Back to Journals » International Journal of General Medicine » Volume 16
Comparison and Validation of Different Risk Assessment Models in Patients with Venous Thromboembolism During Pregnancy and Postpartum: A Retrospective Study in China
Authors Lian Y, Li J , Liang W, Zhong M
Received 28 September 2022
Accepted for publication 16 December 2022
Published 7 January 2023 Volume 2023:16 Pages 95—106
DOI https://doi.org/10.2147/IJGM.S391005
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Yanqin Lian,1,* Jia Li,2,* Weizhang Liang,2 Mei Zhong3
1Department of Operating Room, Guangdong Provincial Key Laboratory of Major Obstetric Diseases, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong Province, People’s Republic of China; 2Department of Obstetrics and Gynecology, Guangdong Provincial Key Laboratory of Major Obstetric Diseases, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong Province, People’s Republic of China; 3Department of Obstetrics and Gynecology, Nanfang Hospital, Southern Medical University, Guangzhou, Guangdong Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Weizhang Liang, Department of Obstetrics and Gynecology, Guangdong Provincial Key Laboratory of Major Obstetric Diseases, The Third Affiliated Hospital of Guangzhou Medical University, No. 63 Duobao Road, Guangzhou, Guangdong Province, 510515, People’s Republic of China, Tel +86 20 81292539, Email [email protected] Mei Zhong, Department of Obstetrics and Gynecology, Nanfang Hospital, Southern Medical University, No. 1838 Guangzhou Avenue North, Guangzhou, Guangdong Province, 510515, People’s Republic of China, Tel +86 20 61641901, Email [email protected]
Introduction: Venous thromboembolism (VTE) causes maternal mortality and morbidity. This study compares the predictive performance of three risk assessment models (Caprini model, Wells Score, and RCOG model) for VTE risk in Chinese patients during pregnancy and postpartum.
Materials and Methods: We conducted a retrospective study in Nanfang Hospital of Southern Medical University and the Third Affiliated Hospital of Guangzhou Medical University from January 2003 to January 2022. Patients were risk-classified using the three risk assessment models, and the models were evaluated for accuracy.
Results: A total of 302 patients with confirmed VTE during pregnancy and postpartum were identified. Of these, 142 (47.0%) were diagnosed during pregnancy and 160 (53.0%) postpartum. A total of 276 (91.4%) patients had DVT only, 14 (4.6%) had PE only, and 12 (4.0%) were diagnosed with both. Of the 142 antepartum patients, 140 were categorized at moderate or above-risk levels by the Caprini model, 134 in the Wells Score model, and 112 in the RCOG model, respectively. The number of postpartum patients at moderate or above-risk levels identified by the Caprini, Wells Score, and RCOG models were 160, 152, and 118. The Caprini model significantly stratified VTE patients into a moderate or high-risk level (p < 0.05, Friedman Test). The Caprini model was also more effective at assessing the risk of VTE among postpartum patients than antepartum patients (p < 0.05, Friedman Test).
Conclusion: We have demonstrated that the Caprini model is an effective prediction tool for the maternal population during peripartum, especially in the postpartum period. Results from the Caprini model will help obstetricians or physicians stratify potential risk patients and guide prophylaxis decisions. The RCOG model was not particularly useful in Chinese VTE patients during pregnancy and postpartum. Multicenter prospective validations of the RCOG model in Chinese maternal populations are needed.
