Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
Co-Design as Enabling Factor for Patient-Centred Healthcare: A Bibliometric Literature Review
Authors Silvola S , Restelli U , Bonfanti M, Croce D
Received 31 December 2022
Accepted for publication 21 April 2023
Published 17 May 2023 Volume 2023:15 Pages 333—347
DOI https://doi.org/10.2147/CEOR.S403243
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Sofia Silvola,1,2 Umberto Restelli,1,3 Marzia Bonfanti,1 Davide Croce1
1LIUC - Università Cattaneo, Castellanza, VA, Italy; 2Department of Public Health Medicine, School of Health System & Public Health, Faculty of Health Sciences, University of Pretoria, Pretoria, South Africa; 3School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Correspondence: Sofia Silvola, Tel +39 0331 572 509, Email [email protected]
Abstract: Service design and in particular co-design are approaches able to align with the need of healthcare contexts of value-based and patient-centered processing through a participatory design of services. The purpose of this study is to identify the characteristics of co-design and its applicability to the reengineering of healthcare services, as well as to detect the peculiarities of the application of this approach in different geographical contexts. The methodology applied for the review, Systematic Literature Network Analysis (SLNA), combines qualitative and quantitative perspectives. In detail, the analysis applied the paper citation networks and the co-word network analysis to detect the main research trends over time and to identify the most relevant publications. The results of the analysis highlight the backbone of literature on the application of co-design in healthcare as well as the advantages and the critical factors of the approach. Three main literature streams emerged concerning the integration of the approach at meso and micro level, the implementation of co-design at mega and macro level, and the impacts on non-clinical related outcomes. Moreover, the findings underline differences in co-design in terms of impacts and success factors in developed countries and economies in transition or developing countries. The analysis shows the potentially added value of the application of a participatory approach to the design and redesign of healthcare services both at different levels of the healthcare organization and in the contexts of developed countries and economies in transition or developing countries. The evidence also highlights potentialities and critical success factors of the application of co-design in healthcare services redesign.
Keywords: co-creation, co-production, systematic literature network analysis, healthcare services
Introduction
The healthcare context is characterized by continuous innovations and changes in treatments and diagnostics, while care processes undergo only small changes.1 To ensure quality and efficiency in healthcare, however, it is not enough to introduce innovations, but it is necessary to analyse and revise the entire service, which includes healthcare but also non-healthcare activities. This consideration should be discussed within increasingly complex healthcare systems. These are characterized by the presence of a growing multitude of actors and a gradual transition towards an integrated organizational/managerial approach capable of facing complexities and multi-morbidities.2
Given the shifting of the healthcare paradigm to a patient-centred and value-based medicine, a holistic approach to the review of healthcare services is essential. The core idea related to value-based healthcare is that organization and management of care should be driven by value generation for the patients.3–5 This renewed approach includes the patient’s perspective and experience in service redesign, moving from a passive role of the users to a participative one.6–8 Service design fits into this context as a multidisciplinary approach capable of capturing the needs of stakeholders and including them in the design of multi-component services.1 From a value-based healthcare perspective, this approach finds a perfect matching as it is capable of organizing services by working on optimization. Service design is not just about creating new services, but it is also used to reorganize existing ones. In this context, participatory design, also known as co-design, co-production, or co-creation, is a methodological approach that is applied to the development of health services through the empowerment of the various subjects involved in the pathways of interest. The application of this approach has potential advantages in quality and social terms.9,10 Co-design also consists in the substantial involvement of experienced or potential users in the redesign processes. This approach moves from the traditional involvement of the user and caregivers in the customer satisfaction phase only, understood as the activity of completing a questionnaire to signal satisfaction with the service received and limited to the reporting of subjective perceptions, towards an approach of total involvement in the processes of innovation and revision of healthcare services from a user-oriented perspective.11,12
The term co-production was first introduced in the United States between 1970s and 1980s to denote an approach that involved citizens in the production of public services. This approach then spread also in European context and it reached the healthcare context. In fact, the health policies in the 1980s and 1990s were more focused on the themes of efficiency and performance. Only at the end of the 1990s a cultural revolution started related to the redesign of healthcare services through a perspective based on patient’s needs and values, thus involving not only policymakers and professionals but also staff, users, families, and the community.13,14
Although scholars outline the potentialities of co-design for the revision of healthcare services, few studies focus on implementation facilitators and applicability of co-design in different contexts.1,9,10,15
However, there is a lack of direct comparisons between these elements in developed countries and economies in transition or developing countries.
Starting from these premises, the authors consider of interest to identify the characteristics of this approach and its applicability in the healthcare context.
In detail, the objective of this work is to identify how co-design can support the reengineering of healthcare services through a patient-centred approach.
Specifically, the research questions addressed are the following:
- What are facilitators and potential outcomes of co-design implementation in healthcare?
- What are the differences in the application of co-design in healthcare in developed countries and economies in transition or developing countries?
