Back to Journals » Infection and Drug Resistance » Volume 16
Comparison of Azvudine and Nirmatrelvir/Ritonavir and Combined Use in Patients with COVID-19
Authors Hu CY, Cui WS, Lei Y, Tang YW, Zhang YY, Su QM, Peng F, Zeng YF, Song JL, Luo CN, Zhou Y, Li XY, Zhao ZX
Received 31 July 2023
Accepted for publication 29 November 2023
Published 22 December 2023 Volume 2023:16 Pages 7797—7808
DOI https://doi.org/10.2147/IDR.S433186
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Sandip Patil
Cheng-Yi Hu,1 Wen-Shuai Cui,1 Yi Lei,1 Yu-Wen Tang,1 Yan-Yan Zhang,1 Qi-Min Su,1 Fang Peng,2 Yun-Fei Zeng,1 Jia-Lin Song,1 Cheng-Na Luo,1 Yan Zhou,1 Xin-Yan Li,1 Zhu-Xiang Zhao1
1Department of Infectious Diseases, Guangzhou First People’s Hospital, School of Medicine, South China University of Technology, Guangzhou, Guangdong, People’s Republic of China; 2Department of Critical Care Medicine, the Third Affiliated Hospital of Guang Zhou Medical University, Guangzhou, Guangdong, People’s Republic of China
Correspondence: Zhu-Xiang Zhao, Department of Infectious Diseases, Guangzhou First People’s Hospital, School of Medicine, South China University of Technology, Guangzhou, 510515, People’s Republic of China, Email [email protected]
Purpose: To compare the effectiveness of azvudine and nirmatrelvir/ritonavir for the treatment of coronavirus disease (COVID-19).
Patients and Methods: We conducted a retrospective analysis of data from 576 patients with COVID-19, comprising 195 patients without antiviral therapy, 226 patients treated with azvudine, 114 patients treated with nirmatrelvir/ritonavir, and 41 patients were treated with azvudine and nirmatrelvir/ritonavir concurrently. We compared their symptoms, mortality rates, and the length and cost of hospitalization.
Results: The incidence of symptoms was similar in patients treated with azvudine and in those treated with nirmatrelvir/ritonavir. However, among patients experiencing weakness, the duration of weakness was significantly shorter in the azvudine group than in the nirmatrelvir/ritonavir group (P=0.029). Mortality did not differ significantly between the azvudine group and the nirmatrelvir/ritonavir group (18.14% vs.10.53%, P=0.068). Among “severe patients”, the mortality rate was markedly lower in patients treated with nirmatrelvir/ritonavir than in patients treated with azvudine (16.92% vs.32.17%, P=0.026). In patients with hepatic insufficiency, those treated with nirmatrelvir/ritonavir had substantially lower mortality than those treated with azvudine (15.09% vs.34.25%, P=0.016). In addition, patients treated with nirmatrelvir/ritonavir had longer hospital stays (P=0.002) and higher hospital costs (P< 0.001) than those receiving azvudine. Compared with patients treated with nirmatrelvir/ritonavir or azvudine alone, patients taking nirmatrelvir/ritonavir and azvudine concurrently had no significant improvement in survival (P> 0.05), length of stay (P> 0.05), or hospital costs (P> 0.05).
Conclusion: Azvudine is recommended for patients with non-severe COVID-19 with weakness. Nirmatrelvir/ritonavir is recommended for patients with severe COVID-19, to reduce mortality, and it could be the best choice for patients with hepatic insufficiency. The concurrent use of nirmatrelvir/ritonavir and azvudine in patients with COVID-19 could be not recommended.
Keywords: azvudine, nirmatrelvir/ritonavir, COVID-19, SARS-CoV-2
Introduction
Azvudine and nirmatrelvir/ritonavir are the two most commonly used antiviral drugs for treating COVID-19 in China. Previous studies have shown that both azvudine and nirmatrelvir/ritonavir are effective antiviral treatments for COVID-19.1–3 However, few studies have compared the effectiveness of azvudine and nirmatrelvir/ritonavir for COVID-19 treatment.
