Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Cognitive Dysfunction and Its Risk Factors in Patients Undergoing Maintenance Hemodialysis
Authors Tian X, Xia X, Yu H, Chen H, Jiang A, Xin L
Received 29 June 2022
Accepted for publication 31 October 2022
Published 24 November 2022 Volume 2022:18 Pages 2759—2769
DOI https://doi.org/10.2147/NDT.S380518
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Xiaolin Tian,1 Xiaoshuang Xia,2 Haibo Yu,3 Haiyan Chen,3 Aili Jiang,3 Li Xin2
1Department of Rehabilitation Medicine, The Second Hospital of Tianjin Medical University, Tianjin, People’s Republic of China; 2Department of Neurology, The Second Hospital of Tianjin Medical University, Tianjin, People’s Republic of China; 3Blood Purification Center, The Second Hospital of Tianjin Medical University, Tianjin, People’s Republic of China
Correspondence: Li Xin, Department of Neurology, The Second Hospital of Tianjin Medical University, Tianjin, People’s Republic of China, Tel +86 22-88329030, Email [email protected] Aili Jiang, Blood Purification Center, The Second Hospital of Tianjin Medical University, No. 23, Pingjiang Road, Hexi District, Tianjin Municipality, Tianjin, 300211, People’s Republic of China, Tel +86 22-88326563, Email [email protected]
Objective: Cognitive impairment (CI) in Maintenance hemodialysis (MHD) is attracting increasing attention. This study aims to clarify the prevalence and risk factors for cognitive dysfunction in patients on MHD who have no history of stroke.
Methods: A total of 99 patients with no history of stroke undergoing MHD were enrolled. Global cognitive function was evaluated using the Montreal Cognitive Assessment scale. Attention and executive functions were evaluated by the Digital Span (DS) test and the Color Trail Test (CTT). The Hamilton Depression and Anxiety scales were used to assess depression and anxiety status. The effects of patient background factors, laboratory indicators, anxiety, and depression on cognitive dysfunction were examined by regression analysis.
Results: There were 69.70% of the patients had general CI, 65.65% had depression, and 57.57% had anxiety. The forward and backward DS in the cognitively impaired (CI) group were shorter than in the normal cognitive function (NCF) group (P< 0.05). Times required for CTT–I, CTT–II, and CTT II − CTT I were longer in the CI group than in the NCF group (P< 0.05). Hemoglobin levels were lower, and parathyroid hormone (PTH) and uric acid levels were higher in the CI group than in the NCF group (P< 0.05). Hemoglobin levels were negatively correlated with CI in these patients (odds ratio [OR] 0.634, P< 0.05) and PTH, and uric acid levels were positively correlated with CI (OR 1.028, P< 0.05; and OR 1.011, P< 0.05). The proportions of patients with diabetes and depression were higher in the CI group (P< 0.05).
Conclusion: There was a high prevalence of CI with significant impairment of attention and executive ability in MHD patients who had no stroke history. Hemoglobin may protect cognitive function, while diabetes, PTH, and uric acid levels may be risk factors. Depressive and anxiety states may aggravate CI in MHD patients.
Keywords: end-stage renal disease, maintenance hemodialysis, cognitive impairment, executive ability, risk factors
Introduction
End-stage renal disease (ESRD) refers to the final stage of irreversible damage to renal function caused by various kidney diseases, including chronic nephritis, diabetic nephropathy, and hypertensive nephropathy. Peritoneal dialysis (PD) and hemodialysis are the main treatments for ESRD in China. Cognitive functioning in patients with ESRD has become a major concern in recent years.1 A meta-analysis of the impact of hemodialysis and PD on cognitive function was completed showed that patients on hemodialysis had worse cognitive functioning and a higher risk of dementia than those undergoing PD.2 Regular hemodialysis is also called maintenance hemodialysis (MHD).
Each year, there are approximately two million patients with ESRD in China. In 2019, the number of patients on hemodialysis exceeded 630,000. Cognitive impairment (CI) may affect patients’ understanding and processing of information, their full participation in decision-making regarding their health care, and their ability to comply with complex medical plans and adjust their diet and water intake correctly.3 Furthermore, hospitalization and mortality rates and the risk of low quality of life are higher in patients with CI.4 Therefore, cognitive dysfunction is considered a serious problem in patients on MHD.