Materials and Methods
The methodology used for this analysis is the quantitative-based method Systematic Literature Network Analysis (SLNA).16
The method relies on objective measures and algorithms, and it combines a systematic literature review and bibliographic network analysis. SLNA method contains the analysis of bibliometric networks based on the papers retrieved, such as citations and keywords analysis, as one of its components.17 SLNA is used to complement the traditional systematic literature review with the aim to retrieve the full amount of relevant material about the topic. This review aims to identify the main research trends and key issue regarding the use of co-design in healthcare services. The research questions and the eligibility criteria used in the review were structured around a CIMO-logic (Context-Intervention-Mechanism-Outcome).18
In detail, the structure considered is the following:
Context: design of services in healthcare;
Intervention: services reengineering;
Mechanism: services reengineering using co-design;
Outcome: definition of the facilitators and potential outcomes concerning the application of co-design to the re-engineering of services in healthcare.
The search was carried out on August 22, 2022, using Scopus bibliographic database, that provides coverage around 60% larger than the one of Web of Science and incorporates the results of the biomedical literature database PubMed.19 To ensure literature saturation, no restrictions have been imposed on the type of document, areas of interest, period of publication, language, or country and no keywords were excluded from the research.
The keywords used to compose the search query are “co-design*” “co-product*” and “co-creat*”. Additionally, the keyword “health*” was added to limit the search to the field of interest. The search string was composed intentionally wide, with the aim of not excluding a priori articles of potential interest. The selected keywords are the most frequent in articles and reviews already published, as well as the most comprehensive and not misleading, to avoid losing information or going out of scope.
The search was carried out with the following search string:
(TITLE(((co-design*) OR (codesign*) OR (co AND design*) OR (co-produc*) OR (coproduc*) OR (co AND produc*) OR (co-creat*) OR (cocreat*) OR (co AND creat*)) AND (health*)))
In case of lack of information referred to the objectives of the research in the articles retrieved, the reference lists of the articles included in main path and the complete list of documents retrieved from Scopus were scanned to include additional articles of interest.
Referring to the secondary question, the distinction between developed countries and economies in transition or developing countries refers to the most recent definition published by the United Nations.20
For the literature review, the Citation Network Analysis (CNA) was used. CNA is a method based on citations, which are the connections between papers (nodes) in the citation network.19,21 Two software packages were used: Vos Viewer and Pajek. Vos Viewer (http://www.vosviewer.com/) is a software tool for creating bibliometric networks. Vos Viewer was adopted for the preliminary analysis, in terms of network visualization and for generating the input file for Pajek. Pajek (http://vlado.fmf.uni-lj.si/pub/networks/pajek/) is a software tool for network analyses and, in this work, it was used for implementing the results of the citation network. The search strategy followed the PRISMA guidelines.22 The main steps of the analysis are the quantification of citation traversal weights and the extraction of the main path component using the default cut-off of 0.5.17 Citation traversal weights are represented by the significance of a particular citation in linking articles in the network, as the ratio between the number of paths including the citation and the total number of paths between articles that do not cite any others and articles that are not cited by any others.
Considering the many sub-areas of the field of study, it is appropriate to optimize modularity and group papers into communities. For the analysis of keywords, the co-occurrence (co-word) network was used. Co-occurrence network contains authors' keywords and the number of times they occur together in the same group of papers at least thirteen times. The Vos Viewer software was used for the analysis implementing the VOS (Visualisation of Similarities) technique.23 The technique consists in the determination of locations of items in a map and the minimization of a function depending on a similarity measure (ASij) between items.
Where: cij = measure of the co‐occurrence of keywords i and j in the same document and c = expected number of co‐occurrences of i and j (under the assumption that the co‐occurrences of i and j are statistically independent).17
With the aim of identifying the central topics in the different time periods, Kleinberg’s Burst detection algorithm was applied to identify the temporal trends in the use of the different keywords.24,25 The burst detection analysis was implemented using Sci2 (https://sci2.cns.iu.edu/user/index.php) which is a software for temporal, geospatial, topical, and network analysis and visualization of scholarly datasets. The process begins with identifying the keywords used by the authors, which are normalized (transformed into symbolic words) and displayed on a timeline in terms of importance represented by the burst weight. Gimp software (https://www.gimp.org/) was used to graphically represent the burst analysis. The gamma value (number of burst) applied in the analysis is 0.65 as this value allowed to include an acceptable number of keywords equal to 24.26
The statistics concerning the papers retrieved have been described with the aim of reporting a clear picture of the literature.
In order to identify additional papers of interest, which may impact on the search stream of analysis, the number of citations of publications retrieved from the review has been ranked. The Global Citation Score (GCS) analysis consists in the identification of the total number of citations for every paper included in the review and it was implemented considering the first most cited 15 publications, to detect seminal or recent breakthrough studies.
Narrative synthesis was performed summarizing the evidence extracted from SLNA. Data extraction was performed by one researcher and independently checked by a second researcher. The reviewers resolved any discrepancy or disagreement through discussion. A data extraction grid of open questions was developed considering first author, year of publication, topic, country, study type, setting, co-design definition, advantages of co-design, critical factors of co-design, and keywords, as reported in Supplementary Table 1.
