Back to Journals » International Journal of General Medicine » Volume 17
Correlation Between Maternal Anxiety During Mid-Pregnancy and Subsequent Infant Sleep Issues: A Cross-Sectional Study from 2015 to 2016
Authors Wang S, Cai Z, Gao G, Yan S
Received 27 October 2023
Accepted for publication 25 January 2024
Published 21 February 2024 Volume 2024:17 Pages 623—633
DOI https://doi.org/10.2147/IJGM.S445604
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Woon-Man Kung
Sumei Wang, Zhiling Cai, Guopeng Gao, Shuangqin Yan
Ma’anshan Maternal and Child Health Center, Ma’anshan, Anhiu Province, 243011, People’s Republic of China
Correspondence: Shuangqin Yan, Ma’anshan Maternal and Child Health Center, No. 446 Jiashan Road, Ma’anshan, Anhiu Province, 243011, People’s Republic of China, Tel/Fax +86 555-2364042, Email [email protected]
Purpose: To explore the correlation between maternal anxiety during mid-pregnancy and infant sleep issues based on the anxiety status of mothers in mid-pregnancy.
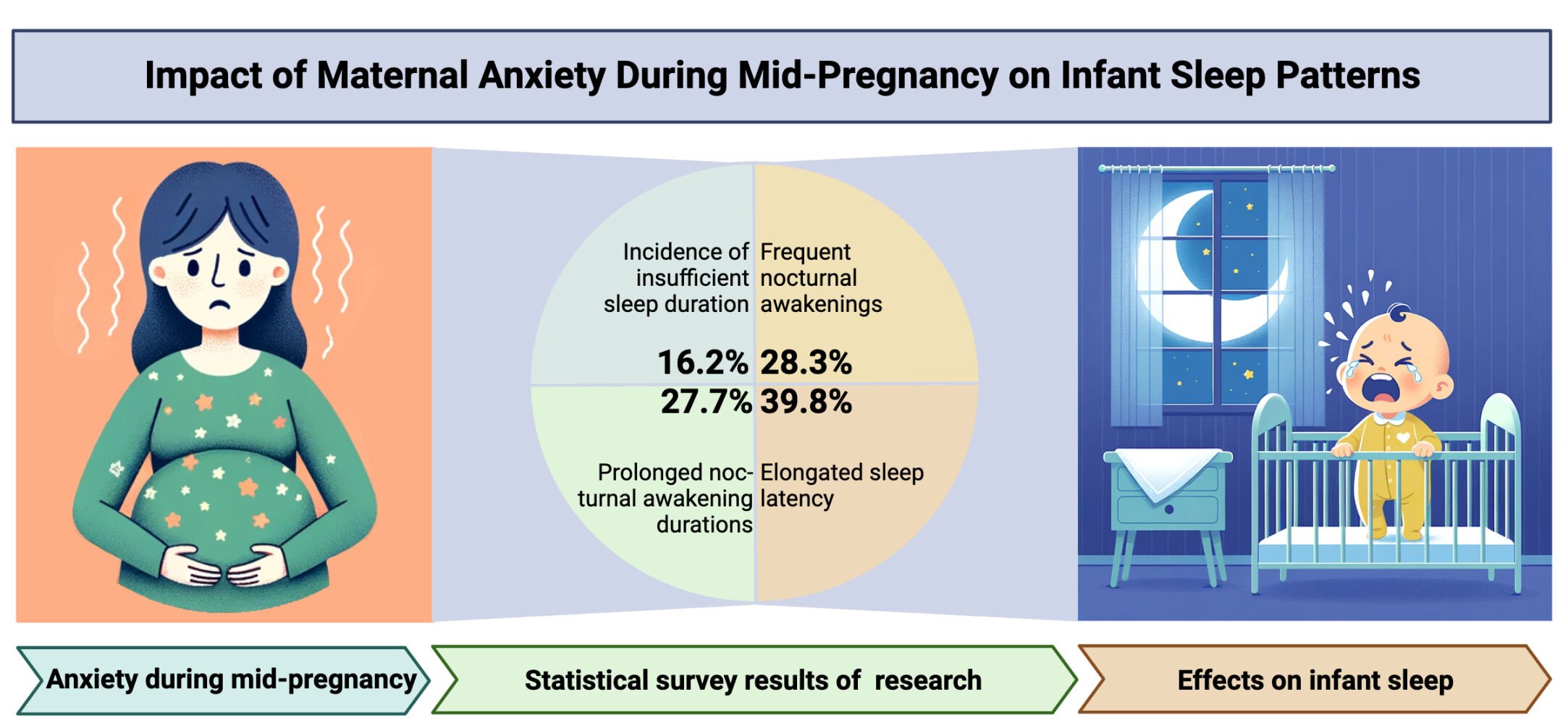
Patients and Methods: A cohort of 2122 primigravida women from Ma’anshan City, Anhui Province, was followed from pregnancy until 6 months postpartum. The study analyzed the impact of maternal anxiety on infant sleep patterns, including primary caregivers, encompassing insufficient sleep duration, frequent nocturnal awakenings, prolonged nocturnal awakening durations, and elongated sleep latency.