Azvudine was authorised for COVID-19 treatment by the State Drug Administration of China on 25 July 2022, and subsequently included in the Diagnosis and Treatment Program for Novel Coronavirus Pneumonia (Ninth Edition) on 9 August 2022.4 Azvudine is a nucleoside analogue with broad-spectrum antiviral activity. Its metabolites are embedded in viral RNA during SARS-CoV-2 RNA synthesis, thereby treating COVID-19 by inhibiting viral replication.5 Azvudine can shorten the time for the first nucleic acid test to turn negative, reduce the duration of symptoms in patients with moderate COVID-19, improve clinical manifestations, and lower the incidence of disease progression.1,6
In December 2021, the US Food and Drug Administration (FDA) granted Emergency Use Authorisation for the use of nirmatrelvir/ritonavir to treat patients with COVID-19 with a high risk of progressing to severe disease.7 On 25 May 2023, the FDA officially approved nirmatrelvir/ritonavir for treating COVID-19 in adults in the USA. Nirmatrelvir is a peptidomimetic inhibitor that prevents viral replication by inhibiting SARS-CoV-2 main protease (Mpro) so that it cannot process polyprotein precursors; ritonavir is an HIV-1 protease inhibitor that slows down metabolism of nirmatrelvir by inhibiting CYP3A4, thereby providing higher systemic exposure.8 A previous study demonstrated that nirmatrelvir/ritonavir effectively reduced mortality and the time to PCR-negative conversion in patients with COVID-19.9 Additionally, nirmatrelvir/ritonavir substantially reduced hospitalisation rates in patients with COVID-19.10
Currently, few studies are available that compare the effectiveness of azvudine and nirmatrelvir/ritonavir in patients with COVID-19. Both drugs appear to have unique advantages for treating COVID-19. Compared with those treated with azvudine, patients treated with nirmatrelvir/ritonavir tend to achieve faster first negative nucleic acid conversion.11 However, in patients with comorbidities, azvudine is associated with a lower risk of composite disease progression than nirmatrelvir/ritonavir is.12 Choosing between azvudine and nirmatrelvir/ritonavir for COVID-19 treatment poses a clinical challenge, necessitating a comprehensive discussion and comparison of their relative effectiveness. Therefore, in this retrospective study, we aimed to better understand the treatment choice between nirmatrelvir/ritonavir and azvudine in patients with COVID-19 who received either or both treatments.
Materials and Methods
Patient Cohort and Study Design
We conducted a retrospective cohort study on 664 patients with COVID-19. The inclusion criteria were: (1) Patients hospitalized at Guangzhou First People’s Hospital owing to SARS-CoV-2 infection between June 2022 and January 2023 and (2) patients able to accurately express their discomfort during hospitalization. The exclusion criteria were: (1) Patients with an unknown vaccination history; (2) patients co-infected with other respiratory viruses; (3) patients with incomplete data. We excluded 88 patients who did not meet the eligibility criteria and included 576 patients in the analysis. Among these patients, 195 did not receive antiviral therapy and were assigned to the control group, 226 were treated with azvudine and assigned to the azvudine group, 114 were treated with nirmatrelvir/ritonavir and assigned to the nirmatrelvir/ritonavir group, and 41 were treated with both azvudine and nirmatrelvir/ritonavir. A flowchart of the patient selection process is presented in Figure 1. We started follow-up on the date of admission to hospital with confirmed COVID-19. If the patient did not return to the hospital for a follow-up visit after discharge, follow-up ended on the date of discharge. If the patient returned to the hospital for follow-up visit within 1 month after discharge, the follow-up time was extended to the date of the first follow-up visit. The median (IQR) overall length of hospital stay was 9 (6–14) days. The overall median (IQR) follow-up period was 12 (8–18) days.
 |
Figure 1 Flowchart of patient selection. |
Definitions
According to the US National Institutes of Health (NIH) COVID-19 Treatment Guidelines,13 COVID-19 severity was grouped into asymptomatic or presymptomatic infection, mild illness, moderate illness, severe illness, and critical illness. In our study, patients with asymptomatic or presymptomatic infection, mild illness, and moderate illness were defined as “non-severe patients”, and those with severe illness and critical illness were defined as “severe patients”.
Antiviral Treatment
Azvudine was administered as 5 mg once daily for up to 14 days. Nirmatrelvir 300 mg and ritonavir 100 mg were administered twice daily for 5 days. In patients with moderate renal insufficiency, a reduced dose of nirmatrelvir 150 mg and ritonavir 100 mg twice daily for 5 days was administered at the attending doctor’s discretion.14
Ethics Approval and Informed Consent
The authors confirm that all procedures undertaken in this study adhere to the ethical standards set by the appropriate national and institutional committees on human experimentation, as well as the Helsinki Declaration of 1975, with its 2008 revisions. The retrospective analysis conducted in this study received approval from the Medical Ethics Committee of Guangzhou First People’s Hospital (Approval number: K-2023-066-01). All data in this study were de-identified and anonymized. A waiver of informed consent was granted as all anonymized data was collected retrospectively in accordance with the ethics approval.
