Back to Journals » International Journal of General Medicine » Volume 16
Comparison of Different Systemic Inflammatory Markers in Predicting Clinical Outcomes with Syntax Score in Patients with Non-ST Segment Elevation Myocardial Infarction: A Retrospective Study
Authors Li H, Meng S, Chen W, Lei X, Kong X, Zhu H
Received 22 March 2023
Accepted for publication 9 June 2023
Published 19 June 2023 Volume 2023:16 Pages 2595—2607
DOI https://doi.org/10.2147/IJGM.S413538
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Hong Li,1 Shuai Meng,2 Weiguang Chen,3 Xuan Lei,4 Xiangyun Kong,5 Huagang Zhu6
1Emergency & Critical Care Center, Beijing Anzhen Hospital, Capital Medical University, Beijing, People’s Republic of China; 2Department of Cardiology, Beijing Tiantan Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Department of Cardiology, 1st Hospital Affiliated of Hebei North University, Zhangjiakou, Hebei Province, People’s Republic of China; 4Department of Cardiology, Beijing Chest Hospital, Capital Medical University, Beijing, People’s Republic of China; 5Department of General Medicine, Beijing Luhe Hospital, Capital Medical University, Beijing, People’s Republic of China; 6Department of Cardiology, Beijing Anzhen Hospital, Capital Medical University, Beijing, People’s Republic of China
Correspondence: Hong Li, Emergency & Critical Care Center, Beijing Anzhen Hospital, Capital Medical University, No. 2 Anzhen Road, Chaoyang District, Beijing, 100029, People’s Republic of China, Tel +86 13311573539, Email [email protected]
Background: The clinical value of the Syntax score in patients with non-ST segment elevation myocardial infarction (NSTEMI) has been well established. The neutrophil–lymphocyte ratio (NLR), the platelet–lymphocyte ratio (PLR), the high sensitivity C-reactive protein (hsCRP)-albumin ratio (hsCAR), and systemic immune-inflammatory (SII) index are promising systemic inflammation (SI) biomarkers in coronary artery diseases. However, studies which compare the predicting value of these SI indicators with the Syntax score in NSTEMI patients are limited.
Material and Methods: NSTEMI patients who underwent coronary angiography (CAG) in our department were retrospectively enrolled. Both univariable and multivariable logistic regression analyses were performed to evaluate the clinical value between SI biomarkers and Syntax score in these patients. The area under the receiver operating characteristic curve (ROC) was used to compare the clinical values of these parameters in predicting 6-month major cardiovascular events (MACE) and over-all mortality.
Results: A total of 429 NSTEMI patients were finally enrolled in this study. The level of NLR, PLR, as well as hsCAR, and SII in patients with high Syntax scores, are significantly higher than patients with the low Syntax score. Multivariable logistic regression analysis demonstrated that all of the SI indicators but not the Syntax score were the independent risk factors of 6-month MACE in NSTEMI patients. ROC showed that all of the SI indicators had better predictive value than the Syntax score in these patients (0.637, 0.592, 0.631, 0.590, 0.559, respectively) in predicting MACE and similar predictive value in over-all mortality (0.530, 0.524, 0.761, 0.553, 0.620, respectively).
Conclusion: Novel SI biomarkers including NLR, PLR, hsCAR, and SII have better predictive value in MACE and similar predictive value in over-all mortality compared with Syntax score in NSTEMI patients.
Keywords: neutrophil–lymphocyte ratio, platelet–lymphocyte ratio, high-sensitivity C-reactive protein–albumin ratio, non-ST segment elevation myocardial infarction
Background
As the most common type of acute coronary syndrome (ACS), non-ST segment elevation myocardial infarction (NSTEMI) carries a poor prognosis even under modern treatment.1,2 Previous studies have demonstrated the clinical value of coronary artery severity (CAS) calculated by Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX) score in patients with coronary artery disease (CAD).3,4 For patients with NSTEMI, the Syntax score was associated with both short-term and long-term clinical events. In a study by De Servi et al, the Syntax score was demonstrated to be associated with one-year major adverse cardiac events (MACE) in non-ST-segment elevation acute coronary syndrome (NSTE-ACS) patients who underwent percutaneous coronary intervention (PCI).5 Rafaeli et al also confirmed that baseline Syntax score was associated with midterm (11.6 ± 3.2 months) clinical outcomes in patients with NSTEMI.6
However, as an angiographic-based scoring system, the Syntax score is not available for CAD patients before coronary angiography (CAG) is performed. Also, Syntax score is not easy to acquire even for trained professionals. Finding a simpler prediction parameter in patients with CAD is important for clinicians.