Results
Paper Citation Networks (Connected Components, Main Path)
Concerning the citation network, the search strategy is represented in Figure 1, while the citation network is represented in Figure 2. The analysis included 889 documents, of which 671 had received at least one citation. Moreover, the largest connected component of the network is composed of 335 nodes, while the “main path” is composed by 16 documents, as represented in Figure 3. The main path was used to detect the main trends in the development of research line’s contents, by shedding lights on the papers, which take on the role of hubs to the next ones (ie,27–43). In the main path, the arrows go from cited to citing papers, representing the flow of knowledge that was obtained by quantifying the transversal weight of the citations (Search Path Count method) and extracting the main path components.16,17,43
 |
Figure 1 Flow chart of the search strategy. |
 |
Figure 2 Citation Network. |
 |
Figure 3 Main path. |
Co-Word Network Analysis (Keywords Analysis: VOS Clustering)
Concerning the keywords co-occurrence network represented in Figure 4, of the 2198 total keywords, 22 occur at least thirteen times. No keywords were excluded from the analysis. From the 22 keywords, five clusters/communities are detected, as reported in Table 1, and they represent the main research trajectories identified.
 |
Table 1 Clusters Identified. |
 |
Figure 4 Keywords network. |
Burst Detection Analysis
The burst detection analysis allowed us to identify when keywords became important over time and their magnitude, as shown in Figure 5.
 |
Figure 5 Kleinberg’s Burst detection analysis output. |
The main research interests from 2001 to 2016 focused on healthcare management, moreover in 2010 references to organizational impact emerged. In 2013, a trend concerning the value of healthcare services manifests. In more recent years, starting from 2018, wide and parallel research lines introduce the issues of e-health and patient engagement in the development of public services, especially in the field of chronic diseases.
Global Analysis (Basic and Advanced Statistics)
Concerning the 889 papers retrieved from Scopus, the first publication refers to the year 1982. The number of publications concerning this field of research has an increasing trend during the years with a peak in 2021, which count for the 23% of the total number of publications, as reported in Figure 6. The publications from the last 5 years (2018–2022) account for the 71% of the total number of publications and this highlights the novelty of the subject.
 |
Figure 6 Documents by year. |
In terms of geographical distribution, the majority of papers are referred to European Union contexts (29%) and to United Kingdom context (22%), followed by papers referred to the Australian context (13%) and to the United States context (12%), while a minority of analysis are related to Asian, Latin American, or African contexts.
Concerning the types of publications, the majority are articles (71%), followed by other types, such as conference papers (10%), reviews (9%), book chapters (4%), and others.
In terms of subject area, the majority of publications are referred to medicine (33%), followed by social sciences (16%), and other areas related to management and healthcare, as represented in Figure 7.
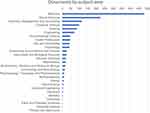 |
Figure 7 Documents by subject area. |
The analysis concerning the Global Citation Score (GCS) of the top 15 papers is reported in Table 2 and in Supplementary Table 2. Only five papers are included in the main path (ie27,31,34,35,37) and four studies were excluded from the analysis since, despite being related to the healthcare context and participatory production, they deal with issues relating to food contamination, wireless sensors, chemical, or drug production, and therefore are not consistent with the objective of the analysis (ie,44–47). To enrich the contribution, the remaining six most cited papers were added to the analysis (ie,48–53). In detail, the journals in which the additional articles are published are for the majority ranked from Scimago Journal & Country Rank in the first quartile, except one ranked in the second quartile, and the majority refers to the areas of medicine, social sciences, and management.54
 |
Table 2 Ranking the Top 15 Cited Papers of the Review. |
Concerning the comparison between developed countries and economies in transition or developing countries, all the studies included in the main path referred to developed countries. Therefore, the reference lists of the articles included in the main path and the complete list of documents retrieved was scanned to include additional articles referring to economies in transition or developing contexts. After the scanning phase, 23 additional documents were selected to be included in the analysis because they report insights of the application of the approach in economies in transition or developing countries (ie,55–77).
Narrative Synthesis
The analysis of the literature was conducted to highlight the backbone of the literature and to rationalize and systematize the scientific knowledge about the topic. The theoretical foundations of co-design in healthcare are based on three main literature streams, as reported in Table 3. The first two parallel streams contain two groups of papers. The first group of papers concerns the integration of this approach at meso and micro level (ie, hospitals, local health, professionals, patients, and caregivers). The second group is related to the implementation of co-design at mega and macro level (ie, government, media, authorities, and insurers) in the healthcare context. The former, although containing a small number of evidence, underlines the advantages and critical success factors for the implementation of a participatory approach to the design of health services. These studies are opinion papers and single or multiple case studies carried out in the European and United States contexts (ie,27–29,36,41). Studies investigating the mega and macro levels reflect the characteristics and results of a collaborative approach within the policy level. These studies are opinion papers, single or multiple case studies, and interpretative analyses carried out in the European, United States, and Australian contexts (ie,29,31–35,37,38). In recent times, not only the impacts on clinical outcomes but also the impacts on non-clinical related outcomes have been highlighted. The most recent research streams have combined the co-design approach’s ability to revise services with its evaluation capability. These studies are reviews, opinion papers, Delphi studies, and case studies carried out in the European, United States, Canadian, and Asian contexts (ie,29,30,39,40,42).
