Back to Journals » Risk Management and Healthcare Policy » Volume 13
Community-Based Health Insurance Membership Dropout Rate and Associated Factors in Dera District, Northwest Ethiopia
Authors Ashagrie B, Biks GA , Belew AK
Received 19 August 2020
Accepted for publication 11 November 2020
Published 4 December 2020 Volume 2020:13 Pages 2835—2844
DOI https://doi.org/10.2147/RMHP.S277804
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Kent Rondeau
Birhanu Ashagrie,1 Gashaw Andargie Biks,1 Aysheshim Kassahun Belew2
1Department of Health System and Policy, Institute of Public Health, University of Gondar, Gondar, Ethiopia; 2Department of Human Nutrition, Institute of Public Health, University of Gondar, Gondar, Ethiopia
Correspondence: Aysheshim Kassahun Belew Email [email protected]
Background: Community-based health insurance is an emerging strategy for providing financial protection against health-related poverty. They have developed into alternative health financing mechanisms for out-of-pocket expenses in low- and middle-income countries. Hence, the aim of this study was to assess the drop-out rate of community-based health insurance membership and associated factors in Dera district, Northwest Ethiopia, 2020.
Methods: Through systematic random sampling techniques, a community-based cross-sectional study was conducted on 584 participants. A structured interviewer-based administered questionnaire was used for data collection. EpI data is used for data entry, while SPSS 20 version is used for analysis. P-value < 0.2 binary logistic regression was entered into multivariable logistic regression. Variables with a P-value of < 0.05 and a 95% confidence level were considered to be significantly associated with the outcome variable.
Results: The CBHI dropout rate in the district is calculated to be 37.3% (95% CI: 34, 41%) in the district. Length of enrollment, ≥ 4 years in the CBHI program (AOR=0.39, 95% CI: 0.26, 0.59), households visit the health facilities 4– 6 times a year (AOR=1.92, 95% CI: 1.10, 3.32), have no access to the hospital (AOR=1.68, 95% CI: 1.02, 2.77), knowledge of CBHI (AOR=1.93, 95% CI: 1.32, 2.82) and official position holder for decision-making in the households (AOR=2.07, 95% CI: 1.33, 3.23) were factors associated with CBHI dropout rate in the scheme.
Conclusion: This finding confirmed that the CBHI dropout rate in the district was high. Length of enrollment, health facility visit, hospital accessibility, knowledge of CBHI, and official position holders used for decision-making are significantly associated with the CBHI dropout rate. Therefore, emphasis should be given on improving members’ understanding of the CBHI package of benefits; increasing access to hospitals and empowering women will increase the utilization of CBHI. In addition, the quality of care for CBHI patients can be improved when they had access to health services.
Keywords: community-based health insurance, dropout rate, Dera district, Northwest, Ethiopia
Background
The governments in lower- and middle-income countries (LMICs) have an increased effort to achieve universal health coverage (UHC) and to improve healthcare access, use, and financial protection by reducing direct out-of-pocket payments (OOP) for health care.1,2 Many low- and middle-income countries cannot meet the necessary healthcare needs of their citizens. These countries face challenges in raising sufficient funds.3 Due to limited economic resources and weak government institutions,4 it is difficult to achieve healthcare financing.