Results: A total of 1891 mother-infant pairs were included in this analysis. After adjusting for confounding factors, a positive correlation was found between maternal anxiety during mid-pregnancy and insufficient sleep duration (OR=1.69, 95% CI:1.13– 2.52), and elongated sleep latency (OR=2.26, 95% CI:1.61– 3.18).
Conclusion: Maternal anxiety during mid-pregnancy is associated with sleep issues in infants. Addressing maternal mental health during pregnancy may enhance sleep quality for mothers and infants, promoting overall maternal-infant health.
Keywords: pregnancy anxiety, pregnancy, infant, sleep
A Letter to the Editor has been published for this article.
Graphical Abstract:
Introduction
Many women experience mental health issues during pregnancy or postpartum. Depression and anxiety are the most common mental health concerns during pregnancy, affecting a significant number of expectant mothers. Antenatal anxiety could potentially predict postpartum depressive symptoms.1 There’s a necessity for active assessment and management of stress, anxiety, and depression, starting from early pregnancy and continuing postpartum.2 As a prevalent type of prenatal stress, pregnancy anxiety can impair the nervous system, neurocognitive functions, brain processing, functional and structural brain region connectivity, hypothalamic-pituitary-adrenal axis, and autonomic nervous system, thereby affecting offspring development and prenatal health.3 Anxiety during pregnancy can lead to a myriad of problems, including but not limited to, lack of focus, irritability, and in severe cases, suicidal tendencies.4 Symptoms such as dry mouth, irritability, sweating, vomiting require attention; severe cases might experience trembling, difficulty in breathing, even suicidal thoughts and actions—these are undoubtedly the most dangerous manifestations of pregnancy syndrome. Factors like hormonal changes during pregnancy, previous miscarriages or problematic pregnancies, and sleep disturbances might contribute to anxiety in expectant mothers.5,6 Concerns may range from worrying about the baby’s health and birth-related issues, the impact of the new baby on relationships with friends and family, to the financial strain of adding a new member to the family. In the post-pandemic era of 2021–2022, many expectant mothers staying at home for extended periods inevitably find themselves scrolling through news of the pandemic on their mobile phones, exacerbating anxiety. Research suggests that anxiety is a natural emotional response when feeling uneasy or threatened.
Although, from an evolutionary perspective, anxiety serves as a primal instinct for self-preservation when facing the unknown, leading to tension and stress due to the necessity of dealing with and resolving new issues.7 However, studies have confirmed that anxiety during pregnancy could have negative effects on both the mother and fetus, increasing the risks of preterm birth, low birth weight, and early pregnancy complications. Moreover, maternal anxiety could affect fetal cortical brain development, enhance the fetus’s alert temperament, and increase the likelihood of behavioral and emotional management disorders in children later in life.8
Currently, infant sleep problems have emerged as a major public health issue. A search through the Wanfang database revealed that in China, the incidence rate of sleep problems among infants and toddlers aged 1–23 months reaches as high as 65.9%.9 Among 0–36-month-old infants and toddlers, the incidence of sleep disorders reported by parents is 30.7%. Good sleep is essential for the healthy growth of infants and toddlers, significantly impacting their physical, cognitive, and central nervous system development.10 Infant sleep problems are influenced by physiological, psychological, and social factors,11 Many studies have confirmed the association between early childhood sleep problems and neurocognition,12 emotion,13 and diseases14 in children. Infant sleep problems can adversely affect various aspects of an infant’s growth, cognition, and socio-emotional interactions and could potentially continue into preschool and school age, even leading to sleep disorders in adulthood, thereby affecting family functioning.15 Persistent infant sleep problems can have numerous adverse effects on the infant and their family. Therefore, early prevention of children’s sleep problems is helpful for both children and families.
