Back to Journals » Clinical Ophthalmology » Volume 17
Combined MIGS: Comparing Additive Effects of Phacoemulsification, Endocyclophotocoagulation, and Kahook Dual Blade
Authors Oberfeld B , Golsoorat Pahlaviani F, Hall N, Falah-Trzcinski H, Trzcinski J, Chang T , Solá-Del Valle D
Received 5 March 2023
Accepted for publication 24 May 2023
Published 8 June 2023 Volume 2023:17 Pages 1647—1659
DOI https://doi.org/10.2147/OPTH.S410471
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Blake Oberfeld,1,2 Fatemeh Golsoorat Pahlaviani,1 Nathan Hall,1 Henisk Falah-Trzcinski,1 Jonathan Trzcinski,1 Ta Chang,3 David Solá-Del Valle1
1Glaucoma Service, Massachusetts Eye and Ear Infirmary and Harvard Medical School, Boston, MA, USA; 2Department of Ophthalmology, University of Florida, Gainesville, FL, USA; 3Department of Ophthalmology, Bascom Palmer Eye Institute, Miami, FL, USA
Correspondence: David Solá-Del Valle, Glaucoma Service, Massachusetts Eye and Ear Infirmary and Harvard Medical, 243 Charles St, Boston, MA, 02114, USA, Tel +1 617-573-3670, Fax +1 617-573-3707, Email [email protected]
Purpose: Combining two or more MIGS (cMIGS) promises to be more efficacious than single MIGS (sMIGS). This study compared the efficacy of PEcK, which combines Phacoemulsification (Phaco), Endocyclophotocoagulation (ECP), and Kahook dual blade (KDB), relative to both of its constituent sMIGS, Phaco/ECP (Endo Optiks, NJ) and Phaco/KDB (New World Medical, CA) for the first time.
Patients and methods: Data was collected retrospectively from 1833 visits of 271 patients who underwent PEcK, Phaco/ECP, or Phaco/KDB from 2016– 2021 at Massachusetts Eye and Ear. Primary outcomes included Generalized Estimating Equations (GEE) of intraocular pressure (IOP) and medication burden, as well as survival models.
Results: Mean preoperative IOP was 17.6 ± 5.0 (SD) mmHg on 3.0 ± 1.4 medications in the PEcK group (n = 128), 17.9 ± 5.1 mmHg on 2.2 ± 1.5 medications in the Phaco/ECP group (n = 78), and 16.1 ± 4.3 mmHg on 0.4 ± 1.0 medications in the Phaco/KDB group (n = 65). For more than 36 months, all procedures resulted in significant patterns of IOP and medication reduction (all p < 0.001), before and after statistical adjustment. The reduction pattern in IOP was significantly different when comparing all groups over time and favored PEcK (p = 0.04), but the reduction pattern in medications was not significantly different (p = 0.11). Procedures did not differ in procedural time (p = 0.18) or in survival to maintain ≥ 20% IOP reduction (p = 0.43) without additional medication or procedure. There was a trend toward significant difference in maintaining IOP ≤ goal IOP that favored PEcK over Phaco/ECP after adjustment (p = 0.09).
Conclusion: PEcK may confer greater IOP reduction without added procedural time compared to Phaco/ECP and Phaco/KDB in predominantly mild or moderate glaucoma. Further research on cMIGS may benefit from adopting this comparative analysis to constituent MIGS.
Keywords: microinvasive glaucoma surgery, cMIGS, generalized estimating equations, GEE, comparative effectiveness, combined efficacy, glaucoma
Précis
In this retrospective study of 271 patients with 1833 clinical visits, we suggest that combined Phacoemulsification, Endocyclophotocoagulation, and Kahook dual blade (PEcK) may confer greater IOP reduction than its constituent MIGS without additional procedural time.
Plain Language Summary
For the first time, in patients undergoing cataract removal, we compared a combination glaucoma surgery to both of its individual procedures, which aim to lower eye pressure by decreasing fluid production (cyclophotocoagulation) or increasing fluid drainage (Kahook Dual Blade) in the front of the eye. We report that the combination of both glaucoma surgeries and cataract removal may lead to greater reduction of eye pressure without added surgical time and without sacrificing safety.