Data Collection
We collected comprehensive data from Guangzhou First People’s Hospital for each COVID-19 patient, which included detailed information on demographics, epidemiology, comorbidities, symptoms, imaging reports (initial results upon admission), laboratory test results (initial results upon admission), treatment, and outcomes. The study endpoint was defined as either death or discharge from Guangzhou First People’s Hospital. A dedicated team of physicians and researchers collaborated to crosscheck and verify the accuracy of patient data.
Statistical Analyses
Statistical analyses were performed using SPSS Version 25.0 (IBM, Armonk, New York, USA). As the Shapiro–Wilk normality test indicated that none of the continuous variables in this study followed a normal distribution, these variables were presented as median values with interquartile ranges. Categorical variables were presented as frequencies and percentages. Group comparisons for continuous variables were conducted using the Mann–Whitney U-test, whereas categorical variables were assessed using the chi-squared or Fisher’s exact test. Survival analysis was employed to compare the duration of symptoms, with group comparisons performed using the Log rank test. All statistical tests were two-sided, and P< 0.05 was considered statistically significant.
SPSS Version 25.0 (IBM, Armonk, New York, USA) and GraphPad Prism version 8.0.0 (GraphPad Software, San Diego, California USA) were used to generate figures.
Results
Patient Characteristics and the Control of Confounding Factors
Considering that variations among the patients in clinical characteristics and laboratory test results may influence the efficacy evaluation comparison between azvudine and nirmatrelvir/ritonavir, we collected and analysed the clinical characteristics and laboratory test results of the patients to control for confounding factors in the results.
As shown in Table 1, there were no significant differences in age (P=0.433); sex (P=0.240); COVID-19 vaccination status (P=0.540); comorbidities such as hypertension (P=0.991), diabetes (P=0.103), coronary heart disease (P=0.620), hepatitis (P=0.174), chronic obstructive pulmonary disease (P=0.150), and chronic kidney disease (P=0.689); severity at admission (P=0.169); or treatments such as systemic steroid (P=0.225) and antibiotic (P=0.339) uses between the azvudine and nirmatrelvir/ritonavir groups. Since there were no significant differences in confounding factors between the two groups, we believe that these factors would not impact the results, thereby increasing the reliability of our findings.
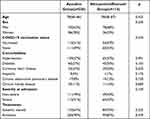 |
Table 1 Patient Characteristics in the Azvudine Group and the Nirmatrelvir/Ritonavir Group |
There were no significant differences in C-reactive protein levels (P=0.596), white blood cell (WBC) count (P=0.441), lymphocyte levels (P=0.126), monocyte levels (P=0.917), neutrophil percentage (P=0.462), total bilirubin levels (P=0.407), direct bilirubin levels (P=0.607), indirect bilirubin levels (P=0.729), creatinine levels (P=0.378), urea nitrogen levels (P=0.909), aspartate transaminase levels (P=0.097), or albumin levels (P=0.070) between the azvudine and nirmatrelvir/ritonavir groups (Table 2). Hence, we do not believe that these confounding factors would affect our findings.
 |
Table 2 The Laboratory Test Results in the Azvudine Group and the Nirmatrelvir/Ritonavir Group |
Supplementary Table 1 presents a detailed comparison between the azvudine and control groups, which did not yield any substantial differences, except for the use of hormones and monocyte levels. Similarly, Supplementary Table 2 details the comparison between the nirmatrelvir/ritonavir and control groups, which also did not exhibit any notable differences, except for the use of hormones and lymphocyte levels.
