Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 10 » Issue 1
Comparative effectiveness of budesonide/formoterol combination and tiotropium bromide among COPD patients new to these controller treatments
Authors Trudo F, Kern D , Davis J, Tunceli O, Zhou S, Graham E, Strange C , Williams S
Received 17 June 2015
Accepted for publication 5 August 2015
Published 28 September 2015 Volume 2015:10(1) Pages 2055—2066
DOI https://doi.org/10.2147/COPD.S90658
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Frank Trudo,1 David M Kern,2 Jill R Davis,1 Ozgur Tunceli,2 Siting Zhou,2 Emma L Graham,3 Charlie Strange,4 Setareh A Williams1
1AstraZeneca Pharmaceuticals LP, 2HealthCore, Inc., Wilmington, DE, USA; 3AstraZeneca Pharmaceuticals LP, Alderley Park, Cheshire, UK; 4Division of Pulmonary and Critical Care Medicine, Department of Medicine, Medical University of South Carolina, Charleston, SC, USA
Background: Inhaled corticosteroid/long-acting β2-agonist combinations and/or long-acting muscarinic antagonists are recommended first-line therapies for preventing chronic obstructive pulmonary disease (COPD) exacerbation. Comparative effectiveness of budesonide/formoterol combination (BFC, an inhaled corticosteroid/long-acting β2-agonist combination) vs tiotropium (long-acting muscarinic antagonist) in the US has not yet been studied.
Methods: Using US claims data from the HealthCore Integrated Research Environment, COPD patients (with or without comorbid asthma) ≥40 years old initiating BFC or tiotropium between March 1, 2009 and February 28, 2012 and at risk for exacerbation were identified and followed for 12 months. Patients were propensity score matched on demographics and COPD disease severity indicators. The primary outcome was time to first COPD exacerbation. Secondary outcomes included COPD exacerbation rate, health care resource utilization, and costs.
Results: The Cox proportional hazards model for time to first exacerbation yielded a hazard ratio (HR) of 0.78 (95% CI =[0.70, 0.87], P<0.001), indicating a 22% reduction in risk of COPD exacerbation associated with initiation of BFC versus tiotropium. A post hoc sensitivity analysis found similar effects in those who had a prior asthma diagnosis (HR =0.72 [0.61, 0.86]) and those who did not (HR =0.83 [0.72, 0.96]). BFC initiation was associated with lower COPD-related health care resource utilization and costs ($4,084 per patient-year compared with $5,656 for tiotropium patients, P<0.001).
Conclusion: In COPD patients new to controller therapies, initiating treatment with BFC was associated with improvements in health and economic outcomes compared with tiotropium.
Keywords: COPD, inhaled corticosteroid/long-acting β2-agonist combinations, long-acting muscarinic antagonist, comparative effectiveness, administrative claims
Introduction
In 2011, >13 million adults in the US reported a chronic obstructive pulmonary disease (COPD) diagnosis.1 Current research continues to address the dissociation between guideline recommendations for managing COPD and clinical practice.2 For patients with a history of exacerbation, inhaled corticosteroid/long-acting β2-agonist combinations (ICS/LABA) and/or long-acting muscarinic antagonist (LAMA) are recommended first-line therapies.3
While the effectiveness of ICS/LABA therapy on preventing COPD exacerbations has been studied in detail compared with placebo, ICS monotherapy, and LABA monotherapy,4–10 very little clinical research has been conducted on the direct comparison between ICS/LABA therapy and tiotropium. In fact, there exists only one clinical trial that compared the effectiveness of fluticasone propionate/salmeterol combination (FSC) 500/50 μg twice daily to tiotropium 18 μg once daily, showing no difference in exacerbation rates.11 In addition to the lack of clinical trial data, few studies have compared the real-world effectiveness of tiotropium and ICS/LABA, and these studies have not accounted for baseline differences in COPD disease activity, a key predictor of future events.12,13 In the US, no published studies have compared the effectiveness of the ICS/LABA combination therapy budesonide/formoterol combination (BFC) with tiotropium, whereas only one study outside of the US has been published.14
The goal of this study was to evaluate real-world effectiveness of BFC compared to tiotropium during the 12 months after initiation of therapy in propensity score matched cohorts. The primary measure of effectiveness was time to first COPD exacerbation, while secondary measures included COPD exacerbation rates, health care resource utilization, health care costs, respiratory medication use, and adherence.