 |
Table 3 Summary of the Results. |
From the first group of articles, it emerges that co-design is a useful tool for integrating generic and specific resources in order to optimize individual problems. In this context, the advantages that emerge from the implementation of the approach relate to an improvement in performance in terms of efficiency, quality of care and clinical outcomes, as well as a positive impact in terms of costs. Those are reached through a better understanding of health states and of evidence-based and personalized approaches. Therefore, the reported critical factors are the patient engagement and the activation of positive relationships between users, caregivers, and professionals. Furthermore, the need to carry out assessments on health professional skills, and professionals and patients knowledges, as well as on relationships, organizational forms, and organizational structures of the delivery system is reported, to facilitate the coproductive partnership between healthcare professionals and patients.27–29,36,41
From the second group of articles, it is highlighted that co-production or co-creation is able to integrate both public and private multiparty resources to improve the quality of services, expanding wealth-welfare-wellbeing. The study shows advantages related to the application of the approach in terms of ability to create patient-centred experiences capable of positively impacting the quality of services, satisfaction, and perceived value by users. Furthermore, the positive impact in terms of holistic understanding, as well as creativity and generated ideas is evident (eg, changes to processes, practices, and clinical environments with impacts on patients and caregivers experience or staff activities; new products or services development; innovative idea for improving existing healthcare services).29,38 Moreover, the positive impact in terms of costs of the innovation process as reduced cost for innovation thanks to the partial substitution of paid personnel with volunteers, emerged.27,32,38 Additionally, the benefits in terms of time to market, understood as the length of time from a product or service conception until its commercialization or delivery, are highlighted.38 The building blocks in this case consist of the knowledge of managerial, governance, and leadership perspectives, the management of resources and relationships between stakeholders, as well as the understanding of possible complexities and vulnerabilities, such as political influences.29,31–35,37,38
From the third group, it is underlined that participatory models represent the new zeitgeist (spirit of our time) and concerns related to the improvement of services through the involvement of different stakeholders, as well as their evaluation. Literature shows the positive impact of this approach on public value and accessibility, as well as on the quality and efficiency of the processes. The factors for obtaining results are the explication of organizational and relational mechanisms, the identification of personal skills and knowledges, the integration of qualitative and quantitative approaches, as well as the balance between the effective application of the method, and legal and budget requirements.29,30,39,40,42
Concerning the most cited papers, as confirmed by the previous literature, they highlight the impacts of the participatory approach for design and redesign of services in terms of perceived quality and satisfaction of users and professionals.48–53 The literature underlines the importance of an active involvement of the user as the only subject capable of fully understanding the pathways, as well as the emphasis on managing the integration process of services in specific contexts.
The keywords analysis identified five clusters and although the topics of the clusters overlap (eg, cluster 2, cluster 3, and cluster 4) clear and distinct thematic emerge from each of them. The first cluster focuses on the topic of the integration of technological tools as a support to participatory design through online communities. It emphasizes the importance of offline interactions as a basis for communication.35,37,38,42 The second cluster shows the emerging issue related to evaluation alongside those of services design.31,33,36,37,42 The third cluster focuses on qualitative studies in the field of participatory design, while the fourth includes studies with a mixed methodology.31,33,36,37,42 The fifth cluster, on the other hand, focuses on the mental healthcare area because the topic of participatory design has shown positive impacts in improving quality in this context.39,40,42
Concerning burst detection, the analysis confirmed and supported what emerged from co-word network analysis and keywords analysis, explaining how the trend of interests in literature over the years shifted from the use of co-design for improving healthcare services at micro and macro levels, to being exploited as a services evaluation method.
The literature presents the evolution of trends in the use of the co-design approach: from an application related to the involvement of users and professional in the improvement of the quality of services, the implementation moves on to a broader objective of evaluation and redesign of healthcare services at different levels.
