Back to Journals » International Journal of General Medicine » Volume 16
Comparative Clinical Implications of Calcified versus Non-Calcified Tissue Protrusion After Coronary Stent Implantation
Authors Wu X, Wu M, Huang H, Wang L, Liu Z, Cai J, Huang H
Received 19 October 2023
Accepted for publication 9 December 2023
Published 15 December 2023 Volume 2023:16 Pages 5935—5946
DOI https://doi.org/10.2147/IJGM.S445493
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Yuriy Sirenko
Xi Wu, Mingxing Wu, Haobo Huang, Lei Wang, Zhe Liu, Jie Cai, He Huang
Department of Cardiology, Xiangtan Central Hospital, Xiangtan, Hunan, 411100, People’s Republic of China
Correspondence: He Huang, Department of Cardiology, Xiangtan Central Hospital, Xiangtan, Hunan, 411100, People’s Republic of China, Email [email protected]
Purpose: The prognostic implications of calcified versus non-calcified tissue protrusions (TPs) following stent implantation remain undetermined. This study aimed to evaluate the differential clinical outcomes associated with calcified and non-calcified TP morphologies.
Patients and Methods: Employing intravascular ultrasound (IVUS), we identified calcified TPs as calcium fragment extrusions permeating the stent struts, while non-calcified TPs were characterized as plaque and/or thrombus extensions through the stent into the arterial lumen. The primary endpoint encompassed target lesion failure (TLF), comprising cardiac death, target vessel myocardial infarction, clinically driven target lesion revascularization (TLR), or stent thrombosis, assessed in patients with a follow-up period exceeding one year.
Results: Of 1033 patients subjected to pre- and post-intervention IVUS, 62 exhibited calcified TPs (6.0%), and 279 presented non-calcified TPs (27.0%), forming the basis of this analysis. Multivariable linear regression indicated calcified nodules as a significant predictor of calcified TP [Odds Ratio (OR) 2.47; 95% Confidence Interval (CI) 2.33 to 2.62; P < 0.001], with ST-segment elevation myocardial infarction emerging as an inverse correlate [OR 0.82; 95% CI 0.73 to 0.93; P = 0.004]. Two-year data revealed a higher incidence of TLF in patients with calcified TPs versus their non-calcified counterparts (11.3% vs 2.2%, P < 0.001), and a marked increase in clinically driven TLR (9.7% vs 1.4%, P < 0.001). Calcified TPs were independently correlated with increased TLF risk in the adjusted model [Hazard Ratio (HR) 2.47; 95% CI 1.17 to 5.16; P = 0.027].
Conclusion: After drug-eluting stent implantation, IVUS-identified calcified TPs correlate with adverse clinical outcomes compared to non-calcified TP formations.
Keywords: percutaneous coronary intervention, intravascular ultrasound, tissue protrusion, prognosis
Introduction
The introduction of drug-eluting stents (DES) represents a significant advancement in percutaneous coronary intervention (PCI) techniques for managing coronary artery disease. However, postoperative complications such as stent thrombosis and in-stent restenosis (ISR) continue to present substantial clinical challenges.1 A prevalent issue in post-PCI scenarios is tissue protrusion (TP), which involves the extrusion of coronary lesion constituents (plaque and/or thrombus) through the struts of the stent, detectable via intravascular ultrasound (IVUS).2–4 This condition is observed in 27–70% of patients treated with DES.2,5 Despite inconsistencies in earlier IVUS studies regarding the prognostic significance of TP, retrospective analyses have implicated TP in the increased occurrence of adverse coronary events, particularly early in-stent thrombosis.3,4,6 A notable association has been identified between refractory ISR and the presence of calcified tissue protrusions in patients.7–10 However, there remains a gap in the comprehensive assessment of the distinct clinical consequences of calcified versus non-calcified TPs, especially considering their prolonged clinical implications. Therefore, this study aims to thoroughly investigate the prevalence, predictive factors, and clinical outcomes associated with both calcified and non-calcified TPs, as identified through post-implantation IVUS analysis.