Currently, global statistics show that the OOP of health care in low- and middle-income countries is very high. People in these countries are also affected by man-made and natural factors, which further increase medical expenses; this fact is true at the individual, family, and national levels.5,6 Because of these financially catastrophic problems, financing the healthcare system is a common agenda for all countries in the world.7 The report shows that the OOP health expenditure of high-income countries8 is 38.5%, and the OOP expenditure of Southeast Asian countries9 is 63% to 86%. Africa accounts for more than 40% of OOP.10 About 37% of the total healthcare expenditure in Ethiopia.11
Community-based health insurance (CBHI) is seen as a promising new tool for improving the health systems of people in low- and middle-income countries, especially in rural areas of sub-Saharan Africa (SSA).12 It improves cost recovery by reducing OOP healthcare spending.12–14 This event is a pledge agreement requiring the health insurer to cover health service costs for premium payments into a collective fund, a benefit designed, owned, controlled, and administered, which provides financial protection from the cost of seeking health care the prepayment of premiums and it is a not-for-profit.15,16
The World Health Organization’s (WHO) view on the CBHI program is that there is a fragile integration between public policy and organizational planning and action.13 Results indicate a high level of drop-out from the CBHI system, but it has not been analyzed in-depth, and this situation may be a sustainability problem of the CBHI scheme in many LMICs; this problem is also high in our country and region.17,18 Dropping out also hinders risk polling and resource mobilization for effective plan management, and creates long-term sustainability issues.14 The Asian report showed that about 80% of the enrolled members dropped out of their CBHI memberships.19 In Africa, the dropout rate increases from 6.8% to 83%.12,14,17,20 Moreover, between 7.8% and 36% of CBHI members were dropped from membership in Ethiopia.15,21
The lack of understanding of health insurance,21 experience with CBH scheme,21 knowledge of the CBHI scheme,21 accessibility of health facilities,12 health-needs and health demand,12 quality of care,12,17 household head and household characteristics,12 long waiting time,12,22 premium not affordable,22 the inconvenient model of premium payment,22 female household head,12 higher age of household head,12 low educational status of household,12 lower numbers of episodes in the last 3 months,12 fewer children or elderly in the household,12 stringent rules of some CBHI scheme,23 inadequate legal and policy frameworks to support CBHI,23 inappropriate benefit package23 were associated with CBHI dropout rate.
Ethiopia has approved and formulated the CBHI plan in 2010/2011,15 the benefit package of outpatient and inpatient services, laboratory, imaging services, the supply of drugs, and related services except for eyeglasses, dental implants, and dialysis with district fulfill the minimum standard of service in all government health facilities.24 However, a 2016 report by the Ethiopian Health Insurance Agency showed that only 30% of the communities had joined the CBHI program when the pilot was launched.25 A large number of health insurance plans cannot cover the entire population, and there are not enough good lessons from the experience of CBHI.14,26 Hence, this study assessed the dropout rate of community-based health insurance membership and associated factors in Dera district, Northwest Ethiopia, 2020.
Methods
Study Setting and Design
A qualitative community-based cross-sectional study was conducted in Dera from February 1 to March 30, 2020. The subjects of the survey were family members who had joined the CBHI program since 2018. The Dera district is 610 km from Addis Ababa, the capital of Ethiopia, 42 km from Bahir Dar, and 80 km from Debre Tabor. According to the region’s 2019 annual report, the region has a total population of 303,571, of which men and women are 136,464 and 167,107, respectively. Amongst 70,598 households, the expected number of households participating in CBHI is 27,470 (39%). Currently, the area has 32 administrative Kebeles, 11 health centers, and 36 health posts.
Study and Source Population
All CBHI members who have enrolled in the Dera District and received CBHI program services since 2018 are the source population of this study.
Sample Size and Sampling Procedure
Sample estimation was calculated using the single population proportion formula by applying the following assumption: the previous dropout rate of CBHI was 36%27 in Northwest Ethiopia with a marginal error of 5%, 95% level of confidence, and a design effect of 1.5. Finally, a sample size of 584 was obtained by considering a 10% non-response rate. A multistage sampling technique followed by a systematic random sampling technique was employed to select the study participants. Seven Kebeles were selected by lottery methods, and then the sample size was allocated to each Kebeles by using a proportionate allocation from the total sample size.
Data Collection Tools and Techniques
A structured pretested questionnaire was used prepared by reviewing different pieces of literature.21,27–30 Data were collected through face-to-face interviews. The questionnaire was initially prepared in English, and it was translated into Amharic and then translated back to English to check for any inconsistencies or distortions in the meaning of words and concepts through language experts. Seven BSc health workers and two supervisors have taken part in data collection and supervision, respectively. A pretest was done before 2 weeks of the actual data collection among 30 samples, from the total sample size out of the study area on simplicity, understandability, completeness, consistency, and coherence, and necessary correction like changing some terms with locally used words was taken after the pretest was done. Two days of training were provided for data collectors and supervisors on how to approach, extract information, and understand the questionnaire and the fieldwork. Supervisors and principal investigators conduct close supervision once a day to check the integrity of the data. Daily feedback is also provided to the data collector.