Materials and methods
Data source
This retrospective cohort study (NCT01917643)15 utilized claims data for commercially insured individuals from the HealthCore Integrated Research Environment (HIRE). The HIRE contains a diverse spectrum of longitudinal claims data for >32 million lives. The terms of the Research Exception provisions of the Privacy Rule, 45 CFR 164.514(e) exempted Institutional Review Board approval for this non-experimental study, which was fully Health Insurance Portability and Accountability Act (HIPAA) compliant. Patient confidentiality was maintained throughout and all data remained anonymous; researchers only had access to the required datasets following the removal of patient identifiers.
Study population
Eligible patients comprised COPD patients 40 years or older initiating BFC (160/4.5 μg)16 or tiotropium (18 μg),17 at risk for an exacerbation, and with health plan enrollment at any point between March 1, 2009 and February 28, 2012. The study intake period was chosen to coincide with the US Food and Drug Administration approval of BFC COPD indication on February 27, 2009, and allowed 12 months of follow-up, as data were available through February 28, 2013. The date of the first pharmacy claim for either of the study medications was defined as the index date. Patients were naïve to ICS/LABA and LAMA therapies in the year prior to the index date. Individuals at risk for an exacerbation had one or more inpatient hospitalizations with a primary diagnosis of COPD, emergency department (ED) visits with a COPD diagnosis, and/or prescription fills for an oral corticosteroid (OCS) within 10 days of an outpatient COPD visit in the 12 months preceding the index date. We excluded patients with ≥180 days of OCSs, or a cancer diagnosis (≥2 claims <60 days apart with ICD-9 diagnosis code 140.xx–209.3x, 230.xx–234.xx) during the previous 12 months. Individuals diagnosed with asthma during the baseline period were not excluded from this study.
Study treatment and follow-up
Patients were assigned to a treatment group based on the prescribed therapy filled on the index date and excluded if prescriptions for both appeared on the index date. All patients were followed for a full 12 months following treatment initiation; thus, individuals who died or left the health plan prior to 12 months of follow-up were excluded from the study.
Outcomes
Primary outcome
The primary outcome measure was time to first COPD exacerbation during the 12 months following the index date. COPD exacerbation included an inpatient hospitalization with a primary COPD diagnosis, an ED visit with any COPD diagnosis, or a pharmacy claim for OCSs and/or antibiotics within 10 days after an outpatient visit for COPD.
Sensitivity and subgroup analyses
The study included two pre-specified sensitivity analyses and two pre-specified subgroup analyses exploring the comparative impact of BFC and tiotropium bromide on time to first COPD exacerbation in the 12 months following the index date. In the primary analysis, the date of a patient’s first COPD exacerbation was the event date. Patients who had no exacerbation were censored 12 months post the index date. One sensitivity analysis censored patients (ie, stopped follow-up) if they filled a study class medication different from their index drug (referred to as “treatment modification”; BFC patients were censored if they filled any other ICS/LABA or any LAMA; tiotropium patients were censored if they filled any other LAMA or any ICS/LABA). Another sensitivity analysis started the follow-up 31 days post the index date to allow adequate exposure to the study medication before assessing outcomes. A subgroup analysis examined differences in the primary outcome separately for patients who did and did not experience treatment modification. Another subgroup analysis evaluated outcomes in patients of age 65 years and older.