Keywords: venous thromboembolism, deep venous thrombosis, pulmonary embolism, risk assessment models, pregnancy and postpartum, antepartum and postpartum
Plain Language Summary
Venous thromboembolism (VTE) remains a significant cause of maternal mortality and morbidity. Accurate risk assessment of VTE can stratify a patient’s true extent of risk and provide appropriate recommendations for prophylactic therapies. Several VTE risk assessment models (RAMs) have already been proposed and evaluated clinically in western populations. However, few studies assess the validity of these models in Chinese maternal people. Thus, we performed this study to compare and evaluate the validity performance of three different RAMs (Caprini model, Wells Score, and RCOG model) in patients with VTE during pregnancy and postpartum, retrospectively. Our study demonstrated that the Caprini model is an effective prediction tool for patients during peripartum, especially in the postpartum, which can help obstetricians stratify potential risk patients and be used to guide prophylaxis decisions. The RCOG model was not particularly useful in Chinese VTE patients during peripartum. Multicenter prospective validations of the RCOG model in Chinese maternal populations are needed.
Introduction
Venous thromboembolism (VTE), referring to deep venous thrombosis (DVT) and pulmonary embolism (PE), is a common disease with high morbidity and mortality among hospitalized patients. Pregnant women have an increased risk (four- to six-fold higher) of thromboembolism than non-pregnant women.10,18 Approximately 75–80% of cases with pregnancy-associated VTE are DVT, and 20–25% of cases are PE, accounting for 1.1 deaths per 100,000 deliveries,3,13,22 or 9% of all maternal deaths in the United States.8 Similarly, in the United Kingdom (UK), thromboembolisms were the leading cause of maternal death from 1985 to 2006 (1.40–2.18 /100,000 maternities).4 Most of these antepartum VTE events occur in the first trimester, but the highest risk period for VTE, PE in particular, is during the postpartum period,3,13 when the risk of VTE has increased five-fold.10 Despite solid evidence that thromboprophylaxis reduces the incidence of VTE, it remains underused in obstetric patients.9 Accurate VTE risk assessment in maternity patients is critical to improving the current situation by taking advantage of thromboprophylaxis to prevent VTE.
Appropriate risk assessment, through identifying and evaluating all possible risk factors, can estimate the true extent of risk for a patient and provide appropriate recommendations for prophylactic therapies. Notable VTE risk assessment models (RAMs) have been proposed and clinically evaluated by Caprini,5 Wells,24 Kucher,14 and Barbar.2 These RAMs have been validated with medicine and general, vascular, and urologic surgical settings in western populations. Cavazza et al6 established a risk-score model to assess the individual need for prophylaxis in preventing Caesarean delivery–related VTE. However, no such risk assessment model was established in China, and few studies evaluate the validity of these foreign models in Chinese populations. Moreover, seldom have RAMs been targeted, especially in obstetric patients.
To identify a convenient, practical, and valuable risk assessment model which applies to Chinese maternity patients, we validated two published RAMs: the modified 2005 Caprini model1 and the modified Wells Score,25 and one empirical RAM adapted from the latest clinical guideline for prevention of VTE during pregnancy and postpartum: the Royal College of Obstetricians and Gynecologists (RCOG) Green-top guideline 37a.20 This retrospective study aimed to compare and assess the validity of the performance of these RAMs in patients with confirmed VTE during pregnancy and postpartum in Guangzhou, China.
Materials and Methods
Study Design and Patients
This is a retrospective study of patients who developed VTE at Nanfang Hospital of Southern Medical University and Third Affiliated Hospital of Guangzhou Medical University. Both are academic tertiary care institutions in Guangzhou, China. This study was performed in line with the principles of the Declaration of Helsinki. The Ethics Committee of Nanfang Hospital of Southern Medical University and the Ethics Committee of Third Affiliated Hospital of Guangzhou Medical University provided ethical approval for this study. Written informed consent was obtained from all participants for their clinical records for use in this study.
All women diagnosed with VTE during pregnancy and the postpartum period who were eligible for this investigation were selected between January 2003 and January 2022. Reviewed cases were selected based on hospital ICD-10 codes for VTE (I26, I80, I82). Patients with confirmed VTE (DVT and/or PE) during pregnancy and the postpartum period, age ≥ 18 years, with a ≥ 2–day duration of hospital stay were eligible for the study. Criteria for exclusion included: incomplete information, VTE with ectopic gestation, thrombosis in a location other than deep veins of the legs or arms, or coding error. DVT was validated based on positive compression ultrasonography or contrast venography. PE was diagnosed from either a positive pulmonary angiogram, spiral computed tomography, or high probability ventilation/perfusion scan.