Variable Measurements
Knowledge of CBHI was assessed by seven yes/no questions. The Yes response of the respondents was the correct response labeled as 1 and No was the wrong response labeled as 0. After summarizing, the result score of 50% or higher is regarded as good knowledge, and the result below 50% is regarded as poor knowledge of the CBHI program.27 The wealth index was computed by using a principal component analysis (PCA) and by considering household assets. The classification range of these assets is 0–1. After classification, variables are input into PCA to generate factors, and then variables with commonality values greater than 0.5 are used to create factor scores. Finally, divide the summary value of factor scores into five quintiles.27
Data Processing and Analysis
All returned questionnaire was checked for completeness and consistency of responses. The collected data were cleaned, coded, and entered EPI-data and it was exported to SPSS version 20 for analysis. Data were cleaned and analyzed using SPSS version 20. The dropout rates of the CBHI indicator are dichotomous variables, which were classified as 0 and 1, which do not meet the criteria and meeting the criteria, respectively. Descriptive statistics such as mean, median, frequency, and a number of variables were summarized by using frequency, tables, graphs, and texts. Carry out variable relationship diagnosis, such as goodness of fit test by Hosmer and Lemeshow test, multicollinearity, and sample adequacy test. The variables with p-value ≤0.2 in the Bivariate analysis were fitted to a multivariate logistic regression model to identify their association with the outcome variable. It is reported that a variable with a 95% CI of P<0.05 can be used as a predictor of the CBHI dropout rate.
Ethical Consideration and Consent Statement
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance and permission were obtained from the Ethical Review Board of the institute of public health, College of Medicine and Health Sciences, University of Gondar (IRB) with ethical clearance letter Ref No/IPH/837/06/2020, and permission was secured from Dera district administration. Then, written informed consent was obtained from each head of the households before the interview, and the University of Gondar approved this. We asked for informed consent from the head of the household because the head of the households can decide any household-related issues including health demand and related costs like a renewal of CBHI membership. Confidentiality issues were insured by using codes to analyze the data. Respondents were briefly informed about the study and asked for their willingness to participate in the study. They had given the right to put an end to the question or segment of questions or refuse to participate at all.
Results
Socio-Demographic and Socio-Economic Status of the Respondents
A total of 584 participants participated in a response rate of 100%. The mean age of the respondents was 42 years old, SD ± 12. Nearly all household respondents, 547 (93.7%) were males and 536 (91.8%) of the respondents were married. Almost half, 291 (49.8%) of participants were unable to read and write. Most, 476 (81.5%) of the participants were rural by residence. Less than half, 275 (47.1) of the respondents were in the age range of 20–24 years old. Nearly all, 565 (96.7%) and 536 (91.8%) were Orthodox and married by religious and marital status, respectively. More than three-fourth, 500 (85.6%), of the study participants were farmers. More than 334 (57.2%) of the participants had less than five household family size. One quarter, 116 (19.9%) of the households were grouped in the poorest wealth status (Table 1).
 |
Table 1 Socio-Economic and Demographic Characteristics of Respondents for CBHI Dropout Rate and Associated Factors at Dera District Northwest Ethiopia, 2020 |
Experience and Expectations of CBHI Members
More than half, 321 (55%), of respondents were enrolled in CBHI program for 1–3 years. Only 86 (14.7%) of participants were participating in CBHI related meetings and training. More than half 345 (59.1%) of participants were visiting healthcare facilities one to three times per year. Nearly all, 575 (98.5%) respondents have got and accessed health care from the nearby health centers. Only one-third of 214 (36.6%) participants were accessible to hospital services. Three-fourth, 456 (78.1%), of the respondents were not agreed on the covenant waiting to time in the health facilities. Only 326 (55.8%) of the CBHI members did not trust the contract agreement signed with the health facilities (Table 2).