In recent years, CI in patients on MHD has received considerable attention. Previous studies have focused on increased uremic toxins, imbalance in dialysis, intracranial infarction, oxidative stress, hyperhomocysteinemia, and chronic inflammation.5 Mel et al investigated the cognitive status of patients with renal insufficiency at different periods in the outpatient clinic and suggested that the degree of CI is related to the severity of chronic kidney disease (CKD) and that MHD improves cognitive performance. Meanwhile, Kovarova et al reported that cognitive dysfunction is related to decreased brain oxygenation in patients on MHD.6 So, the relationship between MHD and cognitive dysfunction has not been established exactly.
MHD can effectively clear creatinine, urea nitrogen, and other metabolic waste products and allow ultrafiltration of excess water accumulated in the body. However, when blood contacts the artificial membrane during extracorporeal circulation, some of the blood components can adhere to it, causing changes in white blood cell (WBC), red blood cell (RBC), and platelet (PLT) counts and hematocrit (HCT) and PLT distribution width (PDW). A cohort study by Dlugaj et al concluded that people with anemia have lower verbal memory and executive function and that anemia is related to mild CI.7 Bahrami et al found that adolescent girls with anemia were 1.73 times more likely to have CI than their nonanemic counterparts.8 As is well known, reduced renal secretion of erythropoietin in patients on MHD can lead to anemia. Although recombinant human erythropoietin is routinely supplemented clinically, anemia is not easy to correct in patients on MHD, and the relationship between hemoglobin levels and CI has yet to be clarified.
Secondary hyperparathyroidism is the most significant endocrine disorder in patients on MHD. Parathyroid hormone (PTH) may cause damage to the skin, bones, and nervous system. Studies have suggested that high variability in serum phosphorus is an independent risk factor for all-cause death in patients on MHD.9 Whether the abnormal levels of PTH, serum calcium, serum phosphorus calcium, and phosphorus are related to CI in patients on MHD needs further research.
Besides global CI, damaged executive ability and attention are considered the typical manifestations of mild CI. In the normal population, depression is significantly negatively correlated with cognitive function, suggesting that anxiety and depression in patients are related to CI.10 Patients on MHD lack an appetite for food, and their water and food intake are controlled, so the proportion with anxiety and depression and the impact of these conditions on their cognitive function is worthy of further study.
Vascular factors play a very important role in dementia, and the incidence of cerebrovascular disease in patients with regular dialysis is 6–10 times that of the normal population.11 The severity of CI in patients with a history of stroke can be judged. However, there are few studies on CI in patients on MHD without stroke history. This study focuses on the proportion of patients with CI in a blood purification center and its influencing factors.
Methods
Ninety-nine patients on MHD in the Blood Purification Center of the Second Hospital of Tianjin Medical University between January 2018 and December 2018 were enrolled in this prospective study, which the hospital ethics committee approved. Each study participant signed a written informed consent form. Each patient underwent a magnetic resonance imaging scan before inclusion. The flowchart of enrollment is shown in Figure 1.
 |
Figure 1 The flowchart of enrollment. |
The study inclusion criteria were as follows: (1) aged 18–80 years and (2) on regular hemodialysis (three times a week) for over 12 months.
The following exclusion criteria were applied: (1) history of a large territorial infarct or intracerebral hemorrhage; (2) history of multiple cerebral lobe microbleeds (excluding cerebral amyloid angiopathy)(3) inability to cooperate with the scale assessment due to hearing impairment, visual impairment, congenital intellectual disability, psychiatric disease, heart failure, or chronic obstructive pulmonary disease; (4) hereditary cerebrovascular disease; and (5) known neurodegenerative disease, such as Alzheimer’s or Parkinson’s disease.