Patient’s medical information (demographics, history of pregnancy and delivery, risk factors for VTE in the RAMs, length of hospital stay, information about VTE prophylaxis, diagnostic test results and physician notes, etc.) was obtained from the hospital electronic medical records by two obstetricians, who received in-depth training given by the local Department of Medical Records on how best to collect and analyze information from clinical notes and on quality assuring data collection to ensure data reliability. Prophylaxis was defined as the administration of any mechanical or pharmacological prophylaxis before the date on which the patient’s VTE was diagnosed.
Risk Assessment Models
The modified Caprini risk assessment model (2005 version), published in 2009, uses a point-scoring system and approximately 40 risk factors listed with weights of 1 to 5 points each.1 The relative sum of scores for individual risk factors produces a cumulative risk score that defines the patient’s risk level: low risk (0–1 score), moderate risk (2 scores), high risk (3–4 score), or highest risk (≥ 5 scores). Each risk level was associated with a prophylaxis regimen.
The modified Wells Score is widely used for pre-test probability assessment of DVT. It consists of 10 clinical items which stratify patients into three risk levels low (≤ 0 scores), intermediate (1–2 score), and high (≥ 3 scores).25
The other VTE risk assessment model was empirically adapted from the latest clinical practice guideline regarding the prevention of VTE during peripartum from the Royal College of Obstetricians and Gynecologists (RCOG)20 (the RCOG model). The RCOG model classified the VTE risk factors into three categories by timeframe. Each risk factor was weighted according to a point scale (3 scores for a major risk factor, two scores for an intermediate one, and one score for a minor one).
Each patient diagnosed with VTE during pregnancy or postpartum were retrospectively assessed for risk by the above three RAMs.
Statistical Analysis
Data from each continuous variable (eg, weight, BMI) with a normal distribution were evaluated as means with standard deviation (SD). A T-Test comparison between each group was achieved. Continuous variables with a skewed distribution were evaluated as median values with interquartile ranges. Categorical variables (eg, risk assessment level) were evaluated with a Mann Whitney U-Test and Friedman Test to determine the significance between groups. Statistical significance was identified if the p-value < 0.05 (two-tailed). All data analyses were performed with IBM SPSS software, version 18.0 (SPSS Inc., Chicago, Illinois, USA).
Results
Clinical Characteristics of Patients
Three hundred seventy patients were recruited into the study, but 68 patients were excluded for incomplete information (n = 16), VTE with ectopic gestation (n = 5), age < 18y (n = 2), < 2-day hospital stay (n = 19), thrombosis in a location other than deep veins of the legs or arms (n = 24), or coding error (n = 2). Thus, 302 eligible patients were diagnosed with VTE during pregnancy or postpartum, distributed among 15 clinical departments in the two hospitals (6 surgical and nine medical departments). Of the 302 VTE patients, 106 (35.1%) were admitted to the Department of Obstetrics and Gynecology, 152 (50.3%) to the Department of Vascular Surgery or General Surgery, 6 (2.0%) to the Intensive Care Unit, and the remaining 38 (12.6%) went to Internal Medicine Departments, such as Respiratory, Cardiology, Hematology, Neurology and Chinese Traditional Medicine. Among the 302 patients, 48 (15.9%) were over 35 years old, 70 (31.0%) had a BMI equal to or greater than 25, only 18 (7.4%) had a parity equal to or greater than 3, 280 (92.7%) were singleton pregnancies or gave birth to a single fetus, and nearly half of the patients (47%) were delivered by Caesarean section. During documentation of VTE, 142 (47.0%) patients were diagnosed during pregnancy and 160 (53.0%) in postpartum. 276 (91.4%) patients had DVT only, 14 (4.6%) had PE only, and 12 (4.0%) were diagnosed with both. Systematic screening for PE was not performed for patients with DVT, and vice versa. Only 38 (12.6%) VTE patients received thromboprophylaxis before the diagnosis of VTE. The basic characteristics of the patients in the study are presented in Table 1.