Comparison of Efficacy Between Azvudine and Nirmatrelvir/Ritonavir in Patients with COVID-19
Figure 2 shows that there were no significant differences in the incidence of cough (P=0.745), fever (P=0.415), myalgia (P=0.362), pharyngitis (P=0.170), weakness (P=0.212), and shortness of breath (P=0.922) between the azvudine and nirmatrelvir/ritonavir groups. This indicates that nirmatrelvir/ritonavir did not reduce the occurrence of COVID-19 symptoms compared to azvudine. Supplementary Figure 1 demonstrates that within the azvudine and nirmatrelvir/ritonavir groups, if patients developed fever, there was no significant difference in their maximum body temperature (P=0.123).
 |
Figure 2 Comparison of the incidence of cough, fever, myalgia, pharyngitis, weakness, and shortness of breath in the azvudine and nirmatrelvir/ritonavir groups. |
Furthermore, when patients experienced symptoms, the azvudine group exhibited no significant differences in the duration of cough (P=0.344), fever (P=0.932), myalgia (P=0.493), pharyngitis (P=0.999), or shortness of breath (P=0.076) compared to the nirmatrelvir/ritonavir group. However, the azvudine group had a significantly shorter duration of weakness (P=0.029) as shown in Figure 3.
Finally, we compared the mortality rates between the azvudine and nirmatrelvir/ritonavir groups (Figure 4). There was no significant difference in mortality between the azvudine and nirmatrelvir/ritonavir groups (P=0.068). However, among severe patients, the azvudine group had a significantly higher mortality rate than the nirmatrelvir/ritonavir group (P=0.026). Additionally, subgroup analysis results revealed that among the patients with renal insufficiency, there was no significant difference in mortality between the azvudine and nirmatrelvir/ritonavir groups (P=0.175). However, among patients with hepatic insufficiency, the nirmatrelvir/ritonavir group exhibited a lower mortality rate (P=0.016).
In addition, we compared the length of hospital stay and hospital expenses between the azvudine and nirmatrelvir/ritonavir groups. We found that patients in the nirmatrelvir/ritonavir groups had longer hospital stays (P=0.002) and higher hospital expenses (P<0.001), compared with patients in the azvudine groups (Figure 5).
The Efficacy Evaluation of Nirmatrelvir/Ritonavir and Azvudine Combined Use for Antiviral
In clinical practice, we observed that a small number of patients received both nirmatrelvir/ritonavir and azvudine during the treatment of COVID-19. In order to evaluate the effect of nirmatrelvir/ritonavir and azvudine combined use, we collected the information of 41 patients who received nirmatrelvir/ritonavir and azvudine at the same time point. We found that the combination of nirmatrelvir/ritonavir and azvudine did not improve patient survival, length of stay, or hospital costs compared with using nirmatrelvir/ritonavir or azvudine alone (Figure 6).
Discussion
When comparing the effectiveness of azvudine and nirmatrelvir/ritonavir in the treatment of COVID-19, it is crucial to control for the effect of confounding factors on the prognosis of the disease to ensure the validity of the results. In our study, we achieved a well-balanced distribution of confounding factors between groups. Age, sex, COVID-19 vaccination status, severity on admission, and treatment all influence the prognosis of COVID-19.15–17 Therefore, these factors were considered potential confounding factors in our study. Furthermore, comorbidities, such as hypertension, diabetes, coronary heart disease, hepatitis, chronic obstructive pulmonary disease (COPD), and chronic kidney disease (CKD) are all factors associated with poor prognosis in COVID-19.18–24 Systemic steroids play an important role in the treatment of patients with COVID-19, particularly in those with severe COVID-19 pneumonia, as they help prevent disease complications and improve clinical outcomes.25 Empiric antibiotic use in patients with COVID-19 does not prevent disease progression, reduce mortality, or shorten hospital stays;26,27 however, the use of antibiotics may be necessary for patients with bacterial infections. It is currently unclear whether antibiotic treatment improves symptoms in patients with bacterial infections. Given that these factors can potentially influence the effectiveness of antiviral drugs in patients with COVID-19, we performed a detailed comparison of these indicators to check the balance of confounding factors between the azvudine and nirmatrelvir/ritonavir treatment groups. Additionally, we conducted a comprehensive comparison of laboratory test results to assess their effect as confounding factors. C-reactive protein (CRP) serves as an early predictive biomarker for hypoxia in COVID-19,28 and elevated CRP levels may indicate a higher susceptibility to shortness of breath. Several studies have shown a strong association between the white blood cell, lymphocyte, monocyte, and neutrophil counts on admission in patients with COVID-19, and mortality.29,30 A single-centre prospective cohort study revealed that serum albumin and creatinine are predictive indicators of acute kidney injury in patients with COVID-19, which can impact patient prognosis.31 We successfully controlled for the influence of these confounding factors on the outcomes by comparing the laboratory test results of the azvudine and nirmatrelvir/ritonavir groups.