Despite the reduced number of articles referred to the application of co-design in economies in transition or developing countries, being more widespread in contexts with a larger welfare state, some differences emerge from the literature, as reported in Table 4.55–77 The positive impacts and success factors reported for developed countries and economies in transition were retrieved from the articles and all the concepts cited by more than one article were collected and aggregated. The articles are related to the three main geographical contexts of Africa, Asia, and Latin America (ie, Bangladesh, Botswana, China, Ghana, India, Indonesia, Mozambique, Nepal, Nigeria, Peru, Rwanda, Saudi Arabia, South Africa, sub-Saharan Africa, Taiwan, and Tanzania). The benefits of this approach are evident in terms of efficiency and effectiveness considering dimensions like accessibility, responsiveness, customer satisfaction, clinical outcomes, and use of inputs or resources.61,71 The main characteristics of engagement of citizens and users are highlighted, while the critical success factors deserve attention. In these contexts, co-design is the evolution of self-organized communities where the presence of several subjects already coexists but in an unorganized way. Furthermore, the application of these approaches is often supported by external donors, and therefore it is not self-generated and may lack coordination and management.61 Moreover, participative initiatives in economies in transition or developing countries often see the involvement of international institutions. Finally, it is important to combine evaluation and implementation with a planning phase to optimize integration, as well as an incentive system that encourages the generation of inputs.71 However, the benefits of the implementation of participatory approaches can be many, especially in terms of better levels of welfare, democracy, equity, and capabilities building.55–77
 |
Table 4 Co-Design in Developed Countries and Economies in Transition or Developing Countries. |
Finally, the literature underlines some gaps, first of all only few studies are detected related to the development and validation of co-creation scales. Moreover, there is a lack of translational research, which demonstrates the real applicability of these approaches, as well as evaluation studies especially in terms of economic evaluations.29,37,42
Discussion and Conclusions
The analyzed body of literature highlights two main active research streams: a first strand, more rooted and mature, which explains the characteristics of the application of participatory design in the healthcare context at different organizational levels, as well as the critical success factors of the implementation of this approach. The second strand, still relatively less mature, relates to the application of the approach in the contexts of economies in transition or developing countries. The analysis shows a potential added value of the application of a participatory approach to the design and redesign of healthcare services both at different levels of the healthcare organization and in the contexts of developed countries and economies in transition. In this sense, as emerged from the literature, there are many critical success factors in the application of this approach. These include the need to define the characteristics of individual contexts and relationship management.
SLNA methodology has some limitations, first of all the citations alone may not be completely informative, the chosen keywords were limited to the research within the titles, and finally a topic often discussed is the “Matthew effect.” According to this effect, researchers often tend to cite articles written by well-known researchers to the detriment of others, equally or more interesting.
Some considerations emerged from the analysis performed. Healthcare system is a complex system composed of a multitude of stakeholders.2 Epidemiological transition of population, increasingly affected by multimorbidity, is causing a gradual transition towards an integrated and patient-centered approach. Accordingly, the concept of “value” in healthcare emerged as a milestone of healthcare organizations.6,8
Based on the literature review performed, the results support and enlarge the findings of other authors (ie,9,10). supporting the findings concerning the potentialities of implementing co-design in service redesign in healthcare in terms of user satisfaction. Furthermore, this work adds to the literature not only details regarding the positive impacts of co-design on process redesign but also insights regarding critical success factors in different contexts such as developed countries and economies in transition or developing countries. This review shows that a significant number of publications consider that co-design has proved to be a useful approach to be applied during design and redesign processes of healthcare services to improve their quality and perceived value. Given the growing need for healthcare facilities to align with value-based and patient centered perspective, co-design can be a support for the evaluation and reengineering of healthcare services though the user’s involvement. Indeed, in order to bring tangible benefits, service design should be the focus of organizations. Users’ involvement is essential to have a clear understanding of the real needs and desires of patients and therefore to provide customized products and services capable of reducing costs and risks, while improving organization’s performances. However, in order to create an efficient co-design process, it is necessary to provide users with adequate tools, to allow them to express their opinions and to collaborate. These tools should take into account the needs of the healthcare environment, characterized by scarce resources both in human and material terms, and also align with the changed needs of the community in terms of technological instruments to support direct and asynchronous communication. Moreover, the advantages of this approach increase in the case of economies in transition or developing countries as the expected benefits are also related to social and welfare issues. The challenge for the future is to investigate in depth the costs and benefits of co-design, to understand how to best incorporate it for the assessment and review of healthcare services and to define how to address and manage this participative approach.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vaz N, Venkatesh R. Service design in the healthcare space with a special focus on non-clinical service departments: a synthesis and future directions. Health Serv Manage Res. 2022;35(2):83–91. doi:10.1177/09514848211010250
2. Lipsitz LA. Understanding health care as a complex system: the foundation for unintended consequences. JAMA. 2012;308(3):243–244. doi:10.1001/jama.2012.7551
3. Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477–2481. doi:10.1056/NEJMp1011024
4. Porter ME, Teisberg EO. Redefining Health Care: Creating Value Based Competition on Results. Harvard Business School Press; 2006.