 |
Table 1 Characteristics of the Hospitalized Patients with Confirmed VTE |
Distribution of VTE Patients by Risk Level and Cumulative Risk Score in Three RAMs
Table 2 shows the distribution of the VTE patients with the associated risk factor from the Caprini risk assessment model. Besides pregnancy or postpartum (100%), the most frequent risk factors were swollen leg (79.47%), major open surgery (eg, Caesarean delivery) (46.36%), obesity (BMI > 25 kg/m2) (30.43%), and minor surgery (eg, vaginal delivery) (25.83%). Of the 302 VTE patients included in the Caprini RAM, 50 (16.56%) reported a history of VTE, but no patients reported having a family history of DVT or PE. Of the 96 patients screened for thrombophilia, 30 (35.42%) had a deficiency of protein S or protein C, and 4 (4.12%) were diagnosed with anti-phospholipid antibody syndrome. The most frequent risk factors derived from the modified Wells Score RAM (Table 3) included: swelling of the entire leg (79.86%), major surgery or recently bedridden (55.56%), and calf swelling of at least 3 cm greater than the asymptomatic side (35.42%). Medical comorbidities (39.74%), elective Caesarean section (33.77%), and immobility (25.17%) were the primary risk factors identified from the RCOG RAM (Table 4).
 |
Table 2 VTE Risk Factors in Caprini RAM |
 |
Table 3 Risk Factors in Modified Wells Score RAM of Patients with DVT |
 |
Table 4 VTE Risk Factors in RCOG RAM |
The distributions of VTE patients by risk level and cumulative risk score are listed in Table 5. According to the Caprini model, more than half (53.64%) of the study population was classified into the highest risk level (score ≥ 5), 33.11% were classified as high-risk level (score 3–4), 12.58% as moderate-risk (score 2), and only 2 (0.66%) patient was assessed to have a low-risk (score 1) for VTE. Consistent with the Caprini model, only 2 (0.69%) patient was classified as low risk of VTE in the Wells Score models. Most patients (59.03% and 66.23%) were classified as moderate-risk patients in the Wells Score and RCOG models.
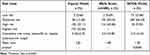 |
Table 5 Classification of VTE Patients by Risk Level and Cumulative Risk Score in Three RAMs |
However, the number of individuals evaluated by each risk assessment model varied. Figure 1 shows a Venn diagram that illustrates the concordance analysis of risk identification for all VTE patients evaluated by each model. 71.52% of the population was classified into the moderate or higher risk level by all three algorithms, and no patients were identified by only one RAM.
 |
Figure 1 Concordance analysis in patients classified as moderate or higher risk level in three RAMs by Venn diagram. |
Both the frequency and percentage of patients with VTE classified into moderate or above risk levels by the Caprini model were significantly higher when compared with the other two RAMs (p < 0.05, Friedman Test). Thus, the Caprini model classified more patients into moderate or above-risk levels.
Classification of Different Risk Levels by Caprini Model, Wells Score, and RCOG Model in Antepartum and Postpartum Patients
Two antepartum patients and zero postpartum patients were categorized to the low-risk level according to the Caprini model and the Wells Score (Table 6). This contrasts with the RCOG model in which more patients were assessed as being a low risk (antepartum/postpartum, 21.13% / 26.25%). Figure 2 shows the number of antepartum and postpartum patients at moderate or above-risk levels identified by the Caprini, Wells Score, and RCOG models. 140 of the 142 antepartum patients were categorized at moderate or above-risk levels by the Caprini model, 134 in the Wells Score model, and 112 in the RCOG model, respectively. And the number of postpartum patients at moderate or above-risk levels identified by the Caprini, Wells Score, and RCOG models were 160, 152, and 118. 53 (74.65%) of the 71 antepartum VTE patients and 55 (68.75%) of the 80 postpartum patients were classified as a moderate or high-risk level by all three algorithms.