To account for potential differential effects of the index medication due to possible comorbid asthma, an interaction model was constructed as a post hoc sensitivity analysis. The interaction model is identical to the primary outcome model with the addition of the main effect of a prior asthma diagnosis and a term for the interaction between index drug and having at least one prior asthma diagnosis. Results stratified by asthma group (those with no prior asthma diagnosis and those with ≥1 prior diagnosis, separately) were obtained from the interaction model. A stratified Kaplan–Meier analysis was also performed to obtain the median time to exacerbation.
Secondary outcomes
We measured COPD exacerbation rate, which was defined as the total number of COPD exacerbations during the 12-month post-index period divided by the total number of person years for each treatment group. ED visits resulting in a hospital stay were counted as an inpatient hospitalization only. OCS or antibiotic fills occurring within 14 days of an ED visit or inpatient hospitalization were counted as a single event. Similar to the primary outcome above, an interaction model – including an interaction term between prior asthma diagnosis and the index medication – was constructed as a post hoc sensitivity analysis of the COPD exacerbation rate outcome, and results stratified by asthma group were obtained.
Other secondary outcomes included respiratory medication fill, COPD-related and all-cause health care utilization and health care costs in the 12 months following the index date. The COPD-related utilization outcome captured outpatient visits with at least one COPD diagnosis code, length of intensive care unit and COPD-related hospital stays and COPD-related procedures in addition to the COPD-related hospital stays and ED visits contained in the primary outcome. COPD-related costs included the costs of inpatient hospitalizations with a primary diagnosis of COPD and any other episode with a diagnosis for COPD, and any COPD medication, including the index therapy. All costs were adjusted to 2012 using the current consumer price index provided by the Bureau of Labor Statistics for Medical Care Services18 and categorized as plan or patient paid. Adherence was documented as proportion of days covered (PDC), defined as the number of days for which the patient received a supply of medication during the post-index period divided by the days in the post-index period.19 An analysis of time to first treatment modification was considered exploratory given the small number of patients expected to have a treatment modification.
Statistical analysis
To reduce selection bias, logistic regression-based propensity score (the probability of receiving BFC conditional on observed baseline characteristics) matching was used to create the analytic cohorts from patients meeting inclusion criteria.20–22 We specified prospectively that cohorts were to balance on age, sex, prior asthma diagnosis, COPD-related hospitalizations, COPD-related ED visits, OCS fills, antibiotic fills, short-acting β2-agonist (SABA) and/or short-acting β2-agonist/short-acting muscarinic antagonist (SABA/SAMA) fills, and LABA fills, during the pre-index period. While considered optional, balance also was achieved for an additional set of variables (Table 1 footnotes). Patients were matched via a Greedy nearest neighbor 1-to-1 matching technique without replacement. Treatment cohorts were considered well balanced for a given variable if the statistical significance of the difference between groups was P≥0.05. The minimum sample size was calculated as 1,111 patients per group to detect a true hazard ratio (HR) of 0.80 with 90% power.
A Cox proportional hazards model was used for time to first exacerbation. Due to successful matching on key potential confounders and the lack of significant improvement to the primary outcome model when considering additional potential covariates, the final model was unadjusted. HRs and 95% confidence intervals are presented. For the primary outcome, and the corresponding sensitivity and subgroup analyses, patients were followed for 12 months or until their first COPD exacerbation, whichever came first. All analyses were based on index medication cohort, regardless of treatment changes following the index date.
A negative binomial model with log link was used to examine the impact of therapy on exacerbation rate and other count outcomes, while logistic regression was used for dichotomous outcomes. Gamma regression was applied to cost outcomes and ordinary least squares regression to PDC. All secondary outcomes included a full 12 months of follow-up and were adjusted for the analogous pre-index variable; for example, the post-index cost model controlled for pre-index costs. Cox regression was used to explore time to treatment modification. Intent-to-treat populations were used for all analyses. All outcomes and statistical analysis methods were defined a priori in the study protocol, and no adjustment was made for multiple testing. All analyses used SAS version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
There were 136,706 patients with at least one prescription for BFC or tiotropium between March 1, 2009 and February 28, 2012. The final sample included 4,051 unmatched patients: 1,381 BFC and 2,670 tiotropium (Figure 1).