Materials and Methods
Study Design and PCI Protocol
This retrospective, single-center, observational study unfolded at Xiangtan Central Hospital spanning January 2015 to April 2020. Initial and subsequent post-PCI intravascular ultrasound (IVUS) assessments in all the patients were routinely conducted following the successful implementation of drug-eluting stents (DES) in primary PCI procedures. Exclusions encompassed: (1) without TPs, (2) chronic total occlusion lesions, (3) bifurcation lesions, (4) deployment of covered stents, (5) suboptimal IVUS image integrity, and (6) post-PCI clinical follow-ups shorter than one year. PCI methodologies, shaped by operator preference, adhered to prevailing standardized approaches. A minimum of 12 hours prior to PCI, patients were administered a dual antiplatelet primer-300 mg of aspirin, complemented by either 300 mg of clopidogrel or 180 mg of ticagrelor. Commencing with the PCI, intravenous heparin was initiated at 80 IU/kg, sustaining an activated clotting time between 250 and 300 seconds throughout the procedure. Post-PCI management mandated a daily dual antiplatelet regimen for at least 12 months (100 mg aspirin and either 75 mg clopidogrel or 180 mg ticagrelor). Conducted under the ethical tenets of the Declaration of Helsinki, the study secured institutional ethics committee endorsement. All participants provided written, informed consent for the PCI interventions. The study’s procedural sequence is delineated in Figure 1.
 |
Figure 1 Study flow. Abbreviations: IVUS, intravascular ultrasound; PCI, percutaneous coronary intervention; DES, drug-eluting stents; TP, tissue protrusion. |
Quantitative Coronary Angiographic Analysis
Quantitative coronary angiography of each lesion was facilitated through QAngio XA (Medis, Leiden, the Netherlands). Automated software delineated reference vessel diameter, minimum lumen diameter, percentage diameter stenosis, and lesion length.11 Calcification manifested as distinct radiopacities within vascular walls at stenotic sites. Coronary perfusion evaluations adhered to Thrombolysis In Myocardial Infarction (TIMI) benchmarks.12 Multivessel pathology was characterized by a visually confirmed >50% diameter stenosis in no less than two primary epicardial arteries.
IVUS Imaging and Analysis
Subsequent to the intracoronary introduction of 1–2mg nitroglycerin, IVUS assessments were conducted during pre- or post-DES deployment phases. Data capture utilized the readily accessible QIvus® system (Medis, Leiden, the Netherlands) alongside a 40-MHz IVUS array (OptiCrossTM, Boston Scientific, Marlborough, MA, USA). The IVUS catheter retraced from the stent’s distal to the target vessel’s proximal reference points, propelled at a consistent retraction speed of 0.5 mm/s. Dual cardiologist oversight, blinded to patients’ clinical characteristics, complied with standards stipulated by the American College of Cardiology’s consensus document on IVUS data handling.13
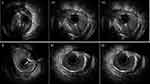
Sequential 1.0 mm intervals underwent quantitative IVUS scrutiny pre- and post-PCI, focusing on external elastic membrane (EEM), lumen, post-PCI stent areas, plaque plus media (EEM minus lumen), and plaque burden (ratio of plaque and media to EEM). Evaluations identified and analyzed the minimal luminal area (MLA) and minimal stent area (MSA) within each implicated lesion and reference segment. Reference segments, positioned 5 mm proximal and distal from each lesion or stent boundary (pre- or post-PCI) and preceding substantial (>1.5 mm diameter) side branches, underwent volumetric IVUS analysis using Simpson’s rule, yielding total and normalized volumes (expressed in mm3/mm).5 Plaque rupture presented as luminal-communicating intraplaque cavities capped by residual fibrous fragments.14 Attenuated plaque, identified by obscured deep arterial echos sans prominent calcification,14 contrasted with calcified TP, characterized by minute calcific extrusions permeating stent struts;9 Non-calcified TP involved non-calcified plaque or thrombus breaching stent confines (Figure 2). Assessments extended to TP dimensions and maximal TP expanses. Stent malapposition, indicated by observable blood speckles behind stent struts absent side branch overlay,3 and edge dissection, evidenced by disruption within or beyond the EEM,14 underwent diagnostic scrutiny. Consistency in TP diagnostic outcomes demonstrated high intra- and inter-observer agreement (κ = 0.93 and 0.90, respectively).
Clinical Follow-Up and Outcomes
Post-PCI, patients underwent a minimum one-year follow-up. The primary endpoint, target lesion failure (TLF), encompassed cardiac death, target vessel myocardial infarction, clinically driven target lesion revascularization (TLR), and stent thrombosis.15 Verification of clinical incidents entailed comprehensive electronic medical record scrutiny and/or telephonic correspondence.