 |
Table 6 Classification of Risk Level for Patients During Antepartum and Postpartum by Three Models |
 |
Figure 2 Venn diagrams classified the concordance analysis of antepartum (top) and postpartum (bottom) patients into moderate or higher risk levels for three RAMs. |
The average Wells cumulative risk score in postpartum patients was higher than that in antepartum patients (2.61 ± 0.98 vs 1.97 ± 0.86 respectively, p < 0.05, T-Test), but the cumulative risk score for the Caprini and RCOG models was not significant (p > 0.05, T-Test). As a consequence, the predictive value of risk assessment between two subgroups was statistically significant in the Wells Score model (p < 0.05, Mann–Whitney U-Test). However, according to the Friedman Test results (p < 0.05), the Caprini model classified antepartum patients into the higher risk level more effectively than the other two RAMs, same in the postpartum subgroup (p < 0.05, Friedman Test).
Discussion
Among the three RAMs, our study demonstrated that the Caprini risk assessment model more effectively stratifies VTE patients into moderate or higher risk levels in the peripartum and particularly postpartum. In patients classified as a moderate or higher risk for VTE, mechanical and/or pharmacological thromboprophylaxis is recommended according to guidelines. Our results are essential for obstetricians because this is the first study that assessed and evaluated the predictive value of three different RAMs among Chinese maternity patients with VTE. The Caprini model is a practical and effective risk assessment model for VTE, which might help reduce the inappropriate use of thromboprophylaxis in China. It can also be used as an educational tool to help draw attention to maternal patients with a high risk of VTE and prescribe appropriate prophylaxis.
We have previously shown that the prevalence of the peripartum thromboembolic disease is 0.13% in the regions of the Guangdong Province.11 By extrapolating from an approximate annual 3000–4000 deliveries in Guangzhou hospitals during the past decade, the incidence of symptomatic VTE during pregnancy and the postpartum determined from our study would be roughly 0.18%, which is below previously reported data (ranges from 0.245–0.325%).12,13,15 Several reasons may account for such low incidences. Firstly, many of the patients in our study had symptomatic VTE, and since there was no systematic screening for asymptomatic VTE, cases may not have been identified. Samama et al21 reported that only 6% of DVT among medical patients was symptomatic and demonstrated that asymptomatic VTE was much more common than symptomatic VTE. Secondly, DVT occurs in Asian populations at a lower rate than in European and American populations due to genetic predispositions and racial differences.16,27 In this study, the lack of patients with a family history of VTE may result from racial differences in genetic polymorphisms. However, understanding the reasons for racial differences in VTE can help develop strategies to minimize VTE in Chinese populations. Finally, and most importantly, obstetricians or physicians in developing countries such as China may not pay enough attention to maternal thrombosis disease and do not fully understand the risk factors for VTE, leading to missed diagnoses of VTE and the underuse of prophylaxis. It has been reported that the rate of missed diagnoses exceeds 80% in much of China, which is much higher than that in western countries.19 Consistent with the poor use of prophylaxis reported in the literature,7,23,26,28 only 12.6% of patients received comprehensive thromboprophylaxis before they were diagnosed with VTE in our study, showing insufficient awareness of VTE risk and VTE prophylaxis in the Chinese health system.