Matching
Propensity score matching yielded 1,198 patients in each group. After matching, there was a similar distribution of propensity scores for the two treatment groups, indicating successful matching. All pre-specified variables were well balanced, including those that were optional (Table 1).
Demographics and baseline characteristics
Matched patients in BFC and tiotropium cohorts had a mean age of 63 years, and 56% were female (Table 1). Patients had similar rates of diagnosed comorbid conditions during the 12-month pre-index period, including hypertension (65% BFC and 66% tiotropium), asthma (41% in both), coronary artery disease (29% in both), diabetes (25% in both), and pneumonia (25% BFC, 26% tiotropium). Rates of prior respiratory medication use were also similar, including at least one fill of OCS, ICS, SABA, SABA/SAMA combination, or leukotriene receptor antagonists. The most recent exacerbation prior to the index date occurred at a median 25 days prior to index, with 72% of patients experiencing an exacerbation within 3 months of the index date.
Primary outcome
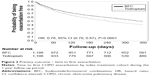
There were 51% of BFC patients and 59% of tiotropium patients with at least one exacerbation during follow-up. The Cox proportional hazards model for time to first exacerbation yielded a HR of 0.78 (95% CI =[0.70, 0.87], P<0.001) indicating a 22% reduction in risk of COPD exacerbation associated with initiation of BFC compared with initiation of tiotropium (Figure 2, Table 2).
The results of all the sensitivity and subgroup analyses were consistent with the primary analysis result, showing that the time to first COPD exacerbation was longer in the BFC cohort: censoring for treatment modification (HR =0.79 [0.71, 0.89], P<0.001), starting follow-up on day 31 (HR =0.78 [0.70, 0.87], P<0.001), subgroups of patients who did not modify treatment (HR =0.85 [0.74, 0.97], P=0.017), individuals who modified treatment (HR =0.88 [0.72, 1.08], P=0.229), and patients 65 years old or older (HR =0.84 [0.71, 0.98], P=0.031) (Table 2).
The interaction between a prior asthma diagnosis and index medication on the primary outcome was not found to be statistically significant (P=0.2195), and the results by asthma status were consistent with the primary analysis result; the time to first COPD exacerbation was longer in the BFC cohort for those with a prior asthma diagnosis (HR =0.72 [0.61, 0.86], P<0.001) and without (HR =0.83 [0.72, 0.96], P=0.011).
Secondary outcomes
Exacerbation rates
Initiation of BFC compared with tiotropium was also associated with reduced exacerbation rates (BFC =1.23 per patient-year, tiotropium =1.50 per patient-year, rate ratio (RR) =0.82 [0.73, 0.91]). Evaluation of exacerbation rates by type of exacerbation event showed fewer exacerbations for BFC: COPD-related ER visits (RR =0.76 [0.60, 0.95]), COPD-related outpatient visits plus antibiotic and/or OCS (RR =0.83 [0.73, 0.94]), and COPD-related inpatient hospitalizations (RR =0.80 [0.59, 1.09]) (Figure 3). In the sensitivity analysis, the interaction between a prior asthma diagnosis and index medication on the primary outcome was not found to be statistically significant (P=0.176), and the direction of results by asthma status was consistent with the primary analysis result. The rate of exacerbation was reduced in individuals initiating BFC compared with tiotropium for those with asthma (RR =0.75 [0.63, 0.89]) and without (RR =0.88 [0.76, 1.02]), although the effect was no longer statistically significant in the latter group.
