Back to Journals » Drug Design, Development and Therapy » Volume 17
Comparison of Dural Puncture Epidural, Epidural and Combined Spinal-Epidural Anesthesia for Cesarean Delivery: A Randomized Controlled Trial
Authors Rao WY, Xu F, Dai SB, Mei Z , Chen XP, Lv CC, Liu CL, Ngan Kee W, Chen XZ
Received 30 April 2023
Accepted for publication 7 July 2023
Published 18 July 2023 Volume 2023:17 Pages 2077—2085
DOI https://doi.org/10.2147/DDDT.S415684
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Georgios Panos
Wan-Yi Rao,1,* Fang Xu,1,* Shao-Bing Dai,1 Zhong Mei,2 Xiao-Ping Chen,1 Chang-Cheng Lv,1 Chun-Lei Liu,1 Warwick Ngan Kee,1 Xin-Zhong Chen1
1Department of Anesthesia, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, People’s Republic of China; 2Department of Anesthesiology, Affiliated Xiaoshan Hospital, Hangzhou Normal University, Hangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xin-Zhong Chen, Department of Anesthesia, Women’s Hospital, Zhejiang University School of Medicine, No. 1 Bachelor’s Road, Hangzhou, 310000, People’s Republic of China, Email [email protected]
Purpose: Catheter-based techniques such as combined spinal-epidural (CSE) anesthesia which are sometimes indicated for obstetric anesthesia have a complex mechanism of action. The application of the dural puncture epidural (DPE) anesthesia for cesarean section (CS) has not been well investigated. The present study compared the relatively novel DPE technique with epidural (EA) and CSE anesthesia.
Patients and Methods: We randomly assigned 150 parturients who underwent elective CS to receive DPE, EA or CSE anesthesia. The primary outcome was the onset of sensory anesthesia to the T5 dermatome assessed using the Cox proportional hazards model. Secondary outcomes included median time to sensory block, quality of block, patient and surgeon satisfaction, APGAR scores and other side effects.
Results: For DPE anesthesia versus EA anesthesia, the onset of anesthesia was faster (hazard ratio 2.47 [95% CI 1.56 to 3.90], adjusted P < 0.001) and the median time to surgical level was shorter (16 [IQR 14– 18] min versus 19 [15.5– 21] min, adjusted P < 0.001); the incidence of intraoperative pain was lower (7/48 versus 17/47, adjusted P = 0.046) and the median patient satisfaction score was higher (9 [IQR 9– 10] versus 8 [8– 9.5], adjusted P = 0.004). In the CSE group, the onset of anesthesia was faster than in the other two but the incidence of hypotension was higher (P < 0.001) and the phenylephrine requirement was greater (P < 0.001).
Conclusion: DPE anesthesia had a faster onset and better quality of block than EA anesthesia and provided less influence to maternal hemodynamic parameters than CSE anesthesia for CS. These results suggest that the dural puncture plays a significant role in enhancing the effectiveness of epidural top-ups during CSE anesthesia and indicates enlightenment that contributes to the satisfaction of anesthetic effect in DPE technique labor analgesia transferred to CS.
Keywords: anesthesia, dural puncture epidural, anesthesia, epidural, cesarean section
Introduction
An ideal neuraxial anesthesia technique should provide effective pain elimination, with minimal adverse effects for both maternal and fetal. The epidural anesthesia (EA) technique can sometimes result in slow onset and inadequate spread of anesthesia to the sacral area, as well as unilateral or patchy sensory blockade, motor impairment, and epidural catheter failure.1 On the other hand, the combined spinal-epidural (CSE) technique involves the direct injection of local anesthetics into the cerebrospinal fluid surrounding the spinal nerves. This technique has gained popularity due to its reliable speed of onset and ability to reduce the number of unblocked segments compared to the conventional EA technique. However, these advantages must be balanced with the risk of potential hemodynamic instability, supine hypotensive syndrome, fetal bradycardia, and other side effects.2 It is important to note that neuraxial anesthesia techniques are not limited to EA or CSE blocks. The dural puncture epidural (DPE) technique is a relatively new innovation that is technically similar to CSE anesthesia but involves no administration of intrathecal drugs.3 It has been well described for labor analgesia, where the dural puncture is believed to enhance certain aspects of pain relief, such as a faster onset and reduction in unblocked segments compared to the conventional EPL (epidural labor analgesia) technique.4–6 However, the potential applicability of these advantages to anesthesia for cesarean delivery remains unknown, particularly in conversion from labor analgesia to surgical anesthesia for CS, or when the initial intrathecal dose does not result in an adequate block.