The Caprini risk assessment model was derived more than a decade ago and has been validated clinically in surgical and medical settings in western and Chinese populations. Bahl et al1 performed a retrospective study that included 8216 surgical in-patients and found that risk level was associated with VTE. The incidence of VTE within 30 days after surgery increased with risk level: 1.94% in the highest risk level, 0.97% in the high, 0.70% in the moderate, and 0% in the low groups. The difference in distribution between high and highest risk levels was statistically significant (p < 0.001), while no significance was found between low and moderate risk levels. Pannucci et al17 compared and validated the 2010 Caprini model and the 2005 Caprini model in 3334 plastic surgical patients and showed that the 2005 Caprini model was more effective at separating the lowest and highest-risk patients. Zhou et al28 performed a retrospective comparison of the Caprini model with the other two RAMs (the Kucher model14 and the Padua prediction score2) in unselected Chinese hospitalized patients: 78.4% of the patients diagnosed with VTE were classified in the high or above risk levels by the Caprini model with a cumulative risk score of more than 3, which was significantly higher than those classified by the two other models.
In our study, we used two notable published RAMs and one RAM adopted from clinical guidelines to retrospectively assess the VTE risk of maternal patients diagnosed with VTE during pregnancy and postpartum. The majority of the patients were stratified into moderate or higher risk levels by the Caprini model and the Wells Score model (99.34% and 99.31%, respectively). Still, in the RCOG model, a significant proportion of the patients remained in the low-risk category (23.84%), for which prophylaxis is not recommended. Although the RCOG model was adapted from an obstetric guideline for thromboprophylaxis, it was based on only 23 risk factors (compared with almost 40 risk factors in the Caprini model). Thus it was less sensitive; ie, some features critical to identifying risk may be absent in this model. Furthermore, to the best of our knowledge, this is the first study evaluating the RCOG RAM, which was derived from clinical guidelines based on European population studies and could incorporate assumptions invalid for the Chinese population. Further validation studies for the RCOG model are needed before this model can be recommended in Chinese populations.
In both antepartum and postpartum patients, the Caprini model classifies more patients as high or highest risk levels (73.24%, and 98.75%, respectively), particularly in the postpartum. In addition to a hypercoagulable state and venous distension, typical during pregnancy, childbirth can lead to increased tissue trauma due to surgery and prolonged bed rest, both of which increase thrombotic risk. If both vaginal delivery and Caesarean section are classified as tissue trauma with surgical procedures, our findings are consistent with previous reports.28 Specifically, it has been reported that compared to nonsurgical patients, the Caprini model was more effective at assessing VTE risk among surgical patients (average risk score, 5.71±2.54 vs 4.36±2.51, p=0.001).
As a retrospective study of patients with VTE, our study has limitations. Firstly, and principally, it is a retrospective study and lacked a negative control group without VTE during pregnancy and postpartum. Therefore, the study only evaluates the false negative rate for each risk assessment model, which means it is impossible to assess false positive rates. Further work to evaluate the false positive rate is required and would need a prospective study to be carried out. Only when both parameters are known can the best model be fully determined. Secondly, a retrospective RAM score calculated after patients had VTE symptoms may overestimate the patient’s cumulative risk score and risk level. In particular, symptom-related factors will only be known after the onset of VTE symptoms, which may cause the Caprini model to appear more sensitive. The Caprini model contains more indicators than other models, which might be why its prediction value is higher than other models, but it’s more complex. It is possible to overestimate the risk of maternal thrombosis. This may lead to increased thromboprophylaxis and treatment and put pregnant women at increased risk of bleeding. Thirdly, risk assessments were conducted by retrospectively reviewing electronic medical records and may not fully represent the risk factors that could have been identified and recorded. Furthermore, thrombophilia tests were not routinely performed on most patients, so some relevant risk factors in the study population cannot be assessed. As a result, the risk level of some patients may have been underestimated. Because of the low incidence of VTE in the Asian population, more patients from more centers need to be recruited for future validation. Further study and a risk assessment model for the Chinese population are needed, combing the more appropriate indicators from all existing models.