Introduction
With many different mechanisms of action among microinvasive glaucoma surgery (MIGS), there is a growing interest in establishing whether combining multiple MIGS (cMIGS) leads to an additive or synergistic effect.1 Although a number of case reports, retrospective studies, and systematic reviews have reported on cMIGS, none has directly compared the combination procedure to all of its constituent MIGS. Despite this, understanding the relative efficacy of cMIGS to their constituent MIGS is fundamental to clinical decision making and to establishing the benefit of combination. This study focuses on the hypothesis that PEcK, a specific cMIGS that combines Phacoemulsification (Phaco), Endocyclophotocoagulation (ECP; Endo Optiks, NJ, USA), and Kahook dual blade (KDB; New World Medical, CA, USA), yields greater IOP reduction, medication reduction, and survival than its constituent MIGS, while maintaining procedural time and safety.2
As one component of PEcK, ECP is used to ablate ciliary processes and decrease aqueous humor production. Although complications including intraocular pressure spikes, postoperative inflammation, and lens dislocation remain concerns, the procedure has an excellent safety profile in mild and moderate glaucoma.3–5 In the literature, at 12 months postoperatively from Phaco/ECP, mean intraocular pressure (IOP) is reduced by 2.7 to 11.5 mmHg in retrospective studies.6
Phacoemulsification is also frequently combined with ab-interno trabecular excision using the Kahook Dual Blade. Relying on retrospective studies and case series, the efficacy of Phaco/KDB has been reported with 12-month IOP reductions between 1.9 to 11.7 mmHg.7–16
Furthermore, PEcK has only been reported in two studies and one systematic review to the best of our knowledge.1,2,17 Izquierdo et al performed a prospective, unblinded study of 49 eyes with mild-to-advanced primary open-angle glaucoma on ≥2 medications, which were randomized to either PEcK or Phaco/ECP. At 12 months postoperatively, mean IOP was reduced by 5.52 mmHg in the PEcK group, resulting in a 32.5% reduction compared to 20.3% after Phaco/ECP (p = 0.031).17 Our group has also reported on PEcK (n = 53) in a retrospective study of predominantly mild or moderate glaucoma compared to another cMIGS procedure combining iStent insertion, Cataract extraction, and ECP (ICE). The study found a 12-month mean IOP reduction of 5.1 ± 4.4 mmHg on 1.6 ± 1.5 fewer medications, reporting a signal of potentially greater mean IOP reduction following PEcK compared to ICE (p = 0.08).
This study reports on the efficacy of PEcK for more than 36 months and establishes the relative efficacy to all of its constituent single MIGS (sMIGS), both Phaco/ECP and Phaco/KDB, for the first time of any cMIGS.
Methods
Overview
The study protocol and waiver of consent for retrospective chart review was approved by the Massachusetts General Brigham Institutional Review Board (IRB Number 2019P002735). All research adhered to the Declaration of Helsinki and the Health Insurance Portability and Accountability Act, as well as standards of reporting.
Population
Subjects were queried from all surgical records at Massachusetts Eye and Ear performed by any fellowship-trained glaucoma surgeon between January 2016 to July 2021 and were included if the operative report confirmed having undergone PEcK, Phaco/ECP, or Phaco/KDB. Patients were excluded from analysis if they had an additional procedure performed at the time of surgery, were less than 18 years of age at the time of surgery or had a history of MicroPulse Trans-Scleral Cyclophotocoagulation (MPCPC) in the operative eye. Additionally, patients were excluded from analysis if they had less than 6 weeks of follow-up to avoid biasing data by ignoring early failures in survival analysis. If both eyes of a patient underwent operation, only the first operated eye was included. If a patient underwent an additional glaucoma surgery or laser trabeculoplasty (LTP) on the operative eye, follow-up was concluded at that time.
Surgical Technique
For PEcK and Phaco/ECP, phacoemulsification was followed by insertion of cohesive viscoelastic and then the ECP probe into the sulcus and treatment of 90–360 degrees of ciliary processes in continuous wave mode at a power of 0.10–0.55 Watts until observing whitening and shrinkage of ciliary processes. After ECP for PEcK and after phacoemulsification for Phaco/KDB, the patient’s head was rotated for visualization, additional cohesive viscoelastic was inserted into the anterior chamber, and the gonioscopy lens was placed onto the cornea. The KDB was introduced into the anterior chamber and an ab-interno trabecular excision was performed. The KDB was passed through the trabecular meshwork (TM) between 1.0–5.0 clock hours in an inside out fashion until two strips of TM were formed. These techniques are represented in the cited surgical video.18 At completion of all procedures, a drop of prednisolone and moxifloxacin antibiotic were placed on the eye before it was patched and shielded.