It is widely accepted that systemic inflammation (SI) is involved in the pathogenesis of coronary artery atherosclerosis.7–10 Some SI indicators like neutrophil–lymphocyte ratio (NLR) and platelet–lymphocyte ratio (PLR) have been associated with the Syntax score.11–13 Lately, a novel SI biomarker, the high sensitivity C-reacting protein/albumin ratio (hsCAR), and Systemic immune-inflammation index (SII = platelet count × neutrophil count/lymphocyte count) have emerged and shown good clinical value in patients with coronary artery disease.14–17 However, the comparison between these inflammation biomarkers with the Syntax score in predicting clinical outcomes of NSTEMI patients has not been evaluated before. In this study, we aim to compare the predictive value of NLR, PLR, hsCAR, and SII in clinical outcomes with Syntax scores in NSTEMI patients.
Materials and Methods
Study Design and Participants
This single-center retrospective study was performed at Beijing Anzhen Hospital, Capital Medical University, Beijing, China. Patients aged 18 years or older diagnosed with acute NSTEMI and underwent CAG in our department between March 1st, 2017, and February 28th, 2019 were enrolled. Patients who did not undergo CAG, patients with severe hepatic or renal disease, active infection, active bleeding, and malignant tumor were excluded. Also, the patients who underwent percutaneous coronary intervention (PCI) as well as coronary artery bypass surgery (CABG) before and patients with missing relative clinical data were not included in this study. Ethics approval was granted by Beijing Anzhen Hospital, Capital Medical University. All of the patients provided written informed consent by themselves and their relatives. All of the procedures were performed in accordance with the Declaration of Helsinki.
The baseline clinical information including demographic characteristics, both previous medical history and personal medical history and pre-admission therapy were collected and analyzed. The Global Registry of Acute Coronary Events (GRACE) score and the Syntax score were evaluated by trained professionals. The definition of left main disease was ≥50% stenosis in the left main and/or ≥70% stenosis in the proximal left descending artery/left circumflex. The definition of chronic total occlusion (CTO) was the total occlusion of more than 3 months with TIMI 0 flow. Laboratory test results include complete blood cell panel, hepatic and renal function, lipid profile on admission, B-type natriuretic peptide (BNP) on admission, and left ventricular ejection fraction (LVEF) on admission were also collected and analyzed. The primary clinical outcomes were major adverse cardiovascular events (MACE) which included cardiovascular death, myocardial infarction, stroke, unstable angina, and coronary revascularization in a 6-month follow-up. The secondary clinical outcome was over-all mortality in a 6-month follow-up.
Statistical Analysis
Categorical variables were presented as numbers and frequencies (percentages) and were compared using the chi-square test. The continuous variables were expressed as mean SD ± mean or median (quartile 1, quartile 3) based on normality assumption and were compared using the independent sample t-test or Mann–Whitney test, as appropriate. A p-value of <0.05 was considered to be significant. Only significant factors according to the univariate analyses and important parameters proved by other studies like the Syntax score were further included in the multivariate analyses. The area under the receiver operating characteristic curve (AUC) was used to compare the predictive value of the parameters. The comparison of different markers was analyzed by the De Long method. Statistical analysis was performed using Statistical Package for the Social Sciences version 16.0 (SPSS Inc., Chicago, IL) and MedCalc version 20.106 (MedCalc Software Ltd, Ostend, Belgium).