Patient information was recorded, including gender, age, duration of dialysis (months), years of education, and history of hypertension, diabetes, and coronary heart disease. The primary disease underlying ESRD was recorded separately as nephrogenic damage, hypertensive renal damage, diabetic renal damage, or other. Biochemical indices included the RBC count, WBC count, PLT count, hemoglobin, HCT, PDW, serum calcium, serum inorganic phosphorus, serum potassium, PTH, alkaline phosphatase, uric acid, albumin, aspartate aminotransferase, triglycerides, total cholesterol, and indicators of CO2 combining power. The values for all laboratory indicators were the average for three months before the scale assessment. The values of all laboratory indicators were the average value over three months before data collection.
The Montreal Cognitive Assessment (MoCA) scale was used to evaluate global cognitive function. Each item was analyzed separately, and patients with a MoCA score < 26/30 were defined as cognitively impaired. The Digital Span (DS) test was scored with the highest number of correct repetitions. The reaction time (RT) and the number of errors on the Color Trail Test (CTT)–I and CTT–II were recorded, and the CTT interference score was calculated as CTT II RT − CTT I RT. The Hamilton Depression Scale–17 and Hamilton Anxiety Scale–14 were used to measure patients’ depression status and anxiety status, respectively. All patients were given these tests on the second day of dialysis by a neurologist in a quiet, undisturbed environment to exclude potential interference factors, such as patient discomfort and poor sleep on the day before the test.
Statistical Analysis
Data that followed a normal distribution were examined using the independent samples t-test, and other data were assessed using the Mann–Whitney U-test. The Chi-squared test was used to compare the data between the CI group and the normal cognitive function (NCF) group. The risk factors for CI were identified by multivariate logistic regression analysis. The threshold P-value was set at 0.05. All statistical analyses were performed using SPSS™ version 17.0 (IBM Corp., Armonk, NY, USA).
Results
Basic Patient Demographic and Clinical Characteristics
The average patient age was 61.50 ± 9.19 years. Of these, 41 patients (41.41%) were female (mean age 63.45 ± 7.69 years), and 58 (58.59%) were male (mean age 59.68 ± 9.68 years). The patients were divided into four subgroups according to age: <49 years, 50–59 years, 60–69 years, and ≥70 years. The age distribution was calculated as percentages.
The primary etiology of ESRD was chronic glomerulonephritis (n = 20), diabetic nephropathy (n = 22), hypertensive nephropathy (n = 21), and unknown (n = 36). Of the enrolled patients, 76 (76.77%) had hypertension, 36 (36.36%) had diabetes, and 41 (41.41%) had coronary heart disease. The participants were also stratified according to years of education: 9 years (including junior high school graduation and below; n = 48, 48.48%), ≥9 years, and ≤12 years (including high school, technical secondary school, vocational high school; n = 25, 25.25%), and >12 years (including university undergraduates, colleges, postgraduates, and above; n = 26, 26.26%). After calculating these data, their impact on cognitive function was investigated.
Cognitive Impairment in Patients on Maintenance Hemodialysis
Patients with a MoCA score <26 points were deemed to have CI, and those with a MoCA score ≥26 points were considered to have NCF. The patients were divided into a CI group (n = 69) and an NCF group (n = 30). Each MoCA subitem was analyzed individually and compared between the two groups. There were statistically significant differences between groups in the seven subitems (P < 0.05), and there was a clear difference in scores between visual space and executive function of >2 points (Table 1).
 |
Table 1 Comparison of Sub-Items on the Montreal Cognitive Assessment Between the Group with Cognitive Impairment and the Group with Normal Cognitive Function |
Comparison of Digital Span Test and Color Trail Test Scores Between the Study Groups
The mean forward DS was 6.28 ± 1.02 in the CI group and 7.33 ± 1.21 in the NCF group. The backward DS was 4.47 ± 1.12 in the CI group and 5.51 ± 0.92 in the NCF group. There was a significant difference in both aspects.