Cost and health care utilization
BFC patients generally had less COPD-related utilization compared with tiotropium patients across all places of service (Table 4). All-cause health care utilization was similar between the two groups; however, the cumulative effect of small differences across service types contributed to lower mean all-cause health care costs for BFC patients (Table 5, $21,681 for BFC vs $24,374 for tiotropium; adjusted mean difference =−$2,702 [−$4,160, −$1,119]). Likewise, COPD-related mean costs were lower for BFC patients at $4,084 compared with $5,656 for tiotropium patients (adjusted mean difference =−$1,360 [−$1,715, −$967]).
Adherence
The BFC cohort filled their index medication an average of 3.3 times during the 12-month follow-up period compared with 4.3 times for tiotropium patients (adjusted mean difference =−1.01 [−1.22, −0.77]). Forty-one percent of BFC patients filled their index medication one time, compared to 31% of tiotropium patients. This resulted in a low PDC in both groups, but especially in BFC patients (0.28 on average [SD =0.25] vs 0.37 [SD =0.30] for tiotropium).
Other COPD medication fills
Prescription fills of most COPD medications were similar between groups (Table 3). An exploratory analysis indicated that treatment modification during the post-index period occurred twice as often in tiotropium patients (37%) as in BFC patients (18%), supported by Cox regression analysis of time to first treatment modification (HR =0.41 [0.35, 0.49]).
Discussion
Results of this real-world COPD study may help to inform treatment decisions for COPD patients at risk of an exacerbation. The outcome of prolonged time to first exacerbation with an inhaled ICS/LABA (BFC) compared to a LAMA (tiotropium) is clinically meaningful and important to patients, clinicians, and health care systems. While this is a non-randomized retrospective study using claims data, propensity score matching to define the study cohorts provides confidence that the groups were comparable at index evaluation and supports a difference in COPD exacerbation protection between the two medication classes.
Initiation of BFC was associated with a reduced risk of COPD exacerbations compared with the tiotropium group across all sensitivity and subgroup analyses. Furthermore, this association was observed for all definitions of a COPD exacerbation used in this study. Since COPD exacerbation is the most costly component of COPD care,23 it was not surprising that lower COPD-specific health care utilization and cost followed the use of BFC.
To our knowledge, there exist no published studies comparing the effectiveness of BFC and tiotropium in a US population. One study from Canada found that those treated with BFC had a significantly lower rate of COPD hospitalizations compared with those treated with tiotropium; however, the overall rate of COPD exacerbations was similar between the two groups.14 Our results are similar with a study that compared exacerbations and health care costs between FSC and tiotropium.13 That study found improved outcomes in exacerbations and costs for patients receiving FSC therapy. Recent Cochrane Collaboration Systematic Reviews have emphasized the need for additional comparative effectiveness studies for LABA combination therapies versus tiotropium as well as direct head-to-head comparisons of alternative combined therapy inhalers.24,25 While observational data is lacking, there is also a sparsity of clinical trial data. Only one study from a clinical trial has been published comparing the effectiveness between ICS/LABA and tiotropium.11 The study found no difference in exacerbation rates; however, the authors note that tiotropium patients had a significantly higher likelihood of dropping out and thus the null finding may be due to a healthy survivor bias. A Cochrane Review of the study concluded that due to a high proportion of missing outcome data large enough to cause a clinically relevant bias, the relative efficacy of the two drugs is uncertain.25
A significant proportion (41%) of this COPD population had at least one diagnosis code of asthma during the pre-index period, with an equal proportion within each treatment group. These patients were not excluded because the goal of this study was to include a COPD population reflective of the real world, and can help generalize results to a wider population than is typically included in clinical trials. It was of interest to see how inclusion of these patients may have affected our results, even with equal proportions in each group. Although power was reduced due to smaller sample sizes, it was found that the time to first COPD exacerbation was longer in patients initiating BFC compared with tiotropium for those with a prior asthma diagnosis and those without. While the magnitude of the estimate was attenuated within patients without a prior asthma diagnosis (HR =0.83 vs 0.72 in those with a prior diagnosis), there remained a 17% risk reduction of a COPD exacerbation for those not diagnosed with asthma who initiated BFC compared with tiotropium. Furthermore, the effect remained significant within each of the two groups, and the difference in effect between the two groups was not found to be statistically significant according to the interaction term. Similar results were observed in the sensitivity analysis of exacerbation rates, though the effect was no longer statistically significant in those without asthma, likely due to the reduced power resulting from a smaller sample size in the subgroup compared to the overall analytic sample.
