Back to Journals » Patient Preference and Adherence » Volume 12
Comparison of health system responsiveness between HIV and non-HIV patients at infectious disease clinics in Yunnan, China
Authors Li J, Chongsuvivatwong V , Assanangkornchai S , McNeil EB , Cai L
Received 22 January 2018
Accepted for publication 28 March 2018
Published 29 June 2018 Volume 2018:12 Pages 1129—1137
DOI https://doi.org/10.2147/PPA.S163416
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Jing Li,1 Virasakdi Chongsuvivatwong,2 Sawitri Assanangkornchai,2 Edward B McNeil,2 Le Cai1
1School of Public Health, Kunming Medical University, Kunming, Yunnan Province, China; 2Epidemiology Unit, Faculty of Medicine, Prince of Songkla University, Hat Yai, Songkhla, Thailand
Background: China is in an epidemiologic transition period. Health system responsiveness (HSR) has become an increasing concern in China. With the burden of increasing human immunodeficiency virus (HIV) infection/acquired immune deficiency syndrome, responsiveness of HIV care is urgently needed. We aimed at comparing the experience of HSR between HIV-positive and non-HIV patients.
Methods: A cross-sectional study was carried out in Yunnan, China, from January to February 2015 among two consecutive groups of HIV and non-HIV patients in two hospitals with the largest HIV admissions. Patients’ experience and expectation of HSR were measured using a self-reported questionnaire containing items of seven domains and 35 vignettes (five per domain). Each of the items and vignettes was ranked from 1 “very good” to 5 “very bad.” For each domain, B-scales were built based on the difference between experience and the vignettes. Ordered probit and censored ordered probit regression models were constructed to compare HSR experience between the two groups adjusted for socioeconomic status (SES) factors.
Results: The majority of HIV patients were at clinical stage 1, were infected via unprotected sexual contact, and had a CD4 count <500 cells/µL. After adjustment by SES factors, HIV patients had better experiences of HSR in six of the seven HSR domains, prompt attention being the only domain that non-HIV patients had better experiences.
Conclusion: Perceptions of HSR experience were better among HIV patients except for prompt attention, which could not be explained by SES factors and difference in expectations. A reform is needed not to neglect the needs of non-HIV patients in the study area.
Keywords: health system responsiveness, anchoring vignettes, HIV care, China
Introduction
China is in an epidemiologic transition period. The quality of health care faces noteworthy challenges, especially due to nonclinical determinants such as patients’ perceptions of their experience in clinics. Public perceptions of responsiveness, trustworthiness, and quality are low. One study revealed that about 55% of residents from the lowest and highest income quintile groups were not satisfied with inpatient services.1 The quality of mental health care has been shown to be significantly associated with dignity and basic amenities.2 With the serious burden of increasing human immunodeficiency virus infections and acquired immune deficiency syndrome (HIV/AIDS), responsiveness of HIV care is an urgent public health concern.
On the one hand, there are low levels of responsiveness in HIV care. A study from China showed that health care providers did not offer adequate emotional support to HIV patients, whereas nurses could not provide normative HIV care.3 On the other hand, there have been attempts to improve the quality of HIV/AIDS care. Another study suggested that an expert system for HIV voluntary counseling could increase patients’ self-efficacy and knowledge.4 However, HIV patients still suffer from indignity and incompetent service and lack the required social support.
Since 2011, there has been an advocacy of “zero discrimination” to eliminate discrimination and stigmatization.5 However, >50% of people living with HIV/AIDS are still fearful of disclosing their infectious status, while almost 80% are afraid of being blamed and are simply refused health care.6 For HIV patients who bear psychosocial problems such as perceived discrimination, health system responsiveness (HSR) has rarely been addressed in HIV care, especially in China. It is therefore important to compare HSR among HIV and non-HIV patients to meet patients’ needs.
HSR is a promising measure of the quality of a health system and focuses on a health care system’s ability to satisfy patients’ expectations in terms of nonfinancial aspects of health care and nonclinical health domains such as dignity, confidentiality, autonomy, prompt attention, the quality of basic amenities, social support, and choice of provider.7 It may promote the use of services8,9 and ultimately promote health. One study from Ethiopia found that HSR was independently associated with satisfaction of HIV care,10 while another study suggested that HSR was related to increasing visit adherence.11 Some domains of HSR such as prompt attention, communication, and autonomy were identified as priority areas to improve responsiveness of health care services.12,13 However, these studies did not compare differences of HSR between HIV and non-HIV patients. Our previous study showed that the expectations of HIV patients among the eight domains were lower than that of non-HIV patients, and the assessment of HSR based on HIV patient’s perceptions may give biased results toward the quality of HIV services.14 Thus, studies are needed to compare differences in HSR based on patients’ experience of health care service simultaneously.