Statistical Analysis
Statistical evaluations employed SPSS version 20.0 (IBM Corporation, Armonk, New York). Initial patient assessments focused on individual clinical presentations, with subsequent angiographic and procedural evaluations conducted at both patient and lesion dimensions, culminating in lesion-specific IVUS analysis. Data representation adopted mean±SD or median (interquartile range [IQR]) for continuous metrics, and frequency (%) delineation for categorical data. Normal distribution continuous variables underwent Student’s t-test analysis, with Fisher’s exact test applied to categorical counterparts. Non-normally distributed continuous variables warranted Mann–Whitney testing. Kaplan-Meier methodology charted clinical outcome survival rates, contrasting cases with and without IVUS-identified calcified TP, subject to Log rank testing. Multivariable linear regression assessed the interplay of clinical, angiographic, procedural, and IVUS factors in precipitating calcified TP. Concurrently, the Cox proportional hazards model interrogated the relationship of these variables with TLF. Lesion-centric investigations, acknowledging patient singularity across multiple lesions, necessitated a generalized estimating equation strategy. Statistical materiality was affirmed at a p-value threshold of <0.05 for all bidirectional tests.
Results
From January 2015 to April 2020, 1033 patients presented 1091 lesions, all undergoing IVUS-assisted PCI for de novo native coronary artery defects, with viable pre- and post-PCI IVUS imagery. Of these, 341 lesions from as many patients exhibited 374 TPs, establishing a TP incidence of 31.3% (341/1091) per lesion and 33.0% (341/1033) per patient. Single TPs manifested in 90.3% (308/341) of cases, while 9.7% (33/341) presented dual TPs, consistently of identical TP classification. Comparative analysis ensued between 73 lesions with calcified TPs from 62 patients and 301 lesions with non-calcified TPs from 279 patients.
Baseline Clinical Characteristics
Table 1 delineates baseline clinical differentials between patients exhibiting calcified versus non-calcified TP. Patients with calcified TP evidenced elevated chronic kidney disease prevalence (50 vs 39.4%, p<0.001) and stable ischemic heart conditions (56.5 vs 32.6%, p<0.001), contra a diminished frequency of ST-segment elevation myocardial infarction (STEMI) (3.2 vs 26.2%, p<0.001). Additionally, patients with calcified TP recorded a depressed estimated glomerular filtration rate (eGFR)(59.4±23.3 vs 76.3±25.7 mL/ min/1.73 m2, p<0.001).
 |
Table 1 Baseline Clinical Characteristics |
Angiographic and Procedural Findings
Table 2 reflects the angiographic and procedural discoveries. Calcified TP cases were correlated with heightened calcium presence(42.5 vs 22.6%, p<0.001), reduced thrombus incidence(13.4 vs 24.6%, p<0.001), and superior baseline TIMI flow (12.3 vs 20.6%, p=0.001).
 |
Table 2 Angiographic and Procedural Findings |
IVUS Findings
Table 3 indicates that of the 374 scrutinized pre-procedural IVUS lesions, those with calcified TP significantly harbored calcified nodules (CN) (79.5 vs 7.6%, p<0.001), and conversely, a lower frequency of plaque rupture and attenuated plaque (20.5 vs 36.2%, p<0.001; 13.7 vs 31.6%, p<0.001, respectively) relative to their non-calcified counterparts. Quantitative discernment disclosed a pronounced dense calcium volume in calcified TP lesions[12.3 (11.6–14.0) vs 7.6 (7.0–8.2), p<0.001]. Table 4 notes a higher prevalence of stent malapposition within calcified TP lesions (17.8 vs 10.3%, p= 0.002), accompanying suboptimal stent expansion and consequentially, diminished post-interventional in-stent MLA, MSA, and average luminal and stent areas, opposed to lesions devoid of calcified TP.