Result
A total of 429 NSTEMI patients who underwent CAG were finally enrolled between March 1st, 2017, and February 28th, 2019. Of whom, 205 (47.8%) patients were divided into high-Syntax score group (MACE group: n = 48; non-MACE group: n = 157) while 224 patients were divided into low-Syntax score group (MACE group: n = 42; non-MACE group: n = 182) (Figure 1).
 |
Figure 1 Study flow chart. |
The comparison results of demographic parameters between the high-Syntax score and the low-Syntax score group are demonstrated in Table 1. In summary, patients with high-Syntax scores and patients with low-Syntax scores were of similar gender distribution (75.1% vs 74.6%, p = 0.912) and body mass index (BMI) (25.1[23.1–27.3] vs 24.8[22.7–26.6], p = 0.327). There was no significant difference in most of the relative parameters except patients with high-Syntax scores were older (61.0[56.0–68.0] vs 57.7[51.0–66.0], p = 0.000), more likely to have diabetes (57.1% vs 28.1%, p = 0.000) and higher heart rate on admission (74.6[68.0–80.5] vs 71.7[64.0–78.0], p = 0.001) when compared with patients with a low-Syntax score.
 |
Table 1 Baseline Demographic and Clinical Characteristics Between Patients with High Syntax Score and Patients with Low Syntax Score |
The comparison results of the angiographic characteristics between the high- and low-syntax score groups are shown in Table 2. Patients with high Syntax scores had a higher rate of the left main lesion (6.3% vs 1.3%, p = 0.009), CTO lesion (12.2% vs 5.4%, p = 0.015), and multi-vessel disease (70.7% vs 42.6%, p = 0.000), while the rate of bifurcation lesion, calcification lesion, and thrombosis lesion was comparable between the two groups (7.8% vs 8.5%, p = 0.861; 5.9% vs 3.6%, p = 0.360; 16.1% vs 14.7%, p = 0.789, respectively).
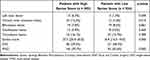 |
Table 2 Angiographic Characteristics Between Patients with High Syntax Score and Patients with Low Syntax Score |
The comparison results of laboratory parameters between the high- and low-syntax score groups are shown in Table 3. In summary, the level of novel SI indicators including NLR, PLR, hsCAR, and SII were significantly higher in patients with high-Syntax scores compared with patients with low-Syntax scores (6.0 [3.6–7.2] vs 4.1 [2.7–5.0], p = 0.000; 179.1 [122.3–209.8] vs 133.9 [90.6–166.3], p = 0.000; 0.6 [0.5–0.7] vs 0.5 [0.4–0.6], p = 0.000; 2.84[1.36–3.40] vs1.90[1.01–2.39], p = 0.000, respectively). Also, patients with high-Syntax score were more likely to have a higher level of white blood cell count (9.7 [8.7–10.9] vs 9.1 [7.8–10.2], 109/L, p = 0.000), platelet count (226.2 [178.0–258.5] vs 209.0 [168.3–244.0], 109/L, p = 0.001), hs-CRP (24.4 [19.7–28.2] vs 23.3 [18.0–27.5], p = 0.011), glucose (7.5 [5.7–9.0] vs 7.0 [5.3–8.3], p = 0.018), glycated hemoglobin (HbA1C) (6.8%[6.0–7.6%] vs 6.6% [5.8–7.2%], p=0.031), as well as triglyceride (1.8 [1.4–2.0] vs 1.7 [1.4–1.9], p = 0.015) while having a lower level of albumin when compared with patients with low-Syntax score (40.7 ± 4.1 vs 43.9 ± 3.7, p = 0.000).
 |
Table 3 Laboratory Test Results Between Patients with High Syntax Score and Patients with Low Syntax Score |
The comparison results of demographic parameters between the MACE group and the non-MACE group are demonstrated in Table 4. In summary, patients with MACE were more likely to have a family CAD history and more likely to be an active smoker than the non-MACE group (16.7% vs 8.0%, p = 0.026; 63.3% vs 47.8%, p = 0.009, respectively).
 |
Table 4 Baseline Demographic and Clinical Characteristics Between Patients with and without MACE |
The comparison results of laboratory parameters between patients with MACE and patients without MACE are shown in Table 5. In summary, the level of novel SI indicators including NLR, PLR, hsCAR, and SII were significantly higher in patients with MACE compared with patients without MACE (6.2 [3.7–7.6] vs 4.7 [2.9–5.6], p = 0.000; 180.6 [124.2–210.5] vs 148.8 [97.5–185.7]; p = 0.007; 0.7 [0.5–0.8] vs 0.5 [0.4–0.6]; p = 0.000 and 23.0[1.2–4.2] vs 2.2[1.2–2.8], p = 0.008, respectively). We also observed a higher level of BNP and white blood cell count as well as peak cTn-I level and lower level of LVEF in patients with MACE when comparing patients without MACE in the whole cohort (516.3 ± 157.1 pg/mL, vs 460.0 ± 138.4, pg/mL, p = 0.002; 10.1 [8.3–10.3] vs 9.2 [7.9–10.3],109/L, p = 0.000; 30.2 [11.0–44.8] vs 24.1[5.9–35.4], ng/mL, p=0.008, and 50.1[45.0–55.0] vs 52.7[48.0–57.0], %, p = 0.001, respectively). However, the Syntax score was not significantly different between the MACE group and the non-MACE group in our study (22[15–33] vs 21[17–26], p = 0.083).