The CTT–I RT was 95.00 (71.895–147.08) s in the CI group and 65.15 (53.255–81.475) s in the NCF group. The CTT–II RT was 186.64 (129.085–249.00) s in the CI group and 129.315 (97.8–166.72) s in the NCF group. The CTT interference score was 73.59 (50.03–135.95) s in the CI group and 53 (37.52–78.9) s in the NCF group. There were statistically significant differences between the groups in these three indices (all P < 0.05) (Table 2).
 |
Table 2 Comparison of Digital Span Test and Color Trail Test Results in the Group with Cognitive Impairment and the Group with Normal Cognitive Function |
Comparison of Clinical Data Between the Study Groups
Age, gender, and dialysis duration were compared between the two groups, and no significant difference was found in these three factors (P > 0.05). A comparison was also made with the RBC count, WBC count, PLT count, hemoglobin, HCT, PDW, serum calcium, serum inorganic phosphorus, PTH, alkaline phosphatase, uric acid, albumin, aspartate aminotransferase, triglycerides, total cholesterol, and CO2 combining power between the two groups. The hemoglobin levels in the CI group were lower than in the NCF group, and the difference was statistically significant (P < 0.05). The PTH and uric acid levels were significantly higher in the CI group than in the NCF group (P < 0.05) (Table 3). The count data were compared between the two groups using the Chi-squared test. There were statistically significant differences in the depression and anxiety status between the CI and NCF groups (P < 0.05) (Table 4). The proportion of patients on MHD who had diabetes was higher in the CI group than in the NCF group. There were no significant differences between the groups regarding the proportion with hypertension, the age distribution, level of education, or primary kidney disease.
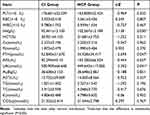 |
Table 3 Comparisons of Clinical Parameters Between Cognitive Impairment Group and Normal Cognitive Function Group |
 |
Table 4 Differences in Hypertension, Diabetes, Anxiety and Depression Status, Causes of End-Stage Renal Disease, Age Distribution, and Education Level Stratification Between the Two Groups |
Logistic Regression Analysis of the Risk Factors for Cognitive Impairment in Patients on Maintenance Hemodialysis
Multivariate logistic regression analysis was performed using NCF and CI as dependent variables and biochemical indicators as independent variables. The results suggested that hemoglobin, HCT, PTH, and uric acid were factors influencing cognitive function. The hemoglobin level was negatively correlated with CI and, therefore, a protective factor (odds ratio 0.634). Higher levels of HCT, PTH, and uric acid were positively correlated with CI, and so were the risk factors. The PLT count, RBC count, WBC count, calcium, inorganic phosphorus, alkaline phosphatase, albumin, aspartate aminotransferase, triglycerides, total cholesterol, potassium, and CO2 combining power were not determinants of CI (Table 5).
 |
Table 5 Logistic Regression Analysis of Laboratory Parameters and Cognitive Impairment |
Discussion
Chronic renal failure is considered a risk factor for CI,12 and MHD is a basic renal replacement therapy for patients with ESRD. However, the mechanism is still unclear. This study investigated the incidence and possible mechanism of CI in patients on MHD.
In China, the number of patients on MHD has increased in recent years. Due to the investment in the national medical insurance policy and the improvement of hemodialysis technology, the survival period of patients with ESRD is getting longer and longer, so the problem of CI is becoming increasingly serious.
In the present study, the MoCA results suggested that 69.70% of patients on MHD were considered to have cognitive dysfunction. Angermann et al reported that the MoCA has high sensitivity and specificity for identifying CI in patients on MHD.13 Therefore, the MoCA score can accurately reflect the actual cognitive level of patients on MHD. However, none of the patients in this study had a history of cerebrovascular disease. Therefore, the actual prevalence of CI in patients on MHD in the present study was higher than 69.70%. Gesualdo et al reported that 76.76% of patients on MHD had CI.14 Angermann et al found that 60.2% of 201 patients on chronic hemodialysis had CI.15 Having CI may affect a patient’s ability to understand and process information, participate fully in making decisions about their health care, adhere to complex medical regimens, and correctly implement dietary and fluid regulations. Patients with CI are at higher risk of hospitalization, mortality, and poorer quality of life.3
The results for the MoCA subitems showed statistically significant differences in visual space and executive ability, naming, attention, language, abstraction, delayed recall, and orientation between the CI and NCF groups. The difference in the scores between visual space and executive ability was >2 points, indicating that the decline in executive function was more prominent in the CI group.