Differences in outcomes occurred despite low refill rates. There may be some mitigation of these low rates by drug sampling, international drug purchases, or medication sharing that is not observable in an administrative database. However, the impact on exacerbation reduction seen in this observational study may not fully reflect the impact of ICS/LABA and LAMA medications on exacerbations and costs in a system that improved adherence to these medications.
Limitations
This study was conducted as an intent-to-treat analysis and required only one prescription for either study medication, and patients were not required to be continuously taking therapy during the 1-year follow-up period. Therefore, interpretation is restricted to differences in time to first exacerbation within the first year after initiation of either BFC or tiotropium, and not differences in time to first exacerbation of patients currently treated with either study medication.
All patients were required to have 12 months of pre- and post-index health plan enrollment, resulting in selection of patients who survived and did not lose health plan coverage during follow-up. This may have resulted in a population that is relatively healthier, and thus less likely to have an exacerbation, than the general population of BFC and tiotropium users. However, this selection bias is not likely to have differentially affected the two treatment cohorts.
The study includes only individuals with medical insurance. The HIRE database is a US commercially insured data sample and is subject to the inherent biases of that population, and generalizability of the results is limited to a similar population. Results may vary in populations outside of the US (eg, where the labeled dose and formulation of BFC is different from the product in this study) and for those without commercial health insurance. While we cannot definitively prove the absence of bias in patient selection for this study, propensity score matching mitigates against significant differences in patient demographic or disease state characteristics that could influence outcomes.26,27 After matching, no statistically significant differences remained in variables of interest between patients in the two groups.
The inclusion of patients with possible comorbid asthma, while improving generalizability to a greater number of COPD patients, could also bias the results of the study. The use of OCS in conjunction with an outpatient visit coded for COPD was considered a COPD exacerbation; however, we could not determine the contribution of co-existent asthma in the decision to treat symptom worsening with systemic steroids. The use of BFC in the US is supported by indications in both asthma and COPD, whereas tiotropium use is driven by indications only in COPD.16,17,28 However, there is evidence that tiotropium significantly improves asthma symptoms and reduces asthma exacerbations when added to ICS or ICS/LABA therapy.29–33 Furthermore, in Europe, the use of tiotropium is indicated as an add-on for the treatment of asthma in those who are uncontrolled with ICS or ICS/LABA therapy,34 and is seeking similar approval in the US.35 Thus, while the inclusion of potential asthma patients may have biased results in favor of BFC, it is unlikely to account for the total magnitude of effect observed in this study, considering the ability of tiotropium to control asthma symptoms and reduce exacerbations. To address this potential limitation, a sensitivity analysis was conducted to test for an interaction between index medication and prior asthma diagnosis. Initiation of BFC was associated with a lower risk of COPD exacerbation, as measured by the time to first exacerbation, in those with and without asthma. While there seemed to be some difference in the magnitude of effect between the two subgroups, no significant interaction was found between the index medication and a prior asthma diagnosis.
Administrative claims data in general are subject to potential coding errors and inconsistencies, and may over-diagnose some conditions and under-diagnose others. Besides, the criteria for how a physician arrived at his or her diagnosis is unknown, and inpatient administered drugs are not present in the claims data. Additionally, a prescription claim date is the date a medication was filled, not necessarily the date a patient started treatment, although this date was assumed to be the beginning of the treatment. Lastly, clinical variables such as results of pulmonary function tests and smoking status were not available in the claims data.