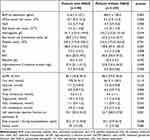 |
Table 5 Laboratory Test Results Between Patients with and without MACE |
The correlation between the novel SI indicators and coronary artery severity calculated by Syntax score was further analyzed and the result showed that all SI indicators were weakly related to the Syntax score (r = 0.221, p = 0.000; r = 0.211, p = 0.000; r = 0.172, p = 0.000; r = 0.182, p = 0.000, respectively) (Table 6).
 |
Table 6 Correlation Between Syntax Score with Different Systemic Inflammation Indicators |
We performed both univariable and multivariable logistic regression analysis to evaluate the predictive value of these SI biomarkers in coronary artery severity and it showed that all of the biomarkers were the independent risk factors for coronary severity (Table 7).
 |
Table 7 Univariable and Multivariable Logistic Regression Results for NLR, PLR, hsCAR, SII in Predicting Coronary Artery Severity |
We also performed both univariable and multivariable logistic regression analysis to evaluate the predictive value of these SI biomarkers and Syntax score in clinical outcomes. In summary, all of the novel SI biomarkers were the independent risk factors for MACE, and the Syntax score was not an independent risk factor for these patients (Table 8).
 |
Table 8 Univariable and Multivariable Logistic Regression Results for NLR, PLR, hsCAR, SII and Syntax Score in Predicting MACE |
We further compared the predicting value of NLR, PLR, hsCAR, SII, and Syntax scores in predicting the MACE and over-all mortality during 6-month follow-up. The result showed that all of the SI indicators have similar predicting values in the MACE and overall mortality in these patients; however, the predictive value of these SI indicators was all better than the Syntax score in predicting MACE during 6-month follow-up (Table 9 and Table 10, Figure 2).
 |
Table 9 Comparison of Area Under Curve Between NLR, PLR, hsCAR, SII and Syntax Score in Predicting MACE in 6-Month Follow-Up |
 |
Table 10 Comparison of Area Under Curve Between NLR, PLR, hsCAR, SII and Syntax Score in Predicting Overall Mortality in 6-Month Follow-Up |
Discussion
In the present study, we evaluated 1) the association between NLR, PLR, hsCAR, and SII with coronary artery severity calculated by Syntax score in NSTEMI patients and 2) compared the predictive value between SI biomarkers with Syntax score in predicting MACE and over-all mortality in the 6-month follow-up. The main findings of our study are as follows:
First, our study shows that novel SI indicators including NLR, PLR, hsCAR, and SII are all independent risk factors of coronary artery severity calculated by Syntax score.