The DS test is a specific neuropsychological test often used to test concentration, attention, instantaneous memory, and memory resistance to information interference. In the present study, forward DS and backward DS were shorter in the CI group than in the NFC group, suggesting that concentration and instantaneous memory were impaired in patients on MHD in the CI group. The Trail Making Test is often used to assess executive function, and the CTT is an improved Chinese version with good objectivity that is a less time-consuming method for evaluating executive function. A prolonged CTT–I RT indicates that the subject has decreased perceptual-motor efficiency, whereas the CTT–II RT indicates the functioning of the brain’s left hemisphere, mainly the effect of attention conversion and perceptual-motor efficiency. The CTT interference score represents executive ability. The present study showed that the CTT–I RT, CTT–II RT, and CTT interference scores were longer in the CI group than in the NCF group (P < 0.01), indicating that patients with CI have decreased perceptual-motor efficiency, decreased attention conversion, and less executive ability.
Compared with the average values in the general population, the time consumption of the CTT–I, CTT–II, and CTT interference scores in this study was clearly prolonged, indicating that the perceptual movement efficiency and attention conversion ability of patients on MHD were reduced and that executive ability was poorer in the CI group than in the NCF group. Sanchez–Fernandez et al used a battery of tests, including the Controlled Oral Word Association Test, the Ruff Figural Fluency Test, the Wechsler Adult Intelligence Scale–III, the Five Digit Test, and the Wisconsin Card Sorting Test, and believed that executive function was lower in patients on MHD than in healthy controls.16 In this study, the test most commonly used to evaluate executive function was selected, and the results showed that it was lower in patients on MHD in the CI group. The prefrontal cortex and the anterior and posterior cingulate cortices are believed to be linked to executive function,17 but the causes of CI in patients on MHD need further research.
Anxiety and depression are common in patients with chronic diseases. Patients on MHD are exposed to long-term hemodialysis, a controlled diet and water intake, frequent hospitalizations, various other complications, and are very prone to psychological problems. The reported prevalence of depression in the dialysis population varies from 22.8% (for interview-based diagnosis) to 39.3%.18 Depression and anxiety are thought to increase mortality in patients on MHD.19 As is well known, cognitive disorder is one of the symptoms of depression. In this study, the different grades of anxiety and depression were compared between the CI and NCF groups. Anxiety and depression were more severe in the CI group. Jung et al used a Korean version of the Mini-Mental State Examination to evaluate patients’ cognitive function and the Korean version of the Beck Depression Inventory to screen for depression. They reported a negative correlation between cognitive function and the prevalence of depressive symptoms and found depression and education level to be independent predictors of CI in multivariate analysis.20 Zhang et al also considered depression a risk factor for CI.21 It was inferred that depression and anxiety might aggravate CI in patients on MHD, and more attention should be paid to psychological problems.
No statistically significant difference was found regarding gender, age distribution, duration of dialysis, or the primary underlying cause of ESRD (diabetic nephropathy, hypertensive nephropathy, nephrogenic disease, and others) between the two study groups. However, when the numbers and count data for patients with hypertension and diabetes were compared in the two groups separately, the proportion of patients with diabetes was higher in the CI group than in the NCF group, but not hypertension. None of these factors were considered to affect cognitive function in the logistic regression analysis.
The laboratory indicators between the groups were compared and revealed that the hemoglobin level was lower in the CI group than in the NCF group. The uric acid and PTH levels were higher in the CI group. In the logistic regression analysis, hemoglobin, uric acid, and PTH were considered to affect cognitive function: hemoglobin was considered a protective factor, and uric acid and PTH were considered the risk factors.
The main factor that affects blood viscosity is HCT. Kutlay et al found that there was no correlation between the Mini-Mental State Examination score and the HCT value in patients with MHD.22 However, a study using resting-state functional magnetic resonance imaging and modularity network analysis showed that the HCT level was significantly correlated with global cognitive functioning in patients with ESRD.23 Zheng et al reported that in young adults with ESRD, the higher the HCT, the lower the cerebral blood flow, suggesting that low HCT may affect cognitive function in patients with ESRD by changing the cerebral blood flow.24 In that study, HCT was positively correlated with cognitive impairment, suggesting that the greater the erythrocyte specific volume, the more likely cognitive impairment is to occur, which was consistent with the above literature. The reverse impacts of hemoglobin and HCT on CI were possibly due to the small sample size.