The self-rated behavior of HSR is systematically biased by demographic, socioeconomic, or cultural factors. A challenge to comparing self-reported responsiveness results is known as “reporting behavior heterogeneity,”15 “differential item functioning (DIF),”16 and “response category cut-point shift.”17 Anchoring vignettes have been proposed to address these problems.17–19 Although anchoring vignettes have been applied to HSR in different settings,20,21 it has not been used to assess HSR across HIV and non-HIV patients to measure the equity of outpatient services.
The main aim of this study was therefore to compare experiences of HSR between HIV and non-HIV patients. It is well known that the two groups are different in terms of socioeconomic status (SES) and expectations on HSR. Thus, the comparison will be adjusted for these two factors.
Methods
Study setting and design
A cross-sectional study was conducted in infectious departments of two large hospitals in Kunming, Yunnan province, China. These two hospitals have the largest number of admissions of HIV and non-HIV-infectious patients in Yunnan.14
Subjects
Eligible patients in this study were HIV and non-HIV inpatients and outpatients aged ≥15 years by consecutive sampling.14 By arrangement of the hospitals, the majority of non-HIV-infectious patients were hepatitis patients. HIV patients with tuberculosis were excluded as they received different services from ordinary non-HIV health care. Those who could not communicate in Mandarin or were too ill to be interviewed were also excluded. Consecutive sampling was used to recruit study subjects.14
Sample size
Sample size estimation used the formula for comparing two population proportions. The percentages of patients who rated the communication domain as “good” among HIV and non-HIV patients in a pilot study were 53% and 61%, respectively. The number of subjects needed to detect a difference of 8% in the proportion of rating communication as “good” between the two groups, with 95% confidence and 80% power, would be 625 per group. To compensate for an estimated 10% nonresponse rate, the sample size was increased to 694 per group.
Development and modification of vignettes
The vignettes were developed and modified which was adopted from World Health Organization in accordance with our previous study.14 Figure 1 shows the framework of HSR in seven domains, with an example vignette shown for communication.
  | Figure 1 Framework of HSR, vignette example, and vignette ordering by investigators. |
Study variables and measurements
The dependent variable was the self-rated experience of HSR in seven domains. The main independent variable was HIV status confirmed by Western blot test. Demographic and socioeconomic variables collected included age, gender, ethnicity, religious affiliation, place of residence, marital status, family size, education, occupation, and household income, which measurements were in consistent with our previous study.14 Among them, occupation, education, and income were on conventionally reflecting SES.
Data collection
HSR data were collected from 1 January to 15 February 2015. The team of interviewers consisted of the main research investigators, HIV/AIDS specialists, and local medical students. Prior to data collection, all interviewers were given training based on concepts of HSR, dimensionality of each domain, meaning of each vignette, common symptoms of HIV/AIDS, psychological support, and investigation skills and protocol for emergency situations. Eligible patients were interviewed face-to-face using an individual questionnaire. Among them, experiences of HSR were self-reported, whereas vignettes were read by the investigators. Each patient was given a gift valued at 10 RMB as compensation for their time.
Statistical methods
B-scale computation
B-scale computation is an approach that was used to calculate the proportions of HSR’s experiences adjusted for expectations by vignettes. B-scale is set as the scale of self-assessments relative to vignettes in a nonparametric setting.22
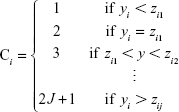
Let yi be the HSR of the self-assessment and zi1,…, ziJ be vignettes (1−J) for the ith respondent. With successively ordered ranks (zj–1<zj, for j=2, …, J) to each respondent on all vignettes, we created the DIF-corrected self-assessment Ci:
|
Values of C that are intervals represent the set of inequalities. Under two assumptions of response consistency and vignette equivalence, the C-scale is used to ensure credible comparisons.22
Based on the same method as the C-scale, a B-scale was built. The difference between these scales lies in information that exists when a self-grading response is tied with the grading of an anchoring object, yi=vij. The C-scale makes strict comparisons with adjacent rank orderings.23 The B-scale states less information in the occurrence of a tie, represented as a set of B-scale values rather than a single index value.23 If yi=vi1, then Bi={1, 2}, if yi=vi2, then Bi={2, 3}. The advantage of the B-scale is that it does not rely on cut-point locations and as a result provides credible comparisons without the requirement of interval equivalence or vignette equivalence.23
Vignette ordering
The ordering of the vignettes is important before the construction of the B-scale. It is normally chosen by the researchers and also possible to draw upon a consensus ordering by the respondents, so long as only one ordering is used for all respondents in the analysis.22 However, differences between hypothesized ordering by the researchers and the consensus ordering may be used for diagnosing problems in the survey instruments, particularly when translating the questions for use in different languages.22 Thus, we confirmed vignette ordering for the construction of B-scales and censored ordered probit regression (COPR) models.