The present study compared the DPE, EA and CSE techniques for elective CS. The primary outcome analyzed was the onset of anesthesia. The main focus was the difference between DPE and EA anesthesia, and CSE anesthesia included as an active (positive) comparator. We considered that our findings would provide insight into the mechanism of CSE anesthesia as well as preliminary evidence for the possible consideration of DPE as a potential option for anesthesia for CS.
Materials and Methods
Ethical approval for this study (no. 20190024) was provided by the Ethical Review Board of Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, China on April 4, 2019, and the study was registered prior to patient enrolment in the Chinese Clinical Trial Registry (http://www.chictr.org.cn/enindex.aspx) (registration no: ChiCTR1900023107, registration date: May 11, 2019). After written informed consent was obtained, we recruited 150 American Society of Anesthesiologists physical status II parturients with singleton pregnancies scheduled for elective CS at term. Exclusion criteria included (1) maternal diseases (ie, diabetes, hypertensive disorder, preeclampsia and eclampsia, cardiovascular or cerebrovascular disease, placenta previa or placental abruption); (2) contraindications to neuraxial anesthesia, including allergies to anesthetics, abnormal coagulation function, anticoagulant therapy, severe hypovolemia, or hemodynamic instability; (3) previous mental illness or other systemic diseases of important organs; (4) body height <150 cm or >170 cm and body mass index (BMI) >30 kg/m2. All participants were recruited in the present study from May 2019 until April 2022.
This study was conducted between February and December 2022 at the Department of Anesthesia, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, China. We randomly assigned parturients to one of the three groups with different catheter-based anesthesia techniques: the DPE group, the EA group or the CSE group (n = 50 per group). Randomization was performed by a research assistant who was not involved with subsequent data collection using computer-generated random numbers (Microsoft Excel, Microsoft Corporation, Redmond, WA, USA). Randomization codes were concealed in numbered, sealed opaque envelopes, one of which was opened for each parturient after informed consent and recruitment.
No premedication was given. Upon arrival in the operating room, we positioned each patient supine with left uterine displacement, inserted an 18-gauge intravenous cannula into a forearm vein and commenced an infusion of 37°C Ringer’s lactate solution at a rate of 5 mL/kg/h. Standard monitoring included automated non-invasive arterial blood pressure (BP), pulse oximetry (SpO2), and electrocardiography (ECG). After a short resting period, baseline measurements of BP and heart rate were recorded as the mean of three consecutive values recorded at 3-min intervals.
All patients had an epidural catheter placed while in the left lateral position. Under local anesthesia, we inserted a 16-gauge Tuohy needle at the estimated L2-L3 vertebral interspace using a midline approach and a loss-of-resistance to saline technique. We then inserted a nylon multiport catheter (AS-E; Lüjian Medical Ltd, Haining, China) 3 cm into the epidural space through the Tuohy needle with the orifice of the needle orientated cephalad, and the catheter was fixed to the skin with a strip of dressing.
In the EA group, after epidural catheter placement we returned the parturients to the tilted supine position. We then injected a test dose of 3 mL of lidocaine 1.5% via the epidural catheter. Three minutes later, after excluding signs of intravascular or intrathecal injection, we injected a total of 18 mL of ropivacaine 0.75% in 6-mL increments every 1.5 min through the epidural catheter.