This study, through a birth cohort research design, aims to explore the association between maternal anxiety during mid-pregnancy and infant sleep problems, to promote psychological assessment and adjustment during pregnancy, reduce infant sleep problems, and enhance maternal-infant health. By elucidating the positive correlation between maternal anxiety during mid-pregnancy and infant sleep problems, this study provides crucial scientific evidence for promoting attention and improvement in maternal mental health during pregnancy, actively contributing to reducing infant sleep problems and promoting maternal-infant health.
Materials and Methods
Objects
This research is a prospective birth cohort study, encompassing a Ma’anshan city maternal and infant health birth cohort established at the Ma’anshan City Maternal and Child Health Hospital from June 2015 to June 2016.
Inclusion Criteria: The study included healthy pregnant women residing in Ma’anshan city who were between 6 to 12 weeks of gestation and planned to give birth at this hospital, with this pregnancy being singleton. After excluding those who had miscarriages or induced abortions, a total of 2122 pregnant women were included, with follow-ups conducted from pregnancy until the infant reached 6 months of age.
Exclusion Criteria: A total of 231 mother-infant pairs were excluded from the study due to lost follow-up, or incomplete information regarding maternal anxiety during pregnancy or infant sleep conditions.
In this research, a total of 1891 mother-infant pairs were included in the analysis. The study received approval from the Medical Ethics Committee of Ma’anshan City Maternal and Child Health Hospital (Approval Number: 2016–003). All subjects signed an informed consent form.
Methods
Basic Information
Demographic information of both pregnant women and their spouses (age, educational level, per capita monthly household income, etc.) were collected during early pregnancy. At the 6-month mark post-birth, information regarding sleep habits, sleeping environments, and feeding methods were gathered.
Anxiety During Mid-Pregnancy
Anxiety levels during mid-pregnancy were assessed using the Self-rating Anxiety Scale (SAS).16,17 This scale comprises 20 items reflecting subjective feelings of anxiety, with scoring based on the frequency of symptoms experienced within a week, categorized into four levels: none or a small amount of time, a small portion of time, a substantial amount of time, and most or all of the time. A standard score is obtained by multiplying the total score of the 20 items by 1.25, where a standard score of <50 indicates no anxiety, and a standard score of ≥50 indicates anxiety.
Infant Sleep Conditions
At the 6-month mark, primary caregivers reported “average nighttime sleep duration” and “average daytime sleep duration” for the infants, the sum of which constitutes the total sleep duration. Referring to the guidelines of the “0 to 5 years old Children Sleep Hygiene Guide” and based on a report retrieved from the Wanfang database, sleep duration of <12 hours is defined as “insufficient sleep duration.” Caregivers also reported the “average number of times baby wakes up at night”, with ≥3 times per night defined as “frequent nocturnal awakenings”, as per the research standards set by Weng et al.9 They reported “how long the baby stays awake during the night (10 PM to 6 AM)”, with total nocturnal wakefulness ≥ the 75th percentile of the surveyed population (60 min) defined as “prolonged nocturnal awakening”.9 Additionally, the time it takes for the baby to fall asleep at night was reported, with sleep latency of >20 minutes defined as “prolonged sleep latency” as per the “0 to 5 years old Children Sleep Hygiene Guide”.
Control Variables
Referring to previous infant sleep studies, factors that may influence infant sleep conditions were taken as control variables. These include sleep habits, sleeping environments, current feeding methods, and any history of illness in the past three months, based on their known potential influence on infant sleep conditions, as evidenced by previous studies in this field.18,19
Quality Control
The survey questionnaire was finalized under the ethical approval of Ma’anshan City Maternal and Child Health Hospital and under the guidance of medical experts holding the title of associate chief physician or above, after multiple revisions. Questionnaires were distributed by trained investigators who explained the purpose of the study and how to complete the questionnaire. During on-site surveys, questionnaires were uniformly coded. Upon completion by parents, investigators carefully checked the content for missing or unclear information, making on-the-spot corrections or additions as necessary. Reasons for lost follow-ups were noted, and phone reminders were sent to pregnant women and children who missed their scheduled check-ups.