Data Collection
Baseline characteristics were collected from electronic health records of subjects and included age, gender, preferred language, race/ethnicity, glaucoma type, and best corrected distance visual acuity (BCVA). Glaucoma type was denoted to be mixed mechanism when there was more than one etiology of glaucomatous disease documented, most frequently with both closed angle and open angle. Baseline medication burden was recorded as the number of medications prescribed, including the number of constituent agents if fixed-dose combination medications were used. Baseline IOP was defined as the mean of measurements made by the surgeon using Goldmann applanation tonometry on two consecutive visits prior to surgery. If Goldmann applanation tonometry was not available for a pre- or postoperative visit, measurements from an iCare tonometer (Tiolat Oy, Helsinki, Finland) or Optical Response Analyzer (Reichert Ophthalmic Instruments, Inc., Buffalo, NY, USA) were recorded. Glaucoma stage was recorded and assigned based on the American Academy of Ophthalmology Preferred Practice Pattern guidelines (ICD-10 Glaucoma Reference Guide).19 Prior history of ocular surgery, laser peripheral iridotomy (LPI), and LTP in the operative eye was recorded. Prior LTP included Argon Laser Trabeculoplasty (ALT) or Selective Laser Trabeculoplasty (SLT). The goal IOP was a preoperatively designated target that corresponded to a 20% IOP reduction from the level at which glaucoma progression was first documented.2
Postoperative data were collected from 1 day, 6 (±2.5) weeks, 3 (±1) months, 6 (±2) months, 12 (±3) months, 18 (±3) months, 24 (±3) months, 36 (±3) months, 48 (±3) months, and 60 (±3) months. Recorded measurements included IOP, BCVA, number of glaucoma medications, and presence of postoperative complications. If subjects required further glaucoma procedure or if patients underwent laser capsulotomy within 12 months, this was recorded.
Outcomes
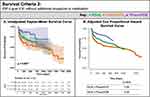
Primary outcomes were the pattern of change in intraocular pressure (IOP) and medication burden for up to 60 months postoperatively compared between procedures, as well as survival analyses. We examined two survival criteria, without receiving additional glaucoma procedure or medication:
- Survival Criteria 1 (SC1): IOP ≤ 21 mmHg and ≥ 20% reduction from baseline.
- Survival Criteria 2 (SC2): IOP ≤ goal IOP, where goal IOP represented a preoperatively designated 20% reduction from the level at which glaucoma progression occurred.2
Separate to additional glaucoma procedure or medication, failure required a demonstrated inability to meet the above IOP criteria at ≥ 2 consecutive visits as this reduced confounding from temporary intraocular pressure fluctuations. Secondary outcomes included the pattern of change in the Logarithm of the Minimum Angle of Resolution (logMAR), as well as the procedure length and incidence of postoperative complications.
Statistical Analysis
Statistical analyses were performed using R statistical programming software (RStudio 2022.02.0). Number of medications and logMAR were treated as continuous variables. Statistical differences in baseline characteristics between cohorts were evaluated by Kruskal–Wallis rank sum tests and Pearson’s Chi-squared tests.20,21
Generalized Estimating Equations (GEE) were used to assess both the magnitude and temporality of change and to properly account for repeated outcome measurements.22,23 Additionally, GEEs are often suggested as the preferred model type for interpreting population findings for continuous variables of repeated measurements without known distributions and with a small sample size.24 Through the GEEs, semi-parametric longitudinal regression models were fit to each outcome, including IOP, medication burden, and logMAR. Models were examined between procedures and across each categorical timepoint throughout 60 months. For selected baseline characteristics that were significantly or near significantly different between procedures, the respective variables were included in the models for adjustment of these differences. Statistical significance of covariates within the models was evaluated using Wald tests, which resulted in a single p-value that compared the pattern of change across all timepoints, between procedures, or under both conditions, while holding all other covariates constant. ANOVA was used in multivariate analysis of all procedures.23
Kaplan–Meier survival probabilities were generated and are presented as plots of event-free survival. Statistical difference in the pattern of survival was evaluated using Log rank tests.25 To assess the impact of selected baseline characteristics that were significantly or near significantly different between procedures, a Cox Proportional Hazards (Cox PH) regression model was fit to the survival criterion, procedure, and selected baseline characteristics. Adjusted Cox PH Survival Curves were generated to show how type of procedure influenced survival estimated from a model that adjusted for group differences.24–27
Results
Baseline Characteristics and Statistical Adjustment
One thousand eight hundred thirty-three (1833) visits from 271 eyes of 271 patients were included. Mean preoperative IOP was 17.6 ± 5.0 (SD) mmHg on 3.0 ± 1.4 medications in the PEcK group (n = 128), 17.9 ± 5.1 mmHg on 2.2 ± 1.5 medications in the Phaco/ECP group (n = 78), and 16.1 ± 4.3 mmHg on 0.4 ± 1.0 medications in the Phaco/KDB group (n = 65) (Table 1). Subjects had a mean age of 72.35, had predominantly mild or moderate glaucoma (69%), and were naïve to surgery (98.9%). Baseline characteristics that were significantly different included fewer medications in the Phaco/KDB group (p<0.001), race-ethnicity (p=0.030), glaucoma type (p<0.001), and more frequent prior LPI on the operative eye in the Phaco/ECP group (p<0.001). For the latter three characteristics, PEcK and Phaco/KDB groups included predominantly primary open-angle glaucoma, while the Phaco/ECP group comprised mostly patients with mixed-mechanism glaucoma who were thus more frequently of Asian race-ethnicity and who had thus more frequently underwent prior LPI.