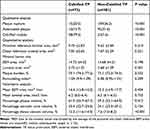 |
Table 3 Pre-Procedural Intravascular Ultrasound Findings |
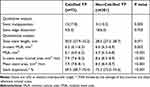 |
Table 4 Post-Procedural Intravascular Ultrasound Findings |
Predictors of Calcified TP
Utilizing a multivariable linear regression model (Table 5), calcified nodules emerged as positive predictors for calcified TP [Odds Ratio (OR) 2.47; 95% Confidence Interval (CI) 2.33 to 2.62; P <0.001], contrasted with ST-segment elevation myocardial infarction (STEMI) serving as a negative predictor (OR 0.82; 95% CI 0.73 to 0.93; P = 0.004).
 |
Table 5 Multivariate Predictors of Calcified Tissue Protrusion |
Clinical Outcomes
The median follow-up period spanned 2.0 years (interquartile range: 1.4–2.0). Table 6 encapsulates the post-implantation clinical outcomes. A cumulative TLF rate of 3.8% (13 events) materialized, predominantly propelled by clinically driven TLR (2.9%, 10 events). Both TLF and clinically driven TLR manifested at elevated rates in lesions featuring calcified TP versus those without (11.3 vs 2.2%, P <0.001; 9.7 vs 1.4%, P <0.001, respectively). Table 7 delineates a multivariate analysis pinpointing significant predictors of target lesion failure, highlighting the presence of calcified tissue protrusion [Hazard Ratio (HR) 2.47; 95% CI 1.17 to 5.16; P = 0.027] and extensive stent length [Hazard Ratio (HR) 2.43; 95% CI 1.63 to 3.63; P = 0.001]. Figure 3 depicts the Kaplan-Meier survival plots for TLF.
 |
Table 6 Kaplan–Meier Adverse Cardiac Event Rates |
 |
Table 7 Multivariate Predictors of Target Lesion Failure at Follow-Up |
 |
Figure 3 Kaplan–Meier cumulative incidence curves for target lesion failure. Abbreviations: HR, hazard ratio; CI, confidence interval; TP, tissue protrusion. |
Discussion
Key insights derived from the current investigation into TP lesions indicate: 1) a discrete prevalence of IVUS-identified calcified TP and non-calcified TP at 6.7% (73/1091) and 27.6% (301/1091) per lesion, respectively; 2) the role of calcified nodules as positive harbingers of calcified TP, opposed by STEMI as a deleterious factor; 3) a pronounced escalation in TLF and clinically driven TLR within the calcified TP cohort relative to its non-calcified counterparts; 4) a direct correlation linking calcified TP and elongated stent length with adverse TLF outcomes. This study is pioneering in its comparative evaluation of clinical repercussions following DES insertion between calcified and non-calcified TP scenarios.
Prevalence and Composition of TP
Intravascular imaging modalities such as IVUS or OCT frequently identify tissue protrusion subsequent to stent deployment. IVUS studies report TP incidence rates of 5–34.3%,4,16 while OCT assessments approximate a 90% occurrence post-stent implantation.17–19 In the present study, TP was detected in 31.3% overall lesions, which was the same as the previous studies. Defined as tissue prolapse between stent struts encroaching into the vascular lumen, the constitutive matter of tissue protrusion is predominantly thrombotic and plaque-derived.20 Hong et al21 demonstrated that intracoronary thrombi and necrotic plaque cores can breach stent struts, culminating in TP and the subsequent no-reflow phenomenon post-primary PCI. Coronary angioscopies have revealed a correlation between OCT-identified TP post-stent deployment and the presence of advanced yellow plaque thrombotic activity.22,23 Calcified nodules represent another prevalent plaque morphology within lesions accompanied by TPs. This study underscored a heightened incidence of calcified nodules within calcified TPs. Specifically, lesions featuring a calcified nodule, absent a calcified sheet, experienced protrusions of fragmented calcified particles through stent struts.9,24
Predictors of TP
TP’s emergence has been linked to various determinants including age, body mass index, statin usage, plaque rupture, intracoronary thrombus presence, elevated lipid content, thin-cap fibroatheroma, extensive plaque burden, positive vascular remodeling, substantial plaque volume, and extended stent implantation durations.2–4,25 This study identified calcified nodules as a conducive factor for calcified TP, while STEMI served as an inhibitory element. Given the higher incidence of angiographic intracoronary thrombi, augmented necrotic core volumes, plaque burdens, and thin-cap fibroatheromas detected via IVUS in STEMI patients compared to those with non-STEMI or stable angina,26,27 it is plausible that STEMI patients exhibit a higher frequency of non-calcified TPs. Histopathological examinations suggest that calcified nodules comprise nodular calcifications and fibrin deposits, with their formation linked to eruptive nodular calcifications originating from fragmented calcified plates, accompanied by surrounding fibrin and thrombi.28–31 This research noted a prevalent occurrence of CN within calcified TPs. Vascular trauma induced by elevated stent or post-dilation balloon pressures could precipitate coronary calcified plate fractures external to the stent, potentially triggering nodular calcification eruptions and subsequent calcified TP genesis. This investigation also highlighted CN’s predictive capacity for calcified TP. Despite CN’s established association with in-stent restenosis,8–10 its exact function within the calcified TP formation continuum remains elusive. The recurrent identification of calcified lesions within calcified TP sites, coupled with the routine presence of CN in such lesions, may elucidate the frequent detection of calcified TP in CN-associated calcified regions.