Statistical Analysis
Data was entered into the Epidata 3.0 database and, after verification for accuracy, analyzed using SPSS 13.0 software. Age distribution was represented as  , while gender, pregnancy anxiety, insufficient sleep duration, frequent nocturnal awakenings, prolonged nocturnal awakening, and prolonged sleep latency were all count data, described by frequency and percentage. The χ2 test was employed to compare the distribution of different characteristic variables of infant sleep conditions and maternal anxiety during pregnancy. Multifactorial non-conditional logistic regression models were used to analyze the impact of pregnancy anxiety on infant sleep conditions before and after adjusting for other factors. Two-sided tests were conducted with a significance level of α=0.05.
, while gender, pregnancy anxiety, insufficient sleep duration, frequent nocturnal awakenings, prolonged nocturnal awakening, and prolonged sleep latency were all count data, described by frequency and percentage. The χ2 test was employed to compare the distribution of different characteristic variables of infant sleep conditions and maternal anxiety during pregnancy. Multifactorial non-conditional logistic regression models were used to analyze the impact of pregnancy anxiety on infant sleep conditions before and after adjusting for other factors. Two-sided tests were conducted with a significance level of α=0.05.
Results
Basic Information
The age of the pregnant women was (26.86±3.73) years, with male infants constituting 51.9% (981/1891) of the cohort. The incidence of insufficient sleep duration in infants was 16.2% (305/1881), frequent nocturnal awakenings was 28.3% (536/1891), prolonged nocturnal awakening was 27.7% (523/1891), and prolonged sleep latency was 39.8% (752/1891).
Distribution of Anxiety During Pregnancy Across Different Characteristic Variables
As demonstrated in Table 1, the detection rate of anxiety during mid-pregnancy was 8.1% (153/1891), indicating a statistically significant correlation (P<0.05) between maternal anxiety during mid-pregnancy and factors such as maternal age, nature of work, pre-pregnancy BMI, and pre-pregnancy alcohol consumption. However, there was no statistically significant difference in the distribution of anxiety during mid-pregnancy among groups characterized by maternal educational level, per capita monthly household income, only-child status, or first-time pregnancy.
 |
Table 1 Anxiety Distribution of Pregnant Women with Different Characteristic Variables in the Second Trimester |
Distribution of Infant Sleep Conditions Across Different Characteristic Variables
Our findings (Table 2) suggest that maternal anxiety during mid-pregnancy, paternal educational level, and per capita monthly household income are associated with insufficient infant sleep duration. Factors such as gender, sleep habits, sleeping environments, and feeding methods are related to frequent nocturnal awakenings in infants. Paternal educational level is correlated with prolonged nocturnal awakening in infants. Maternal anxiety during mid-pregnancy, gender, and feeding methods are associated with prolonged sleep latency in infants, with all differences being statistically significant (P<0.05).
 |
Table 2 Distribution of Infant Sleep Problems Across Various Characteristic Variables |
Correlation Between Anxiety During Mid-Pregnancy and Infant Sleep Conditions
As shown in Table 3, univariate logistic regression analysis revealed that, compared to no anxiety during mid-pregnancy, anxiety during this period is positively correlated with insufficient infant sleep duration (OR=1.75, 95% CI:1.18~2.58) and prolonged sleep latency (OR=2.26, 95% CI:1.61~3.15). After adjusting for variables such as child gender, history of illness in the past three months, paternal educational level, per capita monthly household income, sleep habits, sleeping environments, and current feeding methods, multivariate logistic regression analysis showed that anxiety during mid-pregnancy was associated with insufficient infant sleep duration (OR=1.69, 95% CI:1.13~2.52) and prolonged sleep latency (OR=2.26, 95% CI:1.61~3.18).
 |
Table 3 Logistic Regression Analysis on the Association Between Second Trimester Anxiety and Infant Sleep Conditions [or (95% CI)] |
Discussion
The stress and anxiety experienced by mothers during pregnancy have long-term associations with the development of their infants.20 Exposure to maternal anxiety in utero is linked with a higher risk of emotional and behavioral issues in children, as well as anxiety and depression levels in adulthood.20 While the incidence of anxiety during pregnancy is not lesser than that of depression during pregnancy,21 the majority of existing research concerning maternal mental health and infant sleep primarily focuses on maternal depression22. The impact of anxiety could be as significant as that of depression during pregnancy. This study, by establishing a mother-infant birth cohort, delineates the levels of maternal anxiety during mid-pregnancy and the distribution of infant sleep problems, exploring their interrelation. It underscores the importance and impact of anxiety during pregnancy on maternal mental health and infant sleep quality, alongside the potential role regional variations might play in the incidence of anxiety.