 |
Table 1 Baseline Characteristics |
Additionally, variables for mean preoperative IOP (p = 0.056), prior LTP (p = 0.055), and sex (p = 0.078) approached significant difference. Thus, GEEs were statistically adjusted for baseline mean IOP, medication burden, prior LTP, sex, and glaucoma type. Survival curves were statistically adjusted for baseline mean IOP, medication burden, prior LTP, sex, and prior LPI. We did not adjust simultaneously by glaucoma type, race-ethnicity, and prior LPI because, as discussed above, they trended together. Prior LPI was used for the survival curves over glaucoma type to minimize risk of overfitting in the absence of plans to stratify by severity.
Between PEcK and Phaco/ECP, surgeons performed ECP in PEcK at higher power (p<0.001), often over fewer degrees of ciliary body processes (p = 0.06). Between PEcK and Phaco/KDB, surgeons incised more clock hours in the KDBs performed on PEcK subjects (p < 0.001).
Procedural and Comparative Efficacy
For more than 36 months, all procedures resulted in significant patterns of IOP and medication reduction (all p < 0.001), before and after statistical adjustment (Table 2 and Table 3). At 18 months, mean IOP was reduced to 12.2 ± 3.2 mmHg on 2.0 ± 1.4 medications after PEcK, 13.6 ± 2.4 mmHg on 1.7 ± 1.3 medications after Phaco/ECP, and 14.1 ± 4.4 mmHg on 0.5 ± 1.0 medications after Phaco/KDB. Graphical representations of IOP and medication burden are included in Supplemental Figure 1, and reductions of mean IOP and percent reductions are reported in Supplemental Table 1. The parameters of all GEE models are reported in Supplemental Table 2.
 |
Table 2 Change in Intraocular Pressure |
 |
Table 3 Change in Medication Burden |
The reduction pattern in IOP was significantly different when comparing all groups over time and favored PEcK, before and after statistical adjustment (p = 0.04 and p = 0.03, respectively). In pairwise comparison of PEcK to Phaco/ECP, the reduction pattern in IOP was significantly different and favored PEcK over Phaco/ECP, before and after statistical adjustment (both p = 0.02). The reduction patterns in IOP following PEcK and Phaco/KDB were not different before statistical adjustment (p = 0.13) and trended toward significance favoring PEcK after statistical adjustment (p = 0.07).
The reduction pattern in medications was not significantly different between procedures, with or without statistical adjustment (p = 0.11 and p = 0.17, respectively). In pairwise comparison of PEcK and Phaco/ECP, the reduction patterns in medications were not different, before and after statistical adjustment (p = 0.15 and p = 0.09, respectively). Prior to adjustment, the reduction patterns in medication were different between PEcK and Phaco/KDB, in favor of the latter (p = 0.04). After adjustment, pairwise comparison of the GEEs for medication burden were not different (p = 0.13).
At 12 months, 46% of PEcK patients, 44% of Phaco/ECP patients, and 40% of Phaco/KDB patients survived under SC1 to achieve and maintain a 20% IOP reduction (Figure 1). SC1 survival was not significantly different between procedures prior to adjustment (p = 0.43) or after. Meanwhile, 69% of PEcK patients, 57% of Phaco/ECP patients, and 87% of Phaco/KDB patients survived at 12 months under SC2 to achieve and maintain goal IOP (Figure 2). SC2 survival was significantly different between procedures prior to adjustment (p = 0.008). After adjustment, SC2 survival was not different between PEcK and Phaco/ECP (p = 0.09) or between PEcK and Phaco/KDB (p = 0.39).