 |
Table 2 Experience and Expectation with CBHI for Dropout Rate and Associated Factors at Dera District Northwest Ethiopia 2020 |
Health Status and Health Care Seeking Behavior
Three-fourth of 439 (75.2%) participants were not having sick under-five children for the last 4 weeks and a half, 320 (54.8%), were not having sick adults the last 3 months in their households. Over one-third (40.9%) of the respondents were had poor knowledge about CBHI services. About its own self-rated health, 245 (42%) and 220 (37.7%) were perceived medium and good health self-rated, respectively. Three-fourth of 466 (79.8%) have participated in any solidarity group. Only, 209 (35.8%) of the participants were had ever participated in the local informal credit association. Two-thirds, 379 (64.9%), of household power are holding by the joint of both husband and wife (Table 3).
 |
Table 3 Health Status, Health Care Seeking Behavior, Participation in Informal Networking and Social Support Group for CBHI Dropout Rate Dera District Northwest Ethiopia 2020 |
CBHI Dropout Rate
The CBHI dropout rate in the district is calculated to be 37.3% (95% CI: 34, 41%). In most cases, the dropout rate is due to lack of funds (80, 36.7%) or lack of trust in the CBHI program (79, 36.2%), as shown in (Figure 1).
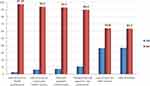 |
Figure 1 Reasons for CBHI dropout rate and associated factors at Dera district Northwest Ethiopia 2020. |
Factors Associated with CBHI Dropout Rate
For age, household size, length of enrollment in the CBHI scheme, number of health facility visits per year, hospital accessibility, knowledge of CBHI, self-rated health status, number of sick adults in the household in the last 3 months, participation in any solidarity group, and the decision-making status in the household, the binary logistic regressions yielded a p-value below 0.2. After adjusting the multivariable logistic regression model, only length of enrollment in the CBHI scheme, number of health facility visits per year, hospital accessibility, knowledge of CBHI, and the decision-making status in the household remained significant to the outcome variable.
The dropout rate among individuals that had participated in the CBHI scheme for more than 4 years was 61% lower than that among those enrolled for 1−3 years (AOR: 0.39, 95% CI: 0.26, 0.59). The odds of dropout rate among households that utilized health facilities 4−6 times a year were 1.92 times greater compared to those that required 1−3 visits (AOR: 1.92, 95% CI= 1.10, 3.32). In addition, the analysis showed that people without hospital access were 1.68 times more likely to give up the CBHI program than those with hospital access (AOR: 1.68, 95% CI: 1.02, 2.77). Correspondingly, individuals who had poor knowledge about CBHI were 1.93 times more likely to abandon their CBHI scheme than those who had no information about the program (AOR: 1.93, 95% CI= 1.32, 2.82). Finally, households in which the husband was a decision-maker were 2.07 times more likely to abandon their CBHI scheme than those where decisions were made by the wife (AOR: 2.07, 95% CI= 1.33, 3.23), as shown in Table 4.
 |
Table 4 Bi-Variable and Multivariable Logistic Regression Analysis for CBHI Dropout Rate and Associated Factors at Dera District Northwest Ethiopia 2020 |
Discussion
The aim of the current study was to identify the reasons behind CBHI dropout rate in the district. Analyses revealed that 37.3% of the community-based health insurance members have abandoned the program, which is in line with the percentages reported for Ghana (34.8%)14 and Ethiopian (36%).27 However, much higher dropout rates were reported in India (45.7−80%),32 Burkina Faso (45.7%),12 Senegal (58−83%),17 and Kenya (59.8%),2 possibly due to the differences in study setting, design, and the socio-demographic characteristics of study participants. The authors of the aforementioned studies recommended reducing the knowledge gap in the community via information dissemination on the CBHI benefit package, which should be a responsibility of health professionals as well as government officials. Still, it is worth noting that lower dropout rates were reported for Nigeria (31.7%),2,19 and Ethiopia 18%21 possibly due to better financial position of the participants in these studies, which would allow them to cover the annual premium payment for membership renewal.2 In addition, lack of trust in the CBHI scheme and low expectations of utility gain and risk minimization through CBHI as the main reasons for dropout from the program.27
In this study, the time of enrollment is related to the dropout rate of the CBHI program. Specifically, compared with 1–3 years of membership, ≥4 years of enrollment is associated with a 61% drop in the dropout rate. This result is supported by the studies done in India,32 and Ethiopia,26,33 where CBHI enrolls with longer length of enrollment were more satisfied and kept their membership than those with shorter length of enrollment and households that were members of an existing CBHI scheme already were more willing to keep into the scheme.34 Long-term members of CBHI can increase awareness and knowledge of the importance of the CBHI program and help reduce the CBHI dropout rate. In addition, when family members stay in the plan for a long time, they may also consider the money they have deposited for a long time.32