In conclusion, our study demonstrated that the Caprini risk assessment model is an effective prediction tool for peripartum women, especially postpartum, which can assist obstetricians or physicians in identifying potential risk patients and guide prophylaxis decisions. However, since the methodology cannot assess the false positive rate, it cannot be known whether the reason for the effectiveness of this model is a complete lack of specificity. The RCOG model was not particularly useful in Chinese VTE patients during pregnancy and postpartum. However, a multicenter prospective validation study of the RCOG model will provide future insight into its accuracy. Thus, appropriate calibrations could be amended into each model and validate their adoption into Chinese maternal populations as a routine clinical tool.
Abbreviations
VTE, venous thromboembolism; DVT, deep venous thrombosis; PE, pulmonary embolism; RAMs, risk assessment models; BMI, body mass index; RCOG, Royal College of Obstetricians and Gynecologists.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Informed Consent
This study was performed in line with the principles of the Declaration of Helsinki. The Ethics Committee of Nanfang Hospital of Southern Medical University and the Third Affiliated Hospital of Guangzhou Medical University approved. Informed consent was obtained from all individual participants included in the study.
Acknowledgments
We greatly acknowledge the collaboration received from the staff of the Medical Records Department of Nanfang Hospital of Southern Medical University and the Third Affiliated Hospital of Guangzhou Medical University. This study was performed at Nanfang Hospital of Southern Medical University and Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong Province, China.
Funding
The study is supported by the Health Appropriate Technology Promotion Project of Guangdong Province (No.202206280010517553), the Health Science and Technology Project of Guangzhou (No.20231A010057), and the Research Project of Population and Family Planning Commission of Guangdong Province, China (No. 20110330).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Bahl V, Hu HM, Henke PK, Wakefield TW, Campbell DJ, Caprini JA. A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg. 2010;251(2):344–350. doi:10.1097/SLA.0b013e3181b7fca6
2. Barbar S, Noventa F, Rossetto V, et al. A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua prediction score. J Thromb Haemost. 2010;8(11):2450–2457. doi:10.1111/j.1538-7836.2010.04044.x
3. Blanco-Molina A, Trujillo-Santos J, Criado J, et al. Venous thromboembolism during pregnancy or postpartum: findings from the RIETE registry. Thromb Haemost. 2007;97(2):186–190. doi:10.1160/TH06-11-0650
4. Cantwell R, Clutton-Brock T, Cooper G, et al. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 2006–2008. The eighth report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG. 2011;118(Suppl 1):1–203. doi:10.1111/j.1471-0528.2010.02847.x
5. Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51(2–3):70–78. doi:10.1016/j.disamonth.2005.02.003
6. Cavazza S, Rainaldi MP, Adduci A, Palareti G. Thromboprophylaxis following cesarean delivery: one site prospective pilot study to evaluate the application of a risk score model. Thromb Res. 2012;129(1):28–31. doi:10.1016/j.thromres.2011.06.028
7. Chopard P, Dorffler-Melly J, Hess U, et al. Venous thromboembolism prophylaxis in acutely ill medical patients: definite need for improvement. J Intern Med. 2005;257(4):352–357. doi:10.1111/j.1365-2796.2005.01455.x
8. Clark SL, Belfort MA, Dildy GA, Herbst MA, Meyers JA, Hankins GD. Maternal death in the 21st century: causes, prevention, and relationship to cesarean delivery. Am J Obstet Gynecol. 2008;199(1):31–36, 91–92. doi:10.1016/j.ajog.2008.03.007
9. Friedman AM, Ananth CV, Lu YS, D’Alton ME, Wright JD. Underuse of postcesarean thromboembolism prophylaxis. Obstet Gynecol. 2013;122(6):1197–1204. doi:10.1097/AOG.0000000000000007
10. Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LR. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann Intern Med. 2005;143(10):697–706. doi:10.7326/0003-4819-143-10-200511150-00006
11. Huang QT, Zhong M, Wang CH, et al. Prevalence and major risk factors of peripartum thromboembolic disease in different regions of Guangdong province. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33(4):413–417.