Procedural time averaged 36.8 minutes and was not different between procedures (p = 0.18) (Table 1). Subjects who underwent either procedure experienced significant improvement in logMAR throughout GEE models across all timepoints, before and after adjustment (both p < 0.001) (Supplemental Table 3). Prior to adjustment, the pattern of improvement in logMAR was similar between procedures (p = 0.81). After adjustment, there was significant difference in the pattern of improvement in logMAR, which favored PEcK over Phaco/ECP (p = 0.04).
Postoperative Complications
Postoperative corneal edema resolved before 3 months, except in 3 cases where the finding persisted ≤ 18 months (Table 4). Postoperative inflammation resolved before 6 months, except in 6 cases which persisted ≤ 12 months and included one PEcK case complicated by rebound iritis. Postoperative hyphema or microhyphema resolved before 3 months, except for 3 cases which persisted ≤ 6 months. There were 10 cases of postoperative cystoid macular edema (CME) in patients who underwent either PEcK or Phaco/ECP, including one case with a preoperative history of CME.
 |
Table 4 Procedural Complications |
Additional procedural intervention was performed for 8.49% of total eyes, including 11 glaucoma drainage implants, 5 Xen Gel implants, 3 trabeculectomies, 3 MPCPC, and 1 LTP. These surgeries were performed on 15 patients in the PEcK group, 5 patients in the Phaco/ECP group, and 3 patients in the Phaco/KDB group.
Discussion
This study examines the efficacy of cMIGS relative to all its constituent sMIGS for the first time. Further, we demonstrate that patients who underwent PEcK, Phaco/ECP, or Phaco/KDB experienced significant reductions in both IOP and medication burden for more than 36 months, which is the first time that PEcK outcomes have been reported for more than 12 months postoperatively.1,2,17
PEcK, Phaco/ECP, and Phaco/KDB resulted in sustained reductions in IOP for more than 36 months, with magnitudes comparable to those reported in the other studies of patients with predominantly mild or moderate glaucoma.1–4,6–17 The IOP reduction following each procedure was also associated with a simultaneous significant reduction in the medication burden. Despite being rarely reported, PEcK was associated in our study with a 12-month reduction in mean IOP of 3.8 mmHg on 1.1 fewer medications, which showed similar efficacy to that reported by Izquierdo et al and Klug et al. The latter study suggested potentially greater efficacy of PEcK compared to ICE which had an associated 12-month reduction in mean IOP of 1.4 mmHg on 0.8 fewer medications.2,17
Furthermore, PEcK and its constituent sMIGS had moderate efficacy in survival maintaining IOP ≤ 21 mmHg and ≥20% IOP reduction without additional procedure or medication at 12 months postoperatively, experiencing 46%, 44%, and 40% SC1 survival following PEcK, Phaco/ECP, and Phaco/KDB respectively. The moderate SC1 efficacies might have been affected by the study population who had a mean baseline IOP within normal range. All procedures had greater efficacy at maintaining IOP ≤ goal IOP without additional procedure or medication (69%, 57%, and 87% SC2 survival at 12 months respectively). Thus, while many subjects did not maintain a 20% IOP reduction from their preoperative baseline, a majority of subjects did achieve and maintain an IOP reduction appropriate to the clinical goal determined by a glaucoma surgeon and corresponding to a 20% IOP reduction from the level at which glaucoma progression was first documented.
In comparative analysis, PEcK conferred greater IOP reduction than its constituent sMIGS by ANOVA (p < 0.001) and by pairwise comparison between PEcK and Phaco/ECP (p = 0.02). Although the IOP reduction patterns following PEcK and Phaco/KDB were not statistically different, they did trend in favor of PEcK (unadjusted p = 0.13, adjusted p = 0.07) despite the baseline and possibly unmeasured characteristics of milder glaucoma in Phaco/KDB.
PEcK and its constituent sMIGS did not differ in the patterns of medication reduction. With this, adjusted comparisons of medication reduction did approach significance in favor of Phaco/KDB over PEcK (p = 0.13) and PEcK over Phaco/ECP (p = 0.09). The improved pattern of medication reduction following Phaco/KDB compared to the other procedures may have been affected by an inability to fully adjust for unmeasured baseline characteristics of disease severity given that the Phaco/KDB group had lower baseline IOP and medication burden.