Conclusion
This retrospective study compares outcomes for patients initiating therapy with BFC or tiotropium in a propensity score matched population. The results demonstrate significant improvements associated with BFC in timing and rate of COPD exacerbation, as well as cost and utilization of COPD-related health care services. This study of the comparative effectiveness of BFC and tiotropium in a US population provides supportive evidence for BFC to prevent exacerbation for COPD patients at risk for an exacerbation, consistent with the Global Initiative for Chronic Obstructive Lung Disease treatment guidelines.
Acknowledgments
AstraZeneca LP sponsored this study. The researchers had complete access to the de-identified data set and formulated the protocol, study design, and statistical analysis. The researchers had full authority over the administration of the study and over the decision to publish their findings. Researchers from both AstraZeneca and HealthCore were involved in the interpretation of results, preparation, and review of the manuscript prior to submission.
Disclosure
FT, JD, EG, and SW have disclosed that they are employed by AstraZeneca LP. DK, OT, and SZ have disclosed that they are employed by HealthCore, Inc., which received funding from AstraZeneca LP for this study. CS has been a consultant for AstraZeneca LP, CSL Behring, Grifols, PneumRx, Pulmonx, and Uptake Medical on the topic of COPD. The authors report no other conflicts of interest in this work.
References
Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance – United States, 1999–2011. Chest. 2013;144(1):284–305. | ||
Bosanquet N, Dean L, Iordachescu I, Sheehy C. The effectiveness gap in COPD: a mixed methods international comparative study. Prim Care Respir J. 2013;22(2):209–213. | ||
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD; 2015. Available from: http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015.pdf. Accessed February 12, 2015. | ||
Calverley P, Pauwels R, Vestbo J, et al. Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 2003;361(9356):449–456. | ||
Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–789. | ||
Calverley PM, Boonsawat W, Cseke Z, Zhong N, Peterson S, Olsson H. Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease. Eur Respir J. 2003;22(6):912–919. | ||
Hanania NA, Darken P, Horstman D, et al. The efficacy and safety of fluticasone propionate (250 microg)/salmeterol (50 microg) combined in the Diskus inhaler for the treatment of COPD. Chest. 2003;124(3):834–843. | ||
Jenkins CR, Jones PW, Calverley PM, et al. Efficacy of salmeterol/fluticasone propionate by GOLD stage of chronic obstructive pulmonary disease: analysis from the randomised, placebo-controlled TORCH study. Respir Res. 2009;10:59. | ||
Szafranski W, Cukier A, Ramirez A, et al. Efficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary disease. Eur Respir J. 2003;21(1):74–81. | ||
Zheng JP, Yang L, Wu YM, et al. The efficacy and safety of combination salmeterol (50 microg)/fluticasone propionate (500 microg) inhalation twice daily via accuhaler in Chinese patients with COPD. Chest. 2007;132(6):1756–1763. | ||
Wedzicha JA, Calverley PM, Seemungal TA, Hagan G, Ansari Z, Stockley RA. The prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromide. Am J Respir Crit Care Med. 2008;177(1):19–26. | ||
Briggs A, Spencer M, Wang H, Mannino D, Sin DD. Development and validation of a prognostic index for health outcomes in chronic obstructive pulmonary disease. Arch Intern Med. 2008;168(1):71–79. | ||
Dalal AA, Roberts MH, Petersen HV, Blanchette CM, Mapel DW. Comparative cost-effectiveness of a fluticasone-propionate/salmeterol combination versus anticholinergics as initial maintenance therapy for chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2011;6:13–22. | ||