Participants who have poor knowledge of CBHI are 1.93 times more likely to withdraw from the CBHI program than participants who know about CBHI. Reports from Tanzania3 and Ethiopia21 support this finding. A possible explanation may be a lack of knowledge and understanding of the risk-sharing principles of the CBHI program, which may increase the dropout rate. Having good knowledge and information on the role of the CBHI program will help CBHI enrollment, and it decreases the dropout rate.3 Sufficient information on the benefits of the CBHI program may contribute to building members’ trust in CBHI system management, and it promotes the retention of members in the program.3
Inaccessibility of the hospital is also an important factor for the dropout rate of the CBHI program. Those who had no access to the hospital were 1.68 times more likely to drop out of their CBHI schemes than those who had access to hospitals. This finding is similar to the study done in Ethiopia.35 The possible reason might be as the distance of hospitals from home increases, it may confront people with additional transportation and other health-related costs like bedroom and food. Then, their interest in the dropout from the program increases.35 The finding in this study is contrary to other studies done in Burkina Faso and Ethiopia. The possible reason might be those CBHI members living far from the health facility may face higher non-medical costs like the cost of transportation, food, bed, and other opportunity costs when seeking health care besides the medical cost.12
The number of official position holders used for decision-making in male-headed households is 2.07 times higher than that of female-headed households. This result is comparable to the results of similar studies conducted in Asian countries,9 Ghana,20 and Ethiopia.9,21,27,36 This may be due to the fact that women have a higher risk tendency than men and are responsible for family health. Women are the largest users of health care, and they may have a special recognition of the CBHI program. Women as caregivers for children and other patients in the family, coupled with their vulnerability and physiologic makeup, may have a more positive attitude toward CBHI decision-making than their male counterparts.20
The frequency of health facility visits has a positive association with CBHI of the dropout rate. Those individuals who had visited health facilities 4–6 times a year were 1.92 times more likely to drop out of their CBHI scheme than those who had visited health facilities 1–3 times per year. The explanation might be as the frequency of health faculty visit increase client’s confrontation to a health professional, and other supporting staff increase, and then their satisfaction may exhaust, and then their trust by a health professional and contracted health facility also decrease, and they may drop from CBHI scheme. However, this finding is different from the Bangladesh study,18 and the possible explanation may be that the client frequently visits the health facilities will be increased medical and non-medical costs, as a result, the likely hood of renewal also increased to reduce the cost.6 Quality of healthcare service in the health facilities might be better in Bangladesh.
Limitation
This research is of great significance. First, it covers a small number of schemes, a single area study, and the sample size is small. Second, the limitation is that for the cross-sectional and non-experimental study design; it is difficult to attribute causality.
Conclusions
The report shows that the CBHI dropout rate in the area is high. Length of enrollment, health facility visit, hospital accessibility, knowledge of CBHI, and official position holders used for decision-making are significantly associated with the CBHI dropout rate. Therefore, we should focus on improving members’ understanding of the CBHI package of benefits; increasing access to hospitals and empowering women will increase the utilization of CBHI. In addition, the quality of medical care for CBHI patients is improved when accessing medical care.
Abbreviations
AOR, adjusted odds ratio; CBHI, community-based health insurance; CI, confidence interval; COR, crude odd ratio; LMICs, lower- and middle-income countries; OOP, out-of-pocket payment; PCA, principal component analysis; SPSS, Statistical Package for Social Sciences; SSA, sub-Saharan Africa; UHC, universal health coverage; WHO, World Health Organization.
Data Sharing Statement
Data will be available upon request from the corresponding authors.
Consent for Publication
Not applicable.
Acknowledgments
The authors would like to thank the data collectors and all respondents for their willingness to participate in this study. We also thanked all District health office staff, ARHB and other individuals for their contributions to this research and the material and ultimate support provided by the University of Gondar.
Author Contributions
All authors made a substantial contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There was no fund for this study.