PEcK and its constituent sMIGS performed similarly by procedural time (p = 0.18) and SC1 survival (p = 0.43). Meanwhile, the results of SC2 survival suggest benefit of PEcK over Phaco/ECP in unadjusted and adjusted analyses, as well as meaningfully similar efficacy to Phaco/KDB given the inability to adjust for unmeasured baseline characteristics of greater disease severity in the PEcK group. Despite greater severity of glaucoma, patients who underwent the cMIGS procedure sustained similar or greater SC1 and SC2 survival relative to the constituent sMIGS performed in patients with lower baseline IOP, fewer baseline medications, less prior LTP, and a greater proportion of patients with mild stage glaucoma. In this way, as a cMIGS, PEcK may be associated with additive or synergistic efficacy. It is also possible that markers of greater disease severity are predictive of surgical efficacy with MIGS, and further research is needed.
PEcK and its constituent sMIGS were all effective at restoring vision and were safe. On post-operative day 1, PEcK was associated with more corneal edema, inflammation, and hyphema or microhyphema than its sMIGS. Beyond this immediate post-operative period, these complications were rare, were similar between procedure categories, and thus were insufficient to detect any hypothesized predisposition to inflammation following ECP and to bleeding following KDB.1,28 Of note, only procedures involving ECP were associated with postoperative CME, albeit the incidence of this complication was within the reported range of 0 to 10% in literature on ECP.5 While the post-operative CME rate seemed to favor Phaco/KDB, given that it lacked an ECP component, PEcK still resulted in a statistically greater pattern of reduction in logMAR (p = 0.04) after adjustment. While this improved visual outcome following PEcK may not be clinically significant, it does reinforce that concern for increased rate of inflammation, hyphema, or CME from the cMIGS did not compromise visual outcomes over time.
This retrospective nonrandomized study is limited by selection bias for undergoing PEcK or its constituent sMIGS at surgeon discretion based on individual practitioner expertise, individual patient factors, and surgical factors, leading to associated and not unexpected differences in baseline characteristics and disease severity. Although we statistically adjusted for many inter-group differences, additional unmeasured differences may exist. Use of GEEs reduced limitations from using repeated outcome measurements without known distributions, with a small sample size, and with attrition in all procedure groups, though these limitations do still affect the study. Further, the generalizability of this study may be diminished given that baseline mean IOP was within a normal range and comprised patients who sought care at a tertiary care center. This study was limited to analysis of clinical efficacy and did not include analysis of cost efficacy, which will be important in future research. The study adhered to the Guidelines on Design and Reporting of Glaucoma Surgical Trials from the World Glaucoma Association.29
In summary, PEcK may confer greater IOP reduction without added procedural time compared to Phaco/ECP and Phaco/KDB in predominantly mild or moderate glaucoma. PEcK may also lead patients to maintain IOP ≤ goal IOP more often than Phaco/ECP and as often as Phaco/KDB. Further, PEcK had a similar safety profile to its constituent sMIGS in patients for whom both ECP and KDB were clinically appropriate. By reporting the efficacy of cMIGS relative to all of its constituent sMIGS for the first time, we hope this methodology will be applied to further research on cMIGS in larger populations, over longer follow-up intervals, and in prospective studies.
Summary
What Was Known
- Understanding the relative efficacy of combined microinvasive glaucoma surgeries (cMIGS) is integral to clinical decision making, but no study or review has directly compared the combination procedure to all constituent MIGS.
- PEcK, which is combined Phacoemulsification, Endocyclophotocoagulation (ECP), and Kahook Dual Blade (KDB), may offer greater IOP reduction than Phaco/ECP for 12 months postoperatively.
- PEcK has never been compared to its constituent Phaco/KDB or studied for longer than 12 months postoperatively.
What This Paper Adds
- PEcK, Phaco/ECP, and Phaco/KDB led to significant patterns of reduction in IOP and medication burden for more than 36 months, supplementing the evidence that MIGS are effective.
- PEcK may be more efficacious than its constituent MIGS by conferring greater IOP reduction and similar outcomes in medications and procedural time.
- PEcK led patients to maintain IOP ≤ goal IOP more often than Phaco/ECP and as often as Phaco/KDB.