Blais L, Forget A, Ramachandran S. Use of health care services in patients with chronic obstructive pulmonary disease (COPD) treated with budesonide/formoterol via dry powder inhaler (BUD/FM DPI) versus tiotropium [presented as an oral presentation]. Value Health. 2009;12(3):A19. | ||
AstraZeneca Pharmaceuticals. Comparative effectiveness of symbicort vs spiriva among COPD patients. Bethesda, MD: National Library of Medicine; 2014. Available from: https://clinicaltrials.gov/ct2/show/NCT01917643. ClinicalTrials.gov NLM Identifier: NCT01917643. Accessed February 13, 2015. | ||
AstraZeneca Pharmaceuticals. SYMBICORT Prescribing Information; 2010. [cited October 24, 2014]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/021929s021lbl.pdf | ||
Boehringer Ingelheim Pharmaceuticals. SPIRIVA HandiHaler Prescribing Information; 2011. [cited February 13, 2015]. Available from: http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021395s033lbl.pdf | ||
Bureau of Labor Statistics. Series CUUR0000SAM2; 2013. Available from: http://www.bls.gov/cpi/home.htm. Accessed June 16, 2015. | ||
Nau DP. Proportion of Days Covered (PDC) as a Preferred Method of Measuring Medication Adherence; 2014. Available from: http://www.pqaalliance.org/on. Accessed October 20, 2014 | ||
Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. 2008;27(12):2037–2049. | ||
Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am J Epidemiol. 2010;172(9):1092–1097. | ||
Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. In: SAS SUGI 26, 2001, Paper 214–226. Available from: http://www2.sas.com/proceedings/sugi26/p214-26.pdf. Accessed August 20, 2015. | ||
Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764. | ||
Nannini LJ, Poole P, Milan SJ, Holmes R, Normansell R. Combined corticosteroid and long-acting beta(2)-agonist in one inhaler versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;11:CD003794. | ||
Welsh EJ, Cates CJ, Poole P. Combination inhaled steroid and long-acting beta2-agonist versus tiotropium for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;5:CD007891. | ||
Lobo FS, Wagner S, Gross CR, Schommer JC. Addressing the issue of channeling bias in observational studies with propensity scores analysis. Res Social Adm Pharm. 2006;2(1):143–151. | ||
Petri H, Urquhart J. Channeling bias in the interpretation of drug effects. Stat Med. 1991;10(4):577–581. | ||
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention; 2014. [updated August 2014; cited February 13, 2015]. Available from: http://www.ginasthma.org/ | ||
Befekadu E, Onofrei C, Colice GL. Tiotropium in asthma: a systematic review. J Asthma Allergy. 2014;7:11–21. | ||
Kerstjens HA, Engel M, Dahl R, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med. 2012;367(13):1198–1207. | ||
Lee SW, Kim HJ, Yoo KH, et al. Long-acting anticholinergic agents in patients with uncontrolled asthma: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2014;18(12):1421–1430. | ||
Rashid Q, Klein R. Tiotropium in the treatment of patients with asthma. South Med J. 2014;107(5):330–337. | ||
Rodrigo GJ, Castro-Rodriguez JA. What is the role of tiotropium in asthma?: a systematic review with meta-analysis. Chest. 2015;147(2):388–396. | ||
Boehringer Ingelheim Pharmaceuticals. SPIRIVA Respimat Prescribing Information; 2014. [cited February 13, 2015]. Available from: http://www.boehringer-ingelheim.com/products/prescription_medicines/respiratory/asthma/spiriva/public/images/14-3946-Blatter-SPC-Spiriva-ERS.pdf | ||
Boehringer Ingelheim Pharmaceuticals. Boehringer Ingelheim Announces U.S. Filing Acceptance of New Drug Application for Spiriva® Respimat® (tiotropium bromide) Inhalation Spray for the Treatment of Asthma; 2014. [updated November 3, 2014; cited March 24, 2015]. Available from: http://us.boehringer-ingelheim.com/news_events/press_releases/press_release_archive/2014/11-03-14-boehringer-ingelheim-announces-us-filing-acceptance-new-drug-application-spiriva-respimat-tiotropium-bromide-inhalation-spray-treatment-asthma.html |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.