The existing tools for measuring anxiety include those based on Rogers’ Self Consistency and Congruence, the Eysenck Personality Questionnaire (EPQ),23 and the Raven’s Standard Progressive Matrices (SPM).24 In China, the Self-rating Anxiety Scale (SAS) is widely used.25 It is a self-assessment scale consisting of 20 items, rated on a four-level scale, designed to evaluate the subjective feelings of anxiety patients. Its structure and specific assessment methods are very similar to those of the Self-rating Depression Scale (SDS), and both are known for their efficiency, simplicity, and ease of analysis, making them suitable evaluation tools. In China, the cutoff values (including severity thresholds) for these scales are based on percentile distributions in the general population and have not undergone clinical validity testing. Internationally, even in developing countries like Brazil, clinical validity tests are conducted for special populations, such as Parkinson’s disease patients. Therefore, it is necessary to conduct related clinical validity studies to better utilize these tools in clinical work.
Our findings indicate that the detection rate of maternal anxiety during mid-pregnancy is 8.1%, which is lower than the rate reported by Sun et al9 in their study conducted across multiple regions in China. Despite the fact that our study only investigated the anxiety detection rate among pregnant women in Ma’anshan city, it nevertheless unveils the influence of regional variations within the same territory on the incidence of anxiety during pregnancy, suggesting that maternal anxiety might be associated with different socioeconomic conditions, cultural disparities, and the availability of healthcare resources across various regions.26 Our results are similar to those in other countries,27–29 these insights call for future research to consider regional differences, potentially necessitating collaborative studies across different regions to gain a more comprehensive understanding and to verify the economic disparities brought about by regional variations, which might, in turn, negatively affect newborns.
However, anxiety does not present as a binary state, but rather exists on a continuum. The cutoff score used for defining “anxiety” in this research, while methodologically useful, should not be interpreted as a definitive demarcation of the absence or presence of anxiety. This approach acknowledges the nuanced and varied manifestations of anxiety symptoms, ranging from mild to severe. Our decision to use a specific cutoff point is a practical choice to facilitate analysis, yet we understand that it does not capture the full spectrum of anxiety experiences. This perspective aligns with contemporary understandings in psychology that emphasize the dimensional nature of mental health symptoms, and we suggest future studies consider this continuum in their analytical frameworks.
The regulation of sleep-wake cycles and sleep architecture undergo rapid development during infancy and continue to mature throughout childhood. Increasing evidence suggests that childhood sleep problems are associated with adverse developmental outcomes concerning physical health, cognition, emotions, and behavior.30,31 Our study identifies a positive correlation between maternal anxiety during mid-pregnancy and insufficient infant sleep duration as well as prolonged sleep latency. That is, infants of mothers who were anxious during mid-pregnancy had higher risks of experiencing insufficient sleep and prolonged sleep latency. Mid-pregnancy is a crucial period for the development of the fetal nervous system, and maternal anxiety may impact fetal neurodevelopment via biological pathways such as cortisol hormone levels. For instance, research indicates that maternal anxiety and stress can affect the fetal Hypothalamic-Pituitary-Adrenal (HPA) axis, which might further impact infant sleep patterns.26 Therefore, early identification and management of anxiety during pregnancy could be key in preventing infant sleep problems.
In addition to the factors already considered, it is important to acknowledge the potential role of genetics in both maternal anxiety and infant sleep issues. Recent studies suggest that genetic predispositions can influence the likelihood of developing anxiety disorders, as well as affect sleep patterns and quality.32–34 These findings imply that the associations observed in our study might be partially influenced by genetic factors. This underscores the complexity of the relationship between maternal anxiety and infant sleep, suggesting that both environmental and genetic factors should be considered in future research to fully understand these associations.
Providing mental health services during pregnancy can not only ameliorate maternal mental health but also may help prevent infant sleep problems and other developmental issues.35 Moreover, collaboration among mental health professionals, obstetricians, and pediatricians may foster a better understanding and addressing of the relationship between anxiety during pregnancy and infant sleep problems. Through interdisciplinary collaboration, more comprehensive and coordinated care can be provided to pregnant women and newborns, thereby improving overall maternal-infant health outcomes.