Data analysis
The comparison of sample characteristics between HIV-positive and non-HIV patients was performed using χ2 goodness-of-fit tests for categorical variables.14 Figure 2 shows the subsequent analysis of experience and HSR vignettes. After vignette ordering (Figure 1), the distributions of experience and B-scales of HSR were described, and ordered probit regression models (OPR) and COPR models were conducted. OPR models were constructed separately for each domain to compare differences of self-reported experiences of HSR between HIV and non-HIV patients before and after adjustment of demographic and socioeconomic factors. COPR models were used to compare B-scale values of HSR before and after adjustment of demographic and socioeconomic factors. Variables with a p-value <0.05 were considered as significant. All the analyses were performed using R language and environment with emphasis on the “anchors” package.22,24
  | Figure 2 Framework of measurement and analysis about HSR experience and vignettes. |
Ethical considerations
The study was approved by Prince Songkla University Institutional Review Board and Kunming Medical University.14 Anonymity of the data was assured, and the participants were requested to give their consent to participate by signing an informed consent form, after providing them with detailed information on the study procedures.14 It was approved that subjects aged <18 years could provide the consent by themselves.
Results
Of the 800 consecutive eligible HIV patients approached, 696 (87%) consented to attend the study, while 699 (66%) of the 1,059 non-HIV patients invited agreed to join the study. Most of the HIV patients who refused to participate stated heavy internalized stigma as the reason for not joining, whereas their counterparts refused mainly because they thought that the study was not relevant to them.
Demographic and socioeconomic characteristics
Majority of both groups of patients were male, of Han ethnicity, married or cohabiting, and employed and had no religious affiliation. About half achieved a junior high school level of education, had a monthly household income of ≤5,000 RMB and were living in a family of two to four members. Both groups were closely matched on gender; however, HIV-positive patients were more likely to belong to a minority ethnicity; have a religious affiliation; live in a rural area; have a higher education level; be separated, divorced, or widowed; have a lower household income; live with fewer family members; and be self-employed.
Clinical characteristics
Table 1 presents the clinical characteristics of HIV patients. The route of HIV transmission among HIV-positive patients was mainly via unprotected sexual contact, accounting for 77.7%. The majority of them were at clinical stage 1, were not tested for virus load, and missed their antiretroviral therapy (ART) dose in the last 7 days. In almost 90% of the patients, the CD4 count was <500 cells/μL, and the majority were followed up between two and four times in the first 3 months after confirmation of HIV/AIDS. The median virus load was 89,377.5 copy/mL among those who were tested, and the median number of days between HIV diagnosis and receiving the first dose of ART was 293. The majority of non-HIV patients had hepatitis (85.7%).
  | Table 1 Clinical status among HIV-positive patients |
Experience of HSR among HIV and non-HIV patients
Table 2 shows the distribution of experiences of HSR among HIV and non-HIV patients. The majority of HIV patients perceived having a “good” experience in all seven HSR domains. Majority of non-HIV patients perceived having a “good” experience in three HSR domains: prompt attention, dignity, and communication, while four domains were perceived as “moderate”: quality of basic amenities, confidentiality, choice, and autonomy. The difference of proportional trends from the OPR models were significant in all domains except for prompt attention, indicating that non-HIV patients were more likely to have a worse experience for these six HSR domains. After adjustment for sociodemographic factors, the differences were still significant among the same six HSR domains.