In the CSE group, after epidural catheter placement, we inserted a 25-gauge Whitacre spinal needle under local anesthesia at the vertebral interspace one level caudad to the epidural puncture level (estimated L3-L4 vertebral interspace). Entry into the intrathecal space was confirmed by observation of free flow of cerebrospinal fluid (CSF). We then injected 3 mL of ropivacaine 0.5% (15 mg) intrathecally at a speed of 1 mL per 10 s. Immediately after completion of intrathecal injection, the spinal needle was removed and we returned the parturients to the tilted supine position.
In the DPE Group, after epidural catheter placement, we inserted a 25-gauge Whitacre spinal needle in exactly the same way as in the CSE group. However, after observing free flow of CSF, the needle was removed without the injection of any drug. We then returned the parturients to the tilted supine position and administered a lidocaine test dose and ropivacaine 0.75% epidurally to establish surgical anesthesia in exactly the same way as in the EA group.
To facilitate blinding, all neuraxial procedures were performed by the same anesthesiologist. This individual was not involved in subsequent patient management and data collection. Patient management was performed by a separate investigator, and the data collection was performed by an assistant.
We measured the sensory blockade bilaterally starting after the completion of injection of the 18 mL of ropivacaine 0.75% epidurally in the EA and DPE groups or the 3 mL of ropivacaine 0.5% intrathecally in the CSE group (time zero); this was done at 2-min intervals for the first 20 min and then at 5-min intervals until the end of the surgery by assessing the loss of discrimination to pinprick stimulus starting at the S2 dermatome and moving cephalad in the anterior axillary lines and then caudad. If sensory block to the T5 dermatome was not achieved by 15 min after the initial local anesthetic dose, we injected additional 3 mL boluses of ropivacaine 0.75% at 5-min intervals as required until a block to the T5 dermatome was achieved.
We recorded the interval from the completion of the initial epidural or intrathecal local anesthetic injection (time zero) to the time when the sensory block reached the T5 dermatome (time of surgical block). Surgery was permitted to start after a sensory block level at the T5 dermatome was achieved. We also recorded the highest dermatomal level of block achieved.
We assessed motor block using a modified Bromage scale (0 = full flexion of knees and ankles, 1 = partial flexion of knees, full flexion of ankles, 2 = inability to flex knees, partial flexion of ankles, 3 = inability to flex knees and ankles) at 5-min intervals for 30 min after completion of the initial epidural or intrathecal local anesthetic injection.
We monitored SpO2 and heart rate continuously. We set the BP monitor to cycle at 2-min intervals from the start of anesthesia for 20 min, and then at 5-min intervals until the end of surgery. Hypotension was defined as a decrease in systolic BP to <90 mmHg or <80% of the baseline value, and it was treated with a rapid infusion of lactated Ringer’s solution and i.v. boluses of phenylephrine 20 to 40 μg. Bradycardia was defined as a heart rate <50 beats/min and was treated with i.v. boluses of atropine 0.5 mg. We recorded the incidence of hypotension, nausea, vomiting, and intraoperative pain which was measured on a 10-cm visual analogue scale (VAS) (0 = no pain, 10 = worst pain imaginable). Intraoperative pain (VAS ≥ 3) was treated with intravenous boluses of 30 mg ketamine when the sensory block level was T5 or above, or treated with epidural boluses of 3 mL ropivacaine 0.75% if the sensory block level was below T5. Fetal Apgar scores at 1 min and 5 min were also documented.
At the end of surgery, we measured satisfaction scores from the patient and surgeon using a VAS (0 = completely dissatisfied and 10 = completely satisfied) scale. The following parameters were also assessed: time to remove the urinary catheter, time of Bromage score return to 0 and postoperative pain VAS scores (0 = no pain, 10 = worst pain imaginable) (6 h and 24 h).
For postoperative analgesia, we injected preservative-free morphine 2 mg in a volume of 3 mL through the epidural catheter at the end of the surgery and in addition provided intravenous patient-controlled intravenous analgesia (PCIA) using sufentanil 0.5 μg/mL and butorphanol 80 μg/mL. All participants were visited on the 1st, 2nd and 3rd postoperative days to check for any adverse effects of the neuraxial anesthesia such as postdural puncture headache, nausea, vomiting and back pain.