In our study, a higher level of NLR was associated with a higher Syntax score in NSTEMI patients. This is consistent with previous studies.18,19 The association between NLR and all stages of CAD was also observed.20 The association between NLR and coronary plaque burden and coronary calcification was also observed in clinical studies.21,22
The association between PLR and coronary artery severity has also been explored in previous studies. In a study by Kurtul et al, a total of 1016 patients with acute coronary syndrome (ACS) who underwent emergent CAG were enrolled, and it turned out that on admission PLR was associated with coronary artery severity.23 In a study that enrolled 502 AMI patients, PLR was also believed to be a risk factor for coronary artery severity.24 In a meta-analysis that enrolled 14 studies, PLR was demonstrated to be associated with coronary artery severity and other parameters in patients with stable CAD.25
HsCAR was also believed to be associated with coronary artery severity in NSTEMI patients in our study. Both C-reactive protein (CRP) and albumin alone have been revealed to be associated with coronary artery severity.26,27 The association between CAR and CAS has been discussed in detail before. Çağdaş et al showed that CAR on admission was a useful parameter for predicting coronary artery severity.28 Moreover, Karabağ et al demonstrated that CAR was more tightly associated with coronary artery severity than CRP and albumin alone.29 Lately, a retrospective study by Kalyoncuoglu et al showed that CAR was associated with the Syntax score in NSETMI patients.30 Lately, the predictive value of hsCAR in COVID-19 patients and heart failure patients was also evaluated.31,32 However, as a novel SI indicator, the clinical value of hsCAR in cardiovascular diseases has only been evaluated in limited studies. Wang et al analyzed 652 patients with ACS and found that hsCAR was independently correlated with short-term MACE which was consistent with the conclusion of our study.14
The albumin is an important marker showing great predictive value in clinical practice. A study which enrolled 1798 patients who received permanent pacemaker implantation showed that albumin level at the time of device implantation was associated with long-term mortality in these patients.33 For patients with heart failure and ICD implantation, serum albumin was also related to the long-term mortality in these patients.34 In another study, lower serum albumin level was demonstrated to be associated with higher in-hospital mortality in COVID-19 patients.35 However, albumin on admission in our study was not an independent risk factor for the CAS and was not associated with short-term clinical outcomes. This difference should be further verified.
The association between systemic inflammation index (SII) and the Syntax score was also evaluated in our study. SII, as a novel biomarker, has also been well evaluated in many diseases. In a retrospective study, of 1011 patients who underwent intracardiac defibrillator implantation for heart failure, it turned out that a higher level of SII was an independent risk factor for long-term mortality.36 The association between SII and coronary artery severity was also evaluated in previous studies. Candemir et al explored the relationship between SII and Syntax score in CAD patients, and the results showed that a higher level of SII was associated with a higher level of Syntax score.37 In a study that enrolled 395 CAD patients who underwent CAG, SII was believed to be the independent risk factor for coronary artery severity.16 All of these studies are consistent with the findings in our study.
The second finding in our study is that all of the novel SI indicators had better prediction values in MACE when compared with the Syntax score.
Syntax score has been widely applied in clinical practice, and its clinical value in predicting MACE has been proven in numerous studies. However, as a complicated and angiographic-based scoring system, the Syntax score has some limitations as we mentioned above. It is important to find an easy way to predict MACE. In our study, we found that all of the SI indicators have better predictive value than the Syntax score.
The predictive value of NLR in MACE has been well studied before. In a study that enrolled 1860 STEMI patients who received pharmaco-invasive therapy, a higher level of NLR was associated with in-hospital MACE and death in these patients.38 Recently, a large meta-analysis that enrolled 60,087 patients confirmed that baseline NLR was associated with different inflammation parameters and was an independent risk factor for MACE.39
The predictive value of PLR, hsCAR and SII in MACE has also been evaluated in different studies. Dong et al performed a meta-analysis and found that a higher level of PLR was associated with worse in-hospital and long-term prognosis in STEMI patients after primary PCI.40 In a study by Wang et al, hsCAR was demonstrated to be associated with the prognosis of ACS.41 In a study by Yang et al, 5602 CAD patients who underwent PCI were enrolled, and the results showed that a higher level of SII score was associated with a higher rate of MACE than conventional risk factors.17 In a large cohort by Zhao et al, SII was demonstrated to be associated with long-term MACE in patients with triple vessel diseases.42
Although the clinical value of different SI indicators in MACE has been well established, the comparison of these SI biomarkers with Syntax scores in predicting clinical outcomes has not been explored before. So far as we know, our study demonstrated that all of the SI indicators have better predictive value than the Syntax score for the first time.
The third finding of our study is that all of the SI indicators including NLR, PLR, hsCAR, and SII have similar predictive value in clinical outcomes in NSTEMI patients. The comparison of clinical values in these SI indicators has been evaluated in previous studies. Atum et al compared the diagnostic performance of NLR and PLR in patients with retinal artery occlusion, and it turned out that NLR had better predictive value than PLR in this study.43 In a retrospective study by He et al, SII was demonstrated to be a superior predictor of long-term outcomes than NLR, and PLR in gastric cancer patients.44 In our study, all of the SI indicators have similar predictive values in MACE.