Experience of HSR after adjusting for vignettes among HIV and non-HIV patients
Table 3 presents B-scale values between self-rated HSR and vignettes in seven domains. B-values ranged from 1 to 6, since there were five vignettes, reflecting more than “very good” to less than “very bad.” Among HIV patients, the highest probabilities mainly concentrated around B-values of 2 reflecting experiences between “very good” and “good” for four domains: prompt attention, dignity, communication, and confidentiality. The highest probabilities of basic amenities and autonomy domains had B-scale values of 3 reflecting experiences between “good” and “moderate” and 1 reflecting experiences more than “very good.” In contrast, the experience of HSR after adjusting for vignettes among non-HIV patients was generally lower than that among HIV patients. The differences of rank probabilities were significant in all seven domains before and after adjusting for sociodemographic factors. In prompt attention, non-HIV patients were less likely to have a worse experience than HIV patients. However, non-HIV patients were more likely to have a worse experience than HIV patients in dignity, communication, quality of basic amenities, confidentiality, choice of providers, and autonomy domains.
Discussion
HIV patients had better experiences about self-rated HSR in six HSR domains, prompt attention being the only exception, after adjustment for demographic and socioeconomic factors. After adjusting for anchoring vignettes, HIV patients still had better perceptions of experiences about HSR in these six domains. Compared with OPR models with no adjustment for vignettes, all the coefficients reduced in COPR models, reflecting more narrow and valid differences among HIV and non-HIV patients.
Perceptions about experience among HIV patients were better than those of their non-HIV counterparts in six domains such as dignity, communication, quality of basic amenities, confidentiality, choice of provider, and autonomy. Many studies among HIV patients showed “logistic choices” to providers or hospitals and lack of dignity without admiration for individual autonomy as medical participation and self-decisions in HIV care.25,26 HIV patients kept more appointments when treated with dignity and patient-centered communication because of communication preferences and patient satisfaction.27,28 Conversely, one study showed that HIV patients were highly satisfied with pharmaceutical services.29 A possible explanation for the finding that HIV patients perceived better HSR than non-HIV patients in this study may reflect the successful evolvement of HIV care in the country. Good care given to HIV patients, good treatment efficacy of highly active ART, and the integration of community and public HIV services30,31 are part of an attempt to control the spread of HIV. HIV prevention has steadily been supported first by internal findings such as Global Fund and has recently become internalized.32 Studies in China recently focused on a scaling-up to increase the number of individuals knowing their HIV status and improving access to HIV-related services.33,34 However, non-HIV health care is overwhelmed by several problems including inequalities of health care utilization and high out-of-pocket payments due to high workloads and inadequate budgets.35,36 In 2012 in China, the wealthiest 20% of the rural and urban populations contributed 49.7% and 55.8% of the total health expenditure, respectively, while the poorest 20% contributed only 4.7% and 4.4%, respectively.37 This finding indicates a need to improve care for ordinary patients in general.
However, HIV patients had worse perceptions about experience of prompt attention compared with their counterparts. There has been no previous study comparing the experience of HSR between HIV and non-HIV patients. One study in South Africa showed that prompt attention had the lowest degree of perceived responsiveness among older adults admitted to hospital.12 Prompt attention may be seen as a priority domain to improve HSR. There is probably a shortage of human resources and an efficient mechanism to allow health personnel to uniformly cooperate with each other in HIV/AIDS care.38,39
Therefore, it may be to promote commonization,40 which, on the one hand, guarantees HIV care and improves ordinary health care service, on the other hand. In other words, it may be better to integrate HIV services into routine care sharing the same medical resources and education.
Anchoring vignettes were used to narrow the differences in perceptions of HSR experiences between HIV and non-HIV patients, thus controlling for patients’ own expectations. Our results are consistent with a study by Grol-Prokopczyk et al,41 indicating that using anchoring vignettes to adjust for self-rated HSR is valid. Our vignettes were comprehensible to the patients and showed minimal violation of the assumptions. Thus, using anchoring vignettes may be a valid method to measure perceptions of HSR to control for DIF to avoid incorrect research findings.
There are certain limitations in our study. First, a poorer response rate among the non-HIV group may affect the internal validity of the study.42 However, this imbalance was in the same direction of the main results in which non-HIV patients perceived poorer HSR. Despite the findings in favor of HIV care, the generalizability of this study is still limited because the data were collected from only two hospitals in one province of China.
Conclusion
Perceptions about experiences of HSR were better among HIV patients than among non-HIV patients in all domains except for prompt attention, even after adjusting for differences in socioeconomic indicators and patients’ own expectation. Commonization or integrating HIV care into the ordinary health care should be considered to improve the quality of care as a whole. A research on management trial should be initiated.
Acknowledgments
The survey was supported by Yunnan Applied Basic Research Projects – Union Foundation (2017FE467[-011]) and National Natural Science Foundation of China (81760617). They both were not involved in the study design; collection, analysis, or interpretation of data; writing of the manuscript; or decision to submit the paper for publication.