Our findings revealed a similar incidence of symptoms between patients receiving azvudine and those receiving nirmatrelvir/ritonavir. However, patients treated with azvudine experienced a considerably shorter duration of weakness than those who received nirmatrelvir/ritonavir. Although there was no substantial difference in overall mortality between patients receiving azvudine and those receiving nirmatrelvir/ritonavir, in patients with severe disease, the mortality rate was substantially lower in patients treated with nirmatrelvir/ritonavir. Notably, among patients with renal insufficiency, no notable difference was observed in the effect of azvudine and nirmatrelvir/ritonavir on mortality. However, among patients with hepatic insufficiency, those receiving nirmatrelvir/ritonavir exhibited a considerably lower mortality rate than those who received azvudine. Ritonavir is a potent hepatic enzyme inhibitor; therefore, in patients with hepatic insufficiency, ritonavir might exert a stronger inhibitory effect on P450 CYP3A4, resulting in higher exposure to nirmatrelvir and lower mortality. In addition, we found that patients in the nirmatrelvir/ritonavir group had higher hospitalization costs. These higher hospitalization costs might be related to the patients’ family economic conditions. In China, the price of a course of azvudine was about 170 RMB. Moreover, patients using azvudine can be reimbursed for part of the cost through medical insurance. However, the price of a course of nirmatrelvir/ritonavir was about 1700 RMB. Patients using nirmatrelvir/ritonavir tended to have a higher household income, and thus were more likely actively pursue better medical care, attention, and treatment, resulting in higher hospitalization costs.
To date, a limited number of studies have compared the effectiveness of azvudine and nirmatrelvir/ritonavir. Gao et al11 conducted a study of 245 patients and used propensity-score matching to control for confounding factors. However, in our study, we achieved a balanced distribution of confounding factors at baseline upon enrolment, and the ratio of patients in the nirmatrelvir/ritonavir group to those in the azvudine group was nearly 2:1. Therefore, we did not employ propensity matching scores and ultimately included 576 patients. Dian et al12 conducted a study involving 456 patients with COVID-19 receiving antiviral therapy and utilized propensity-score matching, but did not control for variables in the admission test results. Similar to Gao et al,11 the confounding factors in the laboratory test results was balanced in our study to ensure the greatest possible reliability of the findings. Consistent with our study’s results, studies by Zhao Q et al32 and Zhao X et al33 also found that there was no significant difference in overall mortality between the nirmatrelvir/ritonavir and azvudine groups. However, Dian et al12 found that among patients with COVID-19 and comorbidities, the risk of composite disease progression was lower in the azvudine group than in the nirmatrelvir/ritonavir group.
Furthermore, we found that the combination therapy of the nirmatrelvir/ritonavir and azvudine did not improve patient survival, length of stay, or hospital costs compared with using nirmatrelvir/ritonavir or azvudine alone. Therefore, we do not recommend the concurrent use of nirmatrelvir/ritonavir and azvudine in patients with COVID-19.
Our study has several limitations. First, owing to the retrospective nature of the study, detailed data on vaccinations, such as the number and type of vaccines administered, were not fully recorded. Second, it was conducted at a single centre, and the sample size was relatively small. Therefore, further multicentre studies with larger sample sizes are necessary for validation. Third, there are numerous potential confounding factors that may affect the effectiveness of azvudine and nirmatrelvir/ritonavir, and residual confounding due to unmeasured confounders may be present. Fourth, SARS-CoV-2 mutations may change the effectiveness of antiviral therapy. Fifth, symptom data from patients with COVID-19 was recorded through patient self-report when the doctor was on the daily ward rounds. Patients’ self-reports may be limited by their medical knowledge, resulting in recorded results that were not entirely consistent with actual conditions.
Conclusion
Our findings suggest that azvudine could be recommended for patients with non-severe COVID-19 and weakness, whereas nirmatrelvir/ritonavir could be recommended for patients with severe disease to reduce mortality, and it might be a better choice for patients with hepatic insufficiency. The concurrent use of nirmatrelvir/ritonavir and azvudine in patients with COVID-19 could be not generally recommended.
Data Sharing Statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
We express our gratitude to the medical staff for their valuable involvement and support in this study.