Statistical Analysis
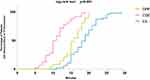
The primary outcome of the study was defined as the speed of onset of sensory anesthesia to the T5 dermatome between the DPE and EA groups. For this comparison, we chose to apply time-to-event (survival) analysis; onset of anesthesia was displayed using Kaplan–Meier survival curves and comparisons between groups were performed using the Cox proportional hazards model. We initially performed a small preliminary pilot investigation on 10 patients to acquire background information on which to base a sample size calculation. This showed a hazard ratio (HR) of 3 when comparing the DPE and EA techniques for the time to sensory anesthesia to the T5 dermatome. We then performed power analysis using PASS version 11.0.7 (NCSS, LLC, Kaysville, UT, USA) which showed that to detect a constant HR of 3.0 in time to sensory block to the T5 dermatome between the groups with 90% power (two-tailed) with a significance level of 0.05, 42 subjects in total (21 per group) were needed. We arbitrarily increased the sample size to 50 per group (150 total in three groups) to allow for possible dropouts and to increase the power of the study to account for the possibility that the true HR might be less than 3.0. Secondary outcomes included comparisons of the absolute time taken to achieve sensory block to the T5 dermatome, highest sensory block level achieved, the presence of a motor block, the incidence of an intraoperative VAS pain score ≥3, the incidence of hypotension, and phenylephrine requirement, Apgar scores, and maternal satisfaction.
Continuous data were tested for normality using the Shapiro–Wilk test. Normally distributed data were analyzed among the groups using one-way analysis of variance (ANOVA) followed by post-hoc pairwise comparisons for significant results. Non-normally distributed data were analyzed using the Kruskal–Wallis test with Dunn’s tests for post-hoc pairwise comparisons. Categorical data were analyzed using the chi-square test with application of Yates correction when the expected number in one or more cells was ≤5. Values of P < 0.05 were considered statistically significant, with Bonferroni adjustments applied to multiple pairwise comparisons. Statistical analysis was performed using SPSS Statistics for Windows version 24.0 (IBM Corp., Armonk, NY, USA) and GraphPad Prism version 8.0 (GraphPad Software Inc., San Diego, CA, USA).
Results
The participant flow is shown in Figure 1, and the patient characteristics are summarized in Table 1. Among a total of 195 patients assessed for eligibility, 150 entered the study and were randomized. Of these, five cases were excluded from the study: two cases in the DPE group because of failure to identify the CSF after insertion of the spinal needle, two cases in the EA group because a low fetal heart rate detected during the epidural procedure necessitated urgent delivery under general anesthesia, and one case in the EA group who had symptoms of suspected local anesthetic toxicity (dizziness, aural symptoms, a transient increase in heart rate and decrease in BP, and a decrease in fetal heart rate to <100 beats/min) and also proceeded to have general anesthesia for delivery. Block characteristics and pain score, maternal adverse effects and fetal outcome assessment are summarized in Table 2.
 |
Table 1 Patient Characteristics |
 |
Table 2 Characteristics of Anesthesia |
 |
Figure 1 Study flow diagram. BMI: body mass index. DPE: dural puncture epidural. Abbreviations: CSE, combined spinal-epidural; EA, epidural anesthesia; CSF, cerebrospinal fluid. |
The results for the primary outcome showed that the onset of anesthesia was significantly faster in the DPE group than in the EA group (HR 2.47 [95% CI 1.56 to 3.90], adjusted P < 0.001) (Figure 2). Further analysis showed that the onset of anesthesia was faster in the CSE group compared with both the DPE group (HR 2.99 [95% CI 1.95 to 4.58], adjusted P < 0.001) and the EA group (HR 6.13 [95% CI 3.70 to 10.16], adjusted P < 0.001). The time required to achieve a sensory anesthesia to the T5 dermatome is shown in Table 2. There was a significant difference between groups (P < 0.001); post-hoc pairwise comparisons showed that time to achieve sensory anesthesia to the T5 dermatome was shorter for the CSE group versus both the DPE group (adjusted P < 0.001) and EA group (adjusted P < 0.001) and for the DPE group versus the EA group (adjusted P < 0.001).