Disclosure
The authors report no conflicts of interest in this work.
References
Tang S, Meng Q, Chen L, Bekedam H, Evans T, Whitehead M. Tackling the challenges to health equity in China. Lancet. 2008;372(9648):1493–1501. | ||
Peng D, Li XS, Zhang Q, et al. [Responsiveness evaluation of mental intervention services system in Wenchuan earthquake area]. Zhonghua Yu Fang YiXxue Za Zhi. 2011;45(2):158–162. Chinese. | ||
Chen WT, Shiu CS, Simoni J, Fredriksen-Goldsen K, Zhang F, Zhao H. Optimizing HIV care by expanding the nursing role: patient and provider perspectives. J Adv Nurs. 2010;66(2):260–268. | ||
Chai J, Wang D, Zhou M, Xu W, Liang G, Shen YF. Developing and piloting an expert system for better routine voluntary HIV counseling and testing in China: preliminary results and lessons. AIDS Care. 2012;24(4):424–433. | ||
Haghdoost A, Karamouzian M. Zero new HIV infections, zero discrimination, and zero AIDS-related deaths: feasible goals or ambitious visions on the occasion of the world AIDS day? Int J Prev Med. 2012;3(12):819–823. | ||
Institute of Social Development Research, China Central Party School. The China Stigma Index report. UNAIDS. Marie Stopes Internatinal China; 2009. Available from: https://wenku.baidu.com/view/6a2d141ca300a6c30c229f40.html?rec_flag=default&mark_pay_doc=0&mark_rec_page=1&mark_rec_position=2&mark_rec=view_r_1&clear_uda_param=1&sxts=1528292667492###. Accessed June 7, 2018. | ||
Bleich SN, Özaltin E, Murray CK. How does satisfaction with the health-care system relate to patient experience? Bull World Health Organ. 2009;87(4):271–278. | ||
Anand S, Sinha R. Quality differentials and reproductive health service utilisation determinants in India. Int J Health Care Qual Assur. 2010;23(8):718–729. | ||
Bhanderi MN, Kannan S. Untreated reproductive morbidities among ever married women of slums of Rajkot City, Gujarat: the role of class, distance, provider attitudes, and perceived quality of care. J Urban Health. 2010;87(2):254–263. | ||
Yakob B, Purity Ncama B. Client satisfaction: correlates and implications for improving HIV/AIDS treatment and care services in southern Ethiopia. Int Health. 2016;8(4):292–298. | ||
Miller JS, Mhalu A, Chalamilla G, et al. Patient satisfaction with HIV/AIDS care at private clinics in Dar es Salaam, Tanzania. AIDS Care. 2014;26(9):1150–1154. | ||
Peltzer K, Phaswana-Mafuya N. Patient experiences and health system responsiveness among older adults in South Africa. Glob Health Action. 2012;5:1–11. | ||
Peltzer K. Patient experiences and health system responsiveness in South Africa. BMC Health Serv Res. 2009;9:117. | ||
Li J, Assanangkornchai S, Lu L, et al. Can socio-economic differences explain low expectation of health services among HIV patients compared to non-HIV counterparts? BMC Public Health. 2016;16:955. | ||
Murray CJ, Kawabata K, Valentine N. People’s experience versus people’s expectations. Health Aff (Millwood). 2001;20(3):21–24. | ||
King G, Murray CJL, Salomon JA, Tandon A. Enhancing the validity and cross-cultural comparability of measurement in survey research. Am Polit Sci Rev. 2004;98(1):191–207. | ||
Murray CJ, Tandon A, Salomon JA, Mathers CD, Sadana R. Cross-population comparability of evidence for health policy. In: Health Systems Performance Assessment: Debates, Methods and Empiricism; 2003:705–713. | ||
King G, Wand J. Comparing incomparable survey responses: evaluating and selecting anchoring vignettes. Polit Anal. 2007;15(1):46–66. | ||
Tandon A, Murray CJ, Salomon JA, King G. Statistical models for enhancing cross-population comparability. In: Health Systems Performance Assessment: Debates, Methods and Empiricism. Geneva: World Health Organization; 2003:727–746. | ||
Valentine N, Verdes-Tennant E, Bonsel G. Health systems’ responsiveness and reporting behaviour: multilevel analysis of the influence of individual-level factors in 64 countries. Soc Sci Med. 2015;138:152–160. | ||