Disclosure
The authors report no conflicts of interest for this work.
References
1. Alebachew A, Hatt L, Kukla M. Monitoring and evaluating progress towards universal health coverage in Ethiopia. PLoS Med. 2014;11(9):e1001696. doi:10.1371/journal.pmed.1001696
2. Ertekin E, Navarrete Moreno C. Micro Insurance Academy: Improving Health Insurance Coverage in India. World Bank; 2017.
3. Macha J, Kuwawenaruwa A, Makawia S, Mtei G, Borghi J. Determinants of community health fund membership in Tanzania: a mixed methods analysis. BMC Health Serv Res. 2014;14(1):538. doi:10.1186/s12913-014-0538-9
4. Fadlallah R, El-Jardali F, Hemadi N, et al. Barriers and facilitators to implementation, uptake and sustainability of community-based health insurance schemes in low-and middle-income countries: a systematic review. Int J Equity Health. 2018;17(1):13. doi:10.1186/s12939-018-0721-4
5. Mekonen AM, Gebregziabher MG, Teferra AS. The effect of community based health insurance on catastrophic health expenditure in Northeast Ethiopia: A cross sectional study. PLoS One. 2018;13(10):e0205972. doi:10.1371/journal.pone.0205972
6. Iqbal M, Chowdhury AH, Mahmood SS, Mia MN, Hanifi S, Bhuiya A. Socioeconomic and programmatic determinants of renewal of membership in a voluntary micro health insurance scheme: evidence from Chakaria, Bangladesh. Glob Health Action. 2017;10(1):1287398.
7. Ali EE. Health care financing in Ethiopia: implications on access to essential medicines. Value Health Regional Issues. 2014;4:37–40. doi:10.1016/j.vhri.2014.06.005
8. Fenny AP, Kusi A, Arhinful DK, Asante FA. Factors contributing to low uptake and renewal of health insurance: a qualitative study in Ghana. Global Health Research Policy. 2016;1(1):18. doi:10.1186/s41256-016-0018-3
9. Dror DM, Hossain SS, Majumdar A, Koehlmoos TLP, John D, Panda PK. What factors affect voluntary uptake of community-based health insurance schemes in low-and middle-income countries? A systematic review and meta-analysis. PLoS One. 2016;11(8):e0160479.
10. Word Health Organization. Regional Office for Africa. State of health financing in the African region. 2013.
11. Minyihun A, Gebregziabher MG, Gelaw YA. Willingness to pay for community-based health insurance and associated factors among rural households of Bugna District, Northeast Ethiopia. BMC Res Notes. 2019;12(1):55. doi:10.1186/s13104-019-4091-9
12. Dong H, De Allegri M, Gnawali D, Souares A, Sauerborn R. Drop-out analysis of community-based health insurance membership at Nouna, Burkina Faso. Health Policy. 2009;92(2–3):174–179. doi:10.1016/j.healthpol.2009.03.013
13. Ajemunigbohun SS, Aduloju SK, Sogunro AB, Azeez FT. Demand for health insurance among individual households in Lagos State, Nigeria: effects of socio-demographic variables. Paradigms. 2017;11(2):236–242.
14. Atinga RA, Abiiro GA, Kuganab‐Lem RB. Factors influencing the decision to drop out of health insurance enrolment among urban slum dwellers in Ghana. Tropical Medicine International Health. 2015;20(3):312–321. doi:10.1111/tmi.12433
15. Workneh SG, Biks GA, Woreta SA. Community-based health insurance and communities’ scheme requirement compliance in Thehuldere district, northeast Ethiopia: cross-sectional community-based study. ClinicoEconomics Outcomes Research. 2017;9:353. doi:10.2147/CEOR.S136508
16. Mladovsky P, Ndiayeii P. Solidarity in community-based health insurance in Senegal: rhetoric or reality. African Health Monitor. 2015;20:20–26.