Patients with ESRD have insufficient erythropoietin secretion. Although most patients on MHD receive weekly injections of recombinant erythropoietin, anemia is still common, and a 13-year longitudinal study in Japan showed that normal elderly people with lower baseline levels of albumin and hemoglobin have a sharper decline in their cognitive scores.25 Trevisan et al reported that elderly individuals with the lowest hemoglobin concentrations at baseline had a significant risk of CI during 4.4 years of follow-up.26 Shaker et al found that mild-to-moderate CI was associated with anemia in patients on hemodialysis; improvement of the anemia resulted in improved blood flow in the middle cerebral artery, which is associated with improved CI.27 Lee et al investigated the association between nutritional status and risk of osteoporosis, sarcopenia, and CI in patients on hemodialysis and found that lower hemoglobin levels were associated with a higher risk of CI in these patients.28 The present study found that the hemoglobin level was lower in the CI group than in the NCF group. Hemoglobin was considered to be a protective factor in the logistic regression analysis. In patients on MHD, higher or near-normal hemoglobin levels are beneficial for cognitive functioning. Therefore, maintaining hemoglobin at a near-normal level is important for cognitive functioning in patients on MHD.
Hyperparathyroidism is very common in patients on MHD and is characterized by a high level of PTH, which is found widely in the human brain. The main role of PTH in vertebrates is to regulate the metabolism of calcium and phosphorus. Hagström et al found that high PTH levels were associated with vascular dementia in two community-based cohorts.29 However, in a close systematic review, Jiang et al analyzed all relevant studies and concluded that there is generally weak and inconsistent evidence to support an association between high PTH levels and CI.30 In the present study, PTH levels were significantly higher in the CI group than in the NCF group, and the logistic regression analysis showed that PTH was positively correlated with CI, suggesting that high PTH levels may be a risk factor for CI in patients on MHD.
Puy et al reported a single-center study that included 54 patients with CKD and found that CI was independently associated with a high uric acid level.31 Liu et al have published a study on mild CI and uric acid levels in the elderly in the Beijing area, which concluded that within the normal range, a higher serum uric acid level was positively correlated with cognitive functioning in the elderly in the Chinese community, but this correlation was unstable in participants with hyperuricemia.32 However, a systematic review and meta-analysis of serum uric acid levels and CI/dementia by Khan et al found no correlation between cognitive function scores and serum uric acid levels.33 Mazumder et al considered that hyperuricemia might be a risk factor for CI in patients with CKD.34
In this study, serum uric acid levels were higher in the CI group than in the NCF group, and the logistic regression analysis suggested that the uric acid level was positively correlated with CI, suggesting that high uric acid may be a risk factor for CI.
Uric acid is the end product of purine nucleotide metabolism and, according to the literature, a potential inhibitor of acetylcholinesterase. A decrease in acetylcholinesterase activity is considered to be an early marker of CI and Alzheimer’s disease35 and may affect cognitive functioning.
This study has some limitations. First, this was the first part of a series of studies. The second part investigates the impact of cerebral small vessel disease on cognitive functioning in patients on MHD. The third part focuses on the impact of white matter lesions on cognition in these patients. Subgroup analysis of patients with different levels of CI will be performed in our upcoming studies. Secondly, this study did not include a control group. However, we compared two groups as a prerequisite for the second part of the study. Thirdly, the volume changes during dialysis therapy were not available for all patients. Lastly, this was a single-center study, further studies with a multi-center design will be needed.
Conclusion
In conclusion, a high prevalence of CI in patients on MHD was found, including significant impairment of attention and executive ability. Hemoglobin may protect cognitive functioning in these patients, while diabetes, PTH, and uric acid level may be the risk factors. Depressive and anxiety states may aggravate CI in patients on MHD.
Abbreviations
MHD, maintenance hemodialysis; ESRD, end-stage renal disease; DS, Digital Span; CTT, Color Trail Test; NCF, normal cognitive function; CI, cognitively impaired; PD, peritoneal dialysis; WBC, white blood cell; RBC, red blood cell; PLT, platelet; HCT, hematocrit; PDW, platelet distribution width; PTH, parathyroid hormone; MoCA, Montreal Cognitive Scale.