There are some limitations in our study. Firstly, this is a retrospective study with a limited number of participants, so further prospective study with a larger number of patients is needed to verify our findings. Secondly, 6-month clinical follow-up might not be sufficient to verify the clinical value of these indicators, especially well-validated Syntax score was not the independent risk factor in our study. Thirdly, the conclusion drawn by this study is limited to NSTEMI patients, and further studies which evaluate the clinical value of these SI biomarkers in other types of CAD patients are needed. Also, the importance value of diastolic dysfunction was not evaluated in our study due to the missing data.
In conclusion, our study evaluates and compares the predicting value of novel SI indicators with the Syntax score in predicting clinical outcomes of NSTEMI. The result shows that NLR, PLR, hsCAR, and SII have better predictive value in MACE and similar predictive value in over-all mortality of NSTEMI patients compared with Syntax score. Our study reveals that for NSTEMI patients, simple calculated on-admission SI indicators are useful in predicting clinical outcomes of these patients and provide even better information than the Syntax score.
Funding
This study was funded by the Beijing Science and Technology Project of Traditional Chinese Medicine (JJ2015-30) and National Health Commission Health Care Research Project (2022YB63).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tan NS, Goodman SG, Yan RT, et al. Comparative prognostic value of T-wave inversion and ST-segment depression on the admission electrocardiogram in non-ST-segment elevation acute coronary syndromes. Am Heart J. 2013;166(2):290–297. doi:10.1016/j.ahj.2013.04.010
2. Cheng CC, Yu FH, Ko PS, et al. Prognostic analysis of patients with acute myocardial infarction undergoing implantation of different stents for the first time. J Clin Med. 2021;10(21):5093. doi:10.3390/jcm10215093
3. Kundu A, Sardar P, O’Day K, et al. SYNTAX score and outcomes of coronary revascularization in diabetic patients. Curr Cardiol Rep. 2018;20(5):28. doi:10.1007/s11886-018-0971-1
4. Hayıroğlu Mİ, Keskin M, Uzun AO, et al. Predictive value of SYNTAX score II for clinical outcomes in cardiogenic shock underwent primary percutaneous coronary intervention; a pilot study. Int J Cardiovasc Imaging. 2018;34(3):329–336. doi:10.1007/s10554-017-1241-9
5. De Servi S, Crimi G, Calabrò P, et al. Relationship between diabetes, platelet reactivity, and the SYNTAX score to one-year clinical outcome in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention. EuroIntervention. 2016;12(3):312–318. doi:10.4244/EIJV12I3A51
6. Rafaeli IR, Kireeva AI, Tsereteli NV, et al. The influence of the initial severity of coronary artery lesion (by the Syntax Score) on the midterm prognosis of patients with acute myocardial infarction without ST segment elevation. Kardiologiia. 2022;62(11):19–25. doi:10.18087/cardio.2022.11.n1984
7. Ruparelia N, Choudhury R. Inflammation and atherosclerosis: what is on the horizon? Heart. 2020;106(1):80–85. doi:10.1136/heartjnl-2018-314230
8. Wang H, Liu Z, Shao J, et al. Immune and inflammation in acute coronary syndrome: molecular mechanisms and therapeutic implications. J Immunol Res. 2020;18:4904217.