Funding
This work was funded by the National Nature Science Foundation of China (Grant No. 81970038 and 8227004) and the Science and Technology Projects in Guangzhou, China (SL2022A04J00473).
Disclosure
The authors have no competing interests to declare that are relevant to the content of this article.
References
1. Ren Z, Luo H, Yu Z, et al. A randomized, open-label, controlled clinical trial of azvudine tablets in the treatment of mild and common COVID-19, a pilot study. Adv Sci. 2020;7(19):e2001435. doi:10.1002/advs.202001435
2. Najjar-Debbiny R, Gronich N, Weber G, et al. Effectiveness of Paxlovid in reducing severe coronavirus disease 2019 and mortality in high-risk patients. Clin Infect Dis. 2023;76(3):e342–349. doi:10.1093/cid/ciac443
3. Weng C, Xie R, Han G, et al. Safety and efficacy of Paxlovid against Omicron variants of coronavirus disease 2019 in elderly patients. Infect Dis Ther. 2023;12(2):649–662. doi:10.1007/s40121-023-00760-x
4. Yu B, Chang J. The first Chinese oral anti-COVID-19 drug Azvudine launched. Innovation. 2022;3(6):100321. doi:10.1016/j.xinn.2022.100321
5. Yu B, Chang J. Azvudine (FNC): a promising clinical candidate for COVID-19 treatment. Signal Transduct Target Ther. 2020;5(1):236. doi:10.1038/s41392-020-00351-z
6. Sun Y, Jin L, Dian Y, et al. Oral Azvudine for hospitalised patients with COVID-19 and pre-existing conditions: a retrospective cohort study. EClinicalMedicine. 2023;59:101981. doi:10.1016/j.eclinm.2023.101981
7. Alsaeed A, Alkhalaf A, Alomran A, Alsfyani W, Alhaddad F, Alhaddad MJ. Paxlovid for treating COVID-19 patients: a case-control study from two hospitals in the eastern province of Saudi Arabia. Cureus. 2023;15(5):e39234. doi:10.7759/cureus.39234
8. Extance A. Covid-19: what is the evidence for the antiviral Paxlovid? BMJ. 2022;377:o1037. doi:10.1136/bmj.o1037
9. Hammond J, Leister-Tebbe H, Gardner A, et al. Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19. N Engl J Med. 2022;386(15):1397–1408. doi:10.1056/NEJMoa2118542
10. Shah MM, Joyce B, Plumb ID, et al. Paxlovid associated with decreased hospitalization rate among adults with COVID-19 – United States, April–September 2022. MMWR Morb Mortal Wkly Rep. 2022;71(48):1531–1537. doi:10.15585/mmwr.mm7148e2
11. Gao Y, Luo Z, Ren S, et al. Antiviral effect of azvudine and nirmatrelvir-ritonavir among hospitalized patients with COVID-19. J Infect. 2023;86(6):e158–e160. doi:10.1016/j.jinf.2023.03.023
12. Dian Y, Meng Y, Sun Y, Deng G, Zeng F. Azvudine versus Paxlovid for oral treatment of COVID-19 in Chinese patients with pre-existing comorbidities. J Infect. 2023;87(2):e24–e27. doi:10.1016/j.jinf.2023.05.012
13. NIH COVID-19 Treatment Guidelines. COVID-19 treatment guidelines. Available from: https://www.covid19treatmentguidelines.nih.gov/management/clinical-management-of-adults/.
14. National Health Commission of the People’s Republic of China Diagnosis and Treatment Plan for COVID-19 (Trial Version 10). In Chinese. Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202301/32de5b2ff9bf4eaa88e75bdf7223a65a.shtml.