The number of supplementary epidural top-ups required was higher in the EA group than in the DPE group (adjusted P < 0.001) and the CSE group (adjusted P < 0.001). The highest recorded level of sensory anesthesia was similar between the groups. The bromage score at 15 min was greater in the CSE group than in the DPE (adjusted P < 0.001) and the EA group (adjusted P < 0.001). Patient satisfaction was greater in the DPE group versus the EA group (adjusted P = 0.004). Surgeon satisfaction was greater in the DPE group versus the EA group (adjusted P = 0.007) and in the CSE group versus the EA group (adjusted P = 0.004).
Intraoperatively, the incidence of hypotension was different between groups and was greater in the CSE group (29/50) versus the DPE group (7/48) (adjusted P < 0.001) and versus the EA group (6/47) (adjusted P < 0.001) with no difference between the DPE and EA groups (adjusted P = 1). Similarly, the requirement for phenylephrine was different between groups (P < 001) and was greater in the CSE group (median 20 [IQR 0–40] µg) versus the DPE group (0 [0–0]µg) (adjusted P < 0.001) and versus the EA group (0 [0–0] µg) (adjusted P < 0.001) with no difference between the DPE and EA groups (adjusted P = 1). No patient required atropine for bradycardia. The number of patients who had an intraoperative VAS pain score ≥3 was different among groups (P = 0.003) and was greater in the EA group (17/47) versus both the DPE group (7/48) (adjusted P = 0.046) and the CSE group (5/50) (adjusted P = 0.006) with no difference between the DPE and CSE groups (adjusted P = 1).
There were no significant differences among the three groups in the occurrence of intraoperative nausea or vomiting, neonate Apgar score at 1 and 5 min, and maternal satisfaction. There were no postpartum headaches, neurological complications or other postoperative complications happened in any group.
Discussion
The main finding of this study was that the DPE technique had a faster onset of anesthesia compared to the conventional EA technique when used for CS. This was supported by the primary outcome, which showed a higher hazard ratio (>1) when comparing the onset of sensory block at the T5 level between the DPE and EA groups. Secondary analyses further demonstrated that the DPE group had a shorter median time to achieve sensory block at the T5 dermatome and required fewer supplementary epidural top-ups compared to the EA group. An additional finding was that there was a lower incidence of intraoperative pain in the DPE group, suggesting a better quality of block compared to the EA group.
Our finding that DPE anesthesia was associated with improved quality of anesthesia compared with EA anesthesia suggests that dural puncture enhances the efficacy of drugs that are subsequently administered epidurally to establish or augment anesthesia for CS. This was suggested in previous studies of the DPE technique for labor analgesia in which dural puncture was thought to enhance passage of epidural drugs across the dura.4,5,7
Epidural analgesia is converted to surgical anesthesia by administering high-concentration local anesthetic. Our study is the first to demonstrate that DPE technique yields superior outcomes when compared to EA techniques when administering the same epidural doses for CS. This evidence could contribute to the requirements and consequences of anesthesia management of parturients with DPE delivery analgesia who have to be transferred to CS.
Furthermore, the results of our study provide information that may inform the consideration of DPE as a possible alternative to CSE anesthesia. Although the CSE technique is effective and has advantages over single-shot spinal anesthesia and EA in selected circumstances, previous research has demonstrated that it can result in a higher level of sensory block.8 In contrast, the DPE technique can address this limitation by providing improved hemodynamic stability, especially in patients with cardiac disease or other unstable conditions, or when prolonged surgery is anticipated. In these situations, CSE techniques have become popular because of the ability to use small intrathecal doses of local anesthetic and the option to supplement anesthesia with epidural top-ups.9 By extrapolation, we contend that the DPE technique can be considered a subset of the CSE technique in which the intrathecal dose is reduced to zero. Further study is required to confirm the advantages of the DPE technique for anesthesia for CS before it can be recommended for general use.