In our quantitative IVUS evaluations, parameters such as EEM area, luminal area, plaque burden, remodeling index at the MSA site, volumetric analysis, and reference luminal area showed no notable disparities between lesions with or without calcified TP, despite challenges in attaining adequate acute gains post-procedure in calcified lesions with calcified TP. Nonetheless, in-stent MLA, MSA, mean luminal and stent areas, along with stent expansion, were markedly reduced in calcified TP lesions compared to non-calcified counterparts. Additionally, stent malapposition prevalence escalated in calcified TP scenarios. Lesions characterized by CN pose a heightened risk for stent underexpansion and malapposition,32,33 likely attributable to stent deployment in highly calcified regions.
While prior IVUS research posits a contributory role for stent type and design in TP prediction,34 several studies contradict, citing negligible variations in TP rates across diverse stent types and designs.3,4,22,35 This study underscores that neither the metal composition nor the structural design of the stent is as critical as the inherent lesion morphology or the rigor of the implantation methodology.
Outcome of TP
The clinical implications of TP following PCI are contentious. Several studies have indicated a higher incidence of the no-reflow phenomenon during primary PCI in patients with TP, accompanied by elevated post-PCI CK-MB and troponin levels, relative to counterparts without TP.2–4 TP is also identified as a predisposing factor for subacute, early, and late stent thrombosis.6,16,36 Okuya et al37 posited that IVUS-identified TP could serve as a surrogate indicator for poorer clinical outcomes across acute, sub-acute, and late stages in STEMI patients. Conversely, prior IVUS and OCT investigations disclosed no significant correlation between TP and adverse clinical events.3,4,17,18,22,38
The present study revealed a pronounced escalation in TLF and clinically driven TLR within the calcified TP cohort relative to the non-calcified group. Corroborating earlier findings, CN is implicated in calcified TP post-DES insertion,8–10 consistent with our observations. Recent literature underscores the role of eccentric calcified protrusions with irregular contours, as verified through intracoronary imaging, in precipitating early in-stent restenosis following DES insertion.39,40 This intimates a potential link between immediate post-DES calcified TPs and deteriorated clinical prognoses. Additionally, it is documented that the majority of TPs, typically resolvable during follow-up, eventually facilitate a more expansive lumen post-PCI.5,17 The subsequent neointimal proliferation within 6–8 months post-DES insertion commonly leads to the disappearance of most TPs,17,24,41 potentially elucidating the fewer adverse outcomes in non-calcified TP scenarios. Moreover, TP-afflicted patients might necessitate intensified secondary preventive measures (eg, statins, β-blockers, and angiotensin-converting enzyme inhibitors) to optimize long-term prognoses.42 Consequently, comprehensive studies with larger cohorts are warranted to discern the precise relationship between calcified TP and early or late in-stent restenosis and thrombosis. Interventional cardiologists must remain cognizant of the potential emergence of calcified TPs following DES placement in lesions characterized by calcified nodules.
Limitations
The current study acknowledges several constraints. Firstly, its single-center, retrospective nature potentially introduces selection bias, as both participant inclusion and IVUS utilization depended on operator preference, possibly diminishing statistical vigor. Secondly, the limited lesion count precludes a precise determination of calcified TPs’ incidence, necessitating broader studies for verification. The study’s brief duration underscores the need to probe the nexus between these preliminary observations and protracted clinical manifestations through expansive sample analysis. Thirdly, the absence of direct one-to-one correspondence between IVUS observations and histological data is a notable shortfall. Fourthly, compared to OCT, IVUS’s lower resolution might contribute to an underestimation of TP, compounded by IVUS’s inability - paralleled by OCT43 - to distinctly characterize histological tissues. Lastly, the study’s cross-sectional design did not incorporate follow-up IVUS, limiting longitudinal insights.