Data Sharing Statement
The original date of the research are included in the article, further inquiries can be provided. The datasets used and/or analysed during the current study available from the corresponding author, Xin Li, on reasonable request.
Ethics Approval and Consent to Participate
This study was conducted with approval from the Ethics Committee of Second Hospital of Tianjin Medical University ([2019](003)). This study was conducted in accordance with the declaration of Helsinki. Written informed consent was obtained from all participants.
Acknowledgments
We thank Dr. Pinghua Meng from the Hemodialysis Center for helping us communicate with patients, We thank all the patients involved in this study for their cooperation and support.
Funding
This work study supported by the National Key Research and Development Program of China (2016YFC1300600).
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Owolabi LF, Abdu A, Ibrahim A, et al. Cognitive function assessment in patients with end- stage renal disease in Nigeria: a single center experience. Ann Afr Med. 2016;15:138–144.
2. Tian X, Guo X, Xia X, Yu H, Li X, Jiang A. The comparison of cognitive function and risk of dementia in CKD patients under peritoneal dialysis and hemodialysis: a prisma-compliant systematic review and meta-analysis. Medicine. 2019;98:e14390.
3. Sorensen EP, Sarnak MJ, Tighiouart H, et al. The kidney disease quality of life cognitive function subscale and cognitive performance in maintenance hemodialysis patients. Am j Kidney Dis. 2012;60:417–426.
4. O’Lone E, Connors M, Masson P, et al. Cognition in people with end-stage kidney disease treated with hemodialysis: a systematic review and meta-analysis. Am j Kidney Dis. 2016;67:925–935.
5. Drew DA, Weiner DE, Sarnak MJ. Cognitive impairment in CKD: pathophysiology, management, and prevention. Am j Kidney Dis. 2019;74:782–790.
6. Kovarova L, Valerianova A, Kmentova T, Lachmanova J, Hladinova Z, Malik J. Low cerebral oxygenation is associated with cognitive impairment in chronic hemodialysis patients. Nephron. 2018;139:113–119.
7. Dlugaj M, Winkler A, Weimar C, et al. Anemia and mild cognitive impairment in the German general population. J Alzheimer’s Dis. 2016;49:1031–1042.
8. Bahrami A, Khorasanchi Z, Tayefi M, et al. Anemia is associated with cognitive impairment in adolescent girls: a cross-sectional survey. Applied neuropsychology. Child. 2020;9:165–171.
9. Tanaka M, Komaba H, Fukagawa M. Emerging association between parathyroid hormone and anemia in hemodialysis patients. Therap Apheresis Dialysis. 2018;22:242–245.
10. Rubin R. Exploring the relationship between depression and dementia. JAMA. 2018;320:961–962.
11. Seliger SL, Gillen DL, Longstreth WT, Kestenbaum B, Stehman-Breen CO. Elevated risk of stroke among patients with end-stage renal disease. Kidney Int. 2003;64(2):603–609. doi:10.1046/j.1523-1755.2003.00101.x
12. Harhay MN, Xie D, Zhang X, et al. Cognitive impairment in non-dialysis-dependent CKD and the transition to dialysis: findings from the chronic renal insufficiency cohort (cric)study. Am j Kidney Dis. 2018;72:499–508.
13. Angermann S, Baumann M, Steubl D, et al. Cognitive impairment in hemodialysis patients: implementation of cut-off values for the Montreal cognitive assessment (moca)-test for feasible screening. PLoS One. 2017;12:e0184589.
14. Gesualdo GD, Duarte JG, Zazzetta MS, et al. Cognitive impairment of patients with chronic renal disease on hemodialysis and its relationship with sociodemographic and clinical characteristics. Dementia Neuropsychol. 2017;11:221–226.
15. Angermann S, Baumann M, Wassertheurer S, et al. Pulse wave velocity is associated with cognitive impairment in hemodialysis patients. Clin Sci. 2017;131:1483–1493.
16. Sánchez-Fernández MDM, Reyes del paso GA, Gil-Cunquero JM, Fernández-Serrano MJ. Executive function in end-stage renal disease: acute effects of hemodialysis and associations with clinical factors. PLoS One. 2018;13:e0203424.