Our results showed that in the CSE group (positive control) the onset of anesthesia was faster than in both the DPE and EA groups. This is an expected effect of direct intrathecal administration of local anesthetic and probably also accounts for the greater motor block in the CSE group versus the DPE and EA groups. The latter may be the reason for the greater surgeon satisfaction in the CSE group, possibly because of better abdominal muscle relaxation and/or less patient movement.
Our finding that the incidence of intraoperative pain was greater in the EA group than in the CSE group is consistent with the findings of a recent systematic review that showed that spinal and CSE anesthesia are associated with a lower prevalence of inadequate neuraxial anesthesia than EA anesthesia in patients undergoing elective CS.1 An additional finding of our study was the lower incidence of intraoperative pain with the DPE technique compared with the EA technique, which to our knowledge has not been demonstrated previously.
We used a double-space technique, wherein separate intervertebral spaces were employed for inserting the epidural catheter and spinal needle in the DPE and CSE groups. This reflects our institutional experience and equipment availability. However, in most other units, the use of a needle-through-needle technique is likely to be more common. The needle-through-needle technique offers several advantages. Firstly, it reduces the occurrence of epidural catheter misplacement and failure.10 Additionally, it eliminates the potential risk of damaging the epidural catheter when it is placed before the insertion of the spinal needle.11 Moreover, by using the same intervertebral space, it ensures close proximity of the epidural injection site to the dural hole. This proximity can positively impact the passage of drugs through the hole.12 Conversely, the double-space technique may have a higher success rate compared to the needle-through-needle technique.13,14 Further work is required to confirm whether our findings are applicable to a needle-through-needle technique.
In our study, we used a 25-gauge Whitacre spinal needle to perform dural puncture. Previously, when using the DPE technique for labor analgesia, it was shown that the onset was faster when dural puncture was performed with a 25-gauge versus a 27-gauge spinal needle.15 This suggests that the size of the spinal needle may be an important consideration for the DPE technique and, therefore, our results may not be generalizable to the use of spinal needles of sizes other than those used in our study.
One case in this study was excluded from the EA group because of symptoms of possible local anesthetic toxicity that occurred during epidural drug administration. We suspect this may have been caused by inadvertent intravenous placement of the epidural catheter, despite a negative response to the lidocaine test dose. Of note, we used our standard test dose of 3 mL of lidocaine 1.5%. Although controversial,16,17 it is possible that use of an epinephrine-containing test dose may have been a more sensitive method for detecting an intravenous epidural catheter. In keeping with our institutional practice, we used an epidural local anesthetic solution with a relatively high concentration (ropivacaine 0.75%); however, this practice is within international recommendations for epidural anesthesia for CS.18
Finally, our study has several limitations. First, although this study was conducted according to a double-blinded protocol, in reality blinding was not possible to fully achieve. Patients were not informed of the group to which they were assigned but would have been aware of the number and sites of injections in their back. The investigator who assessed the patients after induction of anesthesia was not aware of the anesthesia technique that was used but may have inferred the identity of the group when the CSE technique was used because of the relatively fast onset. Second, our exclusion criteria did not include subjects with a history of abdominal surgery or lumbar anesthesia, which may affect the effectiveness of anesthesia and observation results in maternal. In these parturients, the presence of adhesions and scar tissue in the abdominal area can affect the operation and the need for anesthesia. Similarly, patients with a history of spinal anesthesia or epidural anesthesia may have adhesions or altered anatomy due to the previous needle insertion and medication administration. Scar tissue or changes in the lumbar space canal can affect the spread and effectiveness of subsequent epidural anesthesia. In some cases, it may be more difficult to achieve adequate anesthesia levels or to ensure complete pain relief during the surgery. Third, the intrathecal dose of ropivacaine applied in the present study was relatively lower than that (26.8 mg) reported by Khaw et al.19 However, the dose of intrathecal ropivacaine (15 mg) we used in the present study is more suitable for the Chinese population, which was based on the findings of our previous dose–response study that showed that the ED95 of intrathecal hyperbaric ropivacaine for anesthesia for CS was 15.39 mg.20 Furthermore, the omission of fetal acid-base analysis reports in our study design led to an incomplete assessment of fetal well-being, limited evaluation of fetal distress, and compromised safety evaluation. Additionally, we did not include a lipophilic opioid in the intrathecal solution, which may have resulted in a longer onset time. Although this practice is not commonly followed in some centers, we acknowledge that it is recommended in our institution. Having a large dataset would offer further insight. We hope that future studies will take these factors into account to improve the design and outcomes of similar researches.