5. Teisberg E, Wallace S, O’Hara S. Defining and implementing value-based health care: a strategic framework. Acad Med. 2020;95(5):682–685. doi:10.1097/ACM.0000000000003122
6. Sharma AE, Knox M, Mleczko VL, Olayiwola JN. The impact of patient advisors on healthcare outcomes: a systematic review. BMC Health Serv Res. 2017;17(1):693. doi:10.1186/s12913-017-2630-4
7. Bombard Y, Baker GR, Orlando E, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1):98. doi:10.1186/s13012-018-0784-z
8. Lowe D, Ryan R, Schonfeld L, et al. Effects of consumers and health providers working in partnership on health services planning, delivery and evaluation. Cochrane Database Syst Rev. 2021;9(9):CD013373. doi:10.1002/14651858.CD013373.pub2
9. Green T, Bonner A, Teleni L, et al. Use and reporting of experience-based codesign studies in the healthcare setting: a systematic review. BMJ Qual Saf. 2020;29(1):64–76. doi:10.1136/bmjqs-2019-009570
10. Thomas G, Lynch M, Spencer LH. A systematic review to examine the evidence in developing social prescribing interventions that apply a co-productive, co-designed approach to improve well-being outcomes in a community setting. Int J Environ Res Public Health. 2021;18(8):3896. doi:10.3390/ijerph18083896
11. Ouschan R, Sweeney JC, Johnson LW. Dimensions of patient empowerment: implications for professional services marketing. Health Mark Q. 2000;18(1–2):99–114. doi:10.1300/J026v18n01_08
12. Vargo SL, Lusch RF. Why ‘service’. J Acad Mark Sci. 2008;36(1):25–38. doi:10.1007/s11747-007-0068-7
13. Alford J. Why do public-sector clients coproduce?: Toward a contingency theory. Adm Soc. 2002;34(1):32–56. doi:10.1177/0095399702034001004
14. Pestoff V. Citizens and co-production of welfare services childcare in eight European Countries. Public Manag Rev. 2006;8(4):508–519. doi:10.1080/14719030601022882
15. Masterson D, Areskoug Josefsson K, Robert G, Nylander E, Kjellström S. Mapping definitions of co-production and co-design in health and social care: a systematic scoping review providing lessons for the future. Health Expect. 2022;25(3):902–913. doi:10.1111/hex.13470
16. Colicchia C, Strozzi F. Supply chain risk management: a new methodology for a systematic literature review. Supply Chain Manag. 2012;17(4):403–418. doi:10.1108/13598541211246558
17. Strozzi F, Colicchia C, Creazza A, Noè C. Literature review on the ‘Smart Factory’ concept using bibliometric tools. Int J Prod Res. 2017;55(22):6572–6591. doi:10.1080/00207543.2017.1326643
18. Denyer D, Tranfield D. Producing a Systematic Review. In: The Sage Handbook of Organizational Research Methods. Buchanan D, Bryman A, edited by. London: Sage Publications; 2009:671–689.
19. Zhao D, Strotmann A. Analysis and visualization of citation networks. Synthesis lectures on information concepts. Retriev Serv. 2015;7(1):1–207.
20. United Nations. World economic situation and prospects; 2022.
21. Ding Y, Chowdhury GG, Foo S. Bibliometric cartography of information retrieval research by using co-work analysis. Inf Process Manag. 2001;37(6):817–842. doi:10.1016/S0306-4573(00)00051-0
22. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;21(339):b2535. doi:10.1136/bmj.b2535
23. Van Eck NJ, Waltman L. Software survey: vOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi:10.1007/s11192-009-0146-3
24. Kleinberg J. Bursty and hierarchical structure in streams. Data Min Knowl Discov. 2003;7(4):373–397. doi:10.1023/A:1024940629314
25. Pollack J, Adler D. Emergent trends and passing fads in project management research: a scientometric analysis of changes in the field. Int J Proj Manag. 2015;33(1):236–248. doi:10.1016/j.ijproman.2014.04.011
26. Colicchia C, Creazza A, Strozzi F. Citation network analysis for supporting continuous improvement in higher education. Stud High Educ. 2018;43(9):1637–1653. doi:10.1080/03075079.2016.1276550
27. Batalden M, Batalden P, Margolis P, et al. Coproduction of healthcare service. BMJ Qual Saf. 2016;25(7):509–517. doi:10.1136/bmjqs-2015-004315
28. Boye N. Co-production of Health enabled by next generation personal health systems. Stud Health Technol Inform. 2012;177:52–58.
29. Clarke D, Jones F, Harris R, Robert G. Collaborative rehabilitation environments in acute stroke (CREATE) team. What outcomes are associated with developing and implementing co-produced interventions in acute healthcare settings? A rapid evidence synthesis. BMJ Open. 2017;7(7):e014650. doi:10.1136/bmjopen-2016-014650
30. Cox R, Kendall M, Molineux M, Miller E, Tanner B. Refining a capability development framework for building successful consumer and staff partnerships in healthcare quality improvement: a coproduced eDelphi study. Health Expect. 2022;25(4):1563–1579. doi:10.1111/hex.13499