Conclusion
This study offers valuable insights for physicians and other healthcare professionals to understand and support maternal mental health and its implications on infant sleep quality. It also lays a foundation for public health strategy formulation, particularly in rendering mental health services and education during pregnancy, which holds practical significance for the clinical practice of precision medicine in postnatal care. Additionally, it aids in a more accurate understanding of the relationship between child sleep and caregiver anxiety among other mental health issues. Furthermore, in this research, we employed caregiver-reported questionnaires to collect data on infant sleep outcomes, which could potentially introduce issues due to subjective memory bias. Hence, we recommend the incorporation of objective measurement and diagnostic tools in future research endeavors.
Ethical Statement
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Ma’anshan City Maternal and Child Health Hospital (No. 2016-003). We ensured that all participants were fully informed and provided their written informed consent. All procedures in this study were in compliance with international and national ethical standards and were strictly protective of participants’ privacy and personal data.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Chauhan A, Potdar J, Chauhan A, Potdar J. Maternal mental health during pregnancy: a critical review. Cureus. 2022;14(10). doi:10.7759/cureus.30656
2. Cheng CY, Chou YH, Chang CH, Liou SR. Trends of perinatal stress, anxiety, and depression and their prediction on postpartum depression. Int J Environ Res Public Health. 2021;18(17):9307. doi:10.3390/ijerph18179307
3. Van den Bergh BRH, van den Heuvel MI, Lahti M, et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehav Rev. 2020;117:26–64. doi:10.1016/j.neubiorev.2017.07.003
4. Zaręba K, Banasiewicz J, Rozenek H, Wójtowicz S, Jakiel G. Peripartum predictors of the risk of postpartum depressive disorder: results of a case-control study. Int J Environ Res Public Health. 2020;17(23):8726. doi:10.3390/ijerph17238726
5. Wahabi HA, Fayed AA, Esmaeil SA, Bahkali KH. Progestogen for treating threatened miscarriage. Cochrane Database Syst Rev. 2018;2018(8):CD005943. doi:10.1002/14651858.CD005943.pub5
6. Hashmi AM, Bhatia SK, Bhatia SK, Khawaja IS. Insomnia during pregnancy: diagnosis and rational interventions. Pak J Med Sci. 2016;32(4):1030–1037. doi:10.12669/pjms.324.10421
7. Steimer T. The biology of fear- and anxiety-related behaviors. Dialogues Clin Neurosci. 2002;4(3):231–249. doi:10.31887/DCNS.2002.4.3/tsteimer
8. Hasanjanzadeh P. Relationship between maternal general and specific-pregnancy stress, anxiety, and depression symptoms and pregnancy outcome. JCDR. 2017. doi:10.7860/JCDR/2017/24352.9616
9. Wanfang database. Available from: https://d.wanfangdata.com.cn/periodical/ChlQZXJpb2RpY2FsQ0hJTmV3UzIwMjMxMjI2Eg96aGx4YngyMDIwMDMwMDUaCHYyb3Npb3cx.
10. Ramar K, Malhotra RK, Carden KA, et al. Sleep is essential to health: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2021;17(10):2115–2119. doi:10.5664/jcsm.9476
11. Touchette É, Petit D, Paquet J, et al. Factors associated with fragmented sleep at night across early childhood. Arch Pediatr Adolesc Med. 2005;159(3):242–249. doi:10.1001/archpedi.159.3.242
12. Turnbull K, Reid GJ, Morton JB. Behavioral sleep problems and their potential impact on developing executive function in children. Sleep. 2013;36(7):1077–1084. doi:10.5665/sleep.2814
13. Hysing M, Sivertsen B, Garthus-Niegel S, Eberhard-Gran M. Pediatric sleep problems and social-emotional problems. A population-based study. Infant Behav Dev. 2016;42:111–118. doi:10.1016/j.infbeh.2015.12.005
14. Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity. 2008;16(2):265–274. doi:10.1038/oby.2007.63
15. Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2009;14(2):89–96. doi:10.1016/j.smrv.2009.05.003
16. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi:10.1016/S0033-3182(71)71479-0