Based on our findings, it is plausible to suggest that the DPE technique may be the preferred anesthesia regimen for labor analgesia. This conclusion is supported by the superior analgesic effect observed in parturients who received delivery analgesia, as well as the better anesthetic effect achieved when transitioning to CS. Future research should prioritize the compatibility of drugs and the optimal puncture technique associated with the DPE technique. Additionally, comprehensive investigations are needed to assess the potential risks and benefits of the DPE technique compared to other anesthesia regimens, taking into account factors such as maternal and neonatal outcomes and postoperative pain management.
Conclusions
In summary, our study aimed to compare three anesthesia techniques for elective cesarean delivery. Our findings indicate that the use of the DPE technique resulted in a faster onset of anesthesia compared to the EA. Additionally, there was evidence suggesting that the quality of the block achieved with the DPE technique was superior to that of the EA technique. We hypothesize that these results can be attributed to the enhanced passage of epidurally administered drugs across the dura following dural puncture.
Data Sharing Statement
We intend to share the raw data collected during the clinical trial, including demographic information, clinical measurements, and treatment outcomes. The data are available from the corresponding author ([email protected]) upon reasonable request. Access to the data will be granted for research purposes only and subject to compliance with applicable ethical guidelines and data protection regulations. The data may not be shared or used for any commercial purposes without prior permission. The data will be made available upon publication of the manuscript and will remain accessible for a period of 2 years from the date of publication.
Ethics and Consent Statements
Our research was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. We obtained informed consent from all participants involved in the study, and the study protocol was approved by the relevant institutional review board and ethics committee. We ensured the confidentiality and privacy of participant data throughout the study and adhered to all applicable data protection regulations.
Acknowledgments
The authors thank all the staff of the Department of Anesthesia and Operation Theater, Women’s Hospital, Zhejiang University School of Medicine, Hangzhou, China, for their help with this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Patel R, Kua J, Sharawi N, et al. Inadequate neuraxial anaesthesia in patients undergoing elective caesarean section: a systematic review. Anaesthesia. 2022;77(5):598–604. doi:10.1111/anae.15657
2. Lee JE, George RB, Habib AS, et al. Spinal-induced hypotension: incidence, mechanisms, prophylaxis, and management: summarizing 20 years of research. Best Pract Res Clin Anaesthesiol. 2017;31(1):57–68. doi:10.1016/j.bpa.2017.01.001
3. Suzuki N, Koganemaru M, Onizuka S, et al. Dural puncture with a 26-gauge spinal needle affects spread of epidural anesthesia. Anesth Analg. 1996;82(5):
4. Chau A, Bibbo C, Huang C-C, et al. Dural puncture epidural technique improves labor analgesia quality with fewer side effects compared with epidural and combined spinal epidural techniques. Anesth Analg. 2017;124(2):560–569. doi:10.1213/ANE.0000000000001798