31. Elg M, Engström J, Witell L, Poksinska B. Co‐creation and learning in health‐care service development. J Serv Manag. 2012;23(3):328–343. doi:10.1108/09564231211248435
32. Fotaki M. Towards developing new partnerships in public services: users as consumers, citizens and/or co-producers in health and social care in England and Sweden. Public Adm. 2011;89(3):933–955. doi:10.1111/j.1467-9299.2010.01879.x
33. Gill L, White L, Cameron ID. Service co‐creation in community‐based aged healthcare. Manag Serv Qual. 2011;21(2):152–177. doi:10.1108/09604521111113447
34. Greenhalgh T, Jackson C, Shaw S, Janamian T. Achieving research impact through co-creation in community-based health services: literature review and case study. Milbank Q. 2016;94(2):392–429. doi:10.1111/1468-0009.12197
35. Hardyman W, Daunt KL, Kitchener M. Value co-creation through patient engagement in health care: a micro-level approach and research agenda. Public Manag Rev. 2015;17(1):90–107. doi:10.1080/14719037.2014.881539
36. Hyde P, Davies HTO. Service design, culture and performance: collusion and co-production in health care. Hum Relat. 2004;57(11):1407–1426. doi:10.1177/0018726704049415
37. McColl-Kennedy JR, Vargo SL, Dagger TS, Sweeney JC, Kasteren Y. Health care customer value cocreation practice styles. J Serv Res. 2012;15(4):370–389. doi:10.1177/1094670512442806
38. Nambisan P, Nambisan S. Models of consumer value cocreation in health care. Health Care Manage Rev. 2009;34(4):344–354. doi:10.1097/HMR.0b013e3181abd528
39. O’Brien J, Fossey E, Palmer VJ. A scoping review of the use of co-design methods with culturally and linguistically diverse communities to improve or adapt mental health services. Health Soc Care Community. 2021;29:1–17. doi:10.1111/hsc.13105
40. Palmer VJ, Weavell W, Callander R, et al. The Participatory Zeitgeist: an explanatory theoretical model of change in an era of coproduction and codesign in healthcare improvement. Med Humanit. 2019;45(3):247–257. doi:10.1136/medhum-2017-011398
41. Sabadosa KA, Batalden PB. The interdependent roles of patients, families and professionals in cystic fibrosis: a system for the coproduction of healthcare and its improvement. BMJ Qual Saf. 2014;23(Suppl 1):i90–4. doi:10.1136/bmjqs-2013-002782
42. Tindall RM, Ferris M, Townsend M, Boschert G, Moylan S. A first-hand experience of co-design in mental health service design: opportunities, challenges, and lessons. Int J Ment Health Nurs. 2021;30(6):1693–1702. doi:10.1111/inm.12925
43. Lucio-Arias D, Leydesdorff L. Main-path analysis and path- dependent transitions in HistCiteTM-based historiograms. J Am Soc Inform Sci Tech. 2008;59(12):1948–1962. doi:10.1002/asi.20903
44. Hackmann G, Guo W, Yan G, Lu C, Dyke S. Cyber-Physical Codesign of Distributed Structural Health Monitoring with Wireless Sensor Networks. In:
45. Lee HJ, Ryu D. Worldwide occurrence of mycotoxins in cereals and cereal-derived food products: public health perspectives of their co-occurrence. J Agric Food Chem. 2017;65(33):7034–7051. doi:10.1021/acs.jafc.6b04847
46. Shahidi F, Abuzaytoun R. Chitin, chitosan, and co-products: chemistry, production, applications, and health effects. Adv Food Nutr Res. 2005;49:93–135.
47. Trebble T, Arden NK, Stroud MA, et al. Inhibition of tumour necrosis factor-alpha and interleukin 6 production by mononuclear cells following dietary fish-oil supplementation in healthy men and response to antioxidant co-supplementation. Br J Nutr. 2003;90(2):405–412. doi:10.1079/BJN2003892
48. Donetto S, Pierri P, Tsianakas V, Robert G. Experience-based co-design and healthcare improvement: realizing participatory design in the public sector. Design J. 2015;18(2):227–248. doi:10.2752/175630615X14212498964312
49. Dunston R, Lee A, Boud D, Brodie P, Chiarella M. Co-production and health system reform – from re-imagining to re-making. Aust J Public Adm. 2009;68(1):39–52. doi:10.1111/j.1467-8500.2008.00608.x
50. Frow P, McColl-Kennedy JR, Payne A. Co-creation practices: their role in shaping a health care ecosystem. Ind Mark Manag. 2016;56:24–39. doi:10.1016/j.indmarman.2016.03.007
51. Oliver K, Kothari A, Mays N. The dark side of coproduction: do the costs outweigh the benefits for health research? Health Res Policy Syst. 2019;17(1):33. doi:10.1186/s12961-019-0432-3
52. Robert G, Cornwell J, Locock L, Purushotham A, Sturmey G, Gager M. Patients and staff as codesigners of healthcare services. BMJ. 2015;10(350):g7714. doi:10.1136/bmj.g7714
53. Sweeney JC, Danaher TS, McColl-Kennedy JR. Customer effort in value cocreation activities: improving quality of life and behavioral intentions of health care customers. J Serv Res. 2015;18(3):318–335. doi:10.1177/1094670515572128