15. Tanaka C, Tagami T, Nakayama F, et al. Association between mortality and age among mechanically ventilated COVID-19 patients: a Japanese nationwide COVID-19 database study. Ann Intensive Care. 2021;11(1):171. doi:10.1186/s13613-021-00959-6
16. Gomez JMD, Du-Fay-de-Lavallaz JM, Fugar S, et al. Sex differences in COVID-19 hospitalization and mortality. J Womens Health. 2021;30(5):646–653. doi:10.1089/jwh.2020.8948
17. Chen YT. Effect of vaccination patterns and vaccination rates on the spread and mortality of the COVID-19 pandemic. Health Policy Technol. 2023;12(1):100699. doi:10.1016/j.hlpt.2022.100699
18. Baranova A, Cao H, Zhang F. Causal associations and shared genetics between hypertension and COVID-19. J Med Virol. 2023;95(4):e28698. doi:10.1002/jmv.28698
19. Fukushima T, Chubachi S, Namkoong H, et al. Clinical significance of prediabetes, undiagnosed diabetes and diagnosed diabetes on critical outcomes in COVID-19: integrative analysis from the Japan COVID −19 task force. Diabetes Obes Metab. 2023;25(1):144–155. doi:10.1111/dom.14857
20. Liang C, Zhang W, Li S, Qin G. Coronary heart disease and COVID-19: a meta-analysis. Med Clin. 2021;156(11):547–554. doi:10.1016/j.medcli.2020.12.017
21. Yu Y, Li X, Wan T. Effects of hepatitis B virus infection on patients with COVID-19: a meta-analysis. Dig Dis Sci. 2023;68(4):1615–1631. doi:10.1007/s10620-022-07687-2
22. Marron RM, Zheng M, Fernandez Romero G, et al. Impact of chronic obstructive pulmonary disease and emphysema on outcomes of hospitalized patients with coronavirus disease 2019 pneumonia. Chronic Obstr Pulm Dis. 2021;8(2):255–268. doi:10.15326/jcopdf.2020.0200
23. Fedeli U, Barbiellini Amidei C, Marcon A, et al. Mortality related to chronic obstructive pulmonary disease during the COVID-19 pandemic: an analysis of multiple causes of death through different epidemic waves in Veneto, Italy. Int J Environ Res Public Health. 2022;19(19):12844. doi:10.3390/ijerph191912844
24. Gok M, Cetinkaya H, Kandemir T, et al. Chronic kidney disease predicts poor outcomes of COVID-19 patients. Int Urol Nephrol. 2021;53(9):1891–1898. doi:10.1007/s11255-020-02758-7
25. Hassan AT, Elmoniem AEA, Abdelrady MM, et al. Challenges in steroid and anticoagulant therapy in severe COVID-19 pneumonia: a prospective study. Antibiotics. 2021;10(10):1214. doi:10.3390/antibiotics10101214
26. Yin X, Xu X, Li H, et al. Evaluation of early antibiotic use in patients with non-severe COVID-19 without bacterial infection. Int J Antimicrob Agents. 2022;59(1):106462. doi:10.1016/j.ijantimicag.2021.106462
27. Ng TM, Ong SWX, Loo AYX, et al. Antibiotic therapy in the treatment of COVID-19 pneumonia: who and when? Antibiotics. 2022;11(2):184. doi:10.3390/antibiotics11020184
28. Miyata Y, Inoue H, Hirai K, et al. Serum cystatin C and CRP are early predictive biomarkers for emergence of hypoxia in COVID-19. Am J Med Sci. 2022;364(6):706–713. doi:10.1016/j.amjms.2022.06.027
29. Zhu B, Feng X, Jiang C, et al. Correlation between white blood cell count at admission and mortality in COVID-19 patients: a retrospective study. BMC Infect Dis. 2021;21(1):574. doi:10.1186/s12879-021-06277-3
30. Seyit M, Avci E, Nar R, et al. Neutrophil to lymphocyte ratio, lymphocyte to monocyte ratio and platelet to lymphocyte ratio to predict the severity of COVID-19. Am J Emerg Med. 2021;40:110–114. doi:10.1016/j.ajem.2020.11.058
31. Schnabel K, Garam N, Ledó N, et al. Urinary albumin-to-creatinine ratio and serum albumin are predictors of acute kidney injury in non-ventilated COVID-19 patients: a single-center prospective cohort study. Int Urol Nephrol. 2023;55(3):711–720. doi:10.1007/s11255-022-03348-5
32. Zhao Q, Zheng B, Han B, et al. Is Azvudine Comparable to Nirmatrelvir-Ritonavir in Real-World Efficacy and Safety for Hospitalized Patients with COVID-19? A Retrospective Cohort Study. Infect Dis Ther. 2023;12(8):2087–2102. doi:10.1007/s40121-023-00845-7
33. Zhao X, Cheng Y, Zhang M, et al. Efficacy of Nirmatrelvir-Ritonavir versus Azvudine for COVID-19 Treatment in Tibet: a Retrospective Study. Infect Drug Resist. 2023;16:6053–6060. doi:10.2147/IDR.S423725
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