5. Cappiello E, O’Rourke N, Segal S, et al. A randomized trial of dural puncture epidural technique compared with the standard epidural technique for labor analge. Anesth Analg. 2008;107(5):1646–1651. doi:10.1213/ane.0b013e318184ec14
6. Layera S, Bravo D, Aliste J, et al. A systematic review of DURAL puncture epidural analgesia for labor. J Clin Anesthesiol. 2019;53:5–10. doi:10.1016/j.jclinane.2018.09.030
7. Haiying Y, Xin T, Han H. Dural puncture epidural versus conventional epidural analgesia for labor: a systematic review and meta-analysis of randomized controlled studies. J Anaesth. 2022;36(3):413–427. doi:10.1007/s00540-022-03061-8
8. Ithnin F, Lim Y, Sia AT, et al. Combined spinal epidural causes higher level of block than equivalent single-shot spinal anesthesia in elective cesarean patients. Anesth Analg. 2006;102(2):577–580. doi:10.1213/01.ane.0000195440.51717.37
9. Teoh WH, Thomas E, Tan HM, et al. Ultra-low dose combined spinal-epidural anesthesia with intrathecal bupivacaine 3.75 mg for cesarean delivery: a randomized controlled trial. Int J Obstet Anesth. 2006;15(4):273–278. doi:10.1016/j.ijoa.2006.03.004
10. Pan PH, Bogard TD, Owen MD, et al. Incidence and characteristics of failures in obstetric neuraxial analgesia and anesthesia: a retrospective analysis of 19,259 deliveries. Int J Obstet Anesth. 2004;13(4):227–233. doi:10.1016/j.ijoa.2004.04.008
11. Tasneem D, Agrawal P, Khurana A, et al. Breach in the epidural catheter by a spinal needle: is it just a theoretical risk? Indian J Anaesth. 2020;64(2):158–159. doi:10.4103/ija.IJA_634_19
12. Bernards CM, Kopacz DJ, Michel MZ, et al. Effect of needle puncture on morphine and lidocaine flux through the spinal meninges of the monkey in vitro. Implications for combined spinal-epidural anesthesia. Anesthesiology. 1994;80(4):853–858. doi:10.1097/00000542-199404000-00019
13. Backe SK, Sheikh Z, Wilson R, et al. Combined epidural/spinal anaesthesia: needle-through-needle or separate spaces? Eur J Anaesthesiol. 2004;21(11):854–857. doi:10.1097/00003643-200411000-00003
14. Doo AR, Shin YS, Choi JW, et al. Failed dural puncture during needle-through-needle combined spinal-epidural anesthesia: a case series. J Pain Res. 2019;12:1615–1619. doi:10.2147/JPR.S178640
15. Contreras F, Morales J, Bravo D, et al. Dural puncture epidural analgesia for labor: a randomized comparison between 25-gauge and 27-gauge pencil point spinal needles[J]. Reg Anesth Pain Med. 2019;44(7):750–753. doi:10.1136/rapm-2019-100608
16. Norris MC, Ferrenbach D, Dalman H, et al. Does epinephrine improve the diagnostic accuracy of aspiration during labor epidural analgesia?. Anesth Analg. 1999;88(5):1073–1076. doi:10.1097/00000539-199905000-00019
17. Birnbach DJ, Chestnut DH. The epidural test dose in obstetric patients: has it outlived its usefulness?. Anesth Analg. 1999;88(5):971–972. doi:10.1213/00000539-199905000-00001
18. Hillyard SG, Bate TE, Corcoran TB, et al. Extending epidural analgesia for emergency Caesarean section: a meta-analysis. Br J Anaesth. 2011;107(5):668–678. doi:10.1093/bja/aer300
19. Khaw KS, Ngan Kee WD, Wong EL, et al. Spinal ropivacaine for cesarean section: a dose-finding study. Anesthesiology. 2001;95(6):1346–1350. doi:10.1097/00000542-200112000-00011
20. Chen XZ, Chen H, Lou AF, et al. Dose-response study of spinal hyperbaric ropivacaine for cesarean section. J Zhejiang Univ Sci B. 2006;7(12):992–997. doi:10.1631/jzus.2006.B0992
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.