9. Thackeray JT, Hupe HC, Wang Y, et al. Myocardial inflammation predicts remodeling and neuroinflammation after myocardial infarction. J Am Coll Cardiol. 2018;71(3):263–275. doi:10.1016/j.jacc.2017.11.024
10. Stark K, Massberg S. Interplay between inflammation and thrombosis in cardiovascular pathology. Nat Rev Cardiol. 2021;18(9):666–682. doi:10.1038/s41569-021-00552-1
11. Yüksel M, Yıldız A, Oylumlu M, et al. The association between platelet/lymphocyte ratio and coronary artery disease severity. Anatol J Cardiol. 2015;15(8):640–647. doi:10.5152/akd.2014.5565
12. Akboga MK, Canpolat U, Yayla C, et al. Association of platelet to lymphocyte ratio with inflammation and severity of coronary atherosclerosis in patients with stable coronary artery disease. Angiology. 2016;67(1):89–95. doi:10.1177/0003319715583186
13. Uçar FM, Açar B, Gul M, et al. The association between platelet/lymphocyte ratio and coronary artery disease severity in asymptomatic low ejection fraction patients. Korean Circ J. 2016;46(6):821–826. doi:10.4070/kcj.2016.46.6.821
14. Wang W, Ren D, Wang CS, et al. Prognostic efficacy of high-sensitivity C-reactive protein to albumin ratio in patients with acute coronary syndrome. Biomark Med. 2019;13(10):811–820. doi:10.2217/bmm-2018-0346
15. Ren H, Zhao L, Liu Y, et al. The high-sensitivity C-reactive protein to prealbumin ratio predicts adverse cardiovascular events after ST-elevation myocardial infarction. Heart Surg Forum. 2021;24(1):E153–E157. doi:10.1532/hsf.3307
16. Liu Y, Ye T, Chen L, et al. Systemic immune-inflammation index predicts the severity of coronary stenosis in patients with coronary heart disease. Coron Artery Dis. 2021;32(8):715–720. doi:10.1097/MCA.0000000000001037
17. Yang Y-L, Wu C-H, Hsu P-F, et al. Systemic immune-inflammation index (SII) predicted clinical outcome in patients with coronary artery disease. Eur J Clin Invest. 2020;50(5):e13230. doi:10.1111/eci.13230
18. Wada H, Dohi T, Miyauchi K, et al. Neutrophil to lymphocyte ratio and long-term cardiovascular outcomes in coronary artery disease patients with low high-sensitivity C-reactive protein level. Int Heart J. 2020;61(3):447–453. doi:10.1536/ihj.19-543
19. Kurtul S, Sarli B, Baktir AO, et al. Neutrophil to lymphocyte ratio predicts SYNTAX score in patients with non-ST segment elevation myocardial infarction. Int Heart J. 2015;56(1):18–21. doi:10.1536/ihj.14-175
20. Agarwal R, Aurora RG, Siswanto BB, et al. The prognostic value of neutrophil-to-lymphocyte ratio across all stages of coronary artery disease. Coron Artery Dis. 2022;33(2):137–143. doi:10.1097/MCA.0000000000001040
21. Nilsson L, Wieringa WG, Pundziute G, et al. Neutrophil/Lymphocyte ratio is associated with non-calcified plaque burden in patients with coronary artery disease. PLoS One. 2014;9(9):e108183. doi:10.1371/journal.pone.0108183
22. Nam SH, Kang SG, Song SW. The neutrophil-lymphocyte ratio is associated with coronary artery calcification in asymptomatic Korean males: a cross-sectional study. Biomed Res Int. 2017;2017:1989417. doi:10.1155/2017/1989417
23. Kurtul A, Murat SN, Yarlioglues M, et al. Association of platelet-to-lymphocyte ratio with severity and complexity of coronary artery disease in patients with acute coronary syndromes. Am J Cardiol. 2014;114(7):972–978. doi:10.1016/j.amjcard.2014.07.005
24. Li XT, Fang H, Li D, et al. Association of platelet to lymphocyte ratio with in-hospital major adverse cardiovascular events and the severity of coronary artery disease assessed by the Gensini score in patients with acute myocardial infarction. Chin Med J. 2020;133(4):415–423. doi:10.1097/CM9.0000000000000650
25. Qiu Z, Jiang Y, Jiang X, et al. Relationship between platelet to lymphocyte ratio and stable coronary artery disease: meta-analysis of observational studies. Angiology. 2020;71(10):909–915. doi:10.1177/0003319720943810
26. Camaj A, Giustino G, Kocovic N, et al. Effect of elevated C-reactive protein on outcomes after complex percutaneous coronary intervention for angina pectoris. Am J Cardiol. 2022;168:47–54. doi:10.1016/j.amjcard.2021.12.042