17. Wu Q, Liu L, Jiang X, et al. Effect of voluntary breathing exercises on stable coronary artery disease in heart rate variability and rate-pressure product: a study protocol for a single-blind, prospective, randomized controlled trial. Trials. 2020;21(1):602. doi:10.1186/s13063-020-04402-2
18. Smith JP, Forrester RI. Association between breastfeeding and new mothers’ sleep: a unique Australian time use study. Int Breastfeed J. 2021;16(1):7. doi:10.1186/s13006-020-00347-z
19. Ragni B, De Stasio S, Barni D, Gentile S, Giampaolo R. Parental mental health, fathers’ involvement and bedtime resistance in infants. Ital J Pediatr. 2019;45(1):134. doi:10.1186/s13052-019-0731-x
20. Mareckova K, Mareček R, Jani M, et al. Association of maternal depression during pregnancy and recent stress with brain age among adult offspring. JAMA Network Open. 2023;6(1):e2254581. doi:10.1001/jamanetworkopen.2022.54581
21. Fairbrother N, Janssen P, Antony MM, Tucker E, Young AH. Perinatal anxiety disorder prevalence and incidence. J Affective Disorders. 2016;200:148–155. doi:10.1016/j.jad.2015.12.082
22. Armitage R, Flynn H, Hoffmann R, Vazquez D, Lopez J, Marcus S. Early developmental changes in sleep in infants: the impact of maternal depression. Sleep. 2009;32(5):693–696. doi:10.1093/sleep/32.5.693
23. Liu X-K, Chen S-L, Huang D-L. The influence of personality and demographic characteristics on aggressive driving behaviors in Eastern Chinese Drivers. Psychol Res Behav Manag. 2022;15:193–212. doi:10.2147/PRBM.S323431
24. Morrison GE, Simone CM, Ng NF, Hardy JL. Reliability and validity of the NeuroCognitive Performance Test, a web-based neuropsychological assessment. Front Psychol. 2015;6:1652. doi:10.3389/fpsyg.2015.01652
25. Liang B, Zou FH, Fu L, Liao HL. Chinese Herbal Medicine Dingji Fumai Decoction for ventricular premature contraction: a real-world trial. Biomed Res Int. 2020;2020:5358467. doi:10.1155/2020/5358467
26. Ndugga N, Samantha A. Disparities in health and health care: 5 key questions and answers. KFF; 2023. Available from: https://www.kff.org/racial-equity-and-health-policy/issue-brief/disparities-in-health-and-health-care-5-key-question-and-answers/.
27. Nath S, Pearson RM, Moran P, et al. The association between prenatal maternal anxiety disorders and postpartum perceived and observed mother-infant relationship quality. J Anxiety Disord. 2019;68:102148. doi:10.1016/j.janxdis.2019.102148
28. Koutra K, Chatzi L, Bagkeris M, Vassilaki M, Bitsios P, Kogevinas M. Antenatal and postnatal maternal mental health as determinants of infant neurodevelopment at 18 months of age in a mother-child cohort (Rhea Study) in Crete, Greece. Soc Psychiatry Psychiatr Epidemiol. 2013;48(8):1335–1345. doi:10.1007/s00127-012-0636-0
29. Cai S, Phua DY, Tham EKH, et al. Mid-pregnancy and postpartum maternal mental health and infant sleep in the first year of life. J Sleep Res. 2023;32(3):e13804. doi:10.1111/jsr.13804
30. Tham E, Schneider N, Broekman B. Infant sleep and its relation with cognition and growth: a narrative review. NSS. 2017;9:135–149. doi:10.2147/NSS.S125992
31. Short MA, Blunden S, Rigney G, et al. Cognition and objectively measured sleep duration in children: a systematic review and meta-analysis. Sleep Health. 2018;4(3):292–300. doi:10.1016/j.sleh.2018.02.004
32. Brescianini S, Volzone A, Fagnani C, et al. Genetic and environmental factors shape infant sleep patterns: a study of 18-month-old twins. Pediatrics. 2011;127(5):e1296–e1302. doi:10.1542/peds.2010-0858
33. Touchette E, Dionne G, Forget-Dubois N, et al. Genetic and environmental influences on daytime and nighttime sleep duration in early childhood. Pediatrics. 2013;131(6):e1874–e1880. doi:10.1542/peds.2012-2284
34. Fisher-Owens SA, Gansky SA, Platt LJ, et al. Influences on children’s oral health: a conceptual model. Pediatrics. 2007;120(3):e510–520. doi:10.1542/peds.2006-3084
35. Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19(3):313–327. doi:10.1002/wps.20769
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