17. Mladovsky P. Why do people drop out of community-based health insurance? Findings from an exploratory household survey in Senegal. Soc Sci Med. 2014;107:78–88. doi:10.1016/j.socscimed.2014.02.008
18. Khan JA, Ahmed S. Impact of educational intervention on willingness-to-pay for health insurance: a study of informal sector workers in urban Bangladesh. Health Econ Rev. 2013;3(1):12. doi:10.1186/2191-1991-3-12
19. Panda PP, Chakraborty AA, Raza WW, Bedi ASA. Renewing membership in three community-based health insurance schemes in rural India. ISS Working Paper Series/General Series. 2015;608(608):1–28.
20. Boateng D, Awunyor-Vitor D. Health insurance in Ghana: evaluation of policy holders’ perceptions and factors influencing policy renewal in the Volta region. Int J Equity Health. 2013;12(1):50. doi:10.1186/1475-9276-12-50
21. Mebratie AD, Sparrow R, Yilma Z, Alemu G, Bedi AS. Dropping out of Ethiopia’s community-based health insurance scheme. Health Policy Plan. 2015;30(10):1296–1306. doi:10.1093/heapol/czu142
22. Mukangendo M, Nzayirambaho M, Hitimana R, Yamuragiye A. Factors contributing to low adherence to community-based health insurance in rural Nyanza district, Southern Rwanda. J Environ Public Health. 2018;2018.
23. Dror DM, Hossain SS, Majumdar A, Pérez Koehlmoos TL, John D, Panda PK. What factors affect voluntary uptake of community-based health insurance schemes in low-and middle-income countries? A systematic review and meta-analysis. PLoS One. 2016;11(8):e0160479. doi:10.1371/journal.pone.0160479
24. Ethopian Health Insurance Agency. Evaluation of community‐based health insurance pilot schemes in Ethiopia: Final Report. Addis Ababa: EHIA; 2015.
25. Bradley EH, Byam P, Alpern R, et al. A systems approach to improving rural care in Ethiopia. PLoS One. 2012;7(4):e35042. doi:10.1371/journal.pone.0035042
26. Kebede KM, Geberetsadik SM. Household satisfaction with community-based health insurance scheme and associated factors in piloted Sheko district; Southwest Ethiopia. PLoS One. 2019;14(5):e0216411. doi:10.1371/journal.pone.0216411
27. Asmamaw, A. (2018). CBHI in Ethiopia: Enrollment, Membership renewal and Effect on health care utilization. Seoul: Seoul National University; 2018.
28. Bodhisane S, Pongpanich S. The impact of National Health Insurance upon accessibility of health services and financial protection from catastrophic health expenditure: a case study of Savannakhet province, the Lao People’s Democratic Republic. Health Research Policy Systems. 2019;17(1):99. doi:10.1186/s12961-019-0493-3
29. Bodhisane S, Pongpanich S. Factors affecting the willingness to join community‐based health insurance (CBHI) scheme: A case study survey from Savannakhet Province, Lao PDR. Int J Health Plann Manage. 2018.
30. Mirach TH, Demissie GD, Biks GA. Determinants of community-based health insurance implementation in west Gojjam zone, Northwest Ethiopia: a community based cross sectional study design. BMC Health Serv Res. 2019;19(1):544. doi:10.1186/s12913-019-4363-z
31. Tadesse G, Atnafu DD, Ketemaw A, et al. Determinants of enrollment decision in the community based health insurance, North West Ethiopia: A case control study.
32. Panda P, Chakraborty A, Raza W, Bedi AS. Renewing membership in three community-based health insurance schemes in rural India. Health Policy Plan. 2016;31(10):1433–1444. doi:10.1093/heapol/czw090
33. Nageso D, Tefera K, Gutema K. Enrollment in community based health insurance program and the associated factors among households in Boricha district, Sidama Zone, Southern Ethiopia; a cross-sectional study. Plos one. 2020;15(6):e0234028.
34. Adebayo EF, Uthman OA, Wiysonge CS, Stern EA, Lamont KT, Ataguba JE. A systematic review of factors that affect uptake of community-based health insurance in low-income and middle-income countries. BMC Health Serv Res. 2015;15(1):543. doi:10.1186/s12913-015-1179-3
35. Mebratie AD, Sparrow R, Yilma Z, Alemu G, Bedi AS. Enrollment in Ethiopia’s community-based health insurance scheme. World Dev. 2015;74:58–76. doi:10.1016/j.worlddev.2015.04.011
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