54. SJR. Scimago journal & country rank; 2022. Available from: https://www.scimagojr.com/.
55. Assegaai T, Schneider H, Scott V. Developing a district level supportive supervision framework for community health workers through co-production in South Africa. BMC Health Serv Res. 2021;21:337. doi:10.1186/s12913-021-06350-2
56. Agyepong IA, Godt S, Sombie I, Binka C, Okine V, Ingabire MG. Strengthening capacities and resource allocation for co-production of health research in low and middle income countries. BMJ. 2021;15(372):n166. doi:10.1136/bmj.n166
57. Alahmari N, Alswedani S, Alzahrani A, Katib I, Albeshri A, Mehmood R. Musawah: a data-driven ai approach and tool to co-create healthcare services with a case study on cancer disease in Saudi Arabia. Sustainability. 2022;14(6):3313. doi:10.3390/su14063313
58. Beran D, Lazo-Porras M, Cardenas MK, et al. Moving from formative research to co-creation of interventions: insights from a community health system project in Mozambique, Nepal and Peru. BMJ Glob Health. 2018;3(6):e001183. doi:10.1136/bmjgh-2018-001183
59. Boateng MA, Agyei-Baffour E, Angel S, Asare O, Prempeh B, Enemark U. Co-creation and prototyping of an intervention focusing on health literacy in management of malaria at community-level in Ghana. Res Involv Engagem. 2021;7(1):55. doi:10.1186/s40900-021-00302-0
60. Brooks H, Irmansyah I, Susanti H, et al. Evaluating the acceptability of a co-produced and co-delivered mental health public engagement festival: mental Health Matters, Jakarta, Indonesia. Res Involv Engagem. 2019;6(5):25. doi:10.1186/s40900-019-0161-3
61. Cepiku D, Giordano F. Co-Production in Developing Countries: insights from the community health workers experience. Public Manag Rev. 2014;16(3):317–340. doi:10.1080/14719037.2013.822535
62. Duara R, Chowdhury D, Dey R, Goswami S, Madill A. Using cocreated visually informed community mental health education in low- and middle-income countries: a case study of youth substance misuse in Assam, India. Health Expect. 2022;25(4):1930–1944. doi:10.1111/hex.13550
63. Dzinamarira T, Mulindabigwi A, Mashamba-Thompson TP. Co-creation of a health education program for improving the uptake of HIV self-testing among men in Rwanda: nominal group technique. Heliyon. 2020;6(10):e05378. doi:10.1016/j.heliyon.2020.e05378
64. Hugh-Jones S, Janardhana N, Al-Janabi H, et al. Safeguarding adolescent mental health in India (SAMA): study protocol for codesign and feasibility study of a school systems intervention targeting adolescent anxiety and depression in India. BMJ Open. 2022;12(4):e054897. doi:10.1136/bmjopen-2021-054897
65. Mangai MS, De Vries MS. You just have to ask coproduction of primary healthcare in Ghana and Nigeria. Public Organiz Rev. 2019;19:273–291. doi:10.1007/s11115-018-0420-z
66. Manikam L, Shah R, Reed K, Santini G, Lakhanpaul M. Using a co-production prioritization exercise involving South Asian children, young people and their families to identify health priorities requiring further research and public awareness. Health Expect. 2017;20(5):852–861. doi:10.1111/hex.12524
67. Mishu MP, Elsey H, Choudhury AR, et al. Co-producing an intervention for tobacco cessation and improvement of oral health among diabetic patients in Bangladesh. BMC Oral Health. 2021;21(1):516. doi:10.1186/s12903-021-01861-0
68. Mwoka M, Ajayi AI, Kibunja G, et al. Cocreated regional research agenda for evidence-informed policy and advocacy to improve adolescent sexual and reproductive health and rights in sub-Saharan Africa. BMJ Glob Health. 2021;6(4):e005571. doi:10.1136/bmjgh-2021-005571
69. Newland J, Lestari D, Poedjanadi MN, Kelly-Hanku A. Co-locating art and health: engaging civil society to create an enabling environment to respond to HIV in Indonesia. Sex Health. 2021;18(1):84–94. doi:10.1071/SH20125
70. Nkomazana O, Mash R, Wojczewski S, Kutalek R, Phaladze N. How to create more supportive supervision for primary healthcare: lessons from Ngamiland district of Botswana: co-operative inquiry group. Glob Health Action. 2016;24(9):31263. doi:10.3402/gha.v9.31263
71. Ostrom E. Crossing the great divide: coproduction, synergy, and development. World Dev. 1996;24(6):1073–1087. doi:10.1016/0305-750X(96)00023-X
72. Ozdemir V, Muljono DH, Pang T, et al. Asia-pacific health 2020 and genomics without borders: co-production of knowledge by science and society partnership for global personalized medicine. Curr Pharmacogenomics Person Med. 2011;9(1):1–5. doi:10.2174/187569211794728841
73. Sukkird V, Shirahada K. Technology challenges to healthcare service innovation in aging Asia: case of value co-creation in emergency medical support system. Technol Soc. 2015;43:122–128. doi:10.1016/j.techsoc.2015.08.002
74. Willems A, Iyamuremye JD, Misage CN, Smith-Swintosky V, Kayiteshonga Y. Co-creation and evaluation of nationwide remote training service for mental health education of community health workers in Rwanda. Front Public Health. 2021;24(9):632793. doi:10.3389/fpubh.2021.632793
75. Yan YH, Yang CW, Fang SC. Patient-centred e-health supports value cocreation and quality of medical care in Taiwan. Health Info Libr J. 2022;39(1):68–78. doi:10.1111/hir.12372
76. Yin L, Fassi D, Cheng H, Han H, He S. Health co-creation in social innovation: design service for health-empowered society in China. Design J. 2017;20(sup1):S2293–S2303. doi:10.1080/14606925.2017.1352745
77. Yokota F, Biyani M, Islam R, et al. Lessons learned from co-design and co-production in a portable health clinic research project in Jaipur District, India (2016–2018). Sustainability. 2018;10(11):4148. doi:10.3390/su10114148
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