Rottger J, Blumel M, Fuchs S, Busse R. Assessing the responsiveness of chronic disease care – is the World Health Organization’s concept of health system responsiveness applicable? Soc Sci Med. 2014;113:87–94. | ||
Wand J, King G, Lau O. Anchors: software for anchoring vignette data. J Stat Softw. 2011;42(3):1–25. | ||
Wand J. Credible comparisons using interpersonally incomparable data: Nonparametric scales with anchoring vignettes. Am J Polit Sci. 2013;57(1):249–262. | ||
Chongsuvivatwong V. Analysis of Epidemiological Data using R and Epicalc: Songkhla: Prince of Songkla University; 2008. | ||
Ho AH, Leung PP, Tse DM, et al. Dignity amidst liminality: healing within suffering among Chinese terminal cancer patients. Death Studies. 2013;37(10):953–970. | ||
Gattellari M, Voigt KJ, Butow PN, Tattersall MH. When the treatment goal is not cure: are cancer patients equipped to make informed decisions? J Clin Oncol. 2002;20(2):503–513. | ||
Flickinger TE, Saha S, Moore RD, Beach MC. Higher quality communication and relationships are associated with improved patient engagement in HIV care. J Acquir Immune Defic Syndr. 2013;63(3):362–366. | ||
Mulder BC, van Lelyveld MA, Vervoort SC, et al. Communication between HIV patients and their providers: a qualitative preference match analysis. Health Commun. 2016;31(1):35–46. | ||
Okoye MO, Ukwe VC, Okoye TC, Adibe MO, Ekwunife OI. Satisfaction of HIV patients with pharmaceutical services in South Eastern Nigerian hospitals. Int J Clin Pharm. 2014;36(5):914–921. | ||
Zheng JL, Xu Y, He L, et al. [Analysis on antiretroviral therapy efficacy for HIV/AIDS in Zhejiang province, 2009–2014]. Zhonghua Liu Xing Bing Xue Za Zhi. 2016;37(5):673–677. Chinese. | ||
Cheng W, Cai Y, Tang W, et al. Providing HIV-related services in China for men who have sex with men. Bull World Health Organ. 2016;94(3):222–227. | ||
Minghui R, Scano F, Sozi C, Schwartlander B. The Global Fund in China: success beyond the numbers. Lancet Glob Health. 2015;3(2):e75–e77. | ||
Chen J, Yu B, Wang Y, et al. Expansion of HIV care and treatment in Yunnan Province, China: treatment outcomes with scale up of combination antiretroviral therapy. AIDS Care. 2014;26(5):633–641. | ||
Li G, Liang S, Harrison TJ, et al. Prevalence of transmitted HIV-1 drug resistance remains low in Guangxi, China, eight years after scale-up of highly-active antiretroviral therapy. Intervirology. 2014;57(5):270–276. | ||
Zhang X, Wu Q, Shao Y, Fu W, Liu G, Coyte PC. Socioeconomic inequities in health care utilization in China. Asia Pac J Public Health. 2015;27(4):429–438. | ||
Hu S, Tang S, Liu Y, Zhao Y, Escobar ML, de Ferranti D. Reform of how health care is paid for in China: challenges and opportunities. Lancet. 2008;372(9652):1846–1853. | ||
Wang L, Wang A, Zhou D, FitzGerald G, Ye D, Jiang Q. An empirical analysis of rural-urban differences in out-of-pocket health expenditures in a low-income society of China. PLoS One. 2016;11(5):e0154563. | ||
Anand S, Fan VY, Zhang J, et al. China’s human resources for health: quantity, quality, and distribution. Lancet. 2008;372(9651):1774–1781. | ||
Li L, Lin C, Wu Z, et al. Stigmatization and shame: consequences of caring for HIV/AIDS patients in China. AIDS Care. 2007;19(2):258–263. | ||
Oleribe OO, Oladipo O, Osita-Oleribe P, et al. Commonization of HIV/AIDS services in Nigeria: the need, the processes and the prospects. Pan Af Med J. 2014;19:329. | ||
Grol-Prokopczyk H, Freese J, Hauser RM. Using anchoring vignettes to assess group differences in general self-rated health. J Health Soc Behav. 2011;52(2):246–261. | ||
Li J, Assanangkornchai S, Lu L, et al. Development of internalized and personal stigma among patients with and without HIV infection and occupational stigma among health care providers in Southern China. Patient Prefer Adherence. 2016;10:2309–2320. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.