Conclusions
This research indicates a relatively infrequent occurrence of IVUS-identified calcified TP post-DES procedure, particularly in calcified nodule-afflicted lesions. The presence of calcified TP discerned via IVUS correlates with deteriorated clinical prognoses.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The present research was carried out in accordance with the tenets mentioned in the Helsinki Declaration and was approved by the Ethical Board of Xiangtan Central Hospital (approval number: X20212081). Prior to the commencement of the research, our team obtained written informed consent from each patient.
Consent for Publication
Not applicable. No individual patient data will be reported.
Acknowledgment
We are grateful to Bo Chen for their secretarial assistance.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no grants from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no competing interests.
References
1. Piccolo R, Bonaa KH, Efthimiou O, et al. Drug-eluting or bare-metal stents for percutaneous coronary intervention: a systematic review and individual patient data meta-analysis of randomised clinical trials. Lancet. 2019;393(10190):2503–2510. doi:10.1016/s0140-6736(19)30474-x
2. Hong YJ, Jeong MH, Ahn Y, et al. Plaque prolapse after stent implantation in patients with acute myocardial infarction: an intravascular ultrasound analysis. JACC Cardiovascular Imaging. 2008;1(4):489–497. doi:10.1016/j.jcmg.2008.04.004
3. Hong YJ, Jeong MH, Choi YH, et al. Impact of tissue prolapse after stent implantation on short- and long-term clinical outcomes in patients with acute myocardial infarction: an intravascular ultrasound analysis. Int J Cardiol. 2013;166(3):646–651. doi:10.1016/j.ijcard.2011.11.092
4. Qiu F, Mintz GS, Witzenbichler B, et al. Prevalence and Clinical Impact of Tissue Protrusion After Stent Implantation: an ADAPT-DES Intravascular Ultrasound Substudy. JACC Cardiovascular Interventions. 2016;9(14):1499–1507. doi:10.1016/j.jcin.2016.05.043
5. Maehara A, Mintz GS, Lansky AJ, et al. Volumetric intravascular ultrasound analysis of Paclitaxel-eluting and bare metal stents in acute myocardial infarction: the harmonizing outcomes with revascularization and stents in acute myocardial infarction intravascular ultrasound substudy. Circulation. 2009;120(19):1875–1882. doi:10.1161/circulationaha.109.873893
6. Choi SY, Witzenbichler B, Maehara A, et al. Intravascular ultrasound findings of early stent thrombosis after primary percutaneous intervention in acute myocardial infarction: a Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) substudy. Circulation Cardiovascular Interventions. 2011;4(3):239–247. doi:10.1161/circinterventions.110.959791
7. Sugane H, Kataoka Y, Otsuka F, et al. Cardiac outcomes in patients with acute coronary syndrome attributable to calcified nodule. Atherosclerosis. 2021;318:70–75. doi:10.1016/j.atherosclerosis.2020.11.005
8. Nakamura N, Torii S, Tsuchiya H, et al. Formation of Calcified Nodule as a Cause of Early In-Stent Restenosis in Patients Undergoing Dialysis. J Am Heart Assoc. 2020;9(19):e016595. doi:10.1161/jaha.120.016595
9. Sato T, Matsumura M, Yamamoto K, et al. Impact of Eruptive vs Noneruptive Calcified Nodule Morphology on Acute and Long-Term Outcomes After Stenting. JACC Cardiovascular Interventions. 2023;16(9):1024–1035. doi:10.1016/j.jcin.2023.03.009
10. Moses JW, Usui E, Maehara A. Recognition of Recurrent Stent Failure Due to Calcified Nodule: between a Rock and a Hard Place. JACC Case Reports. 2020;2(12):1879–1881. doi:10.1016/j.jaccas.2020.09.004
11. Scanlon PJ, Faxon DP, Audet AM, et al. ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol. 1999;33(6):1756–1824. doi:10.1016/s0735-1097(99)00126-6
12. TIMI IIIb Investigators. Effects of tissue plasminogen activator and a comparison of early invasive and conservative strategies in unstable angina and non-Q-wave myocardial infarction. Results of the TIMI IIIB Trial. Thrombolysis in Myocardial Ischemia. Circulation. 1994;89(4):1545–1556. doi:10.1161/01.cir.89.4.1545
13. Mintz GS, Nissen SE, Anderson WD, et al. American College of Cardiology Clinical Expert Consensus Document on Standards for Acquisition, Measurement and Reporting of Intravascular Ultrasound Studies (IVUS). A report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2001;37(5):1478–1492. doi:10.1016/s0735-1097(01)01175-5
14. Kang SJ, Mintz GS, Witzenbichler B, et al. Effect of obesity on coronary atherosclerosis and outcomes of percutaneous coronary intervention: grayscale and virtual histology intravascular ultrasound substudy of assessment of dual antiplatelet therapy with drug-eluting stents. Circulation Cardiovascular Interventions. 2015;8(1):45.
