.110.600825
43. Hoshino T, Sissani L, Labreuche J, et al. Prevalence of systemic atherosclerosis burdens and overlapping stroke etiologies and their associations with long-term vascular prognosis in stroke with intracranial atherosclerotic disease. JAMA Neurol. 2018;75(2):203–211. doi:10.1001/jamaneurol.2017.3960
44. Chen T, Chen X, Zhang S, et al. The genome sequence archive family: toward explosive data growth and diverse data types. Genomics Proteomics Bioinformatics. 2021;19(4):578–583. PMID=34400360. doi:10.1016/j.gpb.2021.08.001
45. Members CN. Database resources of the national genomics data center, China national center for bioinformation in 2022. Nucleic Acids Res. 2022;50(D1):D27–D38. PMID=34718731. doi:10.1093/nar/gkab951
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