17. Salehinejad MA, Ghanavati E, Rashid MHA, Nitsche MA. Hot and cold executive functions in the brain: a prefrontal-Cingular network. Brain Neurosci Adv. 2021;5:23982128211007769.
18. King-Wing Ma T, Kam-Tao Li P. Depression in dialysis patients. Nephrology. 2016;21:639–646.
19. Farrokhi F, Abedi N, Beyene J, Kurdyak P, Jassal SV. Association between depression and mortality in patients receiving long-term dialysis: a systematic review and meta-analysis. Am j Kidney Dis. 2014;63:623–635.
20. Jung S, Lee YK, Choi SR, Hwang SH, Noh JW. Relationship between cognitive impairment and depression in dialysis patients. Yonsei Med J. 2013;54:1447–1453.
21. Zhang YH, Yang ZK, Wang JW, et al. Cognitive changes in peritoneal dialysis patients: a multicenter prospective cohort study. Am j Kidney Dis. 2018;72:691–700.
22. Murayama H, Shinkai S, Nishi M, et al. Albumin, hemoglobin, and the trajectory of cognitive function in community-dwelling older Japanese: a 13-year longitudinal study. J Prevent Alzheimer’s Dis. 2017;4:93–99.
23. Kutlay S, Nergizoglu G, Duman N, et al. Recognition of neurocognitive dysfunction in chronic hemodialysis patients. Ren Fail. 2001;23:781–787.
24. Mu J, Chen T, Liu Q, et al. Abnormal interaction between cognitive control network and affective network in patients with end-stage renal disease. Brain Imaging Behav. 2018;12:1099–1111.
25. Zheng G, Wen J, Lu H, et al. Elevated global cerebral blood flow, oxygen extraction fraction and unchanged metabolic rate of oxygen in young adults with end-stage renal disease: an MRI study. Eur Radiol. 2016;26:1732–1741.
26. Trevisan C, Veronese N, Bolzetta F, et al. Low hemoglobin levels and the onset of cognitive impairment in older people: the pro.V.A. Study. Rejuvenation Res. 2016;19:447–455.
27. Shaker AM, Mohamed OM, Mohamed MF, El-Khashaba SO. Impact of correction of anemia in end-stage renal disease patients on cerebral circulation and cognitive functions. Saudi j Kidney Dis Transplant. 2018;29:1333–1341.
28. Lee H, Kim K, Ahn J, Lee DR, Lee JH, Hwang SD. Association of nutritional status with osteoporosis, sarcopenia, and cognitive impairment in patients on hemodialysis. Asia Pac J Clin Nutr. 2020;29:712–723.
29. Hagström E, Kilander L, Nylander R, et al. Plasma parathyroid hormone is associated with vascular dementia and cerebral hyperintensities in two community-based cohorts. J Clin Endocrinol Metab. 2014;99:4181–4189.
30. Jiang W, Hu CY, Li FL, Hua XG, Huang K, Zhang XJ. Elevated parathyroid hormone levels and cognitive function: a systematic review. Arch Gerontol Geriatr. 202087:103985.
31. Puy L, Bugnicourt JM, Liabeuf S, et al. Cognitive impairments and dysexecutive behavioral disorders in chronic kidney disease. J Neuropsychiatry Clin Neurosci. 2018;30:310–317.
32. Liu M, Wang J, Zeng J, He Y. Relationship between serum uric acid level and mild cognitive impairment in Chinese community elderly. BMC Neurol. 2017;17:146.
33. Khan AA, Quinn TJ, Hewitt J, Fan Y, Dawson J. Serum uric acid level and association with cognitive impairment and dementia: systematic review and meta-analysis. Age. 2016;38:16.
34. Mazumder MK, Phukan BC, Bhattacharjee A, Borah A. Disturbed purine nucleotide metabolism in chronic kidney disease is a risk factor for cognitive impairment. Med Hypotheses. 2018;111:36–39.
35. Bohnen NI, Kaufer DI, Hendrickson R, et al. Cognitive correlates of alterations in acetylcholinesterase in Alzheimer’s disease. Neurosci Lett. 2005;380:127–132.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