15. Cutlip DE, Windecker S, Mehran R et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007;115(17):2344–2351. doi:10.1161/CIRCULATIONAHA.106.685313
16. Cheneau E, Leborgne L, Mintz GS, et al. Predictors of subacute stent thrombosis: results of a systematic intravascular ultrasound study. Circulation. 2003;108(1):43–47. doi:10.1161/01.Cir.0000078636.71728.40
17. Kawamori H, Shite J, Shinke T, et al. Natural consequence of post-intervention stent malapposition, thrombus, tissue prolapse, and dissection assessed by optical coherence tomography at mid-term follow-up. Eur Heart J Cardiovascular Imaging. 2013;14(9):865–875. doi:10.1093/ehjci/jes299
18. Sugiyama T, Kimura S, Akiyama D, et al. Quantitative assessment of tissue prolapse on optical coherence tomography and its relation to underlying plaque morphologies and clinical outcome in patients with elective stent implantation. Int J Cardiol. 2014;176(1):182–190. doi:10.1016/j.ijcard.2014.07.005
19. Sanuki Y, Sonoda S, Muraoka Y, et al. Contribution of Poststent Irregular Protrusion to Subsequent In-Stent Neoatherosclerosis after the Second-Generation Drug-Eluting Stent Implantation. Int Heart J. 2018;59(2):307–314. doi:10.1536/ihj.17-463
20. Kubo T, Tanaka A, Kitabata H, Ino Y, Tanimoto T, Akasaka T. Application of optical coherence tomography in percutaneous coronary intervention. Circulation J. 2012;76(9):2076–2083. doi:10.1253/circj.cj-12-0828
21. Hong YJ, Jeong MH, Choi YH, et al. Impact of plaque components on no-reflow phenomenon after stent deployment in patients with acute coronary syndrome: a virtual histology-intravascular ultrasound analysis. Eur Heart J. 2011;32(16):2059–2066. doi:10.1093/eurheartj/ehp034
22. Sakai S, Sato A, Hoshi T, Hiraya D, Watabe H, Ieda M. In Vivo Evaluation of Tissue Protrusion by Using Optical Coherence Tomography and Coronary Angioscopy Immediately After Stent Implantation. Circulation J. 2020;84(12):2235–2243. doi:10.1253/circj.CJ-20-0306
23. Miyoshi T, Kawakami H, Seike F, Oshita A, Matsuoka H. Relationship between yellow plaque grade and tissue protrusion after stent implantation: a coronary angioscopy study. J Cardiol. 2017;70(4):342–345. doi:10.1016/j.jjcc.2016.12.007
24. Otagaki M, Fujii K, Matsumura K, et al. The incidence, natural history, and predictive factors for tissue protrusion after drug-eluting stent implantation. Catheterization Cardiovascular Interventions. 2021;98(1):E62–e68. doi:10.1002/ccd.29551
25. Suzuki Y, Murata A, Murase S, Ochiumi Y, Ito T. Short- and long-term clinical impact of tissue protrusion after newer-generation drug-eluting stent implantation for acute coronary syndrome. Cardiovascular Intervention Therapeutics. 2019;34(2):155–163. doi:10.1007/s12928-018-0539-4
26. Dong L, Mintz GS, Witzenbichler B, et al. Comparison of plaque characteristics in narrowings with ST-elevation myocardial infarction (STEMI), non-STEMI/unstable angina pectoris and stable coronary artery disease (from the ADAPT-DES IVUS Substudy). Am J Cardiol. 2015;115(7):860–866. doi:10.1016/j.amjcard.2015.01.008
27. Soeda T, Uemura S, Park SJ, et al. Incidence and Clinical Significance of Poststent Optical Coherence Tomography Findings: one-Year Follow-Up Study From a Multicenter Registry. Circulation. 2015;132(11):1020–1029. doi:10.1161/circulationaha.114.014704