Abbreviations
ALT, Argon Laser Trabeculoplasty; BCVA, Best corrected distance visual acuity; CME, Cystoid macular edema; cMIGS, Combined MIGS, denoting a procedure of two or more MIGS; Cox PH, Cox Proportional Hazards; GEE, Generalized Estimating Equations; ICE, cMIGS procedure combining iStent insertion, Cataract extraction, and ECP; IOP, Intraocular pressure; logMAR, Logarithm of the Minimum Angle of Resolution; LPI, Laser Peripheral Iridotomy; LTP, Laser trabeculoplasty; MIGS, Microinvasive glaucoma surgery; MPCPC, MicroPulse Trans-Scleral Cyclophotocoagulation; PEcK, cMIGS procedure combining Phacoemulsification, Endocyclophotocoagulation, and Kahook Dual Blade; Phaco, Phacoemulsification; Phaco/ECP, Phacoemulsification with endocyclophotocoagulation; Phaco/KDB, Phacoemulsification with Kahook Dual Blade; SC1, Survival Criteria 1; SC2, Survival Criteria 2; SLT, Selective Laser Trabeculoplasty; sMIGS, Single MIGS, denoting a procedure that included only one MIGS; TM, Trabecular meshwork.
Acknowledgments
Varshini Odayar, an undergraduate at Harvard University, contributed to data collection of less than 10 patients. The authors are grateful that this research was generously supported by donations from Mr. and Mrs. Charles and Anne Gifford (Concord, Massachusetts, USA), Mr. and Mrs. Joseph and Cathey S. Leitch (Charleston, South Carolina, USA), and Stephen Traynor. The article has been presented as an e-poster at the American Academy of Ophthalmology (AAO) 2022 Annual Conference, Chicago, USA, October 2022.
Author Contributions
All authors made a significant contribution to the work reported, whether that was in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas. All authors have drafted or written, or substantially revised or critically reviewed the article. All authors have agreed on the journal to which the article will be submitted. All authors have reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. All authors have agreed to take responsibility and accountability for the contents of the article.
Disclosure
Dr David Solá-Del Valle reports being a speaker for Allergan (an AbbVie company) in 2021 for two weeks. The authors report no other conflicts of interest in this work.
References
1. Mai DD, Ingram Z, Oberfeld B, Solá-Del Valle D. Combined microinvasive glaucoma surgery - a review of the literature and future directions. Semin Ophthalmol. 2023;1–8. doi:10.1080/08820538.2023.2181665
2. Klug E, Chachanidze M, Nirappel A, et al. Outcomes of phacoemulsification and endoscopic cyclophotocoagulation performed with dual blade ab interno trabeculectomy or trabecular micro-bypass stent insertion. Eye Lond Eng. 2021. doi:10.1038/s41433-021-01475-4
3. Uram M. Combined phacoemulsification, endoscopic ciliary process photocoagulation, and intraocular lens implantation in glaucoma management. Ophthalmic Surg. 1995;26(4):346–352.
4. Netland PA, Mansberger SL, Lin S. Uncontrolled intraocular pressure after endoscopic cyclophotocoagulation. J Glaucoma. 2007;16(2):265–267. doi:10.1097/01.ijg.0000243475.36213.41
5. Seibold LK, SooHoo JR, Kahook MY. Endoscopic Cyclophotocoagulation. Middle East Afr J Ophthalmol. 2015;22(1):18–24. doi:10.4103/0974-9233.148344
6. Anand N, Klug E, Nirappel A, Solá-Del Valle D. A review of cyclodestructive procedures for the treatment of glaucoma. Semin Ophthalmol. 2020;35(5–6):261–275. doi:10.1080/08820538.2020.1810711
7. Dorairaj SK, Seibold LK, Radcliffe NM, et al. 12-month outcomes of goniotomy performed using the kahook dual blade combined with cataract surgery in eyes with medically treated glaucoma. Adv Ther. 2018;35(9):1460–1469. doi:10.1007/s12325-018-0755-4
8. ElMallah MK, Seibold LK, Kahook MY, et al. 12-month retrospective comparison of kahook dual blade excisional goniotomy with istent trabecular bypass device implantation in glaucomatous eyes at the time of cataract surgery. Adv Ther. 2019;36(9):2515–2527. doi:10.1007/s12325-019-01025-1