27. Çinar T, Hayiroğlu MI, Çiçek V, et al. Predictive value of serum albumin in patients with acute coronary syndrome. Angiology. 2021;72(1):93–94. doi:10.1177/0003319720952293
28. Çağdaş M, Rencüzoğullari I, Karakoyun S, et al. Assessment of relationship between C-reactive protein to albumin ratio and coronary artery disease severity in patients with acute coronary syndrome. Angiology. 2019;70(4):361–368. doi:10.1177/0003319717743325
29. Karabağ Y, Çağdaş M, Rencuzogullari I, et al. Relationship between C-reactive protein/albumin ratio and coronary artery disease severity in patients with stable angina pectoris. J Clin Lab Anal. 2018;32(7):e22457. doi:10.1002/jcla.22457
30. Kalyoncuoglu M, Durmus G. Relationship between C-reactive protein-to-albumin ratio and the extent of coronary artery disease in patients with non-ST-elevated myocardial infarction. Coron Artery Dis. 2020;31(2):130–136. doi:10.1097/MCA.0000000000000768
31. Güney BÇ, Taştan YÖ, Doğantekin B, et al. Predictive value of CAR for In-hospital mortality in patients with COVID-19 pneumonia: a retrospective cohort study. Arch Med Res. 2021;52(5):554–560. doi:10.1016/j.arcmed.2021.02.006
32. Çinier G, Hayıroğlu Mİ, Kolak Z, et al. The value of C-reactive protein-to-albumin ratio in predicting long-term mortality among HFrEF patients with implantable cardiac defibrillators. Eur J Clin Invest. 2021;51(8):e13550. doi:10.1111/eci.13550
33. Hayıroğlu Mİ, Çınar T, Çinier G, et al. Prognostic value of serum albumin for long-term mortality in patients with dual-chamber permanent pacemakers. Biomark Med. 2022;16(5):341–348. doi:10.2217/bmm-2021-0991
34. Çinier G, Hayıroğlu Mİ, Pay L, et al. Prognostic nutritional index as the predictor of long-term mortality among HFrEF patients with ICD. Pacing Clin Electrophysiol. 2021;44(3):490–496. doi:10.1111/pace.14170
35. Çınar T, Hayıroğlu Mİ, Çiçek V, et al. Is prognostic nutritional index a predictive marker for estimating all-cause in-hospital mortality in COVID-19 patients with cardiovascular risk factors? Heart Lung. 2021;50(2):307–312. doi:10.1016/j.hrtlng.2021.01.006
36. Hayıroğlu Mİ, Çınar T, Çinier G, et al. Evaluating systemic immune-inflammation index in patients with implantable cardioverter defibrillator for heart failure with reduced ejection fraction. Pacing Clin Electrophysiol. 2022;45(2):188–195. doi:10.1111/pace.14436
37. Candemir M, Kiziltunç E, Nurkoç S, et al. Relationship between Systemic Immune-Inflammation Index (SII) and the severity of stable coronary artery disease. Angiology. 2021;72(6):575–581. doi:10.1177/0003319720987743
38. Tavares F, Moraes PIM, Souza JM, et al. Prognostic role of neutrophil-to-lymphocyte ratio in patients with ST-elevation myocardial infarction undergoing to pharmaco-invasive strategy. Cardiovasc Revasc Med. 2022;34:99–103. doi:10.1016/j.carrev.2021.01.027
39. Adamstein NH, MacFadyen JG, Rose LM, et al. The neutrophil-lymphocyte ratio and incident atherosclerotic events: analyses from five contemporary randomized trials. Eur Heart J. 2021;42(9):896–903. doi:10.1093/eurheartj/ehaa1034
40. Dong G, Huang A, Liu L. Platelet-to-lymphocyte ratio and prognosis in STEMI: a meta-analysis. Eur J Clin Invest. 2021;51(3):e13386. doi:10.1111/eci.13386
41. Wang W, Ren D, Wang CS, et al. High sensitivity C-reactive protein to prealbumin ratio measurement as a marker of the prognosis in acute coronary syndrome. Sci Rep. 2019;9(1):11583. doi:10.1038/s41598-019-48189-y
42. Zhao J, Lv H, Yin D, et al. Systemic immune-inflammation index predicts long-term outcomes in patients with three-vessel coronary disease after revascularization: results from a large cohort of 3561 patients. J Inflamm Res. 2022;15:5283–5292. doi:10.2147/JIR.S385990
43. Atum M, Alagöz G. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with retinal artery occlusion. J Ophthalmic Vis Res. 2020;15(2):195–200. doi:10.18502/jovr.v15i2.6737
44. He K, Si L, Pan X, et al. Preoperative Systemic Immune-Inflammation Index (SII) as a superior predictor of long-term survival outcome in patients with stage I-II gastric cancer after radical surgery. Front Oncol. 2022;12:829689. doi:10.3389/fonc.2022.829689
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