12. Jacobsen AF, Skjeldestad FE, Sandset PM. Incidence and risk patterns of venous thromboembolism in pregnancy and puerperium--a register-based case-control study. Am J Obstet Gynecol. 2008;198(2):231–233. doi:10.1016/j.ajog.2007.08.041
13. James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. 2006;194(5):1311–1315. doi:10.1016/j.ajog.2005.11.008
14. Kucher N, Koo S, Quiroz R, et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352(10):969–977. doi:10.1056/NEJMoa041533
15. Liu S, Rouleau J, Joseph KS, et al. Epidemiology of pregnancy-associated venous thromboembolism: a population-based study in Canada. J Obstet Gynaecol Can. 2009;31(7):611–620. doi:10.1016/S1701-2163(16)34240-2
16. Neki R, Fujita T, Kokame K, et al. Genetic analysis of patients with deep vein thrombosis during pregnancy and postpartum. Int J Hematol. 2011;94(2):150–155. doi:10.1007/s12185-011-0902-z
17. Pannucci CJ, Barta RJ, Portschy PR, et al. Assessment of postoperative venous thromboembolism risk in plastic surgery patients using the 2005 and 2010 caprini risk score. Plast Reconstr Surg. 2012;130(2):343–353. doi:10.1097/PRS.0b013e3182589e49
18. Pomp ER, Lenselink AM, Rosendaal FR, Doggen CJ. Pregnancy, the postpartum period and prothrombotic defects: risk of venous thrombosis in the MEGA study. J Thromb Haemost. 2008;6(4):632–637. doi:10.1111/j.1538-7836.2008.02921.x
19. Pulmonary Vascular Disease Study Group Of Chinese Society Of Cardiology, Chinese College Of Cardiovascular Physicians(CCCP). Chinese expert consensus on the diagnosis and treatment of acute pulmonary thromboembolism. Zhonghua Nei ke Za Zhi. 2010;49(1):74–81.
20. Royal College Of Obstetricians And Gynaecologists. Reducing the Risk of Thrombosis and Embolism During Pregnancy and the Puerperium Green-Top Guideline No. 37a (2015, Pp.). London: RCOG; 2015.
21. Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. prophylaxis in medical patients with enoxaparin study group. N Engl J Med. 1999;341(11):793–800. doi:10.1056/NEJM199909093411103
22. Simpson EL, Lawrenson RA, Nightingale AL, Farmer RD. Venous thromboembolism in pregnancy and the puerperium: incidence and additional risk factors from a London perinatal database. BJOG. 2001;108(1):56–60. doi:10.1111/j.1471-0528.2001.00004.x
23. Tapson VF, Decousus H, Pini M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: findings from the international medical prevention registry on venous thromboembolism. Chest. 2007;132(3):936–945. doi:10.1378/chest.06-2993
24. Wells PS, Anderson DR, Bormanis J, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997;350(9094):1795–1798. doi:10.1016/S0140-6736(97)08140-3
25. Wells PS, Anderson DR, Rodger M, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003;349(13):1227–1235. doi:10.1056/NEJMoa023153
26. Yu HT, Dylan ML, Lin J, Dubois RW. Hospitals’ compliance with prophylaxis guidelines for venous thromboembolism. Am J Health Syst Pharm. 2007;64(1):69–76. doi:10.2146/ajhp060115
27. Zakai NA, McClure LA. Racial differences in venous thromboembolism. J Thromb Haemost. 2011;9(10):1877–1882. doi:10.1111/j.1538-7836.2011.04443.x
28. Zhou HX, Peng LQ, Yan Y, et al. Validation of the caprini risk assessment model in Chinese hospitalized patients with venous thromboembolism. Thromb Res. 2012;130(5):735–740. doi:10.1016/j.thromres.2012.08.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