9. Sieck EG, Epstein RS, Kennedy JB, et al. Outcomes of Kahook Dual Blade goniotomy with and without phacoemulsification cataract extraction. Ophthalmol Glaucoma. 2018;1(1):75–81. doi:10.1016/j.ogla.2018.06.006
10. Le C, Kazaryan S, Hubbell M, Zurakowski D, Ayyala RS. Surgical outcomes of phacoemulsification followed by istent implantation versus goniotomy with the kahook dual blade in patients with mild primary open-angle glaucoma with a minimum of 12-month follow-up. J Glaucoma. 2019;28(5):411–414. doi:10.1097/IJG.0000000000001143
11. Ventura-Abreu N, García-Feijoo J, Pazos M, Biarnés M, Morales-Fernández L, Martínez-de-la-casa JM. Twelve-month results of ab interno trabeculectomy with Kahook Dual Blade: an interventional, randomized, controlled clinical study. Graefes Arch Clin Exp Ophthalmol. 2021;259(9):2771–2781. doi:10.1007/s00417-021-05213-0
12. Iwasaki K, Takamura Y, Orii Y, Arimura S, Inatani M. Performances of glaucoma operations with Kahook Dual Blade or iStent combined with phacoemulsification in Japanese open angle glaucoma patients. Int J Ophthalmol. 2020;13(6):941–945. doi:10.18240/ijo.2020.06.13
13. Aoki R, Hirooka K, Goda E, et al. Comparison of surgical outcomes between microhook ab interno trabeculotomy and goniotomy with the Kahook Dual Blade in combination with phacoemulsification: a retrospective, comparative case series. Adv Ther. 2021;38(1):329–336. doi:10.1007/s12325-020-01543-3
14. Ansari E, Loganathan D. 12-month clinical outcomes of combined phacoemulsification and ab interno trabeculectomy for open-angle glaucoma in the United Kingdom. PLoS One. 2021;16(6):e0252826. doi:10.1371/journal.pone.0252826
15. Falkenberry S, Singh IP, Crane CJ, et al. Excisional goniotomy vs trabecular microbypass stent implantation: a prospective randomized clinical trial in eyes with mild to moderate open-angle glaucoma. J Cataract Refract Surg. 2020;46(8):1165–1171. doi:10.1097/j.jcrs.0000000000000229
16. Porter M, Garza A, Gallardo M. Excisional goniotomy in latino patients with open-angle glaucoma: outcomes through 24 months. Clin Ophthalmol. 2020;14:3619–3625. doi:10.2147/OPTH.S271923
17. Izquierdo JC, Agudelo N, Rubio B, et al. Combined phacoemulsification and 360-degree endocyclophotocoagulation with and without a Kahook Dual Blade in patients with primary open-angle glaucoma. Clin Ophthalmol. 2021;15:11–17. doi:10.2147/OPTH.S282440
18. PEcK. Phacoemulsification, endoscopic cyclophotocoagulation, & dual blade Ab-interno trabeculectomy; 2020. Available from: https://www.youtube.com/watch?v=OHJpGjc5wsA.
19. Gedde SJ, Vinod K, Wright MM, et al. Primary open-angle glaucoma preferred practice pattern®. Ophthalmology. 2021;128(1):P71–P150. doi:10.1016/j.ophtha.2020.10.022
20. Ho D, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. 2011;42(1):1–28. doi:10.18637/jss.v042.i08
21. Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. doi:10.18637/jss.v067.i01
22. Fitzmaurice GM. Longitudinal Data Analysis. CRC Press; 2009.
23. Molenberghs G, Verbeke G. Models for Discrete Longitudinal Data. Springer Science & Business Media; 2006.
24. Hubbard AE, Ahern J, Fleischer NL, et al. To GEE or not to GEE: comparing population average and mixed models for estimating the associations between neighborhood risk factors and health. Epidemiol Camb Mass. 2010;21(4):467–474. doi:10.1097/EDE.0b013e3181caeb90
25. Kassambara A, Kosinski M, Biecek P, Fabian S. Survminer: drawing Survival Curves using “ggplot2.”; 2021. Available from: https://CRAN.R-project.org/package=survminer.
26. Nieto FJ, Coresh J. Adjusting survival curves for confounders: a review and a new method. Am J Epidemiol. 1996;143(10):1059–1068. doi:10.1093/oxfordjournals.aje.a008670
27. Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. Springer Science & Business Media; 2000.
28. Sng CCA, Barton K. Minimally Invasive Glaucoma Surgery. Springer Nature; 2021.
29. Shaarawy T, Grehn F, Sherwood M, Ebrary I. WGA Guidelines on Design and Reporting of Glaucoma Surgical Trials. Kugler Publications; 2009.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.