28. Hao H, Fujii K, Shibuya M, et al. Different findings in a calcified nodule between histology and intravascular imaging such as intravascular ultrasound, optical coherence tomography, and coronary angioscopy. JACC Cardiovascular Interventions. 2014;7(8):937–938. doi:10.1016/j.jcin.2013.12.212
29. Mori H, Finn AV, Atkinson JB, Lutter C, Narula J, Virmani R. Calcified Nodule: an Early and Late Cause of In-Stent Failure. JACC Cardiovascular Interventions. 2016;9(13):e125–6. doi:10.1016/j.jcin.2016.03.036
30. Sakakura K, Nakano M, Otsuka F, Ladich E, Kolodgie FD, Virmani R. Pathophysiology of atherosclerosis plaque progression. Heart Lung Circulation. 2013;22(6):399–411. doi:10.1016/j.hlc.2013.03.001
31. Otsuka F, Joner M, Prati F, Virmani R, Narula J. Clinical classification of plaque morphology in coronary disease. Nature Rev Cardiol. 2014;11(7):379–389. doi:10.1038/nrcardio.2014.62
32. Fujino A, Mintz GS, Matsumura M, et al. A new optical coherence tomography-based calcium scoring system to predict stent underexpansion. EuroIntervention. 2018;13(18):e2182–e2189. doi:10.4244/eij-d-17-00962
33. Lee SY, Mintz GS, Kim JS, Kim BK, Jang Y, Hong MK. Long-term Clinical Outcomes of Drug-Eluting Stent Malapposition. Korean Circulation J. 2020;50(10):880–889. doi:10.4070/kcj.2020.0198
34. Shen ZJ, Brugaletta S, Garcia-Garcia HM, et al. Comparison of plaque prolapse in consecutive patients treated with Xience V and Taxus Liberte stents. Int J Cardiovascular Imaging. 2012;28(1):23–31. doi:10.1007/s10554-010-9768-z
35. Wu XF, Guo CJ, Chi YP, et al. Attenuated plaque is associated with plaque prolapse accompanied by cardiac enzyme elevation after drug-eluting stent implantation. Coronary Artery Dis. 2014;25(1):4–9. doi:10.1097/mca.0000000000000053
36. Farb A, Burke AP, Kolodgie FD, Virmani R. Pathological mechanisms of fatal late coronary stent thrombosis in humans. Circulation. 2003;108(14):1701–1706. doi:10.1161/01.Cir.0000091115.05480.B0
37. Okuya Y, Saito Y, Sakai Y, Ishibashi I, Kobayashi Y. Impact of tissue protrusion after coronary stenting in patients with ST-segment elevation myocardial infarction. Int J Cardiovascular Imaging. 2019;35(3):401–407. doi:10.1007/s10554-018-1465-3
38. Jin QH, Chen YD, Jing J, et al. Incidence, predictors, and clinical impact of tissue prolapse after coronary intervention: an intravascular optical coherence tomography study. Cardiology. 2011;119(4):197–203. doi:10.1159/000331442
39. Kawai K, Akahori H, Imanaka T, et al. Coronary restenosis of in-stent protruding bump with rapid progression: optical frequency domain imaging and angioscopic observation. J Cardiology Cases. 2019;19(1):12–14. doi:10.1016/j.jccase.2018.08.010
40. Kato Y, Iwata A, Nakamura M, Miura SI, Saku K. In-Stent Restenosis due to Stent Recoil After Third-Generation Drug-Eluting Stent Implantation. J Clin Med Res. 2017;9(6):534–538. doi:10.14740/jocmr3024w
41. Kume T, Okura H, Miyamoto Y, et al. Natural history of stent edge dissection, tissue protrusion and incomplete stent apposition detectable only on optical coherence tomography after stent implantation – preliminary observation –. Circulation J. 2012;76(3):698–703. doi:10.1253/circj.cj-11-0845
42. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. doi:10.1093/eurheartj/ehx393
43. Lutter C, Mori H, Yahagi K, et al. Histopathological Differential Diagnosis of Optical Coherence Tomographic Image Interpretation After Stenting. JACC Cardiovascular Interventions. 2016;9(24):2511–2523. doi:10.1016/j.jcin.2016.09.